Efficacy and Safety of Cone-Beam CT Augmented Electromagnetic Navigation Guided Bronchoscopic Biopsies of Indeterminate Pulmonary Nodules
Abstract
:1. Introduction
2. Methods
2.1. Study Cohort
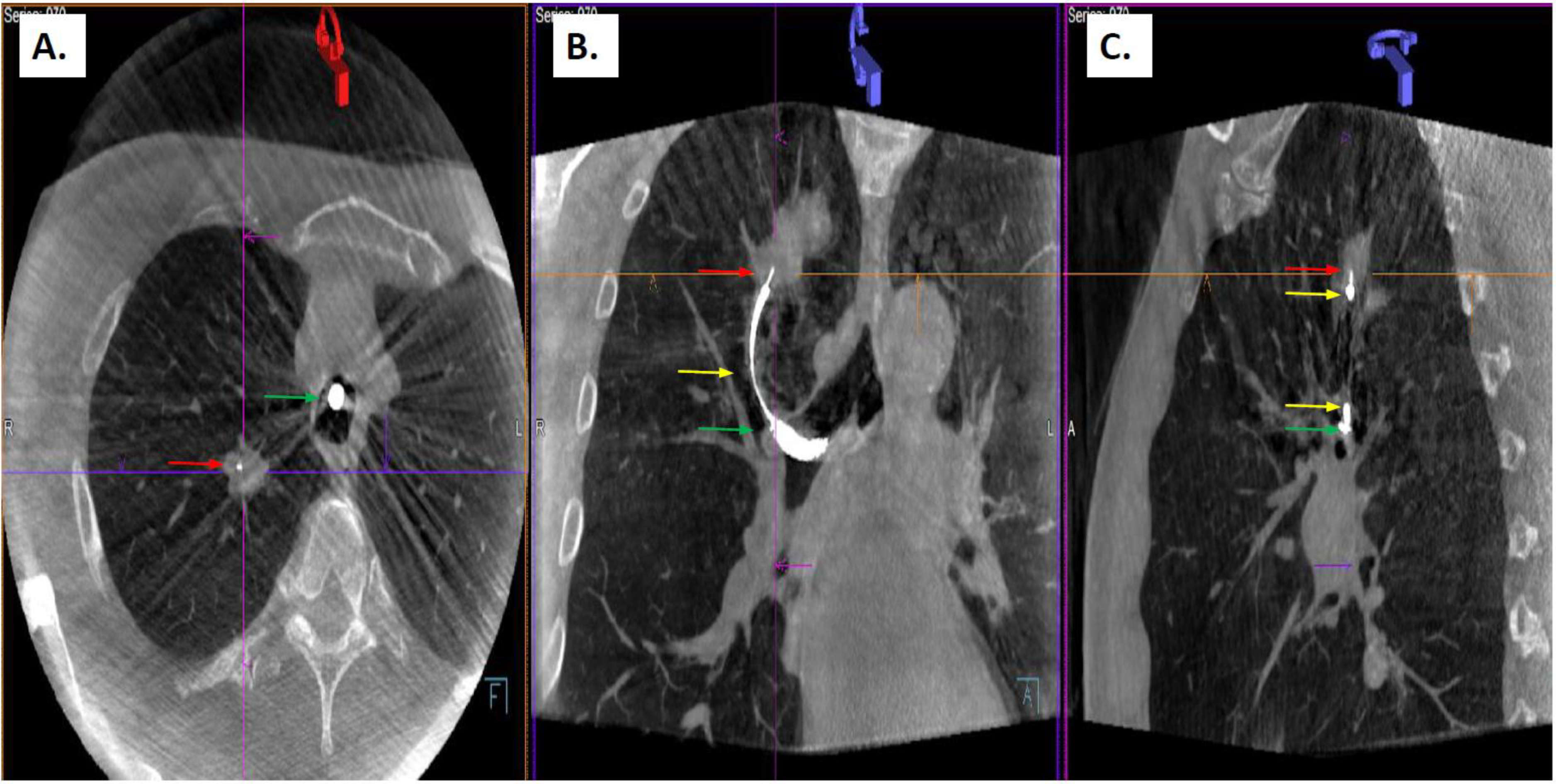
2.2. Procedure Description
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Disclosures
Abbreviations
| CBCT | cone beam CT |
| CT | computed tomography |
| CTBD | CT scan to body divergence |
| ENB | electromagnetic navigation guided biopsy |
| EWC | extended working channel |
| LG | locatable guide |
| RAB | robotic-assisted bronchoscopy |
| REBUS | radial endobronchial ultrasound |
| ssRAB | shape-sensing robotic-assisted bronchoscopy |
| TTNA | transthoracic needle aspiration |
References
- Aberle, D.R.; Adams, A.M.; Berg, C.D.; Black, W.C.; Clapp, J.D. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef] [PubMed]
- De Koning, H.J.; Van Der Aalst, C.M.; De Jong, P.A.; Scholten, E.T.; Nackaerts, K.; Heuvelmans, M.A.; Lammers, J.-W.J.; Weenink, C.; Yousaf-Khan, U.; Horeweg, N.; et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N. Engl. J. Med. 2020, 382, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Jonas, D.E.; Reuland, D.S.; Reddy, S.M.; Nagle, M.; Clark, S.D.; Weber, R.P.; Enyioha, C.; Malo, T.L.; Brenner, A.T.; Armstrong, C.; et al. Screening for Lung Cancer with Low-Dose Computed Tomography: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2021, 325, 971–987. [Google Scholar] [CrossRef] [PubMed]
- Gould, M.K.; Tang, T.; Liu, I.-L.A.; Lee, J.; Zheng, C.; Danforth, K.N.; Kosco, A.E.; Di Fiore, J.L.; Suh, D.E. Recent Trends in the Identification of Incidental Pulmonary Nodules. Am. J. Respir. Crit. Care Med. 2015, 192, 1208–1214. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, M.S.; Drucker, E.A.; McLoud, T.C.; Shepard, J.-A.O. Small Pulmonary Nodules: Detection at Chest CT and Outcome. Radiology 2003, 226, 489–493. [Google Scholar] [CrossRef]
- Swensen, S.J.; Silverstein, M.D.; Ilstrup, D.M.; Schleck, C.D.; Edell, E.S. The probability of malignancy in solitary pulmonary nodules: Application to small radiologically indeterminate nodules. Arch. Intern. Med. 1997, 157, 849–855. [Google Scholar] [CrossRef]
- McWilliams, A.; Tammemagi, M.C.; Mayo, J.R.; Roberts, H.; Liu, G.; Soghrati, K.; Yasufuku, K.; Martel, S.; Laberge, F.; Gingras, M.; et al. Probability of Cancer in Pulmonary Nodules Detected on First Screening CT. N. Engl. J. Med. 2013, 369, 910–919. [Google Scholar] [CrossRef]
- Balekian, A.A.; Silvestri, G.A.; Simkovich, S.M.; Mestaz, P.J.; Sanders, G.D.; Daniel, J.; Porcel, J.; Gould, M.K. Accuracy of Clinicians and Models for Estimating the Probability That a Pulmonary Nodule Is Malignant. Ann. Am. Thorac. Soc. 2013, 10, 629–635. [Google Scholar] [CrossRef]
- Gaga, M.; Loverdos, K.; Fotiadis, A.; Kontogianni, C.; Iliopoulou, M. Lung nodules: A comprehensive review on current approach and management. Ann. Thorac. Med. 2019, 14, 226–238. [Google Scholar] [CrossRef]
- Rivera, M.P.; Mehta, A.C.; Wahidi, M.M. Establishing the diagnosis of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013, 143, e142S–e165S. [Google Scholar] [CrossRef]
- DiBardino, D.M.; Yarmus, L.B.; Semaan, R.W. Transthoracic needle biopsy of the lung. J. Thorac. Dis. 2015, 7, S304–S316. [Google Scholar] [PubMed]
- Jiang, J.; Chang, S.H.; Kent, A.J.; Geraci, T.C.; Cerfolio, R.J. Current Novel Advances in Bronchoscopy. Front. Surg. 2020, 7, 596925. [Google Scholar] [CrossRef] [PubMed]
- Gex, G.; Pralong, J.A.; Combescure, C.; Seijo, L.; Rochat, T.; Soccal, P.M. Diagnostic yield and safety of electromagnetic navigation bronchoscopy for lung nodules: A systematic review and meta-analysis. Respiration 2014, 87, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Memoli, J.S.W.; Nietert, P.J.; Silvestri, G.A. Meta-analysis of Guided Bronchoscopy for the Evaluation of the Pulmonary Nodule. Chest 2012, 142, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Khandhar, S.J.; Bowling, M.R.; Flandes, J.; Gildea, T.R.; Hood, K.L.; Krimsky, W.S.; Minnich, D.J.; Murgu, S.D.; Pritchett, M.; Toloza, E.M.; et al. Electromagnetic navigation bronchoscopy to access lung lesions in 1000 subjects: First results of the prospective, multicenter NAVIGATE study. BMC Pulm. Med. 2017, 17, 59. [Google Scholar] [CrossRef]
- Chen, A.; Pastis, N.; Furukawa, B.; Silvestri, G.A. The effect of respiratory motion on pulmonary nodule location during electromagnetic navigation bronchoscopy. Chest 2015, 147, 1275–1281. [Google Scholar] [CrossRef]
- Pritchett, M.A.; Bhadra, K.; Calcutt, M.; Folch, E. Virtual or reality: Divergence between preprocedural computed tomography scans and lung anatomy during guided bronchoscopy. J. Thorac. Dis. 2020, 8, 4593–4595. [Google Scholar] [CrossRef]
- Aboudara, M.; Roller, L.; Rickman, O.; Lentz, R.J.; Pannu, J.; Chen, H.; Maldonado, F. Improved diagnostic yield for lung nodules with digital tomosynthesis-corrected navigational bronchoscopy: Initial experience with a novel adjunct. Respirology 2020, 25, 206–213. [Google Scholar] [CrossRef]
- Avasarala, S.K.; Roller, L.; Katsis, J.; Chen, H.; Lentz, R.J.; Rickman, O.B.; Maldonado, F. Sight Unseen: Diagnostic Yield and Safety Outcomes of a Novel Multimodality Navigation Bronchoscopy Platform with Real-Time Target Acquisition. Respiration 2022, 101, 166–173. [Google Scholar] [CrossRef]
- Pritchett, M.A.; Bhadra, K.; Mattingley, J.S. Electromagnetic Navigation Bronchoscopy with Tomosynthesis-based Visualization and Positional Correction: Three-dimensional Accuracy as Confirmed by Cone-Beam Computed Tomography. J. Bronc. Interv. Pulmonol. 2021, 28, 10–20. [Google Scholar] [CrossRef]
- Semaan, R.W.; Lee, H.J.; Feller-Kopman, D.; Lerner, A.D.; Mallow, C.M.; Thiboutot, J.; Arias, S.A.; Yarmus, L.B. Same-Day Computed Tomographic Chest Imaging for Pulmonary Nodule Targeting with Electromagnetic Navigation Bronchoscopy May Decrease Unnecessary Procedures. Ann. Am. Thorac. Soc. 2016, 13, 2223–2228. [Google Scholar] [CrossRef]
- Furukawa, B.S.; Pastis, N.J.; Tanner, N.T.; Chen, A.; Silvestri, G.A. Comparing Pulmonary Nodule Location During Electromagnetic Bronchoscopy with Predicted Location on the Basis of Two Virtual Airway Maps at Different Phases of Respiration. Chest 2018, 153, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Lundquist, H.; Hedenstierna, G.; Strandberg, A.; Tokics, L.; Brismar, B. CT-assessment of dependent lung densities in man during general anaesthesia. Acta Radiol. 1995, 36, 626–632. [Google Scholar] [CrossRef]
- Ost, D.E.; Ernst, A.; Lei, X.; Kovitz, K.L.; Benzaquen, S.; Diaz-Mendoza, J.; Greenhill, S.; Toth, J.; Feller-Kopman, D.; Puchalski, J.; et al. Diagnostic Yield and Complications of Bronchoscopy for Peripheral Lung Lesions. Results of the AQuIRE Registry. Am. J. Respir. Crit. Care Med. 2016, 193, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Folch, E.E.; Pritchett, M.A.; Nead, M.A.; Bowling, M.R.; Murgu, S.D.; Krimsky, W.S.; Murillo, B.A.; LeMense, G.P.; Minnich, D.J.; Bansal, S.; et al. Electromagnetic Navigation Bronchoscopy for Peripheral Pulmonary Lesions: One-Year Results of the Prospective, Multicenter NAVIGATE Study. J. Thorac. Oncol. 2019, 14, 445–458. [Google Scholar] [CrossRef] [PubMed]
- Folch, E.E.; Labarca, G.; Ospina-Delgado, D.; Kheir, F.; Majid, A.; Khandhar, S.J.; Mehta, H.J.; Jantz, M.A.; Fernandez-Bussy, S. Sensitivity and Safety of Electromagnetic Navigation Bronchoscopy for Lung Cancer Diagnosis: Systematic Review and Meta-analysis. Chest 2020, 158, 1753–1769. [Google Scholar] [CrossRef]
- McGuire, A.L.; Myers, R.; Grant, K.; Lam, S.; Yee, J. The Diagnostic Accuracy and Sensitivity for Malignancy of Radial-Endobronchial Ultrasound and Electromagnetic Navigation Bronchoscopy for Sampling of Peripheral Pulmonary Lesions: Systematic Review and Meta-analysis. J. Bronchol. Interv. Pulmonol. 2020, 27, 106–121. [Google Scholar] [CrossRef]
- Hohenforst-Schmidt, W.; Zarogoulidis, P.; Vogl, T.; Turner, J.F.; Browning, R.; Linsmeier, B.; Huang, H.; Li, Q.; Darwiche, K.; Freitag, L.; et al. Cone Beam Computer tomography (CBCT) in Interventional Chest Medicine—High Feasibility for Endobronchial Realtime Navigation. J. Cancer 2014, 5, 231–241. [Google Scholar] [CrossRef]
- Benn, B.S.; Romero, A.O.; Lum, M.; Krishna, G. Robotic-Assisted Navigation Bronchoscopy as a Paradigm Shift in Peripheral Lung Access. Lung 2021, 199, 177–186. [Google Scholar] [CrossRef]
- Ali, E.A.; Takizawa, H.; Kawakita, N.; Sawada, T.; Tsuboi, M.; Toba, H.; Takashima, M.; Matsumoto, D.; Yoshida, M.; Kawakami, Y.; et al. Transbronchial Biopsy Using an Ultrathin Bronchoscope Guided by Cone-Beam Computed Tomography and Virtual Bronchoscopic Navigation in the Diagnosis of Pulmonary Nodules. Respiration 2019, 98, 321–328. [Google Scholar] [CrossRef]
- Casal, R.F.; Sarkiss, M.; Jones, A.K.; Stewart, J.; Tam, A.; Grosu, H.B.; Ost, D.E.; Jimenez, C.A.; Eapen, G.A. Cone beam computed tomography-guided thin/ultrathin bronchoscopy for diagnosis of peripheral lung nodules: A prospective pilot study. J. Thorac. Dis. 2018, 10, 6950–6959. [Google Scholar] [CrossRef] [PubMed]
- Steinfort, D.P.; Khor, Y.H.; Manser, R.L.; Irving, L.B. Radial probe endobronchial ultrasound for the diagnosis of peripheral lung cancer: Systematic review and meta-analysis. Eur. Respir. J. 2011, 37, 902–910. [Google Scholar] [CrossRef] [PubMed]
- Kurimoto, N.; Miyazawa, T.; Okimasa, S.; Maeda, A.; Oiwa, H.; Miyazu, Y.; Murayama, M. Endobronchial ultrasonography using a guide sheath increases the ability to diagnose peripheral pulmonary lesions endoscopically. Chest 2004, 126, 959–965. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.S.; Sethi, J.; Taneja, A.; Musani, A.; Maldonado, F. Computed Tomography Bronchus Sign and the Diagnostic Yield of Guided Bronchoscopy for Peripheral Pulmonary Lesions. A Systematic Review and Meta-Analysis. Ann. Am. Thorac. Soc. 2018, 15, 978–987. [Google Scholar] [CrossRef] [PubMed]
- Bowling, M.R.; Kohan, M.W.; Walker, P.; Efird, J.; Ben Or, S. The effect of general anesthesia versus intravenous sedation on diagnostic yield and success in electromagnetic navigation bronchoscopy. J. Bronc. Interv. Pulmonol. 2015, 22, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Solano, J.R.; Ugalde-Gamboa, L.; Machuzak, M. Robotic Bronchoscopy for Diagnosis of Suspected Lung Cancer: A Feasibility Study. J. Bronc. Interv. Pulmonol. 2018, 25, 168–175. [Google Scholar] [CrossRef]
- Chaddha, U.; Kovacs, S.P.; Manley, C.; Hogarth, D.K.; Cumbo-Nacheli, G.; Bhavani, S.V.; Kumar, R.; Shende, M.; Egan, J.P.; Murgu, S. Robot-assisted bronchoscopy for pulmonary lesion diagnosis: Results from the initial multicenter experience. BMC Pulm. Med. 2019, 19, 243. [Google Scholar] [CrossRef]
- Galloway, K.C.; Chen, Y.; Templeton, E.; Rife, B.; Godage, I.S.; Barth, E.J. Fiber Optic Shape Sensing for Soft Robotics. Soft Robot. 2019, 6, 671–684. [Google Scholar] [CrossRef]
- Kalchiem-Dekel, O.; Connolly, J.G.; Lin, I.-H.; Husta, B.C.; Adusumilli, P.S.; Beattie, J.A.; Buonocore, D.J.; Dycoco, J.; Fuentes, P.; Jones, D.R.; et al. Shape-Sensing Robotic-Assisted Bronchoscopy in the Diagnosis of Pulmonary Parenchymal Lesions. Chest 2022, 161, 572–582. [Google Scholar] [CrossRef]
- Chan, J.W.Y.; Lau, R.W.H.; Ngai, J.C.L.; Tsoi, C.; Chu, C.M.; Mok, T.S.K.; Ng, C.S.H. Transbronchial microwave ablation of lung nodules with electromagnetic navigation bronchoscopy guidance—A novel technique and initial experience with 30 cases. Transl. Lung Cancer Res. 2021, 10, 1608–1622. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Mean (Range) |
|---|---|
| Age | 71 (62–84) |
| Race/Ethnicity | N (%) |
| White | 12 (86) |
| Black | 2 (14) |
| Sex | N (%) |
| Female | 6 (43) |
| Male | 8 (57) |
| Smoking Status | N (%) |
| Never | 5 (36) |
| Former or Current | 9 (64) |
| History of Cancer | N (%) |
| Previous cancer | 6 (43) |
| Size | (Mean ± SD) [Range], mm |
|---|---|
| Axial diameter | 21.7 ± 14.9 [9–62] |
| Coronal diameter | 13.2 ± 4.8 [6–46] |
| N (%) | |
| <2 cm in all dimensions | 10 (59) |
| >2 cm in any dimension | 7 (41) |
| Type | N (%) |
| Solid | 14 (82) |
| Mixed | 1 (6) |
| Ground glass | 2 (12) |
| Location | N (%) |
| Left Lower Lobe | 3 (18) |
| Left Upper Lobe | 3 (18) |
| Right Lower Lobe | 1 (6) |
| Right Middle Lobe | 2 (12) |
| Right Upper Lobe | 8 (47) |
| Bronchus Sign | N (%) |
| Present | 6 (35) |
| Absent | 11 (65) |
| REBUS | N (%) |
| Concentric | 4 (24) |
| Eccentric | 13 (76) |
| Biopsy Result | Pathology | N (%) |
|---|---|---|
| Malignancy | Squamous Cell Carcinoma | 4 (23) |
| Metastatic disease * | 3 (18) | |
| Adenocarcinoma | 2 (12) | |
| Small Cell Carcinoma | 1 (6) | |
| Inflammation | Chronic Inflammation | 1 (6) |
| Infectious | Non-tuberculous mycobacteria | 2 (12) |
| Non-diagnostic | 4 (23) |
| Nodule | Size (mm) | Presence of Bronchus Sign | REBUS View * | Biopsy Tool-Lesion Relationship ** | Diagnosis |
|---|---|---|---|---|---|
| 1 | 34 | Positive | Concentric | Within | Chronic Inflammation |
| 2 | 22 | Negative | Concentric | Within | Squamous Cell Lung Carcinoma |
| 3 | 9.7 | Negative | Eccentric | Adjacent | Mycobacterium avium Complex |
| 4 | 12.4 | Negative | Eccentric | Adjacent | Mycobacterium avium Complex |
| 5 | 24 | Negative | Concentric | Within | Lung Adenocarcinoma |
| 6 | 29 | Positive | Concentric | Within | Lung Adenocarcinoma |
| 7 | 15 | Negative | Eccentric | Within | Endometrial Adenocarcinoma |
| 8 | 11 | Negative | Eccentric | Adjacent | Endometrial Adenocarcinoma |
| 9 | 18 | Positive | Eccentric | None | Squamous Cell Lung Carcinoma |
| 10 | 50 | Positive | Eccentric | Adjacent | Squamous Cell Lung Carcinoma |
| 11 | 23 | Negative | Eccentric | Adjacent | Small Cell Carcinoma |
| 12 | 62 | Positive | Eccentric | Within | Non-diagnostic |
| 13 | 13 | Positive | Eccentric | Within | Non-diagnostic |
| 14 | 15 | Negative | None | None | Urothelial Carcinoma |
| 15 | 11 | Negative | None | Adjacent | Non-diagnostic |
| 16 | 11 | Negative | None | None | Non-diagnostic |
| 17 | 9 | Negative | Eccentric | Adjacent | Squamous Cell Lung Carcinoma |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Podder, S.; Chaudry, S.; Singh, H.; Jondall, E.M.; Kurman, J.S.; Benn, B.S. Efficacy and Safety of Cone-Beam CT Augmented Electromagnetic Navigation Guided Bronchoscopic Biopsies of Indeterminate Pulmonary Nodules. Tomography 2022, 8, 2049-2058. https://doi.org/10.3390/tomography8040172
Podder S, Chaudry S, Singh H, Jondall EM, Kurman JS, Benn BS. Efficacy and Safety of Cone-Beam CT Augmented Electromagnetic Navigation Guided Bronchoscopic Biopsies of Indeterminate Pulmonary Nodules. Tomography. 2022; 8(4):2049-2058. https://doi.org/10.3390/tomography8040172
Chicago/Turabian StylePodder, Shreya, Sana Chaudry, Harpreet Singh, Elise M. Jondall, Jonathan S. Kurman, and Bryan S. Benn. 2022. "Efficacy and Safety of Cone-Beam CT Augmented Electromagnetic Navigation Guided Bronchoscopic Biopsies of Indeterminate Pulmonary Nodules" Tomography 8, no. 4: 2049-2058. https://doi.org/10.3390/tomography8040172
APA StylePodder, S., Chaudry, S., Singh, H., Jondall, E. M., Kurman, J. S., & Benn, B. S. (2022). Efficacy and Safety of Cone-Beam CT Augmented Electromagnetic Navigation Guided Bronchoscopic Biopsies of Indeterminate Pulmonary Nodules. Tomography, 8(4), 2049-2058. https://doi.org/10.3390/tomography8040172







