Abstract
Study purpose: This study aims to investigate the impact of CDSS on patient safety through the experiences of nursing staff. Methods: As the study intends to arrive at specific conclusions on the perceptions of nurses on the impact of CDSS on patients’ safety, a cross-sectional quantitative survey design is adopted in this study. The Hospital Survey of Patients’ Safety Culture (HSOPSC) was used in this study to assess the influence of CDSS on various factors of patient safety. A total of 473 nurses from eight hospitals in Saudi Arabia participated in this study. Results: The PRR of ‘team work within units’ was identified to be the highest (65.9%), followed by ‘hands-off and transitions’ (64.7%), ‘overall patents safety’ (64.1%), and ‘frequency of reports’ that were corrected (61.1%). Communication openness (27.9%) achieved the lowest PRR; while team work across units (2.82) achieved the lowest mean score. Conclusion: The CDSS needs to be integrated with other interventions that promote communication and develop a supportive and cooperative culture among the nurses for ensuring a positive patient safety culture in Saudi Arabian hospitals.
1. Introduction
Patient safety is of paramount importance within the realm of healthcare, forming the cornerstone of high-quality and effective medical services. Ensuring patient safety not only preserves the physical well-being of individuals but also safeguards their emotional and psychological welfare [1,2]. When healthcare facilities prioritize patient safety, they establish an environment where medical errors, adverse events, and preventable harm are minimized. This leads to increased trust between patients and healthcare providers, encouraging patients to seek timely medical attention and adhere to treatment regimens [3,4,5]. Moreover, a robust culture of patient safety reduces the financial burden on healthcare systems by lowering the costs associated with litigation, rehospitalization, and extended care resulting from avoidable errors [6]. Overall, patient safety serves as the ethical and professional duty of healthcare institutions, driving continuous improvement in practices, protocols, and communication to guarantee the best possible outcomes for those under their care [7].
Patient safety is not just a desirable aspect of healthcare; it is an ethical imperative that underscores the commitment to the well-being and dignity of every individual seeking medical assistance. Beyond the physical implications, patient safety holds the key to establishing trust and confidence between patients and healthcare providers [8]. When patients feel secure in the knowledge that their safety is a top priority, they are more likely to engage openly with healthcare professionals, share accurate information about their condition, and actively participate in their treatment plans [9]. In the broader context, prioritizing patient safety contributes significantly to the overall effectiveness and efficiency of healthcare systems. By implementing robust safety protocols and guidelines, healthcare facilities can substantially reduce the occurrence of medical errors, adverse events, and infections [10,11]. This not only prevents unnecessary suffering but also conserves valuable medical resources and reduces the strain on healthcare personnel. Patient safety practices also have financial implications, as they help to curtail the financial burden of compensations for medical errors, lengthy legal battles, and repeated hospitalizations that arise due to preventable incidents [6].
Furthermore, a culture of patient safety fosters a continuous learning environment within healthcare organizations [12]. Each reported error or near-miss event becomes an opportunity for analysis, introspection, and improvement. This culture of transparency encourages healthcare providers to collaborate, share insights, and adapt protocols to prevent similar incidents from occurring in the future [8]. However, the occurrence of adverse events has emerged as one of the most significant challenges facing hospital patients’ safety and the quality of care they receive. They are defined by the World Health Organization as mistakes that happen during nursing care and result in measurable injury or damage to the patient that is not related to the underlying disease [13]. These types of occurrences can include mistakes with medication or equipment, delays in taking therapeutic options, incorrect diagnoses, infections, lost devices, and others [14], all of which have the potential to exert a detrimental influence on the safety and quality of care provided to patients. In the United States, mistakes made by medical professionals are the third leading cause of death [15]. In addition, they are the cause of disability, injury, and even death among patients all over the world [16], in addition to driving up the expenses of medical treatment and hospitalization in developing as well as industrialized nations [14,17]. Even though there have been numerous advancements in medical treatment and diagnosis, adverse events (AEs) continue to be a major concern for both hospital personnel and patients. This is due to the fact that medical treatments and diagnoses are frequently extremely complicated and may be influenced by a wide variety of factors, including human error and hospital infrastructure [14]. Estimates of the incidence rate of adverse events (AEs) in various nations can be found in an expanding body of research literature. For example, a recent meta-analysis found that 2.9 to 21.9% of patients have experienced adverse events (AEs) [14]. According to estimates provided by Kang et al. (2016), 36–57% of nurses have reported experiencing at least one of the four AEs in the preceding 12 months [18]. Another study conducted in China found that between 47.8 and 75.6% of nurses experienced AEs in the preceding year [19]. Recent research conducted on a national scale in Iran found that 29.1% of nurses had encountered AEs in the preceding six-month period [20]. The frequency of AEs in Iran was estimated to be between 10 and 80 percent in 2019, according to a systematic review [17]. Another systematic analysis consisting of 48 research works and employing the Global Trigger Tool came to the conclusion that the incidence of AEs ranged anywhere from 7% to 40% [21].
Mistakes are sometimes unavoidable; these mistakes occur when a barrier in the system that involves them is breached, and this can happen at any point between the initial purchase of the material and its subsequent administration. If this is the case, then placing blame on individuals or engaging in punitive behavior will not be effective in preventing adverse events (AEs). It is essential to place an emphasis on system improvement in order to increase the safety of patients [22]. The protection of patients was considered by industry professionals to be the most important factor in determining the quality of medical care. Because of this, they put in a significant amount of effort to strengthen patient safety systems, including the way that professionals view the need to maintain a culture that prioritizes patient safety. The concept of patient safety culture is defined as “management and staff values, beliefs, and norms about what is important in a health care organization, how organization members are expected to behave, what attitudes and actions are appropriate or inappropriate, and what processes and procedures are rewarded and punished, concerning patient safety” [22]. In this context, the CDSS can be an effective intervention to address the issues in patient safety, as it aids nurses and other healthcare providers in effective decision-making and work management.
Studies [23,24,25,26,27] have identified that a CDSS can provide significant benefits to nurses by enhancing their ability to deliver safe, efficient, and effective patient care. Major benefits include: (a): enhanced decision-making: they provide nurses with evidence-based recommendations and guidelines, assisting them in making informed decisions about patient care. These systems can suggest appropriate interventions, drug dosages, and treatment plans, helping nurses adhere to best practices and reducing the risk of errors; (b) efficiency and time savings: CDSS can streamline workflows by providing quick access to patient information, relevant research, and treatment options; (c) continuing education by providing necessary learning resources; (d) interdisciplinary collaboration: the CDSS facilitates communication and collaboration among healthcare team members, allowing nurses to share information, assessments, and care plans more easily; (e) the CDSS can automate certain documentation tasks, reducing the administrative burden on nurses; (f) support for complex cases: in cases where patients have multiple chronic conditions or complex medical histories, the CDSS can help nurses to navigate the complexities of care by providing relevant information and guidance.
CDSSs play a pivotal role in enhancing patient safety by offering healthcare professionals real-time, evidence-based insights at the point of care. These systems utilize patient data and clinical knowledge to provide tailored recommendations for diagnosis, treatment, and medication management [28]. By alerting physicians to potential drug interactions, allergies, or contraindications, CDSS minimizes medication errors [29]. Additionally, CDSS aids in the early detection of medical conditions through predictive analytics, enabling timely interventions. With access to comprehensive patient histories and medical literature, healthcare providers can make informed decisions, reducing diagnostic errors [30]. Overall, CDSS could act as a reliable partner to clinicians and nurses, offering timely and accurate information that ultimately leads to improved patient outcomes and reduced risks [31].
Conducting research on the influence of CDSS on patient safety is crucial to validate its benefits, identify challenges, and inform healthcare practices. Empirical evidence quantifies the CDSS’s positive influence on areas like medication errors and diagnostic accuracy, guiding effective implementation. It justifies resource allocation, garnering support, and funding for CDSS integration. The dissemination of findings enhances medical knowledge, fostering evidence-based practices among healthcare professionals. Ultimately, such research advances patient safety, aligning technological innovation with improved healthcare outcomes. Therefore, this study aims to investigate the impact of CDSSs on patient safety through the experiences of nursing staff.
2. Methods
As the study intends to arrive at specific conclusions on the perceptions of nurses on the influence of CDSSs on patient safety, a cross-sectional quantitative survey design is adopted in this study.
2.1. Study Setting and Participants
Five public and three private hospitals in Saudi Arabia were considered for the study. Prior approval was taken from the registered entity at these hospitals for conducting the study. All registered nurses at these hospitals with one or more years of experience are considered for the study. An online survey questionnaire approach is adopted for improving the accessibility and comfort for nurses to express their opinions freely.
2.2. Questionnaire Design
2.2.1. Demographic Questionnaire
The demographics and work variables of participants included questions related to gender, age, marital status, working unit, educational level, work experience (years) and work time (hours per week), and hospital size (number of beds).
2.2.2. Patient Safety Culture
A pre-validated and academically recognized Hospital Survey of Patients’ Safety Culture (HSOPSC) [22] was used in this study to assess the impact of CDSSs on various factors of patient safety including “Communication openness” (3 items), “Feedback and communication about errors” (3 items), “Frequency of events reported” (3 items), “Handoffs and transitions” (4 items), “Management support for patient safety” (3 items), “Non-punitive response to error” (3 items), “Organizational learning/continuous improvement” (3 items), “Overall perception of patient safety” (4 items), “Staffing” (4 items), “Supervisor/manager expectations and actions promoting safety” (4 items), and “Teamwork across and within units” (4 items) through a five-point Likert rating scale. A pilot study was conducted with seven nursing students at Imam Abdulrahman Bin Faisal University. Cronbach’s alpha was then calculated for all of the factors and found to be greater than 0.7 for all items, which indicated a good internal consistency and reliability [32]. The questionnaire is designed using Google forms, and a survey link is generated for collecting the data.
2.3. Recruitment and Sampling
Registered nurses from five public and three private hospitals were considered for the study. A participants’ information sheet is attached along with the invitation email (containing survey link), explaining the rights of the participants. As the participants are purposively recruited from eight hospitals, convenience and purposive sampling techniques were adopted [33]. The estimated sample for the study was calculated using Cochran’s formula [34] at a 0.05 confidence interval, resulting in an estimated sample of 382.
2.4. Data Collection
The invitation email with a survey link and participants’ information sheet was forwarded to the head of nursing departments at the eight hospitals, who further forwarded the email to the registered nurses at the respective hospitals. At the end of four weeks, a total of 473 nurses had participated in the study.
2.5. Ethical Considerations
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Imam Abdulrahman Bin Faisal University (IRB-2023-04-291 on 17 July 2023).” All the participants were fully informed about the study through an information sheet attached with the invitation email. Informed consent was taken from all the participants using a check button, before starting the survey. The participation was voluntary and the participants were assured of their anonymity and their rights with respect to the data.
2.6. Data Analysis
As most of the data collected were numerical, statistical techniques such as means, relative frequencies, and standard deviations were used for analyzing the general data. Positive response rates (PRRs) were calculated by dividing the participants who rated 3 or more for each patient safety dimension by the total number of participants. Furthermore, Microsoft SPSS was used to conduct t-tests and one-way ANOVAs for comparing the significant differences between the participants’ groups.
3. Results
Table 1 presents the demographic information of the participants. The majority of the participants were females (70.6%) and were married (73.6%). Also, the majority of the participants were aged between 20 and 29 years (53.9%), followed by 28.8% between 30 and 39 years. Most of the participants had graduated with a diploma (47.8%), followed by a bachelor’s degree (28.8%).

Table 1.
Participants demographics.
The majority of the participants had work experience between three and six years (42.5%), followed by 27.3% between seven and ten years, and 19.9% having more than ten years of work experience. Most of the participants work for 21 to 40 h per week (47.1%), followed by 36.8% working more than 40 h per week. Among the participants, 78% were staff nurses and 22% were nurse managers.
The positive response rates (PRRs) and mean scores of the impact of CDSSs on patient safety culture dimensions are presented in Table 2. The mean scores for the dimensions ranged between 2.82 and 3.77; and the PRRs ranged between 27.9% and 65.9%. The impact of CDSSs is mostly realized in dimensions including organizational learning and continuous improvement (mean score = 3.77), team work within units (mean score = 3.58), overall improvement in patient safety (mean score = 3.58), an increased rate of frequency of reports that were caught and corrected (mean score = 3.55), and hands-off and transitions (mean score = 3.51). The PRR of ‘team work within units’ was identified to be the highest (65.9%), followed by ‘hands-off and transitions’ (64.7%), ‘overall patients safety’ (64.1%), and ‘frequency of reports’ that were corrected (61.1%). Communication openness (27.9%) achieved the lowest PRR; while team work across units (2.82) achieved the lowest mean score.

Table 2.
The mean scores and positive response rate of the impact of CDSS on patient safety culture dimensions.
To further analyze if there existed any differences in the perceptions of staff nurses and nurse managers, t-tests were conducted on patient safety culture dimensions (See Table 3). A statistically significant difference (p< 0.05) was observed in relation to ‘Supervisor/Manager Expectations and Actions Promoting Patient Safety’ (p = 0.0444), ‘Organizational Learning-Continuous Improvement’ (p = 0.0014), ‘Overall Perceptions of Patient Safety’ (p = 0.0037), and ‘non-punitive responses to errors’ (p = 0.0409).

Table 3.
Difference of perceptions between nurse managers and staff nurses.
The mean patient safety grade achieved after using the CDSS was calculated to be 3.56 with a PRR of 56.4%, indicating a medium-to-high impact. To compare the patient safety culture dimensions and patient safety grade perceived, Pearson correlation coefficients were calculated (Table 4), which indicated a strong positive relationship between ‘team work within units’ and ‘patients safety grade’ (R = 0.7262). However, a weak positive relationship was identified between patients’ safety grade and all other remaining patient safety culture dimensions.

Table 4.
Correlations between patient safety culture dimensions and patient safety grades.
As shown in Figure 1, there is a high frequency of event reporting that can be observed among the participants, as most of them reported 11–20 events (49.1%) or 6–10 events (36.9%) in the past 12 months.
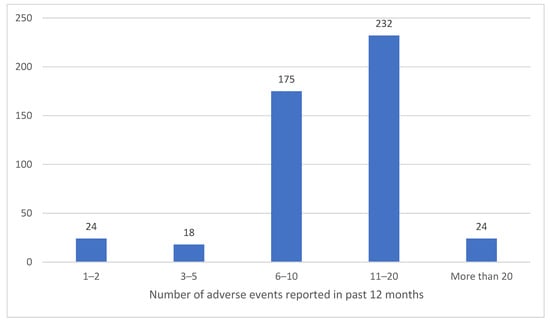
Figure 1.
Number of adverse events reported.
4. Discussion
To the best of the author’s knowledge, this is the first comprehensive research to determine the impact of CDSSs on patient safety through the experiences of nursing staff in Saudi Arabia, where the rapid digitalization of healthcare infrastructure has been observed as a part of the Vision 2030 program [35]. Considering the findings, the PRR for the overall impact of CDSSs on patients safety was calculated to be 64.1%, indicating a significant influence of CDSSs on improving patient safety. The PRR scores for a few dimensions such as feedback and communication about error, non-punitive response to errors, team work across units, and communication openness were less than 50%, indicating a low influence of CDSSs in these areas. This may be attributed to the factors such as ineffective leadership, a blame culture, workload/inadequate staffing, and poor communication hindering a positive patient safety culture as identified in a recent systematic review on patient safety in Saudi Arabia [36]. These issues may be addressed by supervisor/managers actions and through management support; however, both of these dimensions were identified to be less effective in a few settings in Saudi Arabia [37].
The findings in this study were similar to the findings of previous studies [38,39,40,41,42,43,44] conducted in different settings of Saudi Arabia, which have identified dimensions including team work within units, organizational learning and continuous improvement, the frequency of reports, and overall patient safety with high PRRs. Although these dimensions achieved high PRRs in this study, there are slight differences with the mean scores and PRRs identified in other studies in Saudi Arabia. The PRRs of dimensions including organizational learning and continuous improvement achieved in this study were lower compared to the findings in [33,34,35,38]. Contradicting results were observed in relation to non-punitive errors [33], team work within units [40], management support [41], and feedback and communication errors [37,38]. Compared to the low-scored dimensions in previous studies [39,40,41,42,43,44], which include communication openness, feedback and communication about errors, teamwork across units, and hands-off and transitions, this study observed that these dimensions are better scored both in terms of mean scores and PRRs, indicating the positive impact of CDSSs on the poorly rated dimensions in the previous studies. The contrasting results may be attributed to different settings in different studies and varying perceptions of the participants. Accordingly, the differences in the nurses and nurse managers in this study could be identified in managers’ action plans, non-punitive response to errors, and overall patient safety indicating the influence of attitudes, organizational leadership, and culture on the nurses, affecting their perceptions. Accordingly, a strong positive correlation was identified between the ‘team work within units’ dimension and the overall patient safety grade, while other dimensions like management support and communication openness reflected a very weak positive relationship. However, it is interesting to observe the good frequency of reporting observed among the nurses.
CDSSs have been found to improve adherence to clinical guidelines, which can result in improved patient safety [44]. This is noteworthy because it highlights the challenges inherent in implementing conventional clinical guidelines and treatment pathways in practice, where poor levels of adherence have been documented [45,46], which could increase the risk of AEs’ occurrence. A failure to read, comprehend, and apply new standards has been attributed to healthcare practitioners [28]. However, CDSSs can be encoded with the rules that are just implied in guidelines. Such CDSSs may take the form of standardized order sets for a certain case, alerts to a specific protocol for the patients to whom it applies, testing reminders, and so on. For example, a CDSS equipped with glucose monitoring can alert nurses to take readings at different times; and also the digited and personalized CDSSs can facilitate easy hand-offs and transitions minimizing the errors during the change in shifts. In addition to identifying patients suitable for study based on specified criteria, CDSSs can also notify doctors/nurses to reach out to patients who have not followed management plans or are due for follow-up [28]. It has been observed that the use of CDSSs has resulted in an 80% reduction in the occurrence of adverse drug events [29], and decreased medication errors [47,48]. A recent scoping review on patient safety research in Saudi Arabia has observed that a lack of preparedness and issues in integrated learning are the major factors affecting patient safety [30]. Accordingly, another study [48] investigating patient safety has observed that most of the dimensions considered were performing at international benchmarks, with a few performing better than the benchmarks. To improve the performance on several composites of patient safety, CDSSs could be an effective interventional approach, supporting the front-end staff such as nurses in ensuring a positive patient safety culture by empowering them in enhanced decision-making, improved efficiency, and time savings, providing consistent care, enhanced collaboration with other teams, reduced documentation, and support in complex cases [23,24,25,26,27].
As far as the researcher knows, this is the first study to examine the effect of CDSSs on nurses’ perceptions of the frequency of adverse events (AEs) in a Saudi Arabian hospital setting. Even though the study benefited from a number of strengths, including a large sample size (eight hospitals in Saudi Arabia participated), some caveats should be taken into account when analyzing the results. To begin, we enlisted nurses via a method of sampling at our discretion. However, multiple locations were chosen to broaden the applicability of the results. Second, the patients’ own opinions of their own safety culture and the frequency with which AEs occur underpin the study’s conclusions. There may be an exaggeration or underestimation of adverse events (AEs) or patient safety culture items by nurses if they are afraid of repercussions from hospital management. Finally, the study’s cross-sectional design meant that it could only provide a snapshot in time, which dampened the ability to draw causal inferences. To fully analyze the influence of CDSSs on patient safety culture and establish causation, additional study utilizing alternative research designs, such as longitudinal and controlled studies, is required. In conclusion, this study relied on potentially inaccurate nurse estimations of AE frequencies in its assessment of those frequencies.
5. Conclusions
This study examined the influence of CDSSs on patients’ safety from the perspectives of nurses. The findings illustrated that CDSSs could effectively improve various patient safety culture dimensions such as team work within units and continuous learning. In addition, other dimensions including communication openness, feedback and communication about errors, teamwork across units, and hands-off and transitions, which achieved low PRRs in previous studies were significantly improved in the current study findings, indicating the positive influence of CDSSs. The findings in this study contradicted previous studies’ findings in a few contexts, which may be due to the different settings and participants used. It must be understood that while CDSSs can be effective in different patient safety dimensions, there are a few behavioral contexts which need to be managed by effective leadership and management support in order to ensure patient safety. The CDSS needs to be integrated with other interventions that promote communication and develop a supportive and cooperative culture among the nurses. For instance, a non-punitive culture could foster nurses’ initiative to report AEs willingly, as opposed to the prevalent culture of blaming and penalizing healthcare staff for AEs, which can help in developing a positive patient safety culture.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Imam Abdulrahman Bin Faisal University (IRB-2023-04-291 on 17 July 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper. All the participants were fully informed about the study through an information sheet attached with the invitation email. Informed consent was taken from all the participants using a check button, before starting the survey. The participation was voluntary, and the participants were assured of their anonymity and their rights with respect to the data.
Data Availability Statement
Data can be provided upon request.
Conflicts of Interest
The author declares no conflict of interest.
References
- Huang, C.-H.; Wu, H.-H.; Lee, Y.-C.; Van Nieuwenhuyse, I.; Lin, M.-C.; Wu, C.-F. Patient safety in work environments: Perceptions of pediatric healthcare providers in Taiwan. J. Pediatr. Nurs. 2020, 53, 6–13. [Google Scholar] [CrossRef]
- McMullen, S.; Panagioti, M.; Planner, C.; Giles, S.; Angelakis, I.; Keers, R.N.; Robinson, C.; Fu, Y.; Johnson, J.; Tyler, N. Supporting carers to improve patient safety and maintain their well-being in transitions from mental health hospitals to the community: A prioritisation nominal group technique. Health Expect. 2023, 26, 2064–2074. [Google Scholar] [CrossRef]
- Firth-Cozens, J. Organisational Trust: The Keystone to patient safety. BMJ Qual. Saf. 2004, 13, 56–61. [Google Scholar] [CrossRef]
- Auer, C.; Schwendimann, R.; Koch, R.; De Geest, S.; Ausserhofer, D. How Hospital Leaders Contribute to Patient Safety Through the Development of Trust. J. Nurs. Adm. 2014, 44, S38–S44. Available online: https://www.jstor.org/stable/26813189 (accessed on 18 August 2023). [CrossRef]
- Pearson, P.; Steven, A.; Howe, A.; Sheikh, A.; Ashcroft, D.; Smith, P. Learning About Patient Safety: Organizational Context and Culture in the Education of Health Care Professionals. J. Health Serv. Res. Policy 2010, 15 (Suppl. S1), 4–10. [Google Scholar] [CrossRef]
- Slawomirski, L.; Auraaen, A.; Klazinga, N. The Economics of Patient Safety: Strengthening a Value-Based Approach to Reducing Patient Harm at National Level. In OECD Health Working Papers, No. 96; OECD Publishing: Paris, France, 2017. [Google Scholar] [CrossRef]
- McCradden, M.D.; Joshi, S.; Anderson, J.A.; Mazwi, M.; Goldenberg, A.; Zlotnik Shaul, R. Patient Safety and Quality Improvement: Ethical Principles for a regulatory approach to bias in healthcare machine learning. J. Am. Med. Inform. Assoc. 2020, 27, 2024–2027. [Google Scholar] [CrossRef]
- Brenner, M.J.; Hickson, G.B.; Rushton, C.H.; Prince, M.E.P.; Bradford, C.R.; Boothman, R.C. Honesty and transparency, indispensable to the clinical mission—Part II. Otolaryngol. Clin. N. Am. 2022, 55, 63–82. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.-I.; Kim, S.W.; Chin, H.J. Patient participation in patient safety and its relationships with nurses’ patient-centered care competency, teamwork, and Safety Climate. Asian Nurs. Res. 2019, 13, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Gates, P.J.; Hardie, R.-A.; Raban, M.Z.; Li, L.; Westbrook, J.I. How effective are electronic medication systems in reducing medication error rates and associated harm among hospital inpatients? A systematic review and meta-analysis. J. Am. Med. Inform. Assoc. 2020, 28, 167–176. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Patient Safety Action Plan 2021–2030: Towards Eliminating Avoidable Harm in Health Care; World Health Organization: Geneva, Switzerland, 2021; pp. 16–19. [Google Scholar]
- AL Ma’mari, Q.; Sharour, L.A.; Al Omari, O. Fatigue, Burnout, work environment, workload and perceived patient safety culture among critical care nurses. Br. J. Nurs. 2020, 29, 28–34. [Google Scholar] [CrossRef] [PubMed]
- de Vries, E.N.; Ramrattan, M.A.; Smorenburg, S.M.; Gouma, D.J.; Boermeester, M.A. The incidence and nature of in-hospital adverse events: A systematic review. BMJ Qual. Saf. 2008, 17, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Schwendimann, R.; Blatter, C.; Dhaini, S.; Simon, M.; Ausserhofer, D. The occurrence, types, consequences and preventability of in-hospital adverse events–a scoping review. BMC Health Serv. Res. 2018, 18, 521. [Google Scholar] [CrossRef] [PubMed]
- Makary, M.A.; Daniel, M. Medical Error—The Third Leading Cause of Death in the, U.S. BMJ 2016, 353, i2139. [Google Scholar] [CrossRef]
- Vaziri, S.; Fakouri, F.; Mirzaei, M.; Afsharian, M.; Azizi, M.; Arab-Zozani, M. Prevalence of medical errors in Iran: A systematic review and meta-analysis. BMC Health Serv. Res. 2019, 19, 622. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.-H.; Kim, C.-W.; Lee, S.-Y. Nurse-perceived patient adverse events depend on nursing workload. Osong Public Health Res. Perspect. 2016, 7, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Liu, K.; You, L.-M.; Xiang, J.-G.; Hu, H.-G.; Zhang, L.-F.; Zheng, J.; Zhu, X.-W. the relationship between patient safety culture and adverse events: A questionnaire survey. Int. J. Nurs. Stud. 2014, 51, 1114–1122. [Google Scholar] [CrossRef]
- Kakemam, E.; Kalhor, R.; Khakdel, Z.; Khezri, A.; West, S.; Visentin, D.; Cleary, M. Occupational stress and cognitive failure of nurses and associations with on self-reported adverse events: A national cross-sectional survey. J. Adv. Nurs. 2019, 75, 3609–3618. [Google Scholar] [CrossRef] [PubMed]
- Hibbert, P.D.; Molloy, C.J.; Hooper, T.D.; Wiles, L.K.; Runciman, W.B.; Lachman, P.; Muething, S.E.; Braithwaite, J. The application of the global trigger tool: Asystematic review. Int. J. Qual. Health Care 2016, 28, 640–649. [Google Scholar] [CrossRef]
- Reason, J. Human error: Models and management. BMJ Br. Med. J. 2000, 320, 768–770. [Google Scholar] [CrossRef]
- Sorra, J.S.; Dyer, N. Multilevel psychometric properties of the AHRQ hospital survey on patient safety culture. BMC Health Serv. Res. 2010, 10, 199. [Google Scholar] [CrossRef]
- Ayed Aloufi, M. Effect of clinical decision support systems on quality of care by nurses. Int. J. Qual. Res. 2020, 14, 665–678. [Google Scholar] [CrossRef]
- Trzyna, W.; Cox, B.; Coustasse, A. Impact of EMR/EHR and Computer Decision Support Systems on Nursing Homes and Long-Term Care; MBAA International: Chicago, IL, USA, 2023. [Google Scholar]
- Johansson-Pajala, R.-M. Conditions for the Successful Implementation of Computer-Aided Drug Monitoring From Registered Nurses’ Perspective—A Case Site Analysis. CIN Comput. Inform. Nurs. 2019, 37, 196–202. [Google Scholar] [CrossRef]
- Thompson, C.; Mebrahtu, T.; Skyrme, S.; Bloor, K.; Andre, D.; Keenan, A.M.; Ledward, A.; Yang, H.; Randell, R. The effects of computerised decision support systems on nursing and allied health professional performance and patient outcomes: A systematic review and user contextualisation. Health Soc. Care Deliv. Res. 2023, 1–85. [Google Scholar] [CrossRef] [PubMed]
- Ceyhan, O.; Senturk, A.; Karadag, S.; Kilic, Z. Nurses’ Status of Using Information Systems and Opinions about the Benefits to the Profession: Example of a Country. Int. J. Caring Sci. 2021, 14, 137–147. [Google Scholar]
- Sutton, R.T.; Pincock, D.; Baumgart, D.C.; Sadowski, D.C.; Fedorak, R.N.; Kroeker, K.I. An overview of clinical decision support systems: Benefits, risks, and strategies for Success. NPJ Digit. Med. 2020, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Shahmoradi, L.; Safdari, R.; Ahmadi, H.; Zahmatkeshan, M. Clinical decision support systems-based interventions to improve medication outcomes: A systematic literature review on features and effects. Med. J. Islam. Repub. Iran 2021, 35, 27. [Google Scholar] [CrossRef]
- Taheri Moghadam, S.; Sadoughi, F.; Velayati, F.; Ehsanzadeh, S.J.; Poursharif, S. The effects of clinical decision support system for prescribing medication on patient outcomes and physician practice performance: A systematic review and meta-analysis. BMC Med. Inform. Decis. Mak. 2021, 21, 98. [Google Scholar] [CrossRef]
- Menekse, G.G.; Cagiltay, N.E.; Tokdemir, G. Patient Safety & Clinical Decision Support Systems (CDSS): A case study in Turkey. In Proceedings of the 2015 E-Health and Bioengineering Conference (EHB), Iasi, Romania, 19–20 November 2015. [Google Scholar] [CrossRef]
- Taber, K.S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Etikan, I. Comparison of convenience sampling and purposive sampling. Am. J. Theor. Appl. Stat. 2016, 5, 1. [Google Scholar] [CrossRef]
- Woolson, R.F.; Bean, J.A.; Rojas, P.B. Sample Size for Case-Control Studies Using Cochran’s Statistic. Biometrics 1986, 42, 927–932. [Google Scholar] [CrossRef]
- Chowdhury, S.; Mok, D.; Leenen, L. Transformation of health care and the new model of care in Saudi Arabia: Kingdom’s Vision 2030. J. Med. Life 2021, 14, 347–354. [Google Scholar] [CrossRef]
- Albalawi, A.; Kidd, L.; Cowey, E. Factors contributing to the patient safety culture in Saudi Arabia: A systematic review. BMJ Open 2020, 10, e037875. [Google Scholar] [CrossRef] [PubMed]
- Alsulami, A.; A’aqoulah, A.; Almutairi, N. Patient safety culture awareness among healthcare providers in a tertiary hospital in Riyadh, Saudi Arabia. Front. Public Health 2022, 10, 953393. [Google Scholar] [CrossRef] [PubMed]
- Aljabrii, D.I. Assessment of Patient Safety Culture in Saudi Hospitals: A Baseline Study in the Eastern Region. J. King Abdulaziz Univ. Med. Sci. 2012, 19, 43–58. [Google Scholar] [CrossRef]
- Easwaran, V.; Almeleebia, T.M.; Mantargi, M.J.S.; Khan, N.A.; Alshahrani, S.M.; Orayj, K.; Alshehri, O.A.A.; Alqasimi, N.Y.H.; AlFlan, S.A. Patient Safety Culture in the Southern Region of Saudi Arabia: A Survey among Community Pharmacies. Healthcare 2023, 11, 1416. [Google Scholar] [CrossRef]
- Aljaffary, A.; Al Yaqoub, F.; Al Madani, R.; Aldossary, H.; Alumran, A. Patient safety culture in a teaching hospital in Eastern Province of Saudi Arabia: Assessment and opportunities for improvement. Risk Manag. Healthc. Policy 2021, 14, 3783–3795. [Google Scholar] [CrossRef]
- Alotaibi, B.B.; Almadani, A.E.; Salem, O. Saudi nurses perception regarding patient safety in a major tertiary hospital. Open J. Nurs. 2020, 10, 657–664. [Google Scholar] [CrossRef]
- Rawas, H.; Abou Hashish, E.A. Predictors and outcomes of patient safety culture at King Abdulaziz Medical City, Jeddah, Saudi Arabia. A nursing perspective. BMC Nurs. 2023, 22, 229. [Google Scholar] [CrossRef] [PubMed]
- Alahmadi, H.A. Assessment of Patient Safety Culture in saudi arabian hospitals. BMJ Qual. Saf. 2010, 19, e17. [Google Scholar] [CrossRef]
- Kwok, R.; Dinh, M.; Dinh, D.; Chu, M. Improving adherence to asthma clinical guidelines and discharge documentation from emergency departments: Implementation of a dynamic and integrated electronic decision support system. Emerg. Med. Australas. 2009, 21, 31–37. [Google Scholar] [CrossRef]
- Davis, D.A.; Taylor-Vaisey, A. Translating guidelines into practice: A systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. Can. Med. Assoc. J. 1997, 157, 408–416. [Google Scholar]
- Michael, C.; Rand, C.S.; Powe, N.R.; Wu, A.W.; Wilson, M.H. Why don’t physicians follow clinical practice guidelines? a framework for improvement. JAMA 1999, 282, 1458–1465. [Google Scholar] [CrossRef]
- Nuckols, T.K.; Smith-Spangler, C.; Morton, S.C.; Asch, S.M.; Patel, V.M.; Anderson, L.J.; Deichsel, E.L.; Shekelle, P.G. The effectiveness of computerized order entry at reducing preventable adverse drug events and medication errors in hospital settings: A systematic review and meta-analysis. Syst. Rev. 2014, 3, 56. [Google Scholar] [CrossRef] [PubMed]
- Alswat, K.; Abdalla, R.A.; Titi, M.A.; Bakash, M.; Mehmood, F.; Zubairi, B.; Jamal, D.; El-Jardali, F. Improving patient safety culture in Saudi Arabia (2012–2015): Trending, improvement and benchmarking. BMC Health Serv. Res. 2017, 17, 516. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).