Condylar Changes after Maxillary Expansion in Children with Cleft Lip and Palate—A Three-Dimensional Retrospective Study
Abstract
:1. Introduction
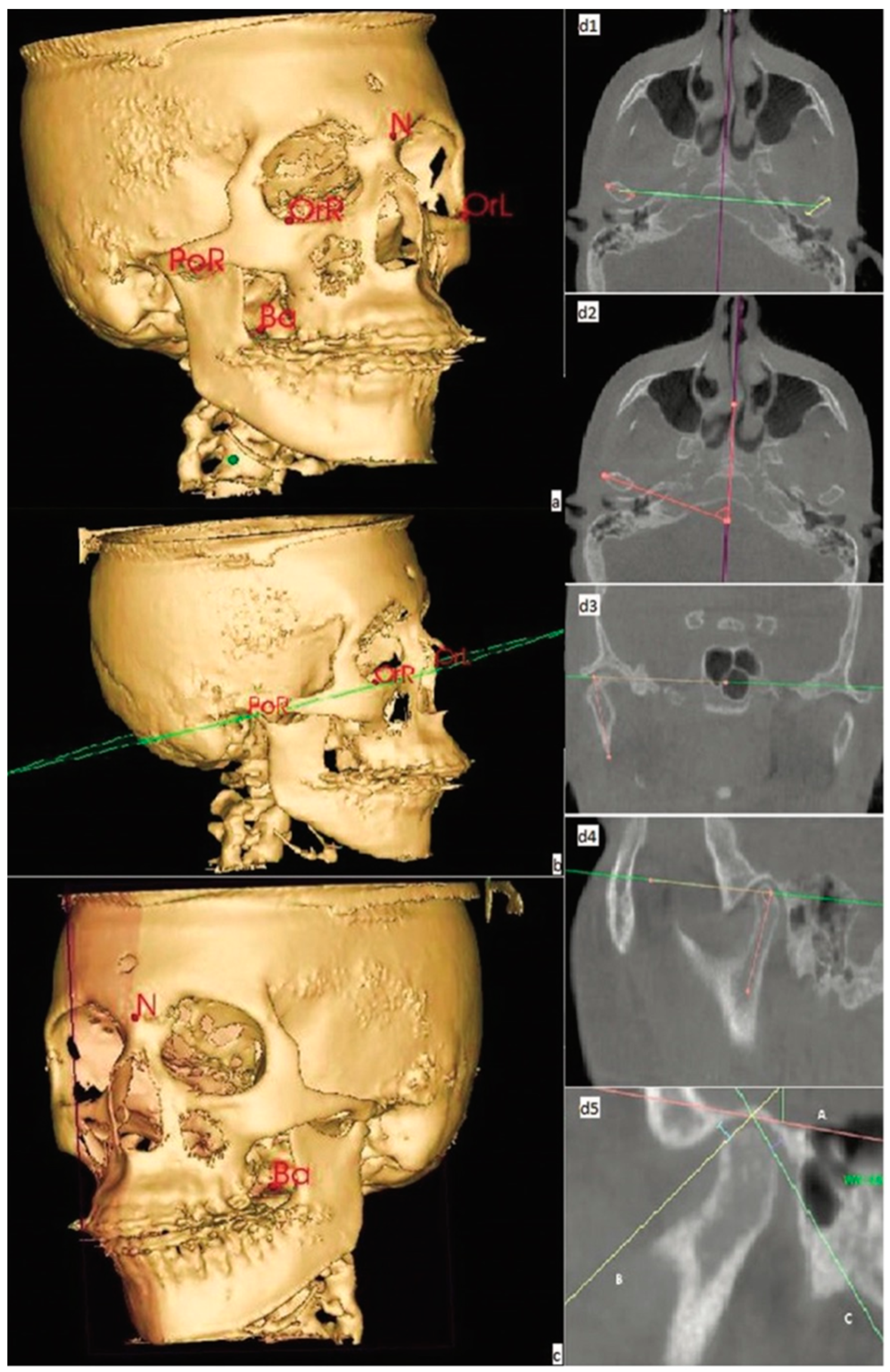
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Celikoglu, M.; Halicioglu, K.; Buyuk, S.K.; Sekerci, A.E.; Ucar, F.I. Condylar and ramal vertical asymmetry in adolescent patients with cleft lip and palate evaluated with cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Celikoglu, M.; Ucar, F.I.; Buyuk, S.K.; Celik, S.; Sekerci, A.E.; Akin, M. Evaluation of the mandibular volume and correlating variables in patients affected by unilateral and bilateral cleft lip and palate: A cone-beam computed tomography study. Clin. Oral Investig. 2016, 20, 1741–1746. [Google Scholar] [CrossRef] [PubMed]
- Uçar, F.I.; Buyuk, S.K.; Şekerci, A.E.; Celikoglu, M. Evaluation of temporomandibular fossa and mandibular condyle in adolescent patients affected by bilateral cleft lip and palate using cone beam computed tomography. Scanning 2016, 38, 720–726. [Google Scholar] [CrossRef] [Green Version]
- Bernheim, N.; Georges, M.; Malevez, C.; De Mey, A.; Mansbach, A. Embryology and epidemiology of cleft lip and palate. B-ENT 2006, 2, 11–19. [Google Scholar]
- Parada, C.; Chai, Y. Roles of BMP signaling pathway in lip and palate development. Front. Oral Biol. 2012, 16, 60–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Francisco, I.; Francisco, C.; Fernandes, M.H.; Vale, F. Parental Risk Factors and Child Birth Data in a Matched Year and Sex Group Cleft Population: A Case-Control Study. Int. J. Environ. Res. Public Health 2021, 18, 4615. [Google Scholar] [CrossRef] [PubMed]
- Leslie, E.J.; Marazita, M.L. Genetics of cleft lip and cleft palate. Am. J. Med. Genet. C Semin. Med. Genet. 2013, 163C, 246–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lammer, E.J.; Shaw, G.M.; Iovannisci, D.M.; Finnell, R.H. Periconceptional multivitamin intake during early pregnancy, genetic variation of acetyl-N-transferase 1 (NAT1), and risk for orofacial clefts. Birth Defects Res. A Clin. Mol. Teratol. 2004, 70, 846–852. [Google Scholar] [CrossRef]
- Little, J.; Gilmour, M.; Mossey, P.A.; Fitzpatrick, D.; Cardy, A.; Clayton-Smith, J.; Hill, A.; Duthie, S.J.; Fryer, A.E.; Molloy, A.M.; et al. Folate and clefts of the lip and palate-a U.K.-based case-control study: Part II: Biochemical and genetic analysis. Cleft Palate Craniofac. J. 2008, 45, 428–438. [Google Scholar] [CrossRef]
- Boyles, A.L.; DeRoo, L.A.; Lie, R.T.; Taylor, J.A.; Jugessur, A.; Murray, J.C.; Wilcox, A.J. Maternal alcohol consumption, alcohol metabolism genes, and the risk of oral clefts: A population-based case-control study in Norway, 1996–2001. Am. J. Epidemiol. 2010, 172, 924–931. [Google Scholar] [CrossRef]
- Zhang, Z.; Stein, M.; Mercer, N.; Malic, C. Post-operative outcomes after cleft palate repair in syndromic and non-syndromic children: A systematic review protocol. Syst. Rev. 2017, 6, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emory, R.E.; Clay, R.P.; Bite, U.; Jackson, I.T. Fistula formation and repair after palatal closure: An institutional perspective. Plast Reconstr. Surg. 1997, 99, 1535–1538. [Google Scholar] [CrossRef] [PubMed]
- Vyas, T.; Gupta, P.; Kumar, S.; Gupta, R.; Gupta, T.; Singh, H.P. Cleft of lip and palate: A review. J. Fam. Med. Prim. Care 2020, 9, 2621–2625. [Google Scholar] [CrossRef] [PubMed]
- Ye, B.; Wu, Y.; Zhou, Y.; Jing, H.; Hu, J.; Zhang, G. A comparative cephalometric study for adult operated cleft palate and unoperated cleft palate patients. J. Craniomaxillofac. Surg. 2015, 43, 1218–1223. [Google Scholar] [CrossRef]
- Naqvi, Z.; Ravi, S.; Shivalinga, B.; Munawwar, S. Effect of cleft lip palate repair on craniofacial growth. J. Orthod. Sci. 2015, 4, 59–64. [Google Scholar] [CrossRef]
- Bugaighis, I.; O’Higgins, P.; Tiddeman, B.; Mattick, C.; Ben Ali, O.; Hobson, R. Three-dimensional geometric morphometrics applied to the study of children with cleft lip and/or palate from the North East of England. Eur. J. Orthod. 2010, 32, 514–521. [Google Scholar] [CrossRef]
- de Almeida, A.M.; Ozawa, T.O.; Alves, A.C.M.; Janson, G.; Lauris, J.R.P.; Ioshida, M.S.Y.; Garib, D.G. Slow versus rapid maxillary expansion in bilateral cleft lip and palate: A CBCT randomized clinical trial. Clin. Oral Investig. 2017, 21, 1789–1799. [Google Scholar] [CrossRef]
- Ellabban, M.T.; Abdul-Aziz, A.I.; Salah Fayed, M.M.; AboulFotouh, M.H.; Elkattan, E.S.; Dahaba, M.M. Positional and dimensional temporomandibular joint changes after correction of posterior crossbite in growing patients: A systematic review. Angle Orthod. 2018, 88, 638–648. [Google Scholar] [CrossRef] [Green Version]
- Paknahad, M.; Shahidi, S.; Bahrampour, E.; Beladi, A.S.; Khojastepour, L. Cone beam computed tomographic evaluation of mandibular asymmetry in patients with cleft lip and palate. Cleft Palate-Craniofac. J. 2018, 55, 919–924. [Google Scholar] [CrossRef]
- Lippold, C.; Hoppe, G.; Moiseenko, T.; Ehmer, U.; Danesh, G. Analysis of condylar differences in functional unilateral posterior crossbite during early treatment--a randomized clinical study. J. Orofac. Orthop. 2008, 69, 283–296. [Google Scholar] [CrossRef]
- Parsaei, Y.; Uribe, F.; Steinbacher, D. Orthodontics for Unilateral and Bilateral Cleft Deformities. Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 297–307. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Oral and Maxillofacial Radiology. Clinical recommendations regarding use of cone beam computed tomography in orthodontics. Position statement by the American Academy of Oral and Maxillofacial Radiology. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 238–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vale, F.; Francisco, I.; Scherzberg, J.; Guimarães, A.; Caramelo, F.; Maló, L. Condylar response to large mandibular advancement combined with maxillary impaction and counterclockwise rotation: A computed tomographic study. J. Clin. Exp. Dent. 2018, 10, e891–e901. [Google Scholar] [CrossRef] [PubMed]
- Janson, H.; Olsson, U. A measure of agreement for interval or nominal multivariate observations by different sets of judges. Educ. Psychol. Meas. 2004, 64, 62–70. [Google Scholar] [CrossRef]
- Chen, S.; Lei, J.; Wang, X.; Fu, K.Y.; Farzad, P.; Yi, B. Short- and long-term changes of condylar position after bilateral sagittal split ramus osteotomy for mandibular advancement in combination with le fort i osteotomy evaluated by cone-beam computed tomography. J. Oral Maxillofac. Surg. 2013, 71, 1956–1966. [Google Scholar] [CrossRef] [PubMed]
- Kilic, N.; Kiki, A.; Oktay, H. Condylar asymmetry in unilateral posterior crossbite patients. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 382–387. [Google Scholar] [CrossRef]
- Leonardi, R.; Caltabiano, M.; Cavallini, C.; Sicurezza, E.; Barbato, E.; Spampinato, C.; Giordano, D. Condyle fossa relationship associated with functional posterior crossbite, before and after rapid maxillary expansion. Angle Orthod. 2012, 82, 1040–1046. [Google Scholar] [CrossRef] [Green Version]
- Kiliaridis, S.; Mahboubi, P.H.; Raadsheer, M.C.; Katsaros, C. Ultrasonographic thickness of the masseter muscle in growing individuals with unilateral crossbite. Angle Orthod. 2007, 77, 607–611. [Google Scholar] [CrossRef] [Green Version]
- Ghoussoub, M.S.; Garcia, R.; Sleilaty, G.; Rifai, K. Effect of rapid maxillary expansion on condyle-fossa relationship in growing patients. J. Contemp. Dent. Pract. 2018, 19, 1189–1198. [Google Scholar]
- Fastuca, R.; Turiaco, H.; Assandri, F.; Zecca, P.A.; Levrini, L.; Caprioglio, A. Condylar Changes in Children with Posterior Crossbite after Maxillary Expansion: Tridimensional Evaluation. Children 2021, 8, 38. [Google Scholar] [CrossRef]
- Holberg, C.; Holberg, N.; Schwenzer, K.; Wichelhaus, A.; Rudzki-Janson, I. Biomechanical analysis of maxillary expansion in CLP patients. Angle Orthod. 2007, 77, 280–287. [Google Scholar] [CrossRef]


| Measure | Description |
|---|---|
| ln (PS/AS) > 0.25 | Anterior position of the condyle in the glenoid fossa |
| ln (PS/AS) < 0.25 | Posterior position of the condyle in the glenoid fossa |
| −0.25 < ln (PS/AS) < 0.25 | Concentric position of the condyle in the glenoid fossa |
| Variable (Plane) | Initial (°) | Final (°) | p § | p £ | |
|---|---|---|---|---|---|
| Condylar angle | Left (frontal) | 79.17 (4.07) | 80.62 (4.02) | 0.030 | 0.114 |
| 70.43/88.70 | 73.93/88.80 | ||||
| Left (axial) | 77.08 (6.35) | 77.81 (5.72) | 0.527 | 0.644 | |
| 59.30/88.63 | 65.10/86.37 | ||||
| Left (sagittal) | 69.63 (8.77) | 71.26 (7.49) | 0.379 | 0.580 | |
| 49.43/84.90 | 58.17/85.23 | ||||
| Right (frontal) | 77.87 (3.79) | 79.17 (4.00) | 0.031 | 0.114 | |
| 70.37/84.97 | 73.03/88.33 | ||||
| Right (axial) | 74.18 (5.70) | 74.70 (6.22) | 0.637 | 0.698 | |
| 61.73/86.87 | 64.07/88.73 | ||||
| Right (sagittal) | 72.83 (5.71) | 71.31 (8.43) | 0.370 | 0.580 | |
| 61.03/84.00 | 47.43/85.10 | ||||
| Condylar position | Left anterior angle | 38.80 (12.12) | 37.12 (10.67) | 0.422 | 0.580 |
| 13.57/65.27 | 10.77/65.00 | ||||
| Left posterior angle | 54.41 (12.11) | 52.27 (11.00) | 0.416 | 0.580 | |
| 28.93/70.43 | 35.53/72.70 | ||||
| Right anterior angle | 37.30 (10.32) | 34.67 (11.21) | 0.270 | 0.580 | |
| 19.30/56.00 | 9.23/60.33 | ||||
| Right posterior angle | 54.50 (13.71) | 53.33 (10.68) | 0.698 | 0.698 | |
| 31.60/80.27 | 30.37/71.20 | ||||
| Variable | Initial (°) | Final (°) | p § | p £ |
|---|---|---|---|---|
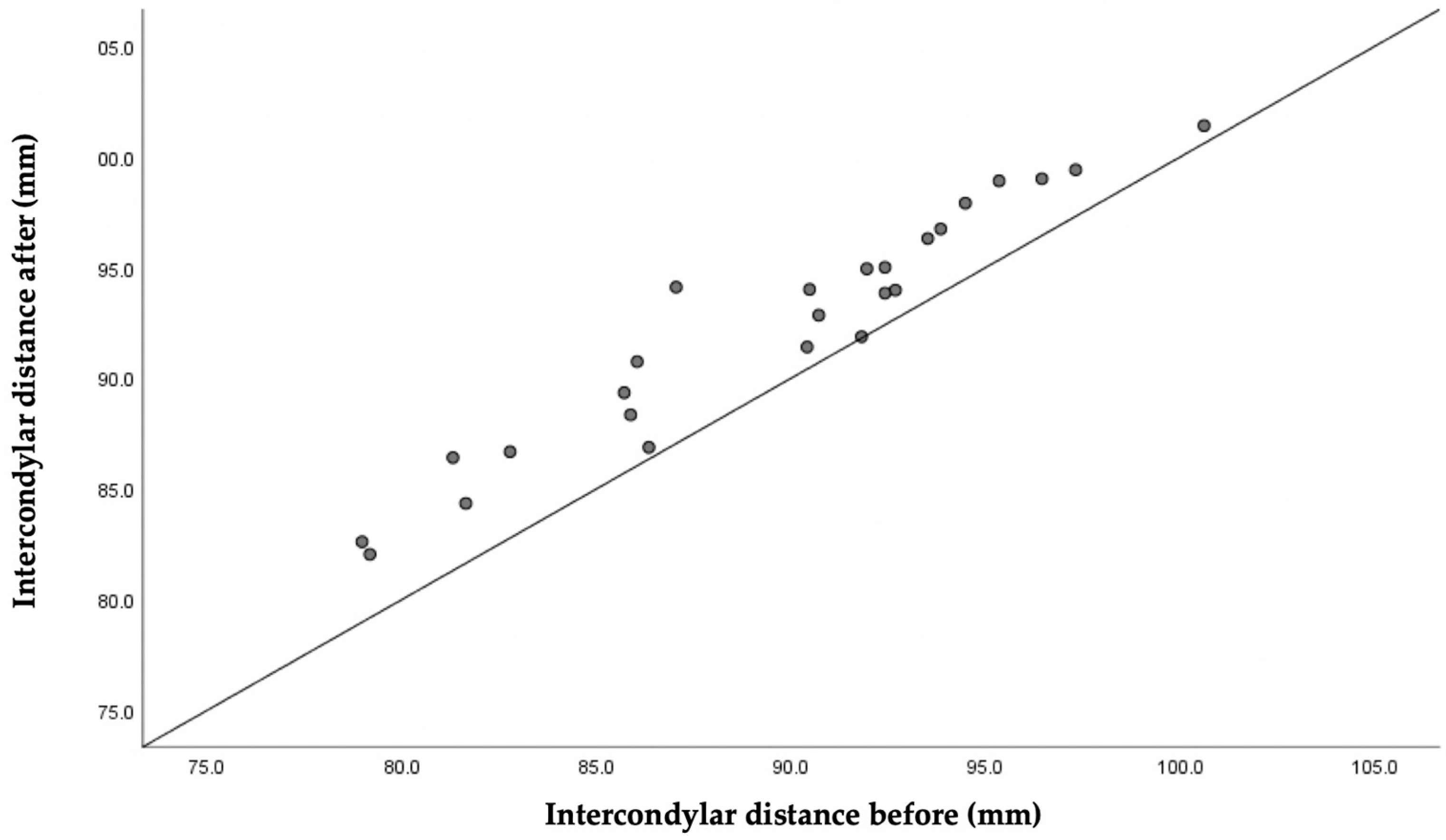
| Intercondylar distance | 89.56 (5.83) 78.97/100.60 | 92.35 (5.41) 82.03/101.40 | <0.001 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Graça, I.C.; Francisco, I.; Guimarães, A.; Caramelo, F.; Vale, F. Condylar Changes after Maxillary Expansion in Children with Cleft Lip and Palate—A Three-Dimensional Retrospective Study. Biomimetics 2022, 7, 73. https://doi.org/10.3390/biomimetics7020073
Graça IC, Francisco I, Guimarães A, Caramelo F, Vale F. Condylar Changes after Maxillary Expansion in Children with Cleft Lip and Palate—A Three-Dimensional Retrospective Study. Biomimetics. 2022; 7(2):73. https://doi.org/10.3390/biomimetics7020073
Chicago/Turabian StyleGraça, Inês Carolina, Inês Francisco, Adriana Guimarães, Francisco Caramelo, and Francisco Vale. 2022. "Condylar Changes after Maxillary Expansion in Children with Cleft Lip and Palate—A Three-Dimensional Retrospective Study" Biomimetics 7, no. 2: 73. https://doi.org/10.3390/biomimetics7020073
APA StyleGraça, I. C., Francisco, I., Guimarães, A., Caramelo, F., & Vale, F. (2022). Condylar Changes after Maxillary Expansion in Children with Cleft Lip and Palate—A Three-Dimensional Retrospective Study. Biomimetics, 7(2), 73. https://doi.org/10.3390/biomimetics7020073









