Disadvantaged by More Than Distance: A Systematic Literature Review of Injury in Rural Australia
Abstract
1. Introduction
- How is remoteness defined for studies of injury in Australia?
- What is the difference in the incidence of unintentional and/or intentional injury by rurality?
- Are there differences in the mechanism of injury by rurality?
- What factors increase injury risk in rural areas?
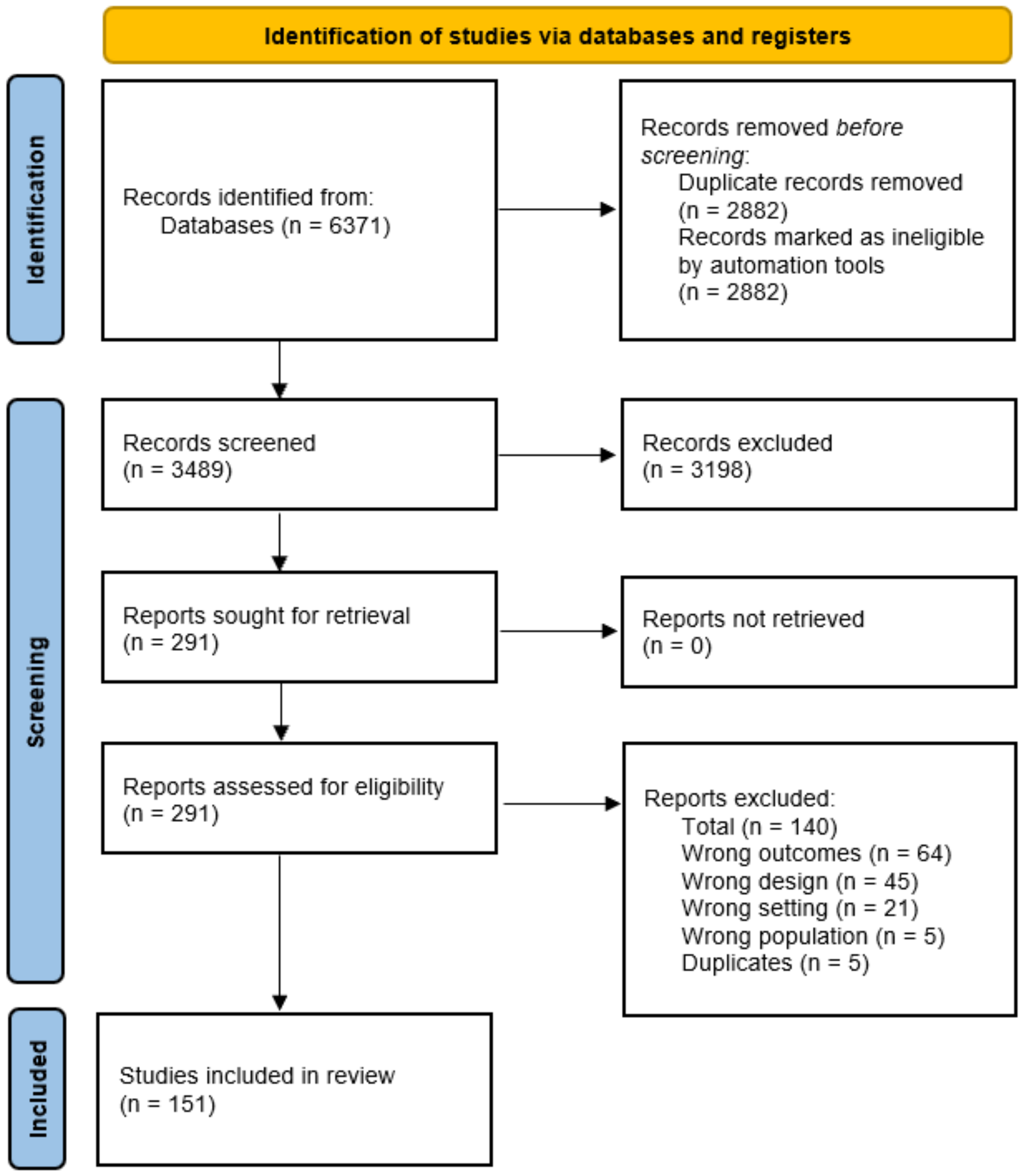
2. Materials and Methods
3. Results
3.1. Rurality as Reported in Australia
3.2. Epidemiology
ASGS Trends in Rural Injury
3.3. Risk Factors
Increase in Morbidity/Mortality—Risk Factors
3.4. Quality Assessment
4. Discussion
4.1. Defining the Burden of Rural Injury
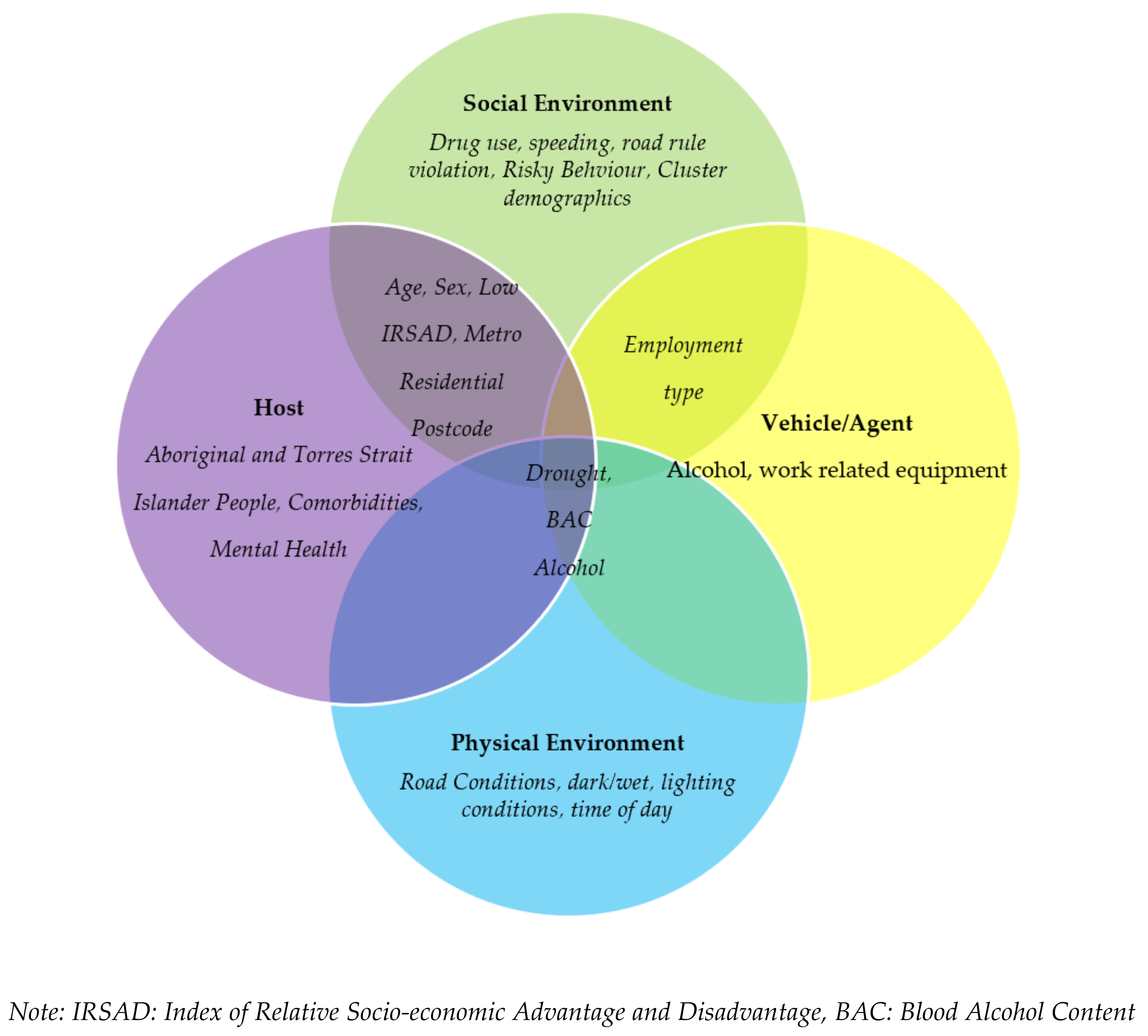
4.2. Risk Factors Affecting Rural Injury
4.2.1. Risk Factors—Age (Host)
4.2.2. Risk Factors—Aboriginal and Torres Strait Islander Peoples (Host)
4.2.3. Risk Factors—Environment
4.3. Protective Factors Affecting Rural Injury
4.4. Rural Injury Severity
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- James, S.L.; Castle, C.D.; Dingels, Z.V.; Fox, J.T.; Hamilton, E.B.; Liu, Z.; Roberts, N.L.; Sylte, D.O.; Henry, N.J.; LeGrand, K.E.; et al. Global injury morbidity and mortality from 1990 to 2017: Results from the Global Burden of Disease Study 2017. Inj. Prev. 2020, 26 (Suppl. 2), i96–i114. [Google Scholar] [CrossRef] [PubMed]
- Ziersch, A.M.; Baum, F.; Darmawan, I.G.N.; Kavanagh, A.M.; Bentley, R.J. Social capital and health in rural and urban communities in South Australia. Aust. N. Z. J. Public Health 2009, 33, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.H.; Peden, A.E.; Franklin, R.C. Next steps for drowning prevention in rural and remote Australia: A systematic review of the literature. Aust. J. Rural Health 2020, 28, 530–542. [Google Scholar] [CrossRef]
- Larson, A. Rural health’s demographic destiny. Rural. Remote Health 2006, 6, 1–8. [Google Scholar] [CrossRef]
- McGrail, M.R.; Humphreys, J.S. Spatial access disparities to primary health care in rural and remote Australia. Geospat. Health 2015, 10, 358. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.L.; Schmidt, T.A.; Newgard, C.D.; Federiuk, C.S.; Christie, M.; Scorvo, S.; DeFreest, M. Search is a time-critical event: When search and rescue missions may become futile. Wilderness Environ. Med. 2007, 18, 95–101. [Google Scholar] [CrossRef]
- Cooper-Stanbury, M.; Nargis, S. (Eds.) Correlates of risky alcohol consumption in regional and remote Australia. In Proceedings of the 10th National Rural Health Conference, Canberra, Australia, 20 July 2009. [Google Scholar]
- Smith, K.B.; Humphreys, J.S.; Wilson, M.G. Addressing the health disadvantage of rural populations: How does epidemiological evidence inform rural health policies and research? Aust. J. Rural Health 2008, 16, 56–66. [Google Scholar] [CrossRef]
- Peden, A.E.; Franklin, R.C. Child injury prevention: It is time to address the determinants of health. Children 2021, 8, 46. [Google Scholar] [CrossRef]
- Australian Government Department of Health. National Injury Prevention Strategy 2020–2030 (Draft for Consultation); Australian Government Department of Health: Canberra, Australia, 2020.
- Higgs, G. Investigating trends in rural health outcomes: A research agenda. Geoforum 1999, 30, 203–221. [Google Scholar] [CrossRef]
- Humphreys, J. Rural health status: What do statistics show that we don’t already know? Aust. J. Rural Health 1999, 7, 60–63. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Haddon, W., Jr. Advances in the epidemiology of injuries as a basis for public policy. Public Health Rep. 1980, 95, 411. [Google Scholar] [PubMed]
- Haddon, W., Jr. Energy damage and the ten countermeasure strategies. Hum. Factors 1973, 15, 355–366. [Google Scholar] [CrossRef] [PubMed]
- 1270.0. 55.005; Australian Statistical Geography Standard (ASGS): Volume 5—Remoteness Structure, July 2016. Australian Bureau of Statistics: Canberra, Australia, 2018.
- Runyan, C.W. Using the Haddon matrix: Introducing the third dimension. Inj. Prev. 1998, 4, 302–307. [Google Scholar] [CrossRef]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid. Synth. 2020, 18, 2127–2133. [Google Scholar] [CrossRef]
- Arraj, G.P.; Rossi-Fedele, G.; Dogramaci, E.J. The association of overjet with traumatic dental injuries: A systematic review protocol. JBI Evid. Synth. 2018, 16, 1511–1518. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. How to Review the Evidence: Systematic Identification and Review of Scientific Literature. 1999. Available online: http://www.nhmrc.gov.au/_files_nhmrc_/publications/attachments/cp65.pdf (accessed on 1 May 2019).
- National Health and Medical Research Council. NHMRC Additional Levels of Evidence and Grades for Recommendations for Developers of Guidelines. 2009. Available online: http://www.nhmrc.gov.au/_files_nhmrc/files/guidlines/developers/nhmrc_levels_grades_evidence_120423.pdf (accessed on 1 May 2019).
- Cairns, R.; Brown, J.A.; Lachireddy, K.; Wylie, C.; Robinson, J.; Dawson, A.H.; Buckley, N.A. Button battery exposures in Australian children: A prospective observational study highlighting the role of poisons information centres. Clin. Toxicol. 2019, 57, 404–410. [Google Scholar] [CrossRef]
- Greenup, E.P.; Potts, B.A. Road deaths relating to the attendance of medical appointments in Queensland. Aust. Health Rev. 2020, 44, 121–124. [Google Scholar] [CrossRef]
- Griffin, B.R.; Kimble, R.M.; Watt, K.; Shields, L. Incidence and characteristics of low-speed vehicle run over events in rural and remote children aged 0–14 years in Queensland: An 11 year (1999–2009) retrospective analysis. Rural. Remote Health 2018, 18, 4224. [Google Scholar] [CrossRef]
- Kruger, E.; Heitz-Mayfield, L.J.A.; Perera, I.; Tennant, M. Geographic modelling of jaw fracture rates in Australia: A methodological model for healthcare planning. Dent. Traumatol. 2010, 26, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Esterman, A.; Thompson, F.; Fitts, M.; Gilroy, J.; Fleming, J.; Maruff, P.; Clough, A.; Bohanna, I. Incidence of emergency department presentations for traumatic brain injury in Indigenous and non-Indigenous residents aged 15–64 over the 9-year period 2007–2015 in North Queensland, Australia. Inj. Epidemiol. 2018, 5, 40. [Google Scholar] [CrossRef]
- Fatovich, D.M.; Phillips, M.; Jacobs, I.G.; Langford, S.A. Major trauma patients transferred from rural and remote Western Australia by the Royal Flying Doctor Service. J. Trauma 2011, 71, 1816–1820. [Google Scholar] [CrossRef] [PubMed]
- Walsh, R.A.; Ryan, L. Hospital admissions in the Hunter Region from trees and other falling objects, 2008–2012. Aust. N. Z. J. Public Health 2017, 41, 121–124. [Google Scholar] [CrossRef]
- Edmonston, C.; Siskind, V.; Sheehan, M. Understanding the Roles of Remoteness and Indigenous Status in Rural and Remote Road Trauma in North Queensland: Using a Mixed-Methods Approach. Int. J. Environ. Res. Public Health 2020, 17, 1467. [Google Scholar] [CrossRef] [PubMed]
- Kavalidou, K.; McPhedran, S.; De Leo, D. Farmers’ contact with health care services prior to suicide: Evidence for the role of general practitioners as an intervention point. Aust. J. Prim. Health 2015, 21, 102–105. [Google Scholar] [CrossRef] [PubMed]
- Schmertmann, M.; Williamson, A.; Black, D. Unintentional poisoning in young children: Does developmental stage predict the type of substance accessed and ingested? Child Care Health Dev. 2014, 40, 50–59. [Google Scholar] [CrossRef]
- Osborne, N.J.; Cairns, R.; Dawson, A.H.; Chitty, K.M.; Buckley, N.A. Epidemiology of coronial deaths from pesticide ingestion in Australia. Int. J. Hyg. Environ. Health 2017, 220, 478–484. [Google Scholar] [CrossRef]
- McPhedran, S.; De Leo, D. Miseries suffered, unvoiced, unknown? Communication of suicidal intent by men in “rural” Queensland, Australia. Suicide Life-Threat. Behav. 2013, 43, 589–597. [Google Scholar] [CrossRef]
- McDermott, K.M.; Brearley, M.B.; Hudson, S.M.; Ward, L.; Read, D.J. Characteristics of trauma mortality in the Northern Territory, Australia. Inj. Epidemiol. 2017, 4, 1–10. [Google Scholar] [CrossRef]
- Liddle, S.E.; McDermott, K.M.; Ward, L.M.; Lim, H.H.; Read, D.J. Quad bike injuries at an Australian regional hospital: A trauma registry review. ANZ J. Surg. 2020, 90, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Lower, T.; Mitchell, R.J. Farm injury hospitalisations in New South Wales (2010 to 2014). Aust. N. Z. J. Public Health 2017, 41, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.J.; Cameron, C.M.; McClure, R. Quantifying the hospitalised morbidity and mortality attributable to traumatic injury using a population-based matched cohort in Australia. BMJ Open 2016, 6, e013266. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.J.; Cameron, C.M.; McClure, R. Patterns of health care use of injured adults: A population-based matched cohort study. Injury 2017, 48, 1393–1399. [Google Scholar] [CrossRef]
- Mitchell, R.J.; Curtis, K.; Foster, K. A 10-year review of child injury hospitalisations, health outcomes and treatment costs in Australia. Inj. Prev. 2018, 24, 344–350. [Google Scholar] [CrossRef]
- Kolves, K.; Potts, B.; De Leo, D. Ten years of suicide mortality in Australia: Socio-economic and psychiatric factors in Queensland. J. Forensic Leg. Med. 2015, 36, 136–143. [Google Scholar] [CrossRef]
- Keel, S.; Xie, J.; Foreman, J.; Taylor, H.R.; Dirani, M. The prevalence of vision loss due to ocular trauma in the Australian National Eye Health Survey. Injury 2017, 48, 2466–2469. [Google Scholar] [CrossRef]
- Katzenellenbogen, J.M.; Atkins, E.; Thompson, S.C.; Hersh, D.; Coffin, J.; Flicker, L.; Hayward, C.; Ciccone, N.; Woods, D.; Greenland, M. Missing voices: Profile, extent, and 12-month outcomes of nonfatal traumatic brain injury in aboriginal and non-aboriginal adults in Western Australia using linked administrative records. J. Head Trauma Rehabil. 2018, 33, 412–423. [Google Scholar] [CrossRef]
- Gilligan, J.; Reilly, P.; Pearce, A.; Taylor, D. Management of acute traumatic intracranial haematoma in rural and remote areas of Australia. ANZ J. Surg. 2017, 87, 80–85. [Google Scholar] [CrossRef]
- Watson, A.; Watson, B.; Vallmuur, K. Estimating under-reporting of road crash injuries to police using multiple linked data collections. Accid. Anal. Prev. 2015, 83, 18–25. [Google Scholar] [CrossRef]
- Mitchell, R.J.; Chong, S. Comparison of injury-related hospitalised morbidity and mortality in urban and rural areas in Australia. Rural. Remote Health 2010, 10, 1326. [Google Scholar] [CrossRef] [PubMed]
- Moller, H.; Falster, K.; Ivers, R.; Clapham, K.; Harvey, L.; Jorm, L. High rates of hospitalised burn injury in Indigenous children living in remote areas: A population data linkage study. Aust. N. Z. J. Public Health 2018, 42, 108–109. [Google Scholar] [CrossRef] [PubMed]
- Baker, T.; Dawson, S.L. Small rural emergency services still manage acutely unwell patients: A cross-sectional study. Emerg. Med. Australas. 2014, 26, 131–138. [Google Scholar] [CrossRef]
- Beck, B.; Teague, W.; Cameron, P.; Gabbe, B.J. Causes and characteristics of injury in paediatric major trauma and trends over time. Arch. Dis. Child. 2019, 104, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Falster, M.O.; Randall, D.A.; Lujic, S.; Ivers, R.; Leyland, A.H.; Jorm, L.R. Disentangling the impacts of geography and Aboriginality on serious road transport injuries in New South Wales. Accid. Anal. Prev. 2013, 54, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Franklin, R.C.; King, J.C.; Aitken, P.J.; Elcock, M.S.; Lawton, L.; Robertson, A.; Mazur, S.M.; Edwards, K.; A Leggat, P. Aeromedical retrievals in Queensland: A five-year review. Emerg. Med. Australas. 2021, 33, 34–44. [Google Scholar] [CrossRef]
- Peden, A.E.; Willcox-Pidgeon, S.M.; Scarr, J.P.; Franklin, R.C. Comparing rivers to lakes: Implications for drowning prevention. Aust. J. Rural Health 2020, 28, 568–578. [Google Scholar] [CrossRef]
- Peden, A.E.; Franklin, R.C.; Pearn, J.H. The prevention of child drowning: The causal factors and social determinants impacting fatalities in portable pools. Health Promot. J. Aust. 2020, 31, 184–191. [Google Scholar] [CrossRef]
- O’Hern, S.; Oxley, J. Fatal cyclist crashes in Australia. Traffic Inj. Prev. 2018, 19 (Suppl. 2), S27–S31. [Google Scholar] [CrossRef]
- Harrison, J.E.; Berry, J.G.; Jamieson, L.M. Head and traumatic brain injuries among Australian youth and young adults, July 2000–June 2006. Brain Inj. 2012, 26, 996–1004. [Google Scholar] [CrossRef]
- Fragar, L.; Inder, K.J.; Kelly, B.J.; Coleman, C.; Perkins, D.; Lewin, T.J. Unintentional injury, psychological distress and depressive symptoms: Is there an association for rural Australians? J. Rural Health 2013, 29, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Cenderadewi, M.; Franklin, R.C.; Peden, A.E.; Devine, S. Pattern of intentional drowning mortality: A total population retrospective cohort study in Australia, 2006–2014. BMC Public Health 2019, 19, 207. [Google Scholar] [CrossRef] [PubMed]
- Berry, J.G.; Jamieson, L.M.; Harrison, J.E. Head and traumatic brain injuries among Australian children, July 2000–June 2006. Inj. Prev. 2010, 16, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Welton, R.E.; Williams, D.J.; Liew, D. Injury trends from envenoming in Australia, 2000–2013. Intern. Med. J. 2017, 47, 170–176. [Google Scholar] [CrossRef] [PubMed]
- West, C.; Rouen, C. Incidence and characteristics of dog bites in three remote Indigenous communities in Far North Queensland, Australia, 2006–2011. J. Vet. Behav. 2019, 31, 17–21. [Google Scholar] [CrossRef]
- Willcox-Pidgeon, S.; Peden, A.E.; Franklin, R.C.; Scarr, J. Boating-related drowning in Australia: Epidemiology, risk factors and the regulatory environment. J. Saf. Res. 2019, 70, 117–125. [Google Scholar] [CrossRef]
- West, C.; Muller, R.; Clough, A.R. Injuries and alcohol management plans in remote Indigenous communities: A two-community comparison. Inj. Prev. 2018, 24, 236–239. [Google Scholar] [CrossRef]
- West, C.; Fitts, M.S.; Rouen, C.; Muller, R.; Clough, A.R. Cause and incidence of injuries experienced by children in remote Cape York Indigenous communities. Aust. J. Prim. Health 2019, 25, 157–162. [Google Scholar] [CrossRef]
- Peck, B.; Terry, D.R.; Kloot, K. Understanding childhood injuries in rural areas: Using Rural Acute Hospital Data Register to address previous data deficiencies. Emerg. Med. Australas. 2020, 32, 646–649. [Google Scholar] [CrossRef]
- Peden, A.E.; Franklin, R.C. Exploring the Impact of Remoteness and Socio-Economic Status on Child and Adolescent Injury-Related Mortality in Australia. Children 2021, 8, 5. [Google Scholar] [CrossRef]
- Derek Cheung, Y.T.; Spittal, M.J.; Williamson, M.K.; Tung, S.J.; Pirkis, J. Predictors of suicides occurring within suicide clusters in Australia, 2004–2008. Soc. Sci. Med. 2014, 118, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Kingston, G.A.; Judd, D.J.; Gray, M.A. The experience of living with a traumatic hand injury in a rural and remote location: An interpretive phenomenological study. Rural. Remote Health 2014, 14, 2764. [Google Scholar] [CrossRef] [PubMed]
- Cheung, Y.T.D.; Spittal, M.J.; Pirkis, J.; Yip, P.S.F. Spatial analysis of suicide mortality in Australia: Investigation of metropolitan-rural-remote differentials of suicide risk across states/territories. Soc. Sci. Med. 2012, 75, 1460–1468. [Google Scholar] [CrossRef]
- McLaren, S. Rurality, reasons for living, and suicidal ideation among Australian men. Death Stud. 2020, 46, 1853–1861. [Google Scholar] [CrossRef] [PubMed]
- Coomber, K.; Miller, P.G.; Livingston, M.; Xantidis, L. Larger regional and rural areas in Victoria, Australia, experience more alcohol-related injury presentations at emergency departments. J. Rural Health 2013, 29, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Lawes, J.C.; Rijksen, E.J.T.; Brander, R.W.; Franklin, R.C.; Daw, S. Dying to help: Fatal bystander rescues in Australian coastal environments. PLoS ONE 2020, 15, e0238317. [Google Scholar] [CrossRef]
- Heathcote, K.; Wullschleger, M.; Gardiner, B.; Morgan, G.; Barbagello, H.; Sun, J. The Importance of Place of Residence on Hospitalized Outcomes for Severely Injured Trauma Patients: A Trauma Registry Analysis. J. Rural. Health 2020, 36, 381–393. [Google Scholar] [CrossRef]
- Inder, K.J.; Holliday, E.G.; Handley, T.E.; Fragar, L.J.; Lower, T.; Booth, A.; Lewin, T.J.; Kelly, B.J. Depression and Risk of Unintentional Injury in Rural Communities-A Longitudinal Analysis of the Australian Rural Mental Health Study. Int. J. Environ. Res. Public Health 2017, 14, 1080. [Google Scholar] [CrossRef]
- Pozzato, I.; Tate, R.L.; Rosenkoetter, U.; Cameron, I.D. Epidemiology of hospitalised traumatic brain injury in the state of New South Wales, Australia: A population-based study. Aust. N. Z. J. Public Health 2019, 43, 382–388. [Google Scholar] [CrossRef]
- Abrari Vajari, M.; Aghabayk, K.; Sadeghian, M.; Shiwakoti, N. A multinomial logit model of motorcycle crash severity at Australian intersections. J. Saf. Res. 2020, 73, 17–24. [Google Scholar] [CrossRef]
- Chen, H.Y.; Senserrick, T.; Martiniuk, A.L.C.; Ivers, R.Q.; Boufous, S.; Chang, H.Y.; Norton, R. Fatal crash trends for Australian young drivers 1997-2007: Geographic and socioeconomic differentials. J. Saf. Res. 2010, 41, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.Y.; Jan, S.; Boufous, S.; Martiniuk, A.L.C.; Ivers, R.; Senserrick, T.; Norton, R.; Muscatello, D. Variations in car crash-related hospitalization costs amongst young adults in New South Wales, Australia. Injury 2012, 43, 1593–1599. [Google Scholar] [CrossRef] [PubMed]
- Johnston, C.I.; Ryan, N.M.; Page, C.B.; Buckley, N.A.; Brown, S.G.; O’Leary, M.A.; Isbister, G.K. The Australian Snakebite Project, 2005–2015 (ASP-20). Med. J. Aust. 2017, 207, 119–125. [Google Scholar] [CrossRef]
- Lang, J.; Sathivelu, M.; Tetsworth, K.; Pollard, C.; Harvey, K.; Bellamy, N. The epidemiology of horse-related injuries for different horse exposures, activities, and age groups in Queensland, Australia. J. Trauma Acute Care Surg. 2014, 76, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Wallis, B.A.; Watt, K.; Franklin, R.C.; Nixon, J.W.; Kimble, R.M. Drowning mortality and morbidity rates in children and adolescents 0-19yrs: A population-based study in Queensland, Australia. PLoS ONE 2015, 10, e0117948. [Google Scholar] [CrossRef]
- Wallis, B.A.; Watt, K.; Franklin, R.C.; Nixon, J.W.; Kimble, R.M. Where children and adolescents drown in Queensland: A population-based study. BMJ Open 2015, 5, e008959. [Google Scholar] [CrossRef] [PubMed]
- Stokes, M.A.; Hemphill, S.; McGillivray, J.; Evans-Whipp, T.; Satyen, L.; Toumbourou, J.W. Self-reported injury in Australian young adults: Demographic and lifestyle predictors. Aust. N. Z. J. Public Health 2020, 44, 106–110. [Google Scholar] [CrossRef]
- Soole, R.; Kolves, K.; De Leo, D. Factors related to childhood suicides: Analysis of the Queensland Child Death Register. Crisis 2014, 35, 292–300. [Google Scholar] [CrossRef]
- Soole, R.; Kolves, K.; De Leo, D. Suicides in Aboriginal and Torres Strait Islander children: Analysis of Queensland Suicide Register. Aust. N. Z. J. Public Health 2014, 38, 574–578. [Google Scholar] [CrossRef]
- Snijder, M.; Calabria, B.; Dobbins, T.; Shakeshaft, A. Factors Associated with Alcohol-Related Injuries for Aboriginal and Non-Aboriginal Australians: An Observational Study. Int. J. Environ. Res. Public Health 2020, 17, 387. [Google Scholar] [CrossRef]
- Lim, K.H.A.; McDermott, K.; Read, D.J. Interpersonal violence and violent re-injury in the Northern Territory. Aust. J. Rural Health 2020, 28, 67–73. [Google Scholar] [CrossRef]
- Meuleners, L.B.; Fraser, M.L.; Bulsara, M.K.; Chow, K.; Ng, J.Q. Risk factors for recurrent injurious falls that require hospitalization for older adults with dementia: A population based study. BMC Neurol. 2016, 16, 188. [Google Scholar] [CrossRef] [PubMed]
- Meuleners, L.B.; Lee, A.H.; Hendrie, D. Interpersonal violence hospitalisations for adolescents: A population-based study. J. Paediatr. Child Health 2010, 46, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Peiris, S.; Berecki-Gisolf, J.; Chen, B.; Fildes, B. Road trauma in regional and remote Australia and New Zealand in preparedness for ADAS technologies and autonomous vehicles. Sustainability 2020, 12, 4347. [Google Scholar] [CrossRef]
- Cheng, D.R.; Ip, C.C.K. Unintentional paediatric poisoning in rural Victoria: Incidence and admission rates. Aust. J. Rural Health 2012, 20, 339–343. [Google Scholar] [CrossRef] [PubMed]
- Cox, S.; Roggenkamp, R.; Bernard, S.; Smith, K. The epidemiology of elderly falls attended by emergency medical services in Victoria, Australia. Injury 2018, 49, 1712–1719. [Google Scholar] [CrossRef]
- Fatovich, D.M.; Phillips, M.; Langford, S.A.; Jacobs, I.G. A comparison of metropolitan vs rural major trauma in Western Australia. Resuscitation 2011, 82, 886–890. [Google Scholar] [CrossRef]
- Giummarra, M.J.; Ekegren, C.L.; Gong, J.; Simpson, P.; Cameron, P.A.; Edwards, E.; Gabbe, B.J. Twelve month mortality rates and independent living in people aged 65 years or older after isolated hip fracture: A prospective registry-based study. Injury 2020, 51, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Giummarra, M.J.; Amoh-Gyimah, R.; Saberi, M.; Gabbe, B.J. Geographic variations in reported and treated pain and mental health problems in the first two years after transport-related major trauma. J. Transp. Health 2019, 14, 14. [Google Scholar] [CrossRef]
- Gregor, S.; Beavan, G.; Culbert, A.; Kan John, P.; Ngo, N.V.; Keating, B.; Sun, R.; Radwan, I. Patterns of pre-crash behaviour in railway suicides and the effect of corridor fencing: A natural experiment in New South Wales. Int. J. Inj. Control Saf. Promot. 2019, 26, 423–430. [Google Scholar] [CrossRef]
- Hanigan, I.C.; Butler, C.D.; Kokic, P.N.; Hutchinson, M.F. Suicide and drought in New South Wales, Australia, 1970–2007. Proc. Natl. Acad. Sci. USA 2012, 109, 13950–13955. [Google Scholar] [CrossRef] [PubMed]
- Hyland, E.J.; Zeni, G.; Harvey, J.G.; Holland, A.J. Rural and Metropolitan Pediatric Burns in New South Wales and the Australian Capital Territory: Does Distance Make a Difference? J. Burn Care Res. 2015, 36, e231–e237. [Google Scholar] [CrossRef] [PubMed]
- Curtis, K.A.; Mitchell, R.J.; Chong, S.S.; Balogh, Z.J.; Reed, D.J.; Clark, P.T.; D’Amours, S.; A Black, D.; E Langcake, M.; Taylor, C.B.; et al. Injury trends and mortality in adult patients with major trauma in New South Wales. Med. J. Aust. 2012, 197, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Wundersitz, L.; Raftery, S. Understanding the context of alcohol impaired driving for fatal crash-involved drivers: A descriptive case analysis. Traffic Inj. Prev. 2017, 18, 781–787. [Google Scholar] [CrossRef] [PubMed]
- Wong Shee, A.; Clapperton, A.; Finch, C.F. Rural v metro: Geographical differences in sports injury hospital admissions across Victoria. Med. J. Aust. 2015, 203, 288. [Google Scholar] [CrossRef]
- Tiemensma, M. Environmental Deaths in the Northern Territory of Australia, 2003–2018. Wilderness Environ. Med. 2019, 30, 177–185. [Google Scholar] [CrossRef]
- Chang, S.S.M.; Symons, R.C.A.; Ozanne-Smith, J. Child road traffic injury mortality in Victoria, Australia (0–14 years), the need for targeted action. Injury 2018, 49, 604–612. [Google Scholar] [CrossRef]
- Chang, S.S.M.; Ozanne-Smith, J. Drowning mortality in children aged 0–14 years in Victoria, Australia: Detailed epidemiological study 2001-2016. Inj. Prev. 2020, 26, 593–598. [Google Scholar] [CrossRef]
- Miu, J.; Curtis, K.; Balogh, Z.J. Profile of fall injury in the New South Wales older adult population. Australas. Emerg. Nurs. J. 2016, 19, 179–185. [Google Scholar] [CrossRef]
- Rintoul, A.C.; Dobbin, M.D.H.; Drummer, O.H.; Ozanne-Smith, J. Increasing deaths involving oxycodone, Victoria, Australia, 2000–2009. Inj. Prev. 2011, 17, 254–259. [Google Scholar] [CrossRef]
- Arnautovska, U.; McPhedran, S.; De Leo, D. A regional approach to understanding farmer suicide rates in Queensland. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 593–599. [Google Scholar] [CrossRef] [PubMed]
- Havard, A.; Shakeshaft, A.P.; Conigrave, K.M.; Sanson-Fisher, R.W. The prevalence and characteristics of alcohol-related presentations to emergency departments in rural Australia. Emerg. Med. J. 2011, 28, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Hill, N.T.M.; Spittal, M.J.; Pirkis, J.; Torok, M.; Robinson, J. Risk factors associated with suicide clusters in Australian youth: Identifying who is at risk and the mechanisms associated with cluster membership. eClinicalMedicine 2020, 29–30, 100631. [Google Scholar] [CrossRef] [PubMed]
- Siskind, V.; Steinhardt, D.; Sheehan, M.; O’Connor, T.; Hanks, H. Risk factors for fatal crashes in rural Australia. Accid. Anal. Prev. 2011, 43, 1082–1088. [Google Scholar] [CrossRef] [PubMed]
- Knight, P.J.; Iverson, D.; Harris, M.F. Early driving experience and influence on risk perception in young rural people. Accid. Anal. Prev. 2012, 45, 775–781. [Google Scholar] [CrossRef]
- Knight, P.J.; Iverson, D.; Harris, M.F. The perceptions of young rural drivers in NSW, Australia of speeding and associated risk: A mixed methods study. Accid. Anal. Prev. 2013, 55, 172–177. [Google Scholar] [CrossRef]
- Hoskins, W.; Jacob, A.; Wijeratne, S.; Campbell, I.; Taylor, P. Splenic injury admitted to a rural Level 3 trauma centre: A 10-year audit. Aust. J. Rural Health 2013, 21, 163–169. [Google Scholar] [CrossRef]
- Handley, T.E.; Inder, K.J.; Kay-Lambkin, F.J.; Stain, H.J.; Fitzgerald, M.; Lewin, T.J.; Attia, J.R.; Kelly, B.J. Contributors to suicidality in rural communities: Beyond the effects of depression. BMC Psychiatry 2012, 12, 105. [Google Scholar] [CrossRef]
- Handley, T.; Rich, J.; Davies, K.; Lewin, T.; Kelly, B. The Challenges of Predicting Suicidal Thoughts and Behaviours in a Sample of Rural Australians with Depression. Int. J. Environ. Res. Public Health 2018, 15, 928. [Google Scholar] [CrossRef]
- Garwood, J.; Wilkinson, B.; Bartholomew, H.; Langford, S.A.; O’Connell, A. Air Ambulance and Emergency Retrieval Services in Western Australia: Caseload Analysis over 5 Years. Air Med. J. 2020, 39, 35–43. [Google Scholar] [CrossRef][Green Version]
- Duke, J.; Rea, S.; Semmens, J.; Wood, F. Urban compared with rural and remote burn hospitalisations in Western Australia. Burns 2012, 38, 591–598. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.; Chapman, M.; McHugh, C.; Sng, A.; Balaratnasingam, S. Rising Indigenous suicide rates in Kimberley and implications for suicide prevention. Australas. Psychiatry 2016, 24, 561–564. [Google Scholar] [CrossRef] [PubMed]
- Wong Shee, A.; Clapperton, A.; Finch, C.F. Increasing trend in the frequency of sports injuries treated at an Australian regional hospital. Aust. J. Rural Health 2017, 25, 125–127. [Google Scholar] [CrossRef] [PubMed]
- Werner, A.K.; Watt, K.; Cameron, C.; Vink, S.; Page, A.; Jagals, P. Examination of child and adolescent hospital admission rates in Queensland, Australia, 1995–2011: A comparison of coal seam gas, coal mining, and rural areas. Matern. Child Health J. 2018, 22, 1306–1318. [Google Scholar] [CrossRef]
- Walker, X.; Lee, J.; Koval, L.; Kirkwood, A.; Taylor, J.; Gibbs, J.; Ng, S.; Steele, L.; Thompson, P.; Leo, C. Predicting ICU admissions from attempted suicide presentations at an Emergency Department in Central Queensland. Australas. Med. J. 2013, 6, 536–541. [Google Scholar] [CrossRef] [PubMed]
- Suen, K.; Skandarajah, A.R.; Knowles, B.; Judson, R.; Thomson, B.N. Changes in the management of liver trauma leading to reduced mortality: 15-year experience in a major trauma centre. ANZ J. Surg. 2016, 86, 894–899. [Google Scholar] [CrossRef]
- Mitchell, R.J.; Lower, T. Rural–urban variation in injury-related hospitalisation, health outcomes and treatment cost in New South Wales. Aust. J. Rural Health 2018, 26, 165–172. [Google Scholar] [CrossRef]
- Holloway-Kew, K.L.; Baker, T.R.; Sajjad, M.A.; Kotowicz, M.A.; Livingston, P.M.; Khasraw, M.; Hakkennes, S.; Dunning, T.L.; Brumby, S.; Page, R.S.; et al. The epidemiology of emergency presentations for falls from height across Western Victoria, Australia. Australas. Emerg. Care 2020, 23, 119–125. [Google Scholar] [CrossRef]
- Holloway-Kew, K.L.; Baker, T.R.; Sajjad, M.A.; Kotowicz, M.A.; Livingston, P.M.; Khasraw, M.; Hakkennes, S.; Dunning, T.L.; Brumby, S.; Page, R.S.; et al. The epidemiology of emergency presentations for falls across Western Victoria, Australia. Australas. Emerg. Care 2019, 22, 206–215. [Google Scholar] [CrossRef]
- Holloway, K.L.; Sajjad, M.A.; Mohebbi, M.; Kotowicz, M.A.; Livingston, P.M.; Khasraw, M.; Hakkennes, S.; Dunning, T.L.; Brumby, S.; Page, R.S.; et al. The epidemiology of hip fractures across western Victoria, Australia. Bone 2018, 108, 1–9. [Google Scholar] [CrossRef]
- Torok, M.; Konings, P.; Batterham, P.J.; Christensen, H. Spatial clustering of fatal, and non-fatal, suicide in new South Wales, Australia: Implications for evidence-based prevention. BMC Psychiatry 2017, 17, 339. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Fletcher, S.; Li, L. Elderly patients with hip fracture are treated promptly in a Tasmanian rural hospital. Aust. J. Rural Health 2013, 21, 130–131. [Google Scholar] [CrossRef] [PubMed]
- LoGiudice, D.C.; Smith, K.; Atkinson, D.; Dwyer, A.; Lautenschlager, N.; Almeida, O.A.; Flicker, L. Preliminary evaluation of the prevalence of falls, pain and urinary incontinence in remote living Indigenous Australians over the age of 45 years. Intern. Med. J. 2012, 42, e102–e107. [Google Scholar] [CrossRef]
- Margolis, S.A.; Ypinazar, V.A.; Muller, R.; Clough, A. Increasing alcohol restrictions and rates of serious injury in four remote Australian Indigenous communities. Med. J. Aust. 2011, 194, 503–506. [Google Scholar] [CrossRef] [PubMed]
- Marshall, T.; Suthersan, M.; Chan, M.K.; Jenkins, B.; Toh, M.; Giddins, V.; Jones, E. Mortality and morbidity of neck of femur fractures: A comparison between Orange and peripheral centres. Aust. J. Rural Health 2016, 24, 253–257. [Google Scholar] [CrossRef]
- McHugh, C.; Balaratnasingam, S.; Campbell, A.; Chapman, M. Suicidal ideation and non-fatal deliberate self-harm presentations in the Kimberley from an enhanced police-mental health service notification database. Australas. Psychiatry 2017, 25, 35–39. [Google Scholar] [CrossRef]
- McPhee, R.; Carlin, E.; Seear, K.; Carrington-Jones, P.; Sheil, B.; Lawrence, D.; Dudgeon, P. Unacceptably high: An audit of Kimberley self-harm data 2014–2018. Australas. Psychiatry 2021, 30, 70–73. [Google Scholar] [CrossRef]
- Miller, P.; Coomber, K.; SØNderlund, A.; McKenzie, S. The long-term effect of lockouts on alcohol-related emergency department attendances within Ballarat, Australia. Drug Alcohol Rev. 2012, 31, 370–376. [Google Scholar] [CrossRef]
- Millhouse, M.G.; Davies, M.J.; Tankel, A.S. Characteristics of short-term re-presentations to a regional emergency department. Emerg. Med. Australas. 2019, 31, 961–966. [Google Scholar] [CrossRef]
- Newman, B.; Berens, H. Occupational health-related experiences in rural Tasmania. Br. J. Community Nurs. 2010, 15, 355–359. [Google Scholar] [CrossRef]
- Northey, L.C.; Bhardwaj, G.; Curran, S.; McGirr, J. Eye trauma epidemiology in regional Australia. Ophthalmic Epidemiol. 2014, 21, 237–246. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Peden, A.E.; Franklin, R.C.; Leggat, P.A. Breathalysing and surveying river users in Australia to understand alcohol consumption and attitudes toward drowning risk. BMC Public Health 2018, 18, 1393. [Google Scholar] [CrossRef] [PubMed]
- Peden, A.E.; Franklin, R.C.; Leggat, P. The flood-related behaviour of river users in Australia. PLoS Curr. 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Pinidiyapathirage, J.; Kitchener, S.; McNamee, S.; Wynter, S.; Langford, J.; Doyle, A.; McMahon, A. Analysis of agriculture-related life-threatening injuries presenting to emergency departments of rural generalist hospitals in Southern Queensland. Emerg. Med. Australas. 2019, 31, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Ponsford, J.; Olver, J.; Ponsford, M.; Schönberger, M. Two-year outcome following traumatic brain injury and rehabilitation: A comparison of patients from metropolitan Melbourne and those residing in regional Victoria. Brain Impair. 2010, 11, 253–261. [Google Scholar] [CrossRef]
- Prabhakaran, S.; Silagy, A.W.; Campbell, N.A.; Flanagan, P.V.; Campbell, I.A. Paediatric injuries during the Australian Junior Motocross Championship treated at a rural centre. Med. J. Aust. 2018, 208, 270. [Google Scholar] [CrossRef]
- Randall, S.M.; Wood, F.M.; Boyd, J.H.; Duke, J.M. Geographic distribution of burn in an Australian setting. Burns 2017, 43, 1575–1585. [Google Scholar] [CrossRef]
- Rouen, C.; Clough, A.R.; West, C. Non-Fatal Deliberate Self-Harm in Three Remote Indigenous Communities in Far North Queensland, Australia. Crisis 2019, 40, 422–428. [Google Scholar] [CrossRef]
- Sankaranarayanan, A.; Carter, G.; Lewin, T. Rural-urban differences in suicide rates for current patients of a public mental health service in Australia. Suicide Life-Threat. Behav. 2010, 40, 376–382. [Google Scholar] [CrossRef]
- Qi, X.; Tong, S.; Hu, W. Spatial distribution of suicide in Queensland, Australia. BMC Psychiatry 2010, 10, 106. [Google Scholar] [CrossRef]
- Qi, X.; Hu, W.; Page, A.; Tong, S. Dynamic pattern of suicide in Australia, 1986–2005: A descriptive-analytic study. BMJ Open 2014, 4, e005311. [Google Scholar] [CrossRef] [PubMed]
- Inder, K.J.; Handley, T.E.; Johnston, A.; Weaver, N.; Coleman, C.; Lewin, T.J.; Slade, T.; Kelly, B.J. Determinants of suicidal ideation and suicide attempts: Parallel cross-sectional analyses examining geographical location. BMC Psychiatry 2014, 14, 208. [Google Scholar] [CrossRef] [PubMed]
- Iversen, J.; Dertadian, G.; Geddes, L.; Maher, L. High risk injecting behaviour among people who inject pharmaceutical opioids in Australia. Int. J. Drug Policy 2017, 42, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Irie, F.; Lang, J.; Kaltner, M.; Le Brocque, R.; Kenardy, J. Effects of gender, indigenous status and remoteness to health services on the occurrence of assault-related injuries in children and adolescents. Injury 2012, 43, 1873–1880. [Google Scholar] [CrossRef]
- Curtis, K.; Kennedy, B.; Lam, M.K.; Mitchell, R.J.; Black, D.; Burns, B.; White, L.; Loudfoot, A.; D’Amato, A.; Dinh, M.; et al. Cause, treatment costs and 12-month functional outcomes of children with major injury in NSW, Australia. Injury 2020, 51, 2066–2075. [Google Scholar] [CrossRef]
- Koo, Y.W.; Kõlves, K.; de Leo, D. Profiles by suicide methods: An analysis of older adults. Aging Ment. Health 2019, 23, 385–391. [Google Scholar] [CrossRef]
- Adams, S.E.; Holland, A.; Brown, J. Management of paediatric splenic injury in the New South Wales trauma system. Injury 2017, 48, 106–113. [Google Scholar] [CrossRef]
- Aitken, L.M.; Burmeister, E.; Lang, J.; Chaboyer, W.; Richmond, T.S. Characteristics and outcomes of injured older adults after hospital admission. J. Am. Geriatr. Soc. 2010, 58, 442–449. [Google Scholar] [CrossRef]
- Beck, B.; Bray, J.E.; Cameron, P.; Straney, L.; Andrew, E.; Bernard, S.; Smith, K. Resuscitation attempts and duration in traumatic out-of-hospital cardiac arrest. Resuscitation 2017, 111, 14–21. [Google Scholar] [CrossRef]
- Boufous, S.; de Rome, L.; Senserrick, T.; Ivers, R.Q. Single—versus multi-vehicle bicycle road crashes in Victoria, Australia. Inj. Prev. 2013, 19, 358–362. [Google Scholar] [CrossRef]
- Boufous, S.; de Rome, L.; Senserrick, T.; Ivers, R. Risk factors for severe injury in cyclists involved in traffic crashes in Victoria, Australia. Accid. Anal. Prev. 2012, 49, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Czech, S.; Shakeshaft, A.P.; Byrnes, J.M.; Doran, C.M. Comparing the cost of alcohol-related traffic crashes in rural and urban environments. Accid. Anal. Prev. 2010, 42, 1195–1198. [Google Scholar] [CrossRef] [PubMed]
- Eranki, V.; Koul, K.; Mendz, G.; Dillon, D. Traumatic facet joint dislocation in Western Australia. Eur. Spine J. 2016, 25, 1109–1116. [Google Scholar] [CrossRef] [PubMed]
- Law C-k Snider, A.-M.; De Leo, D. The influence of deprivation on suicide mortality in urban and rural Queensland: An ecological analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 1919–1928. [Google Scholar]
- Frear, C.C.; Griffin, B.; Watt, K.; Kimble, R.; Watt, K. Barriers to adequate first aid for paediatric burns at the scene of the injury. Health Promot. J. Aust. 2018, 29, 160–166. [Google Scholar] [CrossRef]
- Leckning, B.; Borschmann, R.; Guthridge, S.; Bradley, P.; Silburn, S.; Robinson, G. Aboriginal and non-Aboriginal emergency department presentations involving suicide-related thoughts and behaviors: Characteristics and discharge arrangements. Crisis 2020, 41, 459–468. [Google Scholar] [CrossRef]
- Sukumar, D.W.; Harvey, L.A.; Mitchell, R.J.; Close, J.C.T. The impact of geographical location on trends in hospitalisation rates and outcomes for fall-related injuries in older people. Aust. N. Z. J. Public Health 2016, 40, 342–348. [Google Scholar] [CrossRef]
- Simpson, G.K.; Daher, M.; Hodgkinson, A.; Strettles, B. Comparing the Injury Profile, Service Use, Outcomes, and Comorbidities of People with Severe TBI Across Urban, Regional, and Remote Populations in New South Wales: A Multicentre Study. J. Head Trauma Rehabil. 2016, 31, E26–E38. [Google Scholar] [CrossRef]
- Senserrick, T.; Boufous, S.; de Rome, L.; Ivers, R.; Stevenson, M. Detailed analysis of pedestrian casualty collisions in Victoria, Australia. Traffic Inj. Prev. 2014, 15 (Suppl. 1), S197–S205. [Google Scholar] [CrossRef]
- Lukaszyk, C.; Radford, K.; Delbaere, K.; Ivers, R.; Rogers, K.; Sherrington, C.; Tiedemann, A.; Coombes, J.; Daylight, G.; Draper, B.; et al. Risk factors for falls among older Aboriginal and Torres Strait Islander people in urban and regional communities. Australas. J. Ageing 2018, 37, 113–119. [Google Scholar] [CrossRef]
- Law, C.K.; De Leo, D. Seasonal differences in the day-of-the-week pattern of suicide in Queensland, Australia. Int. J. Environ. Res. Public Health 2013, 10, 2825–2833. [Google Scholar] [CrossRef] [PubMed]
- Dinh, M.M.; Curtis, K.; Mitchell, R.J.; Bein, K.J.; Balogh, Z.J.; Seppelt, I.; Deans, D.; Ivers, R.; Russell, S.B.; Rigby, O. Major trauma mortality in rural and metropolitan NSW, 2009-2014: A retrospective analysis of trauma registry data. Med. J. Aust. 2016, 205, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Dipnall, J.F.; Gabbe, B.J.; Teague, W.J.; Beck, B. Identifying homogeneous patterns of injury in paediatric trauma patients to improve risk-adjusted models of mortality and functional outcomes. Int. J. Environ. Res. Public Health 2020, 17, 892. [Google Scholar] [CrossRef]
- Finch, A.; Cox, S.; Bernard, S.; Teague, W.; Smith, K. The epidemiology of paediatric off-road motorcycle trauma attended by emergency medical services in Victoria, Australia. Injury 2020, 51, 2016–2024. [Google Scholar] [CrossRef] [PubMed]
- Lane, T.J.; Collie, A. Geographic variation in work disability burden: Identifying hotspots, coldspots, and associated sociodemographic factors. Am. J. Ind. Med. 2021, 64, 629–638. [Google Scholar] [CrossRef]
- Kennedy, M.S.; Robinson, J.; Whist, E.; McCallum, G.B.; Mahendrarajah, T. Epidemiology of ocular trauma in the Indigenous vs non-Indigenous population in the Top End. Clin. Exp. Ophthalmol. 2019, 47, 995–999. [Google Scholar] [CrossRef]
- McGrail, M.R.; Humphreys, J.S. Geographical classifications to guide rural health policy in Australia. Aust. N. Z. Health Policy 2009, 6, 28. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Rural, Regional and Remote Health: A Guide to Remoteness Classifications. Canberra; Australian Institute of Health and Welfare, Australia: Darlinghurst, NSW, Australia, 2004. [Google Scholar]
- Wallis, B.A.; Watt, K.; Franklin, R.C.; Kimble, R.M. Drowning in Aboriginal and Torres Strait Islander children and adolescents in Queensland (Australia). BMC Public Health 2015, 15, 795. [Google Scholar] [CrossRef]
- Sun, W.; Jian, L.; Xiao, J.; Akesson, G.; Somerford, P. The Impact of Alcohol Restriction on Hospital and Emergency Department Service Utilizations in Two Remote Towns in the Kimberley Region of Western Australia. Front. Public Health 2019, 7, 17. [Google Scholar] [CrossRef]
- Peden, A.E.; Franklin, R.C.; Leggat, P.A. The hidden tragedy of rivers: A decade of unintentional fatal drowning in Australia. PLoS ONE 2016, 11, e0160709. [Google Scholar] [CrossRef]
- Williams, S.; Bi, P.; Newbury, J.; Robinson, G.; Pisaniello, D.; Saniotis, A.; Hansen, A. Extreme heat and health: Perspectives from health service providers in rural and remote communities in South Australia. Int. J. Environ. Res. Public Health 2013, 10, 5565–5583. [Google Scholar] [CrossRef] [PubMed]
- Perceval, M.; Ross, V.; Kõlves, K.; Reddy, P.; De Leo, D. Social factors and Australian farmer suicide: A qualitative study. BMC Public Health 2018, 18, 1–7. [Google Scholar] [CrossRef]
- Bourke, L.; Humphreys, J.S.; Wakerman, J.; Taylor, J. Understanding rural and remote health: A framework for analysis in Australia. Health Place 2012, 18, 496–503. [Google Scholar] [CrossRef]
- Stiller, L.; Depczynski, J.; Fragar, L.; Franklin, R. An evidence-consultation base for developing child injury prevention priorities for Australian farms. Health Promot. J. Australia 2008, 19, 91–96. [Google Scholar] [CrossRef]
- Humphreys, J.S.; Rolley, F. Health and Health Care in Rural Australia: A Literature Review: Department of Geography and Planning; University of New England: Armidale, Australia, 1991. [Google Scholar]
- Handley, A. Setting the scene: Rural nursing in Australia. In Monograph Series in: Education, Training and Support for Australian Rural Nurses. 1: Association for Australian Rural Nurses Inc.; University of South Australia: Armidale, Australia, 1998. [Google Scholar]
- Nutley, S. Indicators of transport and accessibility problems in rural Australia. J. Transp. Geogr. 2003, 11, 55–71. [Google Scholar] [CrossRef]
- Francis, K. Health and health practice in rural Australia: Where are we, where to from here? Online J. Rural Nurs. Health Care 2012, 5, 28–36. [Google Scholar] [CrossRef]
- Becker, R.; Silvi, J.; Ma Fat, D.; L’Hours, A.; Laurenti, R. A method for deriving leading causes of death. Bull. World Health Organ. 2006, 84, 297–304. [Google Scholar] [PubMed]
- Mackenzie, L.; Byles, J.; Higginbotham, N. A prospective community-based study of falls among older people in Australia: Frequency, circumstances, and consequences. OTJR Occup. Particip. Health 2002, 22, 143–152. [Google Scholar] [CrossRef]
- Finch, C.; Mahoney, M.; Townsend, M.; Zazryn, T. Rural sports and recreational injuries in Australia: What do we know? Aust. J. Rural Health 2003, 11, 151–158. [Google Scholar] [CrossRef]
- Franklin, R.C.; Mitchell, R.J.; Driscoll, T.; Fragar, L. Agricultural work–related fatalities in Australia, 1989–1992. J. Agric. Saf. Health 2001, 7, 213. [Google Scholar] [PubMed]
- Jadhav, R.; Achutan, C.; Haynatzki, G.; Rajaram, S.; Rautiainen, R. Risk factors for agricultural injury: A systematic review and meta-analysis. J. Agromedicine 2015, 20, 434–449. [Google Scholar] [CrossRef] [PubMed]
- Cryer, P.; Fleming, C. A review of work-related fatal injuries in New Zealand 1975-84—numbers, rates and trends. N. Z. Med. J. 1987, 100, 1–6. [Google Scholar] [PubMed]
- Ryan, G.A.; Wright, J.; Hinrichs, R.; McLean, J. An In-Depth Study of Rural Road Crashes in South Australia: Road Accident Research Unit, Adelaide, Australia; South Australia Department of Transport, University of Adelaide: Adelaide, Australia, 1988. [Google Scholar]
- Barnett, D.J.; Balicer, R.D.; Blodgett, D.; Fews, A.L.; Parker, C.L.; Links, J.M. The application of the Haddon matrix to public health readiness and response planning. Environ. Health Perspect. 2005, 113, 561–566. [Google Scholar] [CrossRef]
- Guiney, R. Farming suicides during the Victorian drought: 2001–2007. Aust. J. Rural Health 2012, 20, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Franklin, R.; Simmonds, E.; Peden, A. Drowning Deaths of Rural and Remote Australians. Sydney: Australian Water Safety Council; Secretariat, Royal Life Saving: Sydney, Australia, 2008. [Google Scholar]
- Hirsch, J.K. A review of the literature on rural suicide: Risk and protective factors, incidence, and prevention. Crisis: J. Crisis Interv. Suicide Prevention 2006, 27, 189. [Google Scholar] [CrossRef] [PubMed]
- Williamson, A.; Hatfield, J.; Sherker, S.; Brander, R.; Hayen, A. A comparison of attitudes and knowledge of beach safety in Australia for beachgoers, rural residents and international tourists. Aust. N. Z. J. Public Health 2012, 36, 385–391. [Google Scholar] [CrossRef]
- Della Bona, M.; Crawford, G.; Nimmo, L.; Leavy, J.E. What does ‘Keep Watch’ mean to migrant parents? Examining differences in supervision, cardiopulmonary resuscitation training and water familiarisation. Int. J. Public Health 2019, 64, 755–762. [Google Scholar] [CrossRef]
- Peden, A.E.; Franklin, R.C.; Leggat, P.A. Cardiopulmonary resuscitation and first-aid training of river users in Australia: A strategy for reducing drowning. Health Promot. J. Aust. 2019, 30, 258–262. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Classifications in Included Studies | Transposed Classifications | ||||
|---|---|---|---|---|---|
| Major Cities | Inner Regional | Outer Regional | Remote | Very Remote | |
| ARIA [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40] | Highly accessible | Accessible | Moderately Accessible | Remote | Very Remote |
| ARIA+ [41,42,43,44,45,46,47] | Major Cities | Inner Regional | Outer Regional | Remote | Very Remote |
| ASGS [48,49,50,51,52,53,54] | Major Cities | Inner Regional | Outer Regional | Remote | Very Remote |
| ASGC [55,56,57,58,59,60,61,62,63,64,65] | Major Cities | Inner Regional | Outer Regional | Remote | Very Remote |
| RRMA [66,67,68,69,70] | Metropolitan centers (metropolitan zones 1 and 2) | Large and small rural centers (Rural zones 3–5) | Other rural and remote areas (remote zones 6 and 7) | ||
| Other a [71,72,73] | Major City | Inner Regional | Outer Regional | Remote | |
| Other b [74] | Metro | Rural | Remote | ||
| Other c [146] | Capital Cities | Regional Centres | Rural/Remote Areas | ||
| Other d [75] | City | Town | Rural Areas | ||
| Other e [76,77,78,79,80,81,82,83,84,85,86,87,88,89] | Urban (Metro) | Regional | Rural (or Remote) | ||
| Other f [147,148,149,150] | Major City | Inner Regional | Other | ||
| Other g [151] | Urban | Rural | Remote | ||
| Other h [90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105] | Metro (Urban or City) | Rural (Regional or other or rural/regional) | |||
| Other i [152] | Paediatric TC Metro adult TC Metro local HF | Rural TC Rural local HF | |||
| Other j [153] | Tertiary hospital | Large RH | Small RH | ||
| Other k [154,155,156,157,158,159,160,161,162,163,164,165] | Urban | Rural (or regional or remote) | |||
| Other l [166] | Greater Brisbane | Other Brisbane | |||
| Other m [167,168] | Rural (5000 < 20,000) | ||||
| Other n [169,170] | Rural Scene | ||||
| Other o [171] | Remoteness (100 km from TH) | ||||
| Other p [106,107,108,109] | Statistical Local Areas (2006) (Transposed with ASGS) | ||||
| Other q [90,110,111,112,113,114,115,116,117,118,119,120,121,122] | Single Location (Transposed with ASGS) | ||||
| Other r [123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145] | LGA (Transposed with ASGS) | ||||
| Author | Published | Date Range | Location | Age | Total Participants | Rurality Definition | Intention I/U/B | Injury Type/ Mechanism | ICD Coding | Fatal/ Non-Fatal |
|---|---|---|---|---|---|---|---|---|---|---|
| Berry et al. [58] | 2010 | 2000–2006 | Australia | 0–14 yrs | 95,485 | ASGC | B | TBI (all-cause) | Yes | Non-Fatal |
| Cairns et al. [23] | 2019 | 2015–2017 | NSW | <18 yrs | 506 | ARIA | NR | Button Battery | No | Non-Fatal |
| Cenderadewi et al. [57] | 2019 | 2006–2014 | Australia | all ages | 2731 | Other | B | Drowning | Yes | Fatal |
| Esterman et al. [27] | 2018 | 2007–2015 | North QLD | 15–64 yrs | 3083 | ARIA+ | B | TBI | Yes | NR |
| Falster et al. [50] | 2013 | 2001–2007 | NSW | all ages | 86,969 | ASGS | NR | Road Traffic Injury | Yes | NR |
| Fatovich et al. [28] | 2011a | 1997–2006 | WA | 0–87 yrs | 1328 | ARIA | NR | All-cause Injury | No | NR |
| Franklin et al. [51] | 2021 | 2010–2014 | QLD | all ages | 73,042 | ASGS | B | All-cause Injury | No | NR |
| Gilligan et al. [44] | 2007 | 2000–2013 | SA | 15+ yrs | 162 | ARIA+ | NR | TBI | No | Both |
| Griffin et al. [25] | 2018 | 1999–2009 | QLD | 0–14 yrs | 1506 | ARIA | U | Vehicle Run Over | No | Both |
| Harrison et al. [55] | 2012 | 1970–2007 | Australia | 15–24 yrs | 103,782 | ASGS | B | TBI/HI | Yes | Both |
| Katzenellenbogen et al. [43] | 2018 | 2002–2011 | WA | 15–79 yrs | 16,601 | ARIA+ | U | TBI | Yes | Non-Fatal |
| Mitchell et al. [122] | 2018 | 2010–2014 | NSW | all ages | 496,325 | Other | B | All-cause Injury | Yes | Both |
| Osborne et al. [33] | 2017 | 2001–2013 | Australia | all ages | 209 | ARIA | B | Pesticide Ingestion | No | Both |
| Peden et al. [9] | 2020 | 2007–2017 | Australia | 0–19 yrs | 5153 | ASGS | B | All-cause Injury | Yes | Fatal |
| Peden et al. [52] | 2020 | 2013–2018 | Australia | 0–17 yrs | 342 | ASGC | U | Drowning | Yes | Fatal |
| Age Range | Location | I/UI/B | Injury Type/Mechanism | Fatal/Non-Fatal | Increase with Rurality |
|---|---|---|---|---|---|
| All ages [75] | Victoria | Not Specified | Motorcycle crash injury | Both | Both |
| All ages [48] | Rural Victoria | Not Specified | All injury types and poisoning | Non-Fatal | NR |
| All ages [156] | Victoria | Not Specified | Cyclist crash | Both | Yes |
| All ages [57] | Australia | B | Drowning | Fatal | Yes |
| 0–87 years [28] | Western Australia | Not Specified | All-cause injury | Not Specified | Yes |
| 0–87 years [92] | Western Australia | B | All-cause injury | Not Specified | Yes |
| All ages [24] | Queensland | Not Specified | Road mortality hospitalizations | Fatal | Yes |
| All ages [148] | Australia | I | Opioid injection | Both | Yes |
| All ages [78] | Australia | UI | Snake bites | Both | Yes |
| All ages [31] | Rural Queensland | I | Suicide (all-cause) | Fatal | NR |
| All ages [171] | Northern Territory | Not Specified | Ocular injury—all-cause | Non-fatal | Yes |
| All ages [41] | Queensland | I | Suicide—all-cause | Fatal | Yes |
| All ages [26] | Western Australia | Not Specified | Jaw fractures—all-cause | Non-Fatal | Yes |
| All ages [79] | Queensland | UI | Horse-related injuries—all-cause | Non-fatal | Yes |
| All ages [71] | Australia | UI | Drowning (bystander) | Fatal | Yes |
| All ages [161] | Alice Springs/Darwin (NT) | I | Suicide—all-cause | Non-fatal | Yes |
| All ages [37] | New South Wales | B | Farm Injury (all-cause) | Both | Yes |
| All ages [129] | Rural Queensland | Not Specified | Injury (all hospitalization) | Non-fatal | NR |
| All ages [122] | New South Wales | B | All injury | Both | Yes |
| All ages [136] | Wagga Wagga (NSW) | UI | Eye Trauma (all-cause) | Non-fatal | NR |
| All ages [54] | QLD/NSW/VIC | UI | Cyclist injury | Fatal | NR * |
| All ages [89] | Australia | B | Road Injury (all-cause) | Fatal | Yes |
| All ages [139] | Rural Queensland | UI | Agriculture-related injuries | Both | NR |
| All ages [145] | Queensland | I | Suicide (all-cause) | Fatal | Yes |
| All ages [142] | Western Australia | B | Burns (all-cause) | Both | Yes |
| All ages [143] | Far North Queensland | I | Self-Harm (all-cause) | Non-Fatal | NR |
| All ages [81] | Queensland | UI | Drowning | Both | NR |
| All ages [60] | Far North Queensland | B | Injury—all-cause | Both | NR |
| All ages [68] | Australia | I | Suicide (all-cause) | Fatal | Yes |
| All ages [66] | Australia | I | Suicide (all-cause) | Fatal | Yes |
| All ages [116] | Western Australia | B | Burns | Non-Fatal | Yes |
| All ages [115] | Rural Western Australia | Not specified | Injury and poisoning | Not Specified | NR |
| All ages [165] | New South Wales | UI | Falls (all-cause) | Non-fatal | No |
| All ages [35] | Northern Territory | Both | Injury Trauma (all-cause) | Both | Yes |
| All ages [34] | Queensland | I | Suicidal Ideation (all-cause) | Non-fatal | Yes |
| 10 + years [132] | Western Australia | I | Self-Harm (all-cause) | Non-Fatal | Yes |
| All ages [46] | New South Wales | B | All injury | Both | Yes |
| All ages [135] | Regional Tasmania | UI | All injury | Non-fatal | NR |
| All ages [33] | Australia | B | Pesticide Ingestion (all-cause) | Both | Yes |
| All ages [74] | New South Wales | B | Traumatic Brain Injury () | Both | Yes |
| All ages [141] | Horsham (Victoria) | UI | Motocross injuries | Non-Fatal | NR |
| All ages [146] | Australia | I | Suicide (all-cause) | Fatal | Yes |
| All ages [105] | Victoria | B | Oxycodone Ingestion (all-cause) | Fatal | Yes |
| All ages [126] | New South Wales | I | Suicides and suicide attempts | Both | Yes |
| All ages [45] | Queensland | B | Road crashes | Both | Yes |
| All ages [59] | Australia | UI | Envenoming | Both | Yes |
| All ages [119] | Rural Queensland | B | Injury presentations | Not specified | NR |
| All ages [62] | Far North Queensland | B | Assault hospital presentations | Non-fatal | NR |
| All ages [100] | Victoria | UI | Sports injury hospital admissions | Non-fatal | Yes |
| All ages [118] | Regional Victoria | UI | Hospital sport injury (ED) | Non-fatal | NR |
| All ages [157] | New South Wales | Not Specified | Alcohol-related fatal traffic | Fatal | Yes |
| Age Range | Location | I/UI/B | Injury Type/Mechanism | Fatal/Non-Fatal | Increase with Rurality |
|---|---|---|---|---|---|
| 0–16 years [152] | New South Wales | UI | Splenic injury | Both | Yes |
| <16 years [49] | Victoria | UI | All-cause injury | Non-Fatal | No |
| 0–14 years [58] | Australia | B | Traumatic brain injury | Non-fatal | Yes |
| <18 years [23] | New South Wales | Not Specified | Button battery exposure | Non-fatal | Yes |
| 0–14 years [102] | Victoria | Not Specified | Road traffic injury | Fatal | Yes |
| 0–15 years [168] | Victoria | Not Specified | all-cause pediatric trauma | Both | Yes |
| 0–14 years [25] | Queensland | UI | LSVR injury | Both | Yes |
| <18 years [97] | Westmead (NSW) | B | Pediatric burns—all-cause | Not specified | Yes |
| <17 years [149] | Queensland | I | Assault related injury | Both | Yes |
| 0–17 years [47] | New South Wales | B | Pediatric burns—all-cause | Non-fatal | Yes |
| 0–17 years [53] | Australia | UI | Drowning (portable pools) | Fatal | Yes |
| 0–17 years [9] | Australia | UI | Drowning (all-cause) | Fatal | Yes |
| 0–4 Years [32] | New South Wales | UI | Poisoning (all-cause) | Both | Yes |
| 0–19 years [60] | Far North QLD | UI | Dog bite injuries | Non-fatal | NR |
| 0–14 years [103] | Victoria | UI | Drowning (all-cause) | Fatal | Yes |
| <18 years [77] | New South Wales | UI | Car-crash hospitalizations | Non-fatal | Yes |
| 10–17 years [76] | New South Wales | Not Specified | Road traffic injury | Fatal | Yes |
| 15+ years [98] | New South Wales | Not Specified | All-cause injury | Both | Yes |
| 2–13 years [150] | New South Wales | B | All-cause injury | Non-fatal | No |
| 18+ years [72] | Queensland | N | Injured trauma patients—all-cause | Both | Yes |
| 11–18 years [87] | Western Australia | UI | Falls (all-cause) | Non-Fatal | Yes |
| 0–16 years [40] | Australia | B | All-cause injury | Both | Yes |
| 0–14 years [64] | Regional Victoria | UI | All-cause injury | Non-Fatal | NR |
| 0–19 years [80] | Queensland | UI | Drowning (all-cause) | Both | Yes |
| Age Range | Location | I/U/B | Injury Type/Mechanism | Fatal/Non-Fatal | Increase with Rurality |
|---|---|---|---|---|---|
| all years [106] | Queensland | I | Suicide | Fatal | Yes |
| 16+ years [154] | Victoria | B | Trauma all-cause | Both | No |
| 17–25 years [90] | Wimmera (Victoria) | U | Poisoning | Non-fatal | Yes |
| <45 years [70] | Victoria | No specified | Alcohol-related injury | Non-fatal | Yes |
| 15+ years [44] | South Australia | No specified | TIH—all-cause | Both | No |
| 18+ years [147] | Australia | I | Suicide (all-cause) | Non-fatal | No |
| 15–79 years [43] | Western Australia | U | TBI—all-cause | Non-fatal | Yes |
| 40–98 years [42] | Australia | No specified | Ocular injury all-cause | Non-fatal | Yes |
| 16–30 years [36] | Darwin (NT) | No specified | Quad bike injuries | Both | Yes |
| 27–48 years [86] | Northern Territory | I | Interpersonal violence | Both | Both |
| 45+ years [128] | The Kimberly (WA) | U | Falls (all-cause) | Non-fatal | NR |
| 18–98 years [130] | Orange (NSW) | No specified | Femur fractures (all-cause) | Non-fatal | NA |
| 18+ years [9] | Australia | B | All injury | Fatal | Yes |
| 15–64 years [27] | North Queensland | B | TBI—all mechanism | Not specified | Yes |
| 15–24 years [55] | Australia | B | TBI—all-cause | Both | Yes |
| >40 years [125] | Victoria | No specified | Hip fracture all-cause | Not specified | No |
| >40 years [123] | Victoria | No specified | Fall from height all-cause | Both | No |
| >40 years [124] | Victoria | No specified | Falls all-cause | Not specified | No |
| 18+ years [38] | Australia | B | All injury | Non-fatal | NR * |
| 18+ years [39] | Australia | B | All injury | Non-fatal | NR * |
| 15+ years [144] | Hunter (NSW) | I | Suicide (all-cause) | Fatal | Yes |
| Age Range | Location | I/IU/B | Injury Type/Mechanism | Fatal/Non-Fatal | Increase with Rurality |
|---|---|---|---|---|---|
| 65+ years [153] | Regional QLD | Not Specified | All injury types | Both | NR |
| 65+ years [151] | Queensland | I | Suicide—all-cause | Fatal | Yes |
| 65+ years [91] | Victoria | UI | Falls | non-fatal | Yes |
| 65+ years [127] | Regional Tasmania | UI | Hip fractures (all-cause) | Non-fatal | NA |
| 60+ years [87] | Western Australia | I | Interpersonal violence | Non-Fatal | NR * |
| 55+ years [104] | New South Wales | B | Falls (all-cause) | Both | No |
| Host | Agent/Vehicle | Physical Environment | Social Environment |
|---|---|---|---|
| Age [24,28,31,37,54,56,60,90,92,97,106,113,120,128,140,142,143,159,162] Sex—Male [32,41,44,63,73,96,97,120,136,145,149,162] Sex—Females [41,79,114] Aboriginal and Torres Strait Islander [26,30,43,47,50,83,86,97,131,161,163,171,174] Less comorbidities [162] Comorbidities [43,73,114] Mental Health History [56,73,113,114,147,163] | BAC > 0.05 [99,109] Alcohol [52,107,109,129,133,175] Involving Equipment [139] Sport/Leisure [79] Work-Related Injuries [79,170] Motocross Sport [169] Non-Riders(horse-riding) [79] | Road Conditions—Straight/Open Road [109] Dark/Wet Conditions [155] Unlit/Dawn/Dusk [109] Day of Week/Season [166] Seasonal/Wet Season [117] Drought [96] | Previous attempts and Drug overdose [120] Speeding Related [89,109,164] Road rule violation [109] Low ISRAD [9,147,159,176] Risky Behaviour [54,97,110,111,138] History of abuse/neglect [108] Parent Separation [108] Retired/Unemployed [56] Employment Type (Farmer) [106] Cluster Demographics [145] Metropolitan Residential Postcode [137] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taylor, D.H.; Peden, A.E.; Franklin, R.C. Disadvantaged by More Than Distance: A Systematic Literature Review of Injury in Rural Australia. Safety 2022, 8, 66. https://doi.org/10.3390/safety8030066
Taylor DH, Peden AE, Franklin RC. Disadvantaged by More Than Distance: A Systematic Literature Review of Injury in Rural Australia. Safety. 2022; 8(3):66. https://doi.org/10.3390/safety8030066
Chicago/Turabian StyleTaylor, Danielle H., Amy E. Peden, and Richard C. Franklin. 2022. "Disadvantaged by More Than Distance: A Systematic Literature Review of Injury in Rural Australia" Safety 8, no. 3: 66. https://doi.org/10.3390/safety8030066
APA StyleTaylor, D. H., Peden, A. E., & Franklin, R. C. (2022). Disadvantaged by More Than Distance: A Systematic Literature Review of Injury in Rural Australia. Safety, 8(3), 66. https://doi.org/10.3390/safety8030066






