1. Introduction
Femoroacetabular impingement (FAI) was first described in a publication by Reinhold Ganz [
1], a Swiss orthopedic surgeon, who proposed that certain anatomical variations between the femur and the acetabulum led to abnormal contact, causing early osteoarthritis of the hip. It is possible to define femoroacetabular impingement as a set of signs and symptoms derived from anatomical abnormalities of the femoral head and/or acetabulum that cause abnormal friction between them and which manifests during hip movement—either in flexion or rotation of the hip—which leads to structural damage to the acetabular labrum and articular cartilage [
2,
3].
The overall prevalence of FAI syndrome is highly variable, as it has been estimated using a wide range of methodologies and in diverse populations, being observed in 3 to 57% of the samples studied, with a discordance according to region, population, and physical activities, while the local prevalence is unknown [
4,
5]. This is because the methods for assessing and validating prevalence are often missing or only roughly explained. Epidemiological differences in prevalence could undoubtedly indirectly manifest in the anatomical particularities of a specific ethnic group, given that the human species has great phenotypic variation, with intragroup and intergroup patterns according to their ethnic origins, as reflected by anthropometric variables [
6].
Given its etiology, FAI can be classified into cam-, pincer-, and mixed-type, depending on the site of anatomical variation. The cam-type is more prevalent in individuals who perform a variety of high-performance sports activities, where the lesion is generated by a repetitive axial load, causing bone overgrowth at the junction of the head with the femoral neck; determination of this type typically requires radiological assessment [
6,
7].
Pincer-type FAI is commonly characterized by acetabular over-coverage, resulting in compression of the labrum and articular cartilage between the femoral neck and the acetabular border, typically seen in hips that present with deep coxa or acetabular retroversion [
8]. The angle of the acetabular version is measured using axial imaging [
9,
10]; similarly, marginal acetabular bone growths can be observed due to continuous microtrauma and labral degeneration, with later bone metaplasia, which generates over-coverage and is part of the diagnostic findings [
11,
12,
13]. In a high percentage of patients, a mixed pattern, including concomitant cam- and pincer-type morphological changes, is observed.
The population of contemporary Mayan and mestizo descent in Yucatan has been widely characterized as having a shorter stature compared to other American ethnic groups. Although this aspect could be considered as an anatomical peculiarity, it could also be associated clinically and radiographically with the presence, degree, and manifestations of FAI as, in the human body, there are anatomical associations among the different segments, proportional and net circles, diameters, and lengths. In particular, the associations between length or stature and shoulder girdle dimensions by segments and totals have been studied, and it has been found that these associations may be of epidemiological importance [
14].
In the contemporary Yucatecan population—both Mayan and mestizo—the authors have described a high prevalence of short and very short stature in the Yucatecan men and women. Furthermore, the body mass index status in the ranges of overweight and obesity is particularly high among the population of Yucatan, with a combined overweight and obesity prevalence of 82.6% for both sexes reported in 2022 [
15,
16,
17]. The degree of overweight/obesity was higher among individuals with a short height [
18], as observed in a sample comprising 1424 participants. Although the literature has suggested that there could be an association among anthropometric measurements, radiological measurements, and pincer-type femoroacetabular impingement, the importance and meaning of this possible association is unknown [
6]; however, it seems reasonable to consider that, given these phenotypic differences characterizing the Mayan and mestizo population of Yucatan, the prevalence and presentation of FAI may also differ from those of reference human groups. The objective of the present study was to describe the femoroacetabular impingement morphological changes prevalence in a sample of patients from a population with short height, as well as evaluate the reliability of angle measurements for the prediction of FAI.
2. Participants and Methods
The inclusion criteria considered patients of both sexes, aged ≥30 years old, who were scheduled for abdominopelvic tomography at the outpatient clinic of the Regional High Specialty Hospital of the Yucatan Peninsula (HRAEPY). Patients were referred from an ambulatory consultation with the medical doctor in charge, with suspected compressive symptoms accompanying pain in one or both hips but had not received a diagnosis of femoroacetabular impingement. Those with imaging findings suggesting a tumor causing femoroacetabular impingement, amputees, or with standing disabilities were excluded. The elimination criteria further included incapability for full visualization of the femoroacetabular joint in tomography. The sample size calculation was obtained using the sample calculation formula for comparison of two proportions:
where Zα
2/2 is the critical value of the normal distribution in α/2 (95% confidence level, with α of 0.05/2 and critical value of 3.84), Zβ is the critical value of the normal distribution in β (for a power of 80%, the value of β is 0.2 and the critical value is 0.85), P1 is the sample proportion of the first group (patients with FAI findings), and P2 is the sample proportion of the second group (patients without FAI findings). The proposed sample size was 49 participants per group, for a total of 98 [
19,
20,
21].
The main outcome variable was the presence of FAI (dichotomous), along with the type of FAI (cam or pincer). Version, excrescence, calcification, and osteoarthritis were also considered as dependent variables in logistic regression; while the exposure variables were sex (binary) and body mass index and stature as of numeric continuous type.
The tomographic studies were reviewed by two radiologists with training in musculoskeletal imaging between August and October of 2021. Prior to the collection of images, informed consent was obtained, and patients who agreed to participate in the study were asked to complete a sociodemographic data form. Furthermore, anthropometric measurements were obtained using previously described methods—with respect to the Frankfort line as described by Lohman, Roche, and Martorell (1991) [
22]—while patients were barefoot, using a portable stadiometer (Seca© 206 (Vogel & Halke, Hamburg, Germany)) and recording the measurements to the nearest millimeter. Weight was measured with a digital scale to the nearest 100 g.
The FAI diagnosis was made through a detailed physical examination, in which the pain was reproduced using two different tests, which simulate the triggering movements, namely, the FADDIR and FABER tests (flexion–adduction/abduction–internal rotation/external rotation). In the first test, flexion was performed in the affected joint at 90°, with adduction and internal rotation; in the second test, flexion was carried out at 90°, with subsequent abduction and external rotation. These tests have a sensitivity of 78% and 60%, respectively, and a specificity of only 10% and 18% prior to tomographic assessment.
Tomographic images were taken using 128 multi-slice CT scanner (Revolution Evo, GE Healthcare, Waukesha, WI, USA) with 64 sections of 1.25 mm thickness, with the patient in a supine position and both lower limbs in parallel. The obtained images were analyzed using AW VolumeShare7 software, performing multiplanar reconstructions and volume rendering, which allowed for the measurement of C-sign, Alpha, Wiberg, and acetabular angles, thus determining morphological changes consistent with FAI and determining its subtypes. Laterality was considered a nominal variable with three possible values: right, left, or both (for cases of left plus right). The radiologists evaluating CT had expertise with MSK, with R.C.D. having five and A.M.B. having eight years of experience.
2.1. Statistical Analysis
With respect to the statistical analysis, an anonymized worksheet was used with unique codes for each participant, which was further exported and processed using Stata for Windows version 12 (Stata Corp., Texas College, TX, USA).
Descriptive statistics include frequencies, percentages, and proportions of the general sample and by group. The tables present the means for numerical data and standard deviations as a measure of dispersion with respect to the numerical and categorical variables. For the hypothesis contrast tests, a single-tailed comparison was used; meanwhile, for comparisons between groups (no FAI vs. FAI; no FAI vs. pincer and cam), ANOVA tests were performed.
For the association analysis, logistic regression was performed; models were selected using maximum likelihood closer to 0 and variance explained by pseudo r2 values closer to 1 in the range of 0–1. For the analysis, the chosen measure of association was the odds ratio, and the dependent variable was the presence of labral calcification and version, while the independent variables were the presence of left pincer, left cam, right pincer, and right cam. In the regression analysis, odds for ipsilateral labral calcification and version were assessed.
Early osteoarthrosis findings were also included. Finally, a post hoc test was performed, with values above
p > 0.05 being considered acceptable in the Hosmer–Lemeshow goodness-of-fit test [
23], for which a value of
p > 0.05 was taken as indicating a good fit in the regression models.
Inter-observer agreement was assessed using a kappa test based on the type of FAI. The observed agreement was contrasted against the expected agreement, and significant differences were established when
p < 0.05; if the observed agreement significantly exceeded the expected agreement, this indicates a better concordance. Finally, the agreement was interpreted as proposed by Landis and Koch, as follows: (a) below 0.0 = Poor; (b) 0.00–0.20 = Slight; (c) 0.21–0.40 = Fair; (d) 0.41–0.60 = Moderate; (e) 0.61–0.80 = Substantial; and (f) 0.81–1.00 = Almost perfect [
24].
Receiver operating characteristic (ROC) analyses were performed to assess the area under the curve, and predictor variables were plotted to test the equality of more than two ROC areas, where the explained variables were the type and laterality of FAI and the predictor variables were ipsilateral version and excrescence, along with Alpha and Wiberg angles. The predictive values at cutoff points, including sensitivity and specificity, are presented in the
Supplementary Materials.
2.2. Ethical Approval
The study was submitted and approved on 4 February 2021, and was carried out in accordance with the Federal Law on the Protection of Personal Data and the Declaration of Helsinki. The Institutional Review Board and Ethics Committee of the Regional High Specialty Hospital of the Yucatan Peninsula approved the protocol in March 2021, with the authorization number 2020-012. Consent was obtained from all the patients prior to participation.
3. Results
A total of 98 patients were included, of which 63% were women. The mean general age was 50.8 years. Regarding the sociodemographic characteristics, 80.61% (
n = 79) of patients were living in the state of Yucatán, while the remaining patients resided elsewhere in the Yucatan peninsula. They all reported being born in the Yucatan, 55.78% (
n = 55) had at least one Mayan surname, 47.36% (
n = 46) spoke both Spanish and Mayan, and 50.52% (
n = 49) only spoke Spanish. The sociodemographic, anthropometric, and tomographic characteristics of the patient population are detailed in
Table 1.
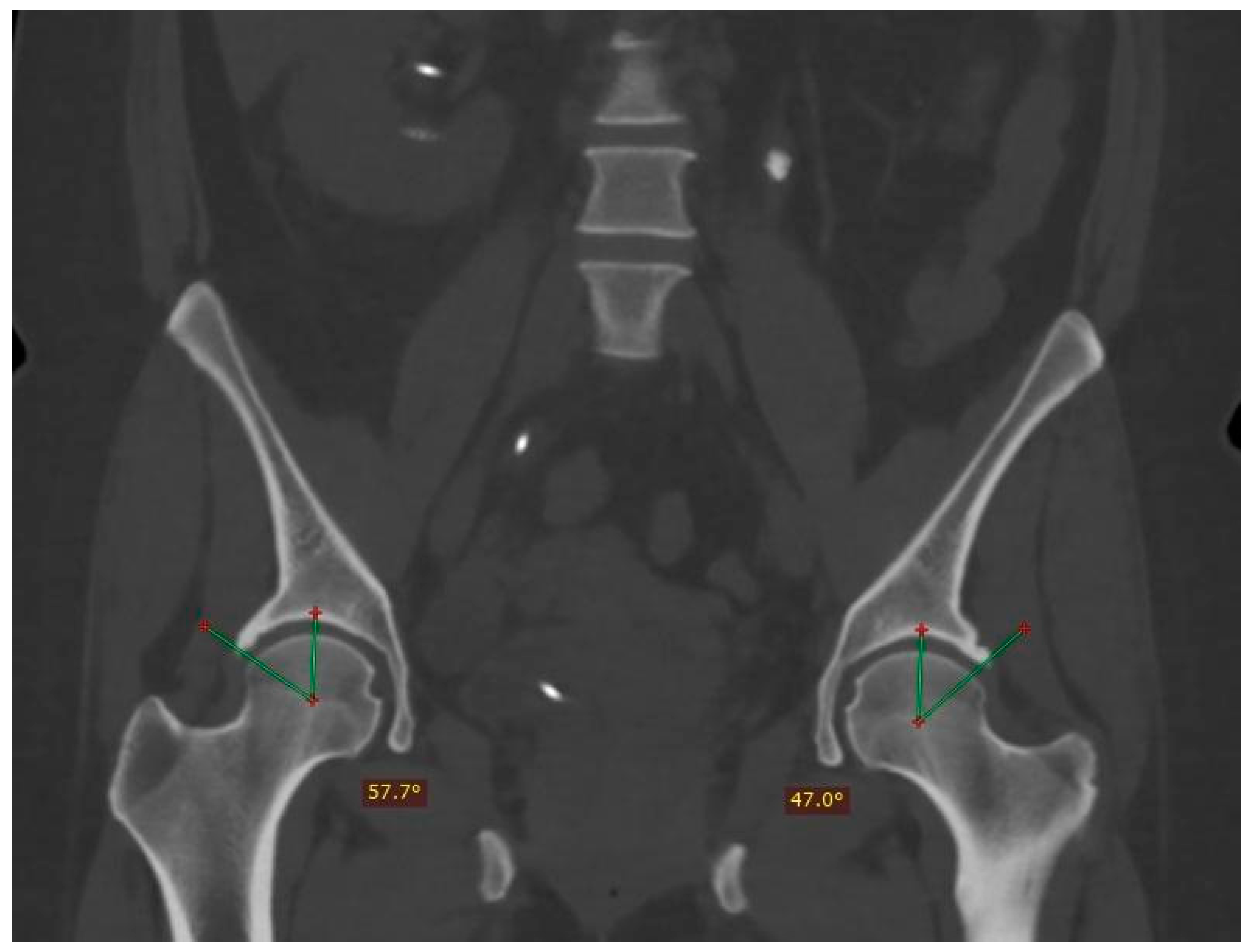
The anthropometric data revealed a general average height of 1.53 m and weight of 68.26 kg (SD ± 14.3). With respect to BMI, the mean was 29 (SD ± 14.3). Of the total patients, 47% presented morphological changes in femoroacetabular impingement, of which 37 correspond to the pincer-type, 17 to the cam-type, and 7 to the mixed-type (an example of mixed-type is shown in
Figure 1).
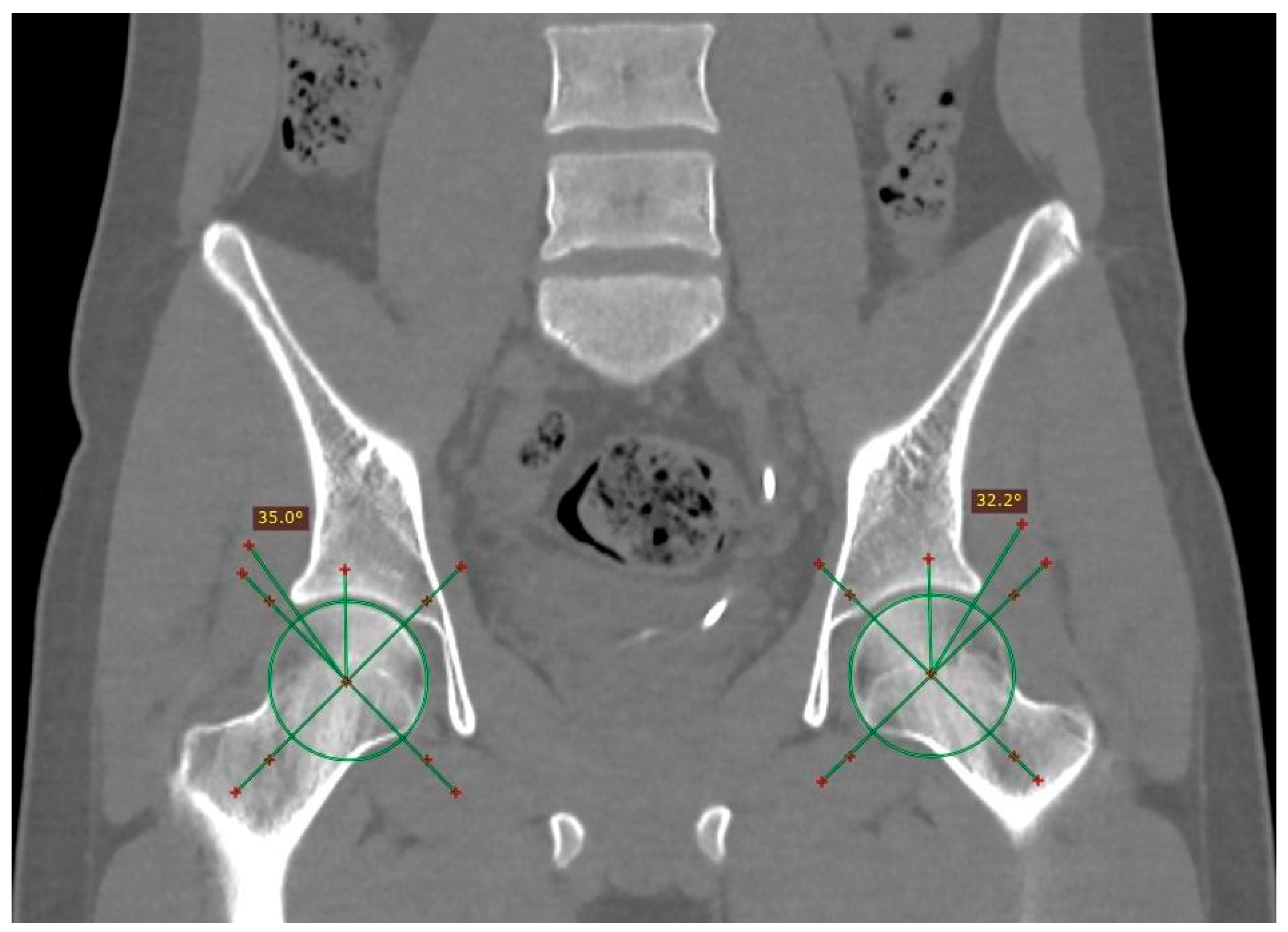
The distribution of pincer impingement with respect to laterality was 5.5% on the right side, 16.6% on the left side; while CAM impingement was present in 20% on the left side, 47% on the right, and 33% bilaterally (an example of bilateral FAI is shown in
Figure 2).
The cam-type was more prevalent among men, with this type also more commonly occurring among taller individuals, compared with those patients without FAI and those with pincer-type only. Clinical manifestations were significantly more common in patients with cam-type FAI type, while right and left Alpha angles differed between cam-type patients and others.
Wiberg angles had higher amplitude among patients with pincer-type FAI when compared to the overall sample, and labral calcification was also more common among patients with pincer-type FAI. Excrescence (either right or left) and osteoarthritis signs were less prevalent among patients without FAI, when compared to patients with either type of FAI.
Regarding the acetabular version by gender, the right acetabular version in men was 21.085° and, in the left, 20.341°; for women, the right version presented an average of 23.696° and, in the left version, 23.308°.
Patients who had compressive symptoms more often presented with C-sign, mixed impingement with 16.66% differences in Wiberg’s angle in patients with and without C-sign; furthermore, the average of the angles was greater in patients with C-sign, with a difference of 0.8112 degrees in the right angle and an even more pronounced difference between the averages of the left angle, at 2.7715 degrees (measurement of the Wiberg angle is depicted in
Figure 3).
The Kolmogorov–Smirnoff test confirmed the normal distribution of data (
p = 0.084). Regarding the interpretation of the mean comparison test, the
p-values of the variables right Wiberg angle, left Wiberg angle, right excrescence, left excrescence, pincer, and cam suggested significant differences in the frequency of pincer-type FAI among the height groups (
Table 1), where the compressing type with alpha angle was more common than non-compressing (
Figure 4 depicts the measurement of the Alpha angle).
In the logistic regression results, pincer-type was significantly associated with excrescence but not version; meanwhile, cam-type was not associated with version or excrescence, as detailed in
Table 2. The osteoarthritis and labral calcification goodness-of-fit indicated that associations with either pincer- or cam-type FAI were not reliable, as the post hoc test showed
p < 0.05. Consequently, these variables were omitted.
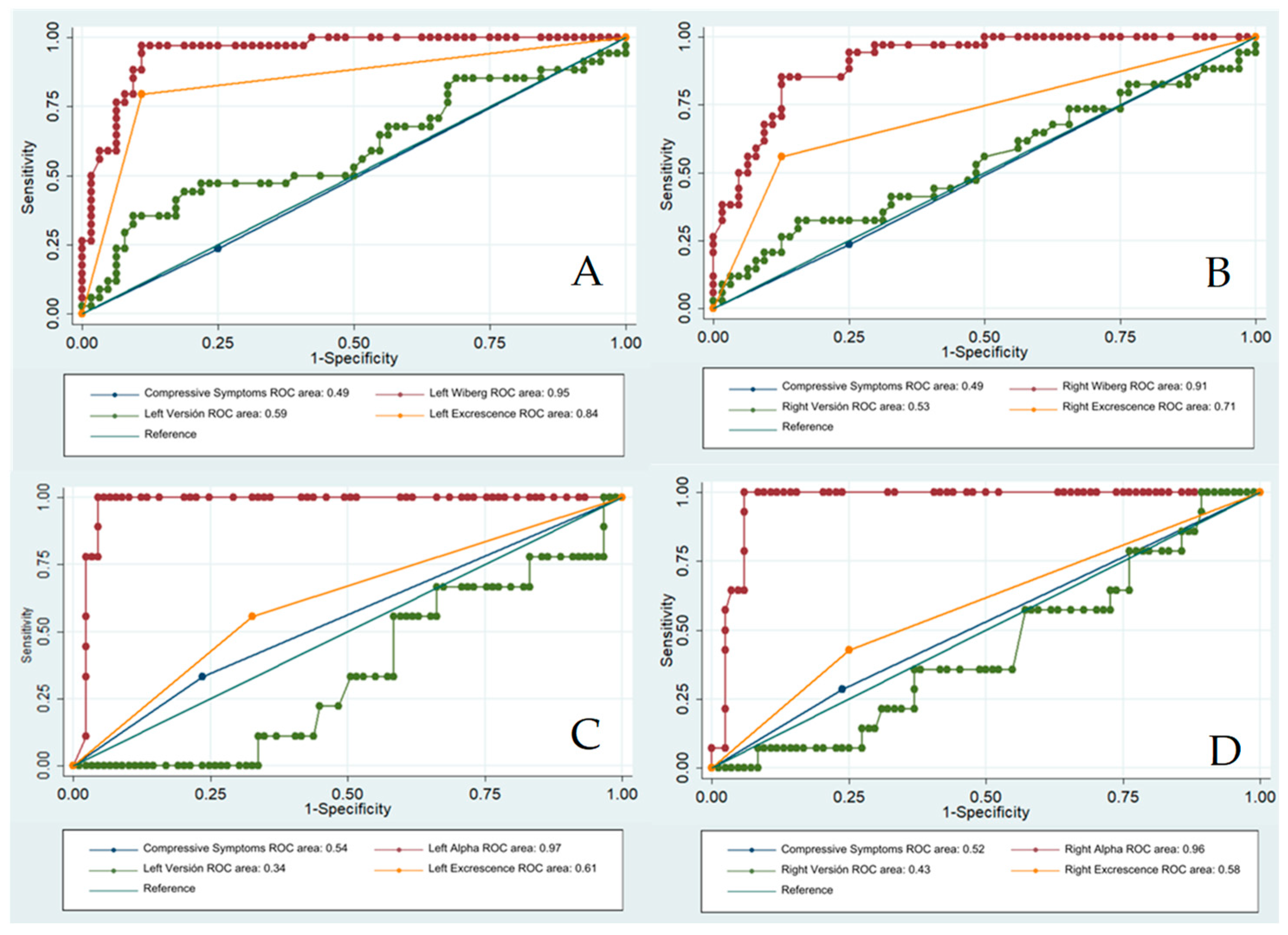
Regarding the receiver operating characteristic (ROC) analyses, Wiberg predicted the presence of the left pincer type with an area under the curve (AUC) of 0.95 ± 0.02 and, on the right side, Wiberg obtained an AUC of 0.96 ± 0.02. The Alpha angle obtained an AUC of 0.97 ± 0.01 for predicting left cam and an AUC of 0.96 ± 0.02 for right cam FAI, as shown in
Figure 5. Furthermore, considering version and excrescence AUCs in independent analyses, it was found that excrescence, but not version, may predict ipsilateral pincer-type FAI.
The inter-rater agreement determined using the kappa test showed an average of 0.81, which can be classified as almost perfect. For both types of FAI, the observed agreement significantly exceeded the expected agreement. Nevertheless, pincer-type FAI exhibited greater agreement, as expressed with respect to the observed agreement and kappa variables shown in
Table 3.
4. Discussion
We studied the prevalence of FAI in a sample of the Mayan–Mestizo population in southern Mexico. The findings revealed that the study population had a shorter stature compared to participants in the other earlier studies [
6]. However, no significant association between height and the presence of femoroacetabular impingement was observed; it was only observed that cam-type FAI was more common among individuals with higher stature. Nevertheless, we may also consider this finding with caution, as the cam type is more prevalent in men, and the men in the studied sample were taller than the women on average.
The overall prevalence of morphological changes that predispose individuals to femoroacetabular impingement in the analyzed population varied in relation to that reported in the literature, compared to the work of Zhou et al. [
25]. There are also studies reporting a 37% prevalence in asymptomatic athletes. The most recent studies on FAI frequency have been conducted in athlete populations, compared to any other population; as such, studies such as ours conducted in unsuspected and undiagnosed populations are less common. It has been reported that FAI is more common in the Western world when compared to Eastern regions, but detailed references are not very common for non-athlete and undiagnosed populations, and there is a chance that patients from Eastern regions are as affected but remain undiagnosed [
26,
27]. Although assessing FAI in athletes is critical for their performance, it may be time to start helping patients with different health conditions to be diagnosed and treated, as their quality of life can be improved. With this statement, we do not imply that all patients with morphological changes consistent with FAI should be considered for surgical intervention, as it pertains to the clinician to assess the patients as a whole, considering the symptoms but also their risks, their lifestyle, and most of all, respecting their autonomy by accompanying their patients in a decision-making process. FAI may present intermittently and may be confused with other symptoms in patients with concomitant conditions causing pain, with or without compressive symptoms.
Estimating the prevalence of FAI in an open population using CT is difficult due to the ethical constraints of exposing healthy individuals to ionizing radiation; for this reason, the studies on patients undergoing CT for different reasons are used in the clinical context for estimating the prevalence of FAI, as was recently the case for the study of Bartlett et al., who observed an increased prevalence in patients with acetabular fractures [
28]. Furthermore, there exist limitations regarding the use of MRI in an open population, particularly related to the associated costs.
With our study, we hope to raise awareness among health professionals for the consideration of FAI as a concomitant or overlapping cause of pain in their patients as, once a patient is already scheduled for an abdominal CT, it only takes a few more minutes to assess their angle measurements. If diagnosed using CT, further studies may be added, such as MRI.
High-field and high-resolution imaging techniques—particularly 3-Tesla magnetic resonance imaging (3-T MRI)—may be considered the gold standard for FAI diagnosis. We consider that, in patients who are suspected of or diagnosed with FAI, MRI may be the best technique for initial diagnosis and follow-up after interventions or over time. Advancements in high-resolution magnetic resonance imaging (MRI) systems, particularly those with a resolution up to 35 μm, have proven to ensure accuracy in hip assessment and more comfort for patients because no intra-articular injection of contrast media is needed [
29]. As the costs for MRI are high for the under-resourced population, CT can be considered as a more affordable option with acceptable sensitivity and specificity, as observed in our study.
We found the proportion of patients with pincer morphology to be higher compared to the figures reported by other centers in the country [
6,
10]. Meanwhile, the proportion with cam morphology was lower. This finding is consistent with the findings of Albers et al. [
8], who observed a higher frequency of anterior femoroacetabular impingement in their case series, a finding that could correspond to the study population, as the cam morphology has been more commonly observed in young subjects who perform high-impact physical activities. The higher proportion of cam-type clamping in men is consistent with the results of the systematic review conducted by Mascarenhas et al. [
30].
Our comparisons of acetabular anteversion between men and women—both on the right and left sides—yielded findings similar to those of Ruvalcaba et al. [
10] in the Mexican adult population. Gutiérrez-Ramos et al. [
6] analyzed the differences in FAI between men and women in a hospital in Mexico City. Their results differed from those reported in the present work, as they identified a higher prevalence of cam-type impingement in men on the right hip; in contrast, in this study, it was the second most prevalent type. Furthermore, the pincer-type predominated in women on the left side in their study, while, in this study, bilateral pincer was the most common FAI.
The prevalence in the present study remains higher than the reported for an adult population from Japan and middle-aged white adults from Canada [
31,
32].
This study had limitations inherent to risk and cost minimizations. As tomographic studies involve exposure to radiation, the sample size may be considered to be small. The prevalence obtained does not represent the general population in the region, and thus, the generalizability of the results is limited, and they should be considered with caution. Additionally, not all variables that could predispose individuals to FAI were assessed here; for example, occupation, physical activity, and other related characteristics were not assessed. It would be advisable, in future studies, to collect information on the physical activity, occupation, and dietary habits of patients. Our approach to the condition was only conducted from the perspective of diagnostic imaging, enabling a better understanding of clinical context and multidisciplinary related aspects. Long-term follow-up and serial clinical assessments would be useful in order to characterize aspects related to progression.
5. Conclusions
In the patient population of Yucatan, Mexico, attending ambulatory consultation unrelated to femoroacetabular impingement, an overall morphological change prevalence of 47% was observed. Angle measurements using tomographic techniques can be used to predict cam- and pincer-type FAI. The average stature was shorter than that observed for patients with cam-type FAI, while the body mass index did not vary among groups. Angle measurement of tomographic images—even when CT is performed for reasons unrelated to femoroacetabular impingement symptoms—can provide reliable diagnoses in symptomatic or symptomatic undiagnosed patients, improving their chances of receiving specific treatment.
Author Contributions
R.C.-D. proposed the topic and methods, wrote the first manuscript, developed a literature review, developed the sub-dataset, and conducted data transformation. N.M.-D. designed the methods and statistical analysis, supervised the data collection, and revised and amended the first proposal draft; M.R.-P. and A.F.-R. provided insightful comments and contributed to the theoretical framework. All authors have read and agreed to the published version of the manuscript.
Funding
The present study was financed by Servicios de Salud para el Bienestar IMSS-BIENESTAR.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved on 4 December 2021 by the Ethics Committee of the Regional High Specialty Hospital of the Yucatan Peninsula (HRAEPY) under ethical approval number 2020-012.
Informed Consent Statement
Informed consent was obtained from all participants.
Data Availability Statement
Databases can be found at the ResearchGate profiles of the first and corresponding authors.
Acknowledgments
The present study was developed at Hospital Regional de Alta Especialidad de la Peninsula de Yucatan, financed by Instituto de Mexicano del Seguro Social para el Bienestar IMSS-BIENESTAR, in collaboration with the academic institutions represented by the authors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ganz, R.; Parvizi, J.; Beck, M.; Leunig, M.; Nötzli, H.; Siebenrock, K.A. Femoroacetabular Impingement. Clin. Orthop. Relat. Res. 2003, 417, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Assassi, S.; Weisman, M.H.; Lee, M.; Savage, L.; Diekman, L.; Graham, T.A.; Rahbar, M.H.; Schall, J.I.; Gensler, L.S.; Deodhar, A.A.; et al. New Population-Based Reference Values for Spinal Mobility Measures Based on the 2009–2010 National Health and Nutrition Examination Survey. Arthritis Rheumatol. 2014, 66, 2628–2637. [Google Scholar] [CrossRef] [PubMed]
- Rade, M.; Könönen, M.; Marttila, J.; Vanninen, R.; Shacklock, M.; Kankaanpää, M.; Airaksinen, O. Correlation analysis of demographic and anthropometric factors, hip flexion angle and conus medullaris displacement with unilateral and bilateral straight leg raise. Eur. Spine J. 2016, 25, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Mascarenhas, V.V.; Rego, P.; Dantas, P.; Morais, F.; McWilliams, J.; Collado, D.; Marques, H.; Gaspar, A.; Soldado, F.; Consciência, J.G. Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: A systematic review. Eur. J. Radiol. 2016, 85, 73–95. [Google Scholar] [CrossRef] [PubMed]
- Röling, M.A.; Mathijssen, N.M.; Bloem, R.M. Incidence of symptomatic femoroacetabular impingement in the general population: A prospective registration study. J. Hip Preserv. Surg. 2016, 3, 203–207. [Google Scholar] [CrossRef]
- Gutiérrez-Ramos, R.; Ávalos-Calderón, S.A.; Bahena-Peniche, L.A. Prevalence of X-ray signs of femoroacetabular impingement in Mexican population. Acta Ortop. Mex. 2017, 31, 134–140. [Google Scholar]
- Rhee, C.; Le Francois, T.; Byrd, J.W.T.; Glazebrook, M.; Wong, I. Radiographic Diagnosis of Pincer-Type Femoroacetabular Impingement: A Systematic Review. Orthop. J. Sports Med. 2017, 5, 2325967117708307. [Google Scholar] [CrossRef]
- Albers, C.E.; Wambeek, N.; Hanke, M.S.; Schmaranzer, F.; Prosser, G.H.; Yates, P.J. Imaging of femoroacetabular impingement-current concepts. J. Hip Preserv. Surg. 2016, 3, 245–261. [Google Scholar] [CrossRef]
- Barrientos, C.; Díaz, J.; Barahona, M.; Brañes, J.; Chaparro, F.; Salazar, A.; Rañilao, I.; Hinzpeter, J.; Ramírez, N. Relación entre el signo de Entrecruzamiento y el ángulo de versión acetabular en tomografía axial computada. Rev. Chil. Radiol. 2015, 21, 5–9. [Google Scholar] [CrossRef]
- Rubalcava, J.; Gómez-García, F.; Ríos-Reina, J.L. Acetabular anteversion angle of the hip in the Mexican adult population measured with computed tomography. Acta Ortop. Mex. 2012, 26, 155–161. [Google Scholar]
- Li, A.E.; Jawetz, S.T.; Greditzer, H.G.; Burge, A.J.; Nawabi, D.H.; Potter, H.G. MRI for the preoperative evaluation of femoroacetabular impingement. Insights Imaging 2016, 7, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Egger, A.C.; Frangiamore, S.; Rosneck, J. Femoroacetabular Impingement: A Review. Sports Med. Arthrosc. Rev. 2016, 24, e53–e58. [Google Scholar] [CrossRef] [PubMed]
- Frank, J.M.; Harris, J.D.; Erickson, B.J.; Slikker, W.; Bush-Joseph, C.A.; Salata, M.J.; Nho, S.J. Prevalence of Femoroacetabular Impingement Imaging Findings in Asymptomatic Volunteers: A Systematic Review. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 1199–1204. [Google Scholar] [CrossRef] [PubMed]
- Owusu, W.; Willett, W.; Ascherio, A.; Spiegelman, D.; Rimm, E.; Feskanich, D.; Colditz, G. Body Anthropometry and the Risk of Hip and Wrist Fractures in Men: Results from a Prospective Study. Obes. Res. 1998, 6, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Leatherman, T.L.; Goodman, A.H.; Stillman, T. Changes in stature, weight, and nutritional status with tourism-based economic development in the Yucatan. Econ. Hum. Biol. 2010, 8, 153–158. [Google Scholar] [CrossRef]
- Laviada-Molina, H.; Huchim-Lara, O.; Méndez-Domínguez, N. Health and Well-being in the Yucatan Peninsula Revisited with a Human Ecology Perspective. In Culture, Environment and Health in the Yucatan Peninsula; Springer International Publishing: Cham, Switzerland, 2020; pp. 259–276. [Google Scholar] [CrossRef]
- Shamah-Levy, T.; Vielma-Orozco, E.; Heredia-Hernández, O.; Romero-Martínez, M.; Mojica-Cuevas, J.; Cuevas-Nasu, L.; Méndez Gómez-Humaran, I.; Antonio Avila-Arcos, M.; Rivera-Dommarco, J.A. National Health and Nutrition Survey 2018–2019: National Results; National Institute of Public Health: Cuernavaca, Mexico, 2020. [Google Scholar]
- Lara, P.C.B.; Medina, V.G.; Vázquez, R.C.; Contreras, D.M.; Aguilar, J.R.C.; Pérez, E.G.; Perera, E.A. Exceso de peso, obesidad abdominal y talla baja en adultos económicamente activos de Mérida, México. Res. Soc. Dev. 2023, 12, e0712842746. [Google Scholar] [CrossRef]
- Demidenko, E. Sample size and optimal design for logistic regression with binary interaction. Stat. Med. 2008, 27, 36–46. [Google Scholar] [CrossRef]
- Wang, X.; Ji, X. Sample Size Estimation in Clinical Research. Chest 2020, 158, S12–S20. [Google Scholar] [CrossRef]
- Montilla, M.C.F.; Gómez, R.A.; Amaya-Aguilar, F.; Méndez-Domínguez, N. Pinzamiento femoroacetablar secundario a osteocondroma ilíaco solitario. Rev. Cubana Ortop. Traumatol. 2018, 32, 1–10. Available online: https://revortopedia.sld.cu/index.php/revortopedia/article/view/152 (accessed on 29 November 2020).
- Lohman, T.G.; Roche, A.F.; Martorell, R. Anthropometric Standardization Reference Manual; Human Kinetics Books: Champaign, IL, USA, 1991. [Google Scholar]
- Munro, B.H. Munro’s Statistical Methods for Health Care Research, 6th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2011; pp. 1–567. [Google Scholar]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Zhou, J.; Melugin, H.P.; Hale, R.F.; Leland, D.P.; Bernard, C.D.; Levy, B.A.; Krych, A.J. The Prevalence of Radiographic Findings of Structural Hip Deformities for Femoroacetabular Impingement in Patients with Hip Pain. Am. J. Sports Med. 2020, 48, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Bezuglov, E.; Izmailov, S.; Grinchenko, A.; Emanov, A.; Shoshorina, M.; Malyakin, G.; Telyshev, D.; Lyubushkina, A.; Lazarev, A.; Morgans, R. Prevalence of Asymptomatic Changes in the Groin Region Among Adult Professional Soccer Players and Their Association With Limb Dominance. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2024, 34, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Kelly, B.T.; Larson, C.M. Femoroacetabular impingement: I. Pathoanatomy, clinical evaluation, and arthroscopic treatment strategies. In Sports Hip Injuries; CRC Press: Boca Raton, FL, USA, 2024; pp. 25–48. [Google Scholar]
- Bartlett, G.E.; Stephens, A.S.; Norton, M.R.; Fern, E.D. High incidence of femoroacetabular impingement deformity in bi-column acetabular fractures. HIP Int. 2024, 34, 789–796. [Google Scholar] [CrossRef] [PubMed]
- Crespo-Rodríguez, A.M.; De Lucas-Villarrubia, J.C.; Pastrana-Ledesma, M.; Hualde-Juvera, A.; Méndez-Alonso, S.; Padron, M. The diagnostic performance of non-contrast 3-Tesla magnetic resonance imaging (3-T MRI) versus 1.5-Tesla magnetic resonance arthrography (1.5-T MRA) in femoro-acetabular impingement. Eur. J. Radiol. 2017, 88, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Mascarenhas, V.V.; Castro, M.O.; Rego, P.A.; Sutter, R.; Sconfienza, L.M.; Kassarjian, A.; Schmaranzer, F.; Ayeni, O.R.; Dietrich, T.J.; Robinson, P.; et al. The Lisbon Agreement on Femoroacetabular Impingement Imaging—Part 1: Overview. Eur. Radiol. 2020, 30, 5281–5297. [Google Scholar] [CrossRef]
- Hasegawa, M.; Morikawa, M.; Seaman, M.; Cheng, V.K.; Sudo, A. Population-based prevalence of femoroacetabular impingement in Japan. Mod. Rheumatol. 2021, 31, 899–903. [Google Scholar] [CrossRef]
- Kopec, J.A.; Hong, Q.; Wong, H.; Zhang, C.J.; Ratzlaff, C.; Cibere, J.; Li, L.C.; Prlic, H.; Wilson, D.R.; Forster, B.B.; et al. Prevalence of Femoroacetabular Impingement Syndrome among Young and Middle-aged White Adults. J. Rheumatol. 2020, 47, 1440–1445. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).