Internal Jugular Central Venous Catheter Tip Migration: Patient and Procedural Factors
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Firstenberg, M.S.; Kornbau, C.; Lee, K.C.; Hughes, G.D. Central line complications. Int. J. Crit. Illn. Inj. Sci. 2015, 5, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Ullman, A.J.; Marsh, N.; Mihala, G.; Cooke, M.; Rickard, C.M. Complications of Central Venous Access Devices: A Systematic Review. Pediatrics 2015, 136, e1331–e1344. [Google Scholar] [CrossRef]
- McGee, D.C.; Gould, M.K. Preventing Complications of Central Venous Catheterization. N. Engl. J. Med. 2003, 348, 1123–1133. [Google Scholar] [CrossRef]
- Seelig, M.H.; Oldenburg, W.A.; Klingler, P.J.; Odell, J.A. Superior vena cava syndrome caused by chronic hemodialysis catheters: Autologous reconstruction with a pericardial tube graft. J. Vasc. Surg. 1998, 28, 556–560. [Google Scholar] [CrossRef]
- Herse, B.; Hannekum, A.; Hügel, W.; Dalichau, H. Superior vena cava occlusion. Demonstration of surgical therapeutic possibilities. Der Chir. 1986, 57, 565–572. [Google Scholar]
- Vesely, T.M. Central Venous Catheter Tip Position: A Continuing Controversy. J. Vasc. Interv. Radiol. 2003, 14, 527–534. [Google Scholar] [CrossRef]
- Song, Y.G.; Byun, J.H.; Hwang, S.Y.; Kim, C.W.; Shim, S.G. Use of vertebral body units to locate the cavoatrial junction for optimum central venous catheter tip positioning. Br. J. Anaesth. 2015, 115, 252–257. [Google Scholar] [CrossRef]
- Hade, A.D.; Beckmann, L.A.; Basappa, B.K. A checklist to improve the quality of central venous catheter tip positioning. Anaesthesia 2019, 74, 896–903. [Google Scholar] [CrossRef] [PubMed]
- Frykholm, P.; Pikwer, A.; Hammarskjöld, F.; Larsson, A.T.; Lindgren, S.; Lindwall, R.; Taxbro, K.; Öberg, F.; Acosta, S.; Åkeson, J. Clinical guidelines on central venous catheterisation. Acta Anaesthesiol. Scand. 2014, 58, 508–524. [Google Scholar] [CrossRef]
- Mandolfo, S.; Galli, F.; Costa, S.; Ravani, P.; Gaggia, P.; Imbasciati, E. Factors Influencing Permanent Catheter Performance. J. Vasc. Access 2001, 2, 106–109. [Google Scholar] [CrossRef]
- Schutz, J.C.L.; Patel, A.A.; Clark, T.W.I.; Solomon, J.A.; Freiman, D.B.; Tuite, C.M.; Mondschein, J.I.; Soulen, M.C.; Shlansky-Goldberg, R.D.; Stavropoulos, S.W.; et al. Relationship between Chest Port Catheter Tip Position and Port Malfunction after Interventional Radiologic Placement. J. Vasc. Interv. Radiol. 2004, 15, 581–587. [Google Scholar] [CrossRef]
- Xiang, D.Z.; Verbeken, E.K.; Van Lommel, A.T.L.; Stas, M.; De Wever, I. Composition and formation of the sleeve enveloping a central venous catheter. J. Vasc. Surg. 1998, 28, 260–271. [Google Scholar] [CrossRef]
- Caers, J.; Fontaine, C.; Vinh-Hung, V.; De Mey, J.; Ponnet, G.; Oost, C.; Lamote, J.; De Greve, J.; Van Camp, B.; Lacor, P. Catheter tip position as a risk factor for thrombosis associated with the use of subcutaneous infusion ports. Support. Care Cancer 2005, 13, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Tesselaar, M.E.T.; Ouwerkerk, J.; Nooy, M.A.; Rosendaal, F.R.; Osanto, S. Risk factors for catheter-related thrombosis in cancer patients. Eur. J. Cancer 2004, 40, 2253–2259. [Google Scholar] [CrossRef]
- Puel, V.; Caudry, M.; Le Métayer, P.; Baste, J.-C.; Midy, D.; Marsault, C.; Demeaux, H.; Maire, J.-P. Superior vena cava thrombosis related to catheter malposition in cancer chemotherapy given through implanted ports. Cancer 1993, 72, 2248–2252. [Google Scholar] [CrossRef]
- Seo, M.; Shin, W.-J.; Jun, I.-G. Central venous catheter-related superior vena cava syndrome following renal transplantation -A case report-. Korean J. Anesthesiol. 2012, 63, 550–554. [Google Scholar] [CrossRef]
- Frias, P.F.; Cross, C.G.; Kaufman, C.S.; Quencer, K.B. Port malposition in the azygos vein resulting in a veno-broncho and broncho-esophageal fistula: A case report. J. Vasc. Access 2021. [Google Scholar] [CrossRef]
- Gapp, J.; Krishnan, M.; Ratnaraj, F.; Schroell, R.P.; Moore, D. Cardiac Arrhythmias Resulting from a Peripherally Inserted Central Catheter: Two Cases and a Review of the Literature. Cureus 2017, 9, e1308. [Google Scholar] [CrossRef]
- Vaideeswar, P.; Chaudhari, J.; Karnik, N.; Sahu, T.; Gupta, A. Right atrial mural thrombi: An autopsy study of an under-diagnosed complication at an unusual site. J. Postgrad. Med. 2017, 63, 21. [Google Scholar] [CrossRef]
- Jahnke, C.; Hoxha, E.; Söffker, G.; Seiffert, M. Cardiac perforation due to delayed migration of a chronic dialysis catheter: A case report. Eur. Hear. J.-Case Rep. 2021, 5, ytab332. [Google Scholar] [CrossRef]
- Moureau, N. Impact and Safety Associated with Accidental Dislodgement of Vascular Access Devices: A Survey of Professions, Settings, and Devices. J. Assoc. Vasc. Access 2018, 23, 203–215. [Google Scholar] [CrossRef]
- Prabaharan, B.; Thomas, S. Spontaneous migration of central venous catheter tip following extubation. Saudi, J. Anaesth. 2014, 8, 131. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, C.M.; Kaufman, J.A.; Rivitz, S.M.; Geller, S.C.; Waltman, A.C. Migration of Central Venous Catheters: Implications for Initial Catheter Tip Positioning. J. Vasc. Interv. Radiol. 1997, 8, 443–447. [Google Scholar] [CrossRef]
- Nazarian, G.K.; Bjarnason, H.; Dietz, C.A.; Bernadas, C.A.; Hunter, D.W. Changes in Tunneled Catheter Tip Position when a Patient Is Upright. J. Vasc. Interv. Radiol. 1997, 8, 437–441. [Google Scholar] [CrossRef]
- Fry, A.C.; Stratton, J.; Farrington, K.; Mahna, K.; Selvakumar, S.; Thompson, H.; Warwicker, P. Factors affecting long-term survival of tunnelled haemodialysis catheters a prospective audit of 812 tunnelled catheters. Nephrol. Dial. Transplant. 2008, 23, 275–281. [Google Scholar] [CrossRef]
- Karam, J.L.; Haddad, F.F.; Medawar, W.; Daouk, M.; Khalil, I. Tunneled dialysis catheter tip migration in obese and large-breasted individuals. Kidney Int. 2009, 75, 760. [Google Scholar] [CrossRef] [PubMed]
- Bream, P.R., Jr. Update on Insertion and Complications of Central Venous Catheters for Hemodialysis. Semin. Intervent. Radiol. 2016, 33, 031–038. [Google Scholar] [CrossRef]
- Gibson, F.; Bodenham, A. Misplaced central venous catheters: Applied anatomy and practical management. Br. J. Anaesth. 2013, 110, 333–346. [Google Scholar] [CrossRef]
- Kim, M.-C.; Kim, K.-S.; Choi, Y.-K.; Kim, D.-S.; Kwon, M.-I.; Sung, J.-K.; Moon, J.-Y.; Kang, J.-M. An Estimation of Right- and Left-Sided Central Venous Catheter Insertion Depth Using Measurement of Surface Landmarks Along the Course of Central Veins. Anesthesia Analg. 2011, 112, 1371–1374. [Google Scholar] [CrossRef] [PubMed]
- Salik, E.; Daftary, A.; Tal, M.G. Three-dimensional Anatomy of the Left Central Veins: Implications for Dialysis Catheter Placement. J. Vasc. Interv. Radiol. 2007, 18, 361–364. [Google Scholar] [CrossRef]
- Zdrahala, R.J.; Spielvogel, D.E.; Strand, M.A. Softening of Thermoplastic Polyurethanes: A Structure/Property Study. J. Biomater. Appl. 1987, 2, 544–561. [Google Scholar] [CrossRef] [PubMed]
- Quaretti, P.; Galli, F.; Moramarco, L.P.; Corti, R.; Leati, G.; Fiorina, I.; Maestri, M. Dialysis Catheter-Related Superior Vena Cava Syndrome with Patent Vena Cava: Long Term Efficacy of Unilateral Viatorr Stent-Graft Avoiding Catheter Manipulation. Korean J. Radiol. 2014, 15, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Dağdelen, S. Superior vena cava syndrome arising from subclavian vein port catheter implantation and paraneoplastic syndrome. Turk Kardiyol. Dernegi Arsivi-Archives Turk. Soc. Cardiol. 2009, 37, 125–127. [Google Scholar]
- Shaikh, I.; Berg, K.; Kman, N. Thrombogenic Catheter-Associated Superior Vena Cava Syndrome. Case Rep. Emerg. Med. 2013, 2013, 793054. [Google Scholar] [CrossRef] [PubMed]
| Gender | 101 Female (57%) | 76 Male (43%) | ||
| Laterality | 127 R (72%) | 50 L (28%) | ||
| Catheter type | 122 Ports (69%) | 50 lbTCVC (28%) | 5 sbTCVC (3%) | |
| Left Sided CVC (n = 50) | Right Sided CVC (n = 127) | Statistical Analysis | |
|---|---|---|---|
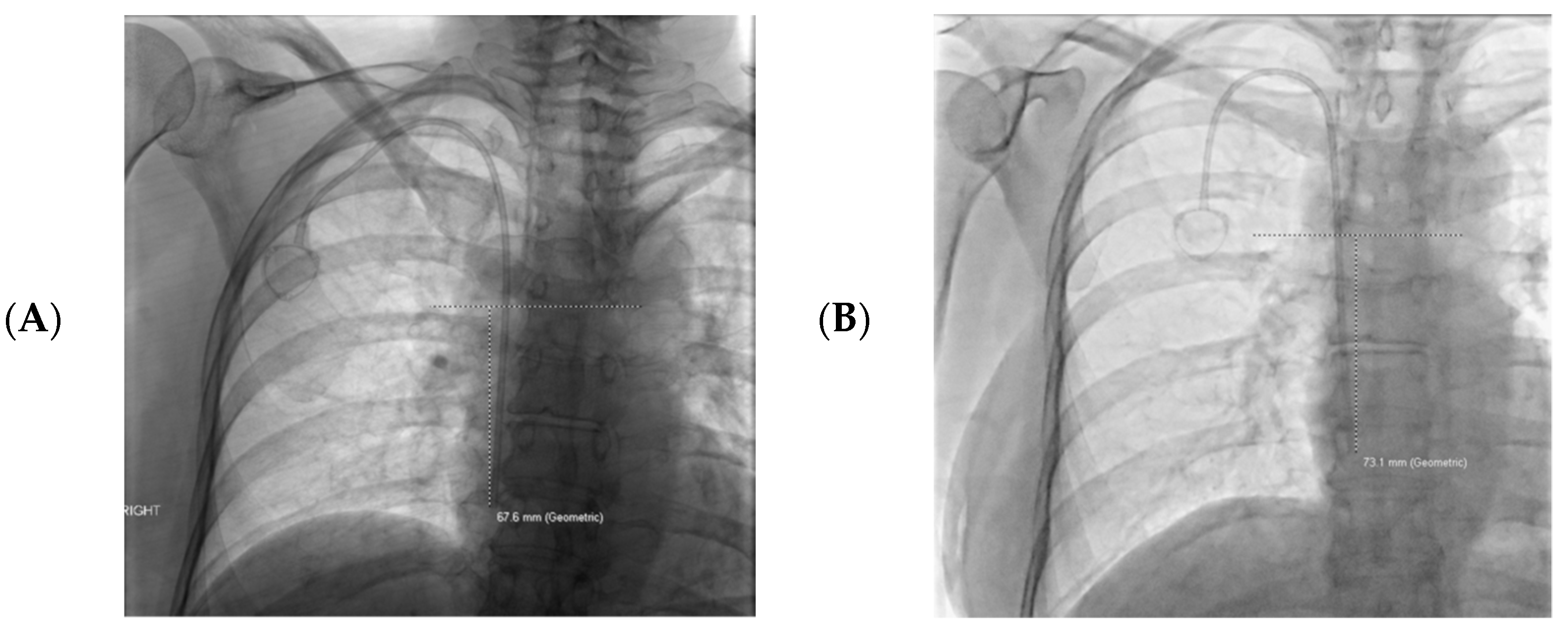
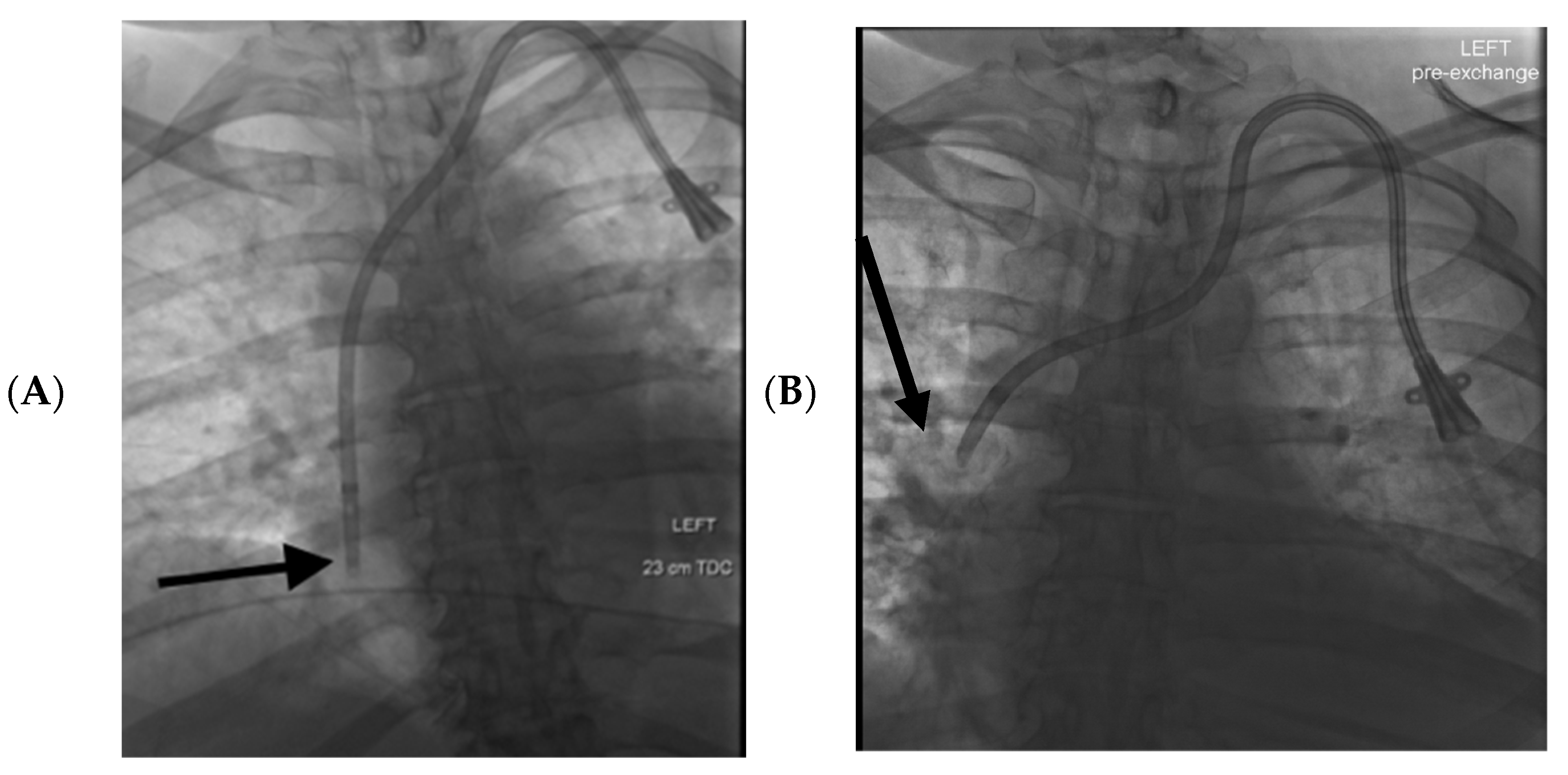
| Mean catheter tip migration | 3.2 cm cranially | 0.8 cm cranially | p = 0.000008 * |
| Catheter Dysfunction | 16 (32%) | 6 (4.7%) | Odds ratio for CVC dysfunction and >2 cm cranial tip migration: Odds ratio: 7.2 95% confidence interval 2.6–19.6 p = 0.0001 |
| >2 cm catheter tip cranial migration | 32 (64%) | 26 (20.5%) | Odds ratio for >2 cm of cranial catheter tip migration in left vs. right CVCs Odds ratio: 6.9 95% confidence interval 3.4–14.2 p < 0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smith, T.; Kaufman, C.; Quencer, K. Internal Jugular Central Venous Catheter Tip Migration: Patient and Procedural Factors. Tomography 2022, 8, 1033-1040. https://doi.org/10.3390/tomography8020083
Smith T, Kaufman C, Quencer K. Internal Jugular Central Venous Catheter Tip Migration: Patient and Procedural Factors. Tomography. 2022; 8(2):1033-1040. https://doi.org/10.3390/tomography8020083
Chicago/Turabian StyleSmith, Tyler, Claire Kaufman, and Keith Quencer. 2022. "Internal Jugular Central Venous Catheter Tip Migration: Patient and Procedural Factors" Tomography 8, no. 2: 1033-1040. https://doi.org/10.3390/tomography8020083
APA StyleSmith, T., Kaufman, C., & Quencer, K. (2022). Internal Jugular Central Venous Catheter Tip Migration: Patient and Procedural Factors. Tomography, 8(2), 1033-1040. https://doi.org/10.3390/tomography8020083






