Mapping Alveolar Oxygen Partial Pressure in COPD Using Hyperpolarized Helium-3: The Multi-Ethnic Study of Atherosclerosis (MESA) COPD Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. HP 3He Production and MRI Hardware
2.3. MRI Acquisition
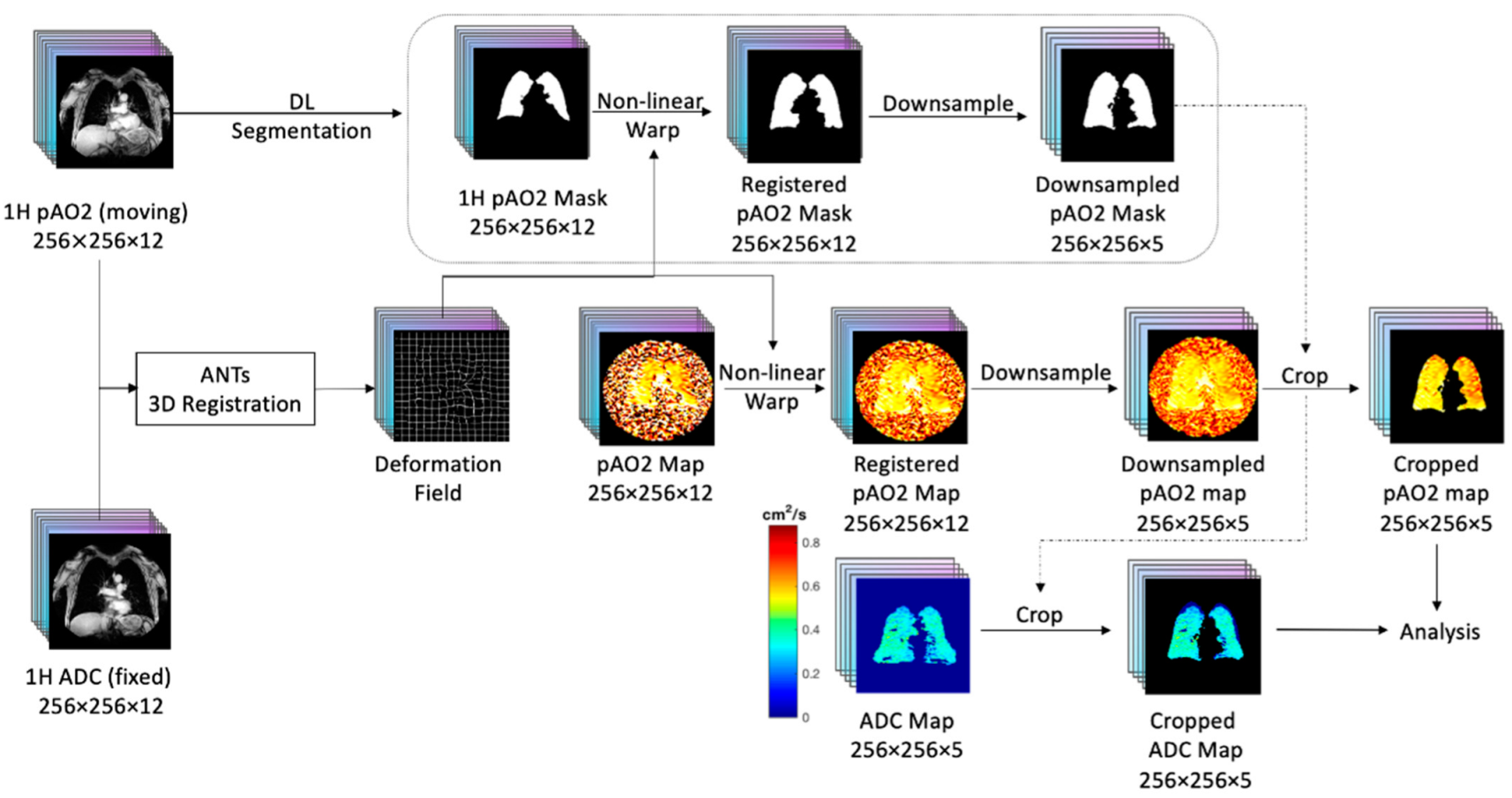
2.4. Co-Registration of HP 3He ADC with pAO2
2.5. Regional Divisions Using Proton MRI and 3He Ventilation Data
2.6. Non-Physiologic Results for pAO2
2.7. CT Measures
2.8. Pulmonary Function Testing
2.9. Statistical Analysis
3. Results
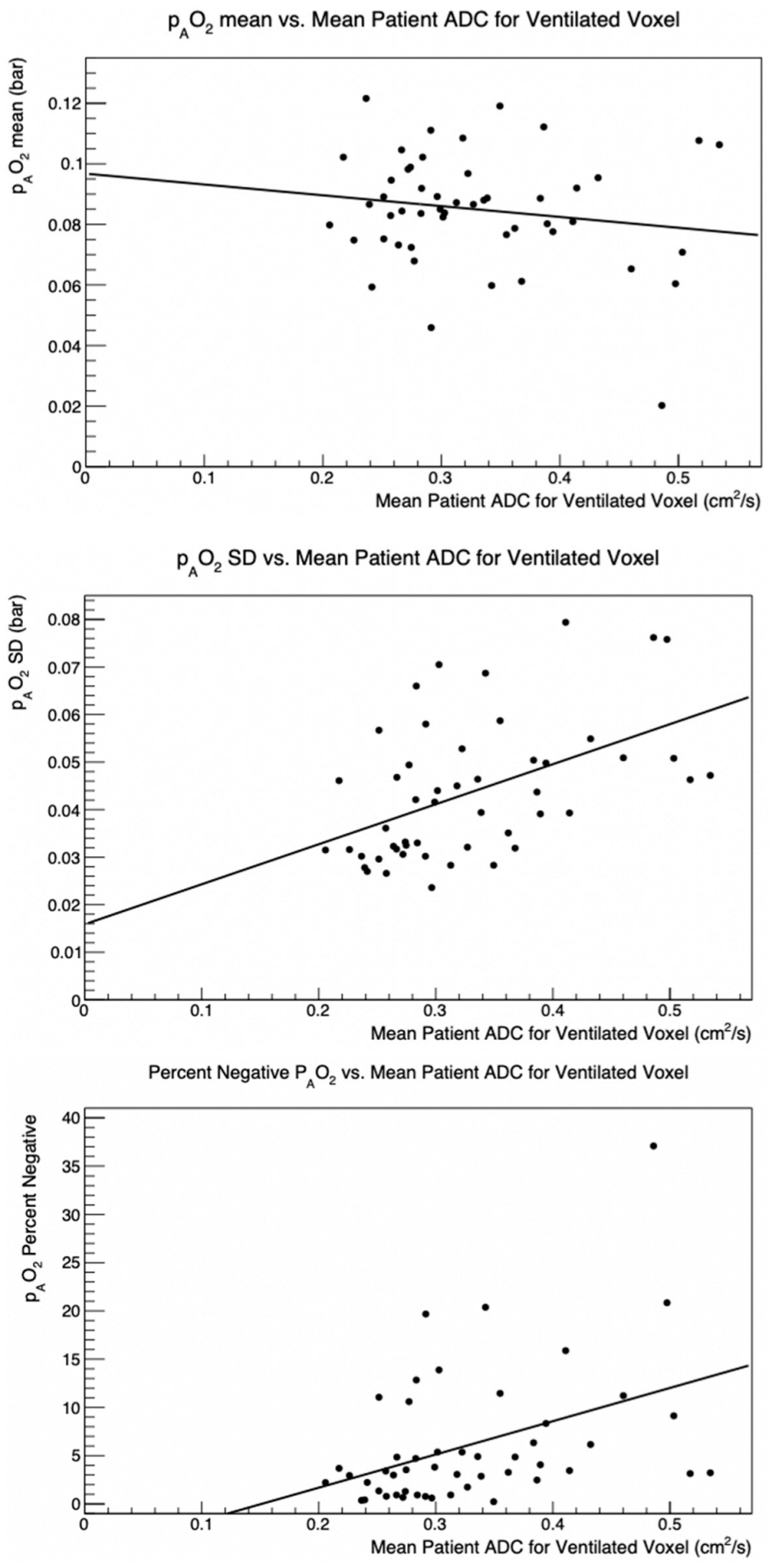
3.1. Global pAO2 versus ADC
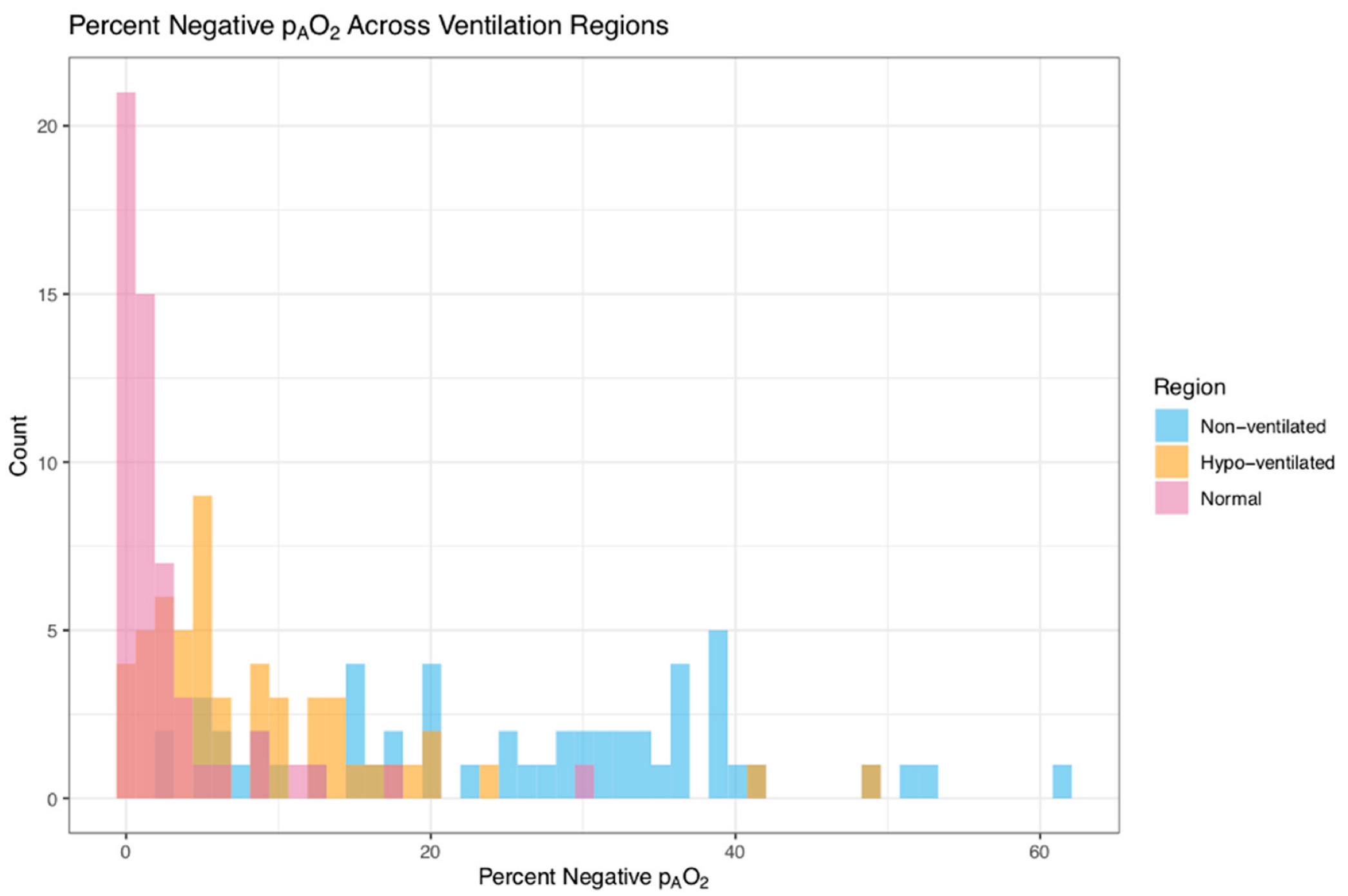
3.2. Negative pAO2 Results
3.3. Global pAO2 and Percent Emphysema
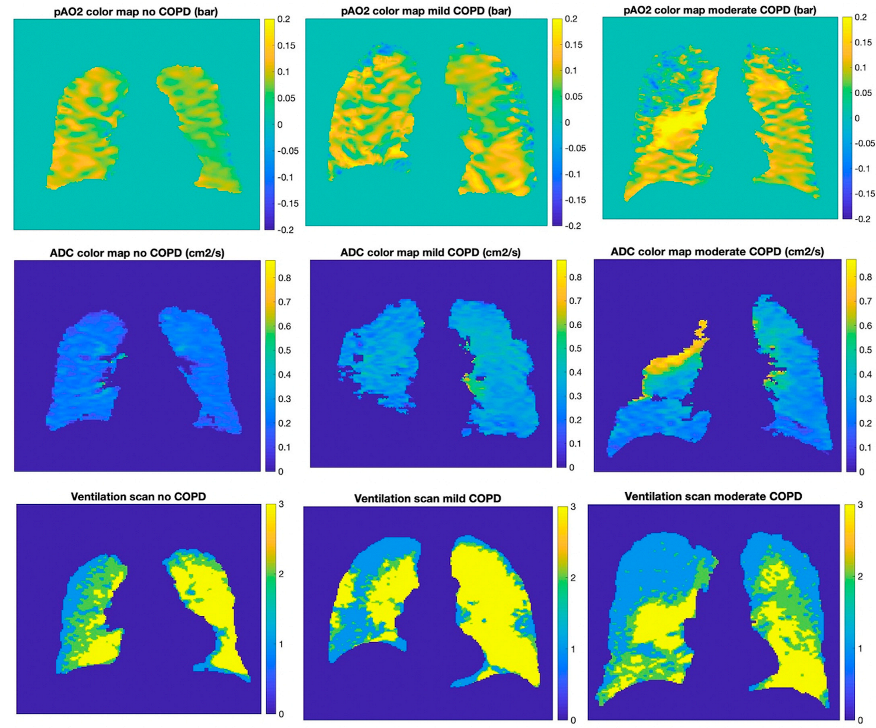
3.4. Measurements of pAO2 in Different Ventilation Regions
3.5. Global pAO2 Measurements Compared to Carbon Monoxide Diffusion Capacity
3.6. Regional pAO2 Measurements Compared to Traditional Emphysema Subtypes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. The Top 10 Causes of Death; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Scadding, J. Meaning of diagnostic terms in broncho-pulmonary disease. Br. Med. J. 1963, 2, 1425–1430. [Google Scholar] [CrossRef]
- James, J.; Dyson, J. Cave Science Topics: CO2 in Caves. Caving Int. 1981, 13, 54–59. [Google Scholar]
- Smith, B.M.; Austin, J.H.; Newell, J.D.; D’Souza, B.M.; Rozenshtein, A.; Hoffman, E.; Ahmed, F.; Barr, R.G. Pulmonary emphysema subtypes on computed tomography: The MESA COPD study. Am. J. Med. 2014, 127, 94.e7–94.e23. [Google Scholar] [CrossRef]
- MacNeil, J.L.; Capaldi, D.P.I.; Westcott, A.R.; Eddy, R.L.; Barker, A.L.; McCormack, D.G.; Kirby, M.; Parraga, G. Pulmonary Imaging Phenotypes of Chronic Obstructive Pulmonary Disease Using Multiparametric Response Maps. Radiology 2020, 295, 227–236. [Google Scholar] [CrossRef]
- Albert, M.S.; Cates, G.; Driehuys, B.; Happer, W.; Saam, B.; Springer, C.S., Jr.; Wishnia, A. Biological magnetic resonance imaging using laser-polarized 129Xe. Nature 1994, 370, 199–201. [Google Scholar] [CrossRef]
- Kirby, M.; Mathew, L.; Wheatley, A.; Santyr, G.E.; McCormack, D.G.; Parraga, G. Chronic obstructive pulmonary disease: Longitudinal hyperpolarized 3He MR imaging. Radiology 2010, 256, 280–289. [Google Scholar] [CrossRef]
- Wild, J.M.; Fichele, S.; Woodhouse, N.; Paley, M.N.; Kasuboski, L.; van Beek, E.J. 3D volume-localized pO2 measurement in the human lung with 3He MRI. Magn. Reson. Med. 2005, 53, 1055–1064. [Google Scholar] [CrossRef]
- Miller, G.W.; Mugler, J.P., 3rd; Altes, T.A.; Cai, J.; Mata, J.F.; de Lange, E.E.; Tobias, W.A.; Cates, G.D.; Brookeman, J.R. A short-breath-hold technique for lung pO2 mapping with 3He MRI. Magn. Reson. Med. 2010, 63, 127–136. [Google Scholar] [CrossRef]
- Hamedani, H.; Kadlecek, S.J.; Emami, K.; Kuzma, N.N.; Xu, Y.; Xin, Y.; Mongkolwisetwara, P.; Rajaei, J.; Barulic, A.; Wilson Miller, G.; et al. A multislice single breath-hold scheme for imaging alveolar oxygen tension in humans. Magn. Reson. Med. 2012, 67, 1332–1345. [Google Scholar] [CrossRef]
- Rizi, R.R.; Baumgardner, J.E.; Ishii, M.; Spector, Z.Z.; Edvinsson, J.M.; Jalali, A.; Yu, J.; Itkin, M.; Lipson, D.A.; Gefter, W. Determination of regional VA/Q by hyperpolarized 3He MRI. Magn. Reson. Med. 2004, 52, 65–72. [Google Scholar] [CrossRef]
- De Lange, E.E.; Mugler, J.P., 3rd; Brookeman, J.R.; Knight-Scott, J.; Truwit, J.D.; Teates, C.D.; Daniel, T.M.; Bogorad, P.L.; Cates, G.D. Lung air spaces: MR imaging evaluation with hyperpolarized 3He gas. Radiology 1999, 210, 851–857. [Google Scholar] [CrossRef]
- Guenther, D.; Eberle, B.; Hast, J.; Lill, J.; Markstaller, K.; Puderbach, M.; Schreiber, W.G.; Hanisch, G.; Heussel, C.P.; Surkau, R.; et al. 3He MRI in healthy volunteers: Preliminary correlation with smoking history and lung volumes. NMR Biomed. 2000, 13, 182–189. [Google Scholar] [CrossRef]
- Parraga, G.; Ouriadov, A.; Evans, A.; McKay, S.; Lam, W.W.; Fenster, A.; Etemad-Rezai, R.; McCormack, D.; Santyr, G. Hyperpolarized 3He ventilation defects and apparent diffusion coefficients in chronic obstructive pulmonary disease: Preliminary results at 3.0 Tesla. Investig. Radiol. 2007, 42, 384–391. [Google Scholar] [CrossRef]
- Mathew, L.; Evans, A.; Ouriadov, A.; Etemad-Rezai, R.; Fogel, R.; Santyr, G.; McCormack, D.G.; Parraga, G. Hyperpolarized 3He magnetic resonance imaging of chronic obstructive pulmonary disease: Reproducibility at 3.0 tesla. Acad. Radiol. 2008, 15, 1298–1311. [Google Scholar] [CrossRef]
- Van Beek, E.J.; Dahmen, A.M.; Stavngaard, T.; Gast, K.K.; Heussel, C.P.; Krummenauer, F.; Schmiedeskamp, J.; Wild, J.M.; Søgaard, L.V.; Morbach, A.E.; et al. Hyperpolarised 3He MRI versus HRCT in COPD and normal volunteers: PHIL trial. Eur. Respir. J. 2009, 34, 1311–1321. [Google Scholar] [CrossRef]
- Deninger, A.J.; Eberle, B.; Ebert, M.; Grossmann, T.; Heil, W.; Kauczor, H.; Lauer, L.; Markstaller, K.; Otten, E.; Schmiedeskamp, J.; et al. Quantification of regional intrapulmonary oxygen partial pressure evolution during apnea by 3He MRI. J. Magn. Reson. 1999, 141, 207–216. [Google Scholar] [CrossRef]
- Marshall, H.; Parra-Robles, J.; Deppe, M.H.; Lipson, D.A.; Lawson, R.; Wild, J.M. 3He pO2 mapping is limited by delayed-ventilation and diffusion in chronic obstructive pulmonary disease. Magn. Reson. Med. 2014, 71, 1172–1178. [Google Scholar] [CrossRef]
- Achekzai, T.; Hamedani, H.; Kadlecek, S.J.; Ruppert, K.; Xin, Y.; Baron, R.J.; Duncan, I.F.; Sertic, F.; Siddiqui, S.; Amzajerdian, F.; et al. Multibreath Hyperpolarized 3He Imaging Scheme to Measure Alveolar Oxygen Tension and Apparent Diffusion Coefficient. Acad. Radiol. 2019, 26, 367–382. [Google Scholar] [CrossRef]
- Quirk, J.D.; Lutey, B.A.; Gierada, D.S.; Woods, J.C.; Senior, R.M.; Lefrak, S.S.; Sukstanskii, A.L.; Conradi, M.S.; Yablonskiy, D.A. In vivo detection of acinar microstructural changes in early emphysema with 3He lung morphometry. Radiology 2011, 260, 866–874. [Google Scholar] [CrossRef]
- Yablonskiy, D.A.; Sukstanskii, A.L.; Leawoods, J.C.; Gierada, D.S.; Bretthorst, G.L.; Lefrak, S.S.; Cooper, J.D.; Conradi, M.S. Quantitative in vivo assessment of lung microstructure at the alveolar level with hyperpolarized 3He diffusion MRI. Proc. Natl. Acad. Sci. USA 2002, 99, 3111–3116. [Google Scholar] [CrossRef]
- Sukstanskii, A.L.; Yablonskiy, D.A. In vivo lung morphometry with hyperpolarized 3He diffusion MRI: Theoretical background. J. Magn. Reson. 2008, 190, 200–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paulin, G.A.; Ouriadov, A.; Lessard, E.; Sheikh, K.; McCormack, D.G.; Parraga, G. Noninvasive quantification of alveolar morphometry in elderly never- and ex-smokers. Physiol. Rep. 2015, 3, e12583. [Google Scholar] [CrossRef] [PubMed]
- Fichele, S.; Paley, M.N.; Woodhouse, N.; Griffiths, P.D.; Van Beek, E.J.; Wild, J.M. Finite-difference simulations of 3He diffusion in 3D alveolar ducts: Comparison with the “cylinder model”. Magn. Reson. Med. 2004, 52, 917–920. [Google Scholar] [CrossRef]
- Chan, H.F.; Stewart, N.J.; Norquay, G.; Collier, G.J.; Wild, J.M. 3D diffusion-weighted 129Xe MRI for whole lung morphometry. Magn. Reson. Med. 2018, 79, 2986–2995. [Google Scholar] [CrossRef] [PubMed]
- Evans, A.; McCormack, D.G.; Santyr, G.; Parraga, G. Mapping and quantifying hyperpolarized 3He magnetic resonance imaging apparent diffusion coefficient gradients. J. Appl. Physiol. 2008, 105, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Capaldi, D.P.; Zha, N.; Guo, F.; Pike, D.; McCormack, D.G.; Kirby, M.; Parraga, G. Pulmonary Imaging Biomarkers of Gas Trapping and Emphysema in COPD: 3He MR Imaging and CT Parametric Response Maps. Radiology 2016, 279, 597–608. [Google Scholar] [CrossRef] [PubMed]
- Shen, W.; Yang, J.; Sun, Y.; Hiura, G.; Balte, P.; Dashnaw, S.; Prince, M.; Hoffman, E.; Venkatesh, B.; Lima, J.; et al. Late Breaking Abstract—Apparent Diffusion Coefficient by 3He MRI and quantitative emphysema subtypes by CT. Eur. Respir. J. 2019, 54, OA1929. [Google Scholar]
- Barker, A.L.; Eddy, R.L.; MacNeil, J.L.; McCormack, D.G.; Kirby, M.; Parraga, G. CT pulmonary vessels and MRI ventilation in chronic obstructive pulmonary disease: Relationship with worsening FEV1 in the TINCan cohort study. Acad. Radiol. 2021, 28, 495–506. [Google Scholar] [CrossRef]
- Bild, D.E.; Bluemke, D.A.; Burke, G.L.; Detrano, R.; Diez Roux, A.V.; Folsom, A.R.; Greenland, P.; Jacob, D.R., Jr.; Kronmal, R.; Liu, K.; et al. Multi-Ethnic Study of Atherosclerosis: Objectives and design. Am. J. Epidemiol. 2002, 156, 871–881. [Google Scholar] [CrossRef]
- Smith, B.M.; Hoffman, E.A.; Rabinowitz, D.; Bleecker, E.; Christenson, S.; Couper, D.; Donohue, K.M.; Han, M.K.; Hansel, N.N.; Kanner, R.E.; et al. Comparison of spatially matched airways reveals thinner airway walls in COPD. The Multi-Ethnic Study of Atherosclerosis (MESA) COPD Study and the Subpopulations and Intermediate Outcomes in COPD Study (SPIROMICS). Thorax 2014, 69, 987–996. [Google Scholar] [CrossRef]
- Chupp, T.E.; Wagshul, M.E.; Coulter, K.P.; McDonald, A.B.; Happer, W. Polarized, high-density, gaseous 3He targets. Phys. Rev. C Nucl. Phys. 1987, 36, 2244–2251. [Google Scholar] [CrossRef] [PubMed]
- Deninger, A.J.; Eberle, B.; Bermuth, J.; Escat, B.; Markstaller, K.; Schmiedeskamp, J.; Schreiber, W.G.; Surkau, R.; Otten, E.; Kauczor, H.U. Assessment of a single-acquisition imaging sequence for oxygen-sensitive 3He-MRI. Magn. Reson. Med. 2002, 47, 105–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deninger, A.J.; Eberle, B.; Ebert, M.; Grossmann, T.; Hanisch, G.; Heil, W.; Kauczor, H.U.; Markstaller, K.; Otten, E.; Schreiber, W.; et al. 3He-MRI-based measurements of intrapulmonary pO2 and its time course during apnea in healthy volunteers: First results, reproducibility, and technical limitations. NMR Biomed. 2000, 13, 194–201. [Google Scholar] [CrossRef]
- Hamedani, H.; Clapp, J.; Kadlecek, S.; Rizi, R.R. PAO2 Mapping using HP Gas MRI. In Hyperpolarized Inert Gas MRI; Elsevier: Amsterdam, The Netherlands, 2017. [Google Scholar]
- Saam, B.; Happer, W.; Middleton, H. Nuclear relaxation of 3He in the presence of O2. Phys. Rev. A 1995, 52, 862–865. [Google Scholar] [CrossRef] [PubMed]
- Avants, B.B.; Tustison, N.; Song, G. Advanced Normalization Tools (ANTS); University of Pennsylvania: Philadelphia, PA, USA, 2011. [Google Scholar]
- Hughes, P.J.C.; Smith, L.; Chan, H.F.; Tahir, B.A.; Norquay, G.; Collier, G.J.; Biancardi, A.; Marshall, H.; Wild, J.M. Assessment of the influence of lung inflation state on the quantitative parameters derived from hyperpolarized gas lung ventilation MRI in healthy volunteers. J. Appl. Physiol. 2019, 126, 183–192. [Google Scholar] [CrossRef]
- Zhang, X.; Angelini, E.D.; Haghpanah, F.S.; Laine, A.F.; Sun, Y.; Hiura, G.T.; Dashnaw, S.M.; Prince, M.R.; Hoffman, E.A.; Ambale-Venkatesh, B.; et al. Quantification of lung ventilation defects on hyperpolarized MRI: The Multi-Ethnic Study of Atherosclerosis (MESA) COPD study. Magn. Reson. Imaging 2022, 92, 140–149. [Google Scholar] [CrossRef]
- Sieren, J.P.; Newell, J.D., Jr.; Barr, R.G.; Bleecker, E.R.; Burnette, N.; Carretta, E.E.; Couper, D.; Goldin, J.; Guo, J.; Han, M.K. SPIROMICS protocol for Multicenter Quantitative Computed Tomography to phenotype the lungs. Am. J. Respir. Crit. Care Med. 2016, 194, 794–806. [Google Scholar] [CrossRef]
- Grau, M.; Barr, R.G.; Lima, J.A.; Hoffman, E.A.; Bluemke, D.A.; Carr, J.J.; Chahal, H.; Enright, P.L.; Jain, A.; Prince, M.R.; et al. Percent emphysema and right ventricular structure and function: The Multi-Ethnic Study of Atherosclerosis-Lung and Multi-Ethnic Study of Atherosclerosis-Right Ventricle Studies. Chest 2013, 144, 136–144. [Google Scholar] [CrossRef]
- Smith, B.M.; Kawut, S.M.; Bluemke, D.A.; Basner, R.C.; Gomes, A.S.; Hoffman, E.; Kalhan, R.; Lima, J.A.; Liu, C.Y.; Michos, E.D.; et al. Pulmonary hyperinflation and left ventricular mass: The Multi-Ethnic Study of Atherosclerosis COPD Study. Circulation 2013, 127, 1503–1511, 1511.e1–1511.e6. [Google Scholar] [CrossRef]
- Ouriadov, A.; Farag, A.; Kirby, M.; McCormack, D.G.; Parraga, G.; Santyr, G.E. Pulmonary hyperpolarized 129Xe morphometry for mapping xenon gas concentrations and alveolar oxygen partial pressure: Proof-of-concept demonstration in healthy and COPD subjects. Magn. Reson. Med. 2015, 74, 1726–1732. [Google Scholar] [CrossRef]
| Characteristic | All Participants (n = 54) |
|---|---|
| Age, years—mean ± SD | 73.3 ± 7.4 |
| Female—N (%) | 22 (40.7%) |
| Race/Ethnicity—N (%) | |
| White | 28 (51.9%) |
| Black | 17 (31.5%) |
| Hispanic | 9 (16.6%) |
| Height, cm—mean ± SD | 175.8 ± 4.8 |
| Weight, lb—mean ± SD | 75.8 ± 14.2 |
| Smoking status—N (%) | |
| Former smoker | 38 (70.4%) |
| Current smoker | 16 (29.6%) |
| Pack-years—mean ± SD | 41.3 ± 23.0 |
| Educational attainment—N (%) | |
| <High school degree | 15 (27.8%) |
| College degree | 24 (44.4%) |
| Some college/2-year degree | 15 (27.8%) |
| Spirometry (post-bronchodilator) | |
| FEV1 (mL)—mean ± SD, n = 53 | 2157 ± 577 |
| FVC (mL)—mean ± SD, n = 53 | 3326 ± 965 |
| FEV1/FVC—mean ± SD, n = 53 | 0.67 ± 0.13 |
| COPD—No. (%) | 29 (53.7%) |
| COPD severity—N (%) | |
| None | 25 (46.3%) |
| Mild | 13 (24.1%) |
| Moderate | 16 (29.6%) |
| CT measures | |
| Total lung volume (mL)—mean ± SD | 5460 ± 1353 |
| Total tissue volume (mL)—mean ± SD | 835 ± 176 |
| Total air volume (mL)—mean ± SD | 4625 ± 1220 |
| % emphysema −950 HU—median [IQR] | 2.1 [0.9, 7.1] |
| Visual emphysema severity (%) 1—median [IQR] | 0.24 [0, 2.31] |
| DLCO measures, n = 34 | |
| DLCO (%)—mean ± SD | 18.1 ± 4.9 |
| 3He MRI measures | |
| pAO2 mean (bar)—median [IQR] | 0.093 [0.084, 0.103] |
| pAO2 SD (bar)—median [IQR] | 0.052 [0.037, 0.064] |
| pAO2 %negative—median [IQR] | 4.9 [2.1, 7.5] |
| ADC mean (cm2/s)—median [IQR] | 0.302 [0.267, 0.383] |
| Scan | 3He | N2 | Breath-Hold |
|---|---|---|---|
| Calibration | 150 cc | - | - |
| Ventilation | 300 cc | 700 cc | TLC |
| ADC | 500 cc | 500 cc | TLC |
| pAO2 | 350 cc | 650 cc | FRC + 1 L |
| Global pAO2 Mean 1 | Global pAO2 SD 1 | Global pAO2 %Negative 1 | ADC Mean 1 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Measure | N | ρ (95% CI) | p | ρ (95% CI) | p | ρ (95% CI) | p | ρ (95% CI) | p |
| %emphysema −950 HU | 54 | −0.08 (−0.34, 0.20) | 0.59 | 0.48 (0.24, 0.66) | 0.0002 * | 0.50 (0.27, 0.68) | <0.0001 * | 0.81 (0.68, 0.89) | <0.0001 * |
| Visual emphysema severity (%) 2 | 50 | 0.24 (−0.05, 0.48) | 0.10 | 0.38 (0.11, 0.59) | 0.006 * | 0.32 (0.04, 0.55) | 0.02 * | 0.66 (0.44, 0.79) | <0.0001 * |
| ADC mean (cm2/s) | 50 | −0.07 (−0.34, 0.21) | 0.61 | 0.53 (0.29, 0.70) | <0.0001 * | 0.45 (0.20, 0.65) | 0.0008 * | - | - |
| pAO2 Mean | pAO2 SD | pAO2 %Negative | |||||
|---|---|---|---|---|---|---|---|
| Exposure | N | β (95% CI) | p | β (95% CI) | p | β (95% CI) | p |
| %emphysema −950 HU | |||||||
| Unadjusted | 54 | −0.0007 (−0.002, 0.0005) | 0.26 | 0.002 (0.0009, 0.003) | 0.0002 * | 0.57 (0.29, 0.86) | 0.0002 * |
| Model 1 | 54 | −0.0003 (−0.002, 0.0009) | 0.62 | 0.001 (0.0003, 0.002) | 0.005 * | 0.37 (0.11, 0.63) | 0.007 * |
| Model 2 | 53 | −0.0001 (−0.001, 0.001) | 0.85 | 0.001 (0.0003, 0.002) | 0.006 * | 0.32 (0.05, 0.60) | 0.02 * |
| Visual emphysema severity (%) 1 | |||||||
| Unadjusted | 50 | −0.0002 (−0.001, 0.0006) | 0.64 | 0.0008 (0.0002, 0.001) | 0.01 * | 0.29 (0.10, 0.48) | 0.004 * |
| Model 1 | 50 | −0.00005 (−0.0008, 0.0007) | 0.90 | 0.0005 (0.0001, 0.001) | 0.02 * | 0.22 (0.05, 0.38) | 0.01 * |
| Model 2 | 49 | 0.00006 (−0.0008, 0.0009) | 0.89 | 0.0005 (0.00003, 0.001) | 0.04 * | 0.19 (0.01, 0.36) | 0.04 * |
| ADC 2 | |||||||
| Unadjusted | 50 | −0.0005 (−0.001, 0.0002) | 0.17 | 0.0008 (0.0003, 0.001) | 0.003 * | 0.36 (0.12, 0.61) | 0.004 * |
| Model 1 | 50 | −0.0004 (−0.001, 0.0004) | 0.33 | 0.0007 (0.0002, 0.001) | 0.005 * | 0.30 (0.08, 0.53) | 0.01 * |
| Model 2 | 49 | −0.0002 (−0.001, 0.0006) | 0.63 | 0.0006 (0.0002, 0.001) | 0.01 * | 0.24 (0.02, 0.47) | 0.04 * |
| DLCO | |||||||
| Unadjusted | 34 | −0.0003 (−0.002, 0.001) | 0.65 | 0.001 (0.0003, 0.002) | 0.007 * | 0.23 (0.05, 0.41) | 0.01 * |
| Model 1 | 34 | −0.0001 (−0.002, 0.002) | 0.93 | −0.001 (−0.002, −0.00003) | 0.04 * | −0.22 (−0.46, 0.01) | 0.06 |
| Model 2 | 34 | −0.0001 (−0.002, 0.002) | 0.91 | −0.001 (−0.002, −0.00004) | 0.04 * | −0.22 (−0.45, 0.01) | 0.06 |
| pAO2 Mean | pAO2 SD | pAO2 %Negative | ||||
|---|---|---|---|---|---|---|
| Exposure | β (95% CI) | p | β (95% CI) | p | β (95% CI) | p |
| %emphysema, log-transformed 1 | ||||||
| Unadjusted (n = 54) | 0.0001 (−0.003, 0.003) | 0.94 | 0.0006 (−0.002, 0.003) | 0.61 | 0.43 (−0.44, 1.30) | 0.33 |
| Model 1 (n = 54) | 0.0008 (−0.002, 0.004) | 0.59 | 0.00002 (−0.002, 0.002) | 0.99 | 0.15 (−0.71, 1.01) | 0.73 |
| Model 2 (n = 53) | 0.001 (−0.002, 0.004) | 0.39 | −0.0004 (−0.003, 0.002) | 0.74 | −0.05 (−0.92, 0.81) | 0.90 |
| Visual emphysema severity (%), log-transformed 1,2 | ||||||
| Unadjusted (n = 50) | −0.0007 (−0.005, 0.004) | 0.73 | 0.006 (0.002, 0.009) | 0.001 * | 1.61 (0.36, 2.86) | 0.01 * |
| Model 1 (n = 50) | −0.0005 (−0.005, 0.004) | 0.80 | 0.005 (0.002, 0.008) | 0.003 * | 1.46 (0.29, 2.63) | 0.01 * |
| Model 2 (n = 49) | 0.0009 (−0.004, 0.005) | 0.69 | 0.003 (0.0001, 0.007) | 0.04 * | 0.87 (−0.38, 2.11) | 0.17 |
| Severity scores of pulmonary emphysema subtypes, log-transformed 1,3 | ||||||
| Unadjusted (n = 50) | ||||||
| CLE severity | 0.003 (−0.004, 0.009) | 0.38 | −0.0006 (−0.006, 0.005) | 0.82 | −0.42 (−2.31, 1.48) | 0.67 |
| PLE severity | 0.001 (−0.005, 0.008) | 0.68 | 0.002 (−0.002, 0.007) | 0.33 | 0.96 (−0.84, 2.76) | 0.30 |
| PSE severity | −0.006 (−0.01, 0.002) | 0.13 | 0.008 (0.002, 0.01) | 0.005 * | 2.29 (0.22, 4.37) | 0.03 * |
| Model 1 (n = 50) | ||||||
| CLE severity | 0.003 (−0.004, 0.009) | 0.39 | −0.0001 (−0.005, 0.005) | 0.97 | −0.20 (−2.02, 1.62) | 0.83 |
| PLE severity | 0.001 (−0.005, 0.007) | 0.76 | 0.002 (−0.002, 0.007) | 0.29 | 1.31 (−0.46, 3.08) | 0.15 |
| PSE severity | −0.004 (−0.01, 0.003) | 0.24 | 0.006 (0.0002, 0.01) | 0.04 * | 1.53 (−0.54, 3.60) | 0.15 |
| Model 2 (n = 49) | ||||||
| CLE severity | 0.004 (−0.003, 0.01) | 0.29 | −0.001 (−0.006, 0.004) | 0.69 | −0.56 (−2.42, 1.30) | 0.56 |
| PLE severity | 0.0009 (−0.005, 0.007) | 0.77 | 0.003 (−0.002, 0.007) | 0.28 | 1.33 (−0.44, 3.09) | 0.14 |
| PSE severity | −0.003 (−0.01, 0.005) | 0.50 | 0.004 (−0.002, 0.01) | 0.17 | 0.69 (−1.45, 2.83) | 0.53 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taskiran, N.P.; Hiura, G.T.; Zhang, X.; Barr, R.G.; Dashnaw, S.M.; Hoffman, E.A.; Malinsky, D.; Oelsner, E.C.; Prince, M.R.; Smith, B.M.; et al. Mapping Alveolar Oxygen Partial Pressure in COPD Using Hyperpolarized Helium-3: The Multi-Ethnic Study of Atherosclerosis (MESA) COPD Study. Tomography 2022, 8, 2268-2284. https://doi.org/10.3390/tomography8050190
Taskiran NP, Hiura GT, Zhang X, Barr RG, Dashnaw SM, Hoffman EA, Malinsky D, Oelsner EC, Prince MR, Smith BM, et al. Mapping Alveolar Oxygen Partial Pressure in COPD Using Hyperpolarized Helium-3: The Multi-Ethnic Study of Atherosclerosis (MESA) COPD Study. Tomography. 2022; 8(5):2268-2284. https://doi.org/10.3390/tomography8050190
Chicago/Turabian StyleTaskiran, Naz P., Grant T. Hiura, Xuzhe Zhang, R. Graham Barr, Stephen M. Dashnaw, Eric A. Hoffman, Daniel Malinsky, Elizabeth C. Oelsner, Martin R. Prince, Benjamin M. Smith, and et al. 2022. "Mapping Alveolar Oxygen Partial Pressure in COPD Using Hyperpolarized Helium-3: The Multi-Ethnic Study of Atherosclerosis (MESA) COPD Study" Tomography 8, no. 5: 2268-2284. https://doi.org/10.3390/tomography8050190
APA StyleTaskiran, N. P., Hiura, G. T., Zhang, X., Barr, R. G., Dashnaw, S. M., Hoffman, E. A., Malinsky, D., Oelsner, E. C., Prince, M. R., Smith, B. M., Sun, Y., Sun, Y., Wild, J. M., Shen, W., & Hughes, E. W. (2022). Mapping Alveolar Oxygen Partial Pressure in COPD Using Hyperpolarized Helium-3: The Multi-Ethnic Study of Atherosclerosis (MESA) COPD Study. Tomography, 8(5), 2268-2284. https://doi.org/10.3390/tomography8050190






