Abstract
This study aimed to evaluate the accuracy of the Digital Imaging software in the prediction of soft tissue changes following three types of orthodontic interventions: non-extraction, extraction, and orthognathic surgery treatments. Ninety-six patients were randomly selected from the records of three orthodontic interventions (32 subjects per group): (1) non-extraction, (2) extraction, and (3) orthodontic treatment combined with orthognathic surgery. The cephalometric analysis of soft tissue changes in both the actual post-treatment and the predicted treatment was performed using Dolphin Imaging software version 11.9. A paired t-test was utilized to assess the statistically significant differences between the predicted and actual treatment outcomes of the parameters (p < 0.05). In the non-extraction group, prediction errors were exhibited only in the lower lip parameters. In the extraction group, prediction errors were observed in both the upper and lower lip parameters. In the orthognathic surgery group, prediction errors were identified in chin thickness, facial contour angle, and upper and lower lip parameters (p < 0.05). Digital Imaging software exhibited inaccurate soft tissue prediction of 0.3–1.0 mm in some parameters of all treatment groups, which should be considered regarding the application of Dolphin Imaging software in orthodontic treatment planning.
1. Introduction
Facial soft tissue plays a pivotal role in facial aesthetics [1], which constitutes a significant objective in contemporary orthodontic treatments and is often a primary motivation for patients seeking orthodontic care. Variations in soft tissue changes were observed across different age groups, genders, treatment approaches, and pre-treatment soft tissue characteristics [2]. Moreover, predicting a post-treatment soft tissue profile change is a complex task that necessitates consideration of various variables to account for the variability [2]. Therefore, orthodontists encounter significant challenges in forecasting soft tissue outcomes; however, accurate soft tissue prediction is crucial in clinical practice.
Previous manual treatment prediction using cephalometric tracing methods is susceptible to errors in the identification of anatomical landmarks and demands more time for measurement [3]. Consequently, the integration of contemporary digital software aims to overcome the limitations of conventional cephalometric tracing. Computer-assisted cephalometric prediction software, such as the Dolphin Imaging system, offers significant advantages over traditional methods by enabling rapid measurements shortly after marking anatomical landmarks on the radiograph. This not only minimizes the time and effort invested by the orthodontist in treatment planning but also eliminates measurement errors [4,5]. Therefore, digital software has witnessed increased utilization for visual simulation and the prediction of orthodontic treatment outcomes.
Digital prediction software forecasts treatment outcomes by superimposing the patient’s lateral cephalogram and lateral profile photographs. The program represents the expected treatment results in accordance with orthodontic interventions. This information facilitates valuable comparisons among diverse treatment approaches [6,7] that can enable orthodontists to effectively communicate treatment overviews and expected outcomes to patients [8]. However, inaccuracies in simulating soft tissue changes persist with these software applications. Consequently, it is essential to delineate the magnitude, direction, and location of such errors to comprehensively evaluate their potential clinical implications [9].
The accuracy of predictions of soft tissue changes plays a crucial role in orthodontic treatment planning. Although numerous studies have investigated the accuracy and reliability of prediction software, the outcomes have often been inconsistent [10,11,12]. Most of these inaccuracies and disputes are specifically associated with soft tissue predictions. The final outcomes typically deviate from the simulated image due to individual variations in soft tissue adaptation to accommodate skeletal and dental alterations [7]. Furthermore, variations in treatment modalities have been shown to significantly impact these soft tissue responses [2,13]. The potential inaccuracy in soft tissue prediction can lead to unrealistic patient expectations and subsequent dissatisfaction with post-treatment outcomes. Consequently, the aim of this study was to assess the accuracy of Digital Imaging software in predicting soft tissue changes following orthodontic treatment, encompassing cases of non-extraction, extraction, and orthodontic treatment combined with orthognathic surgery. This evaluation compared the discrepancies between the predicted and actual values of these changes.
2. Materials and Methods
This study was designed as a retrospective, cross-sectional observational study. All orthodontic patients from the dental hospital at the Faculty of Dentistry, Prince of Songkla University, who completed their treatment and fulfilled the inclusion criteria were randomly enrolled in this study. This study was approved by the institutional human research ethics committee (No. EC6502-005) and conducted in accordance with the Declaration of Helsinki.
2.1. Subject Selection
Determination of the sample size was conducted by referencing a previous study [10] using the G*Power program version 3.1 (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany), with a significance level set at 0.05 and a study power of 80%. A minimum of 32 subjects per group was required. All subjects were randomly selected from three categories based on the treatment modalities: (1) non-extraction, (2) extraction, and (3) orthodontic treatment combined with orthognathic surgery. As a result, a total of 96 subjects were included in this study. The inclusion and exclusion criteria are shown in Table 1.

Table 1.
Inclusion and exclusion criteria.
2.2. Cephalometric Analysis
The lateral cephalograms were traced and digitized by the same investigator using the Dolphin Imaging program version 11.9 (Chatsworth, CA, USA) under standard settings (Figure 1). All lateral cephalograms were digitized by one expert investigator who had board certification in orthodontics and more than five years of clinical experience.
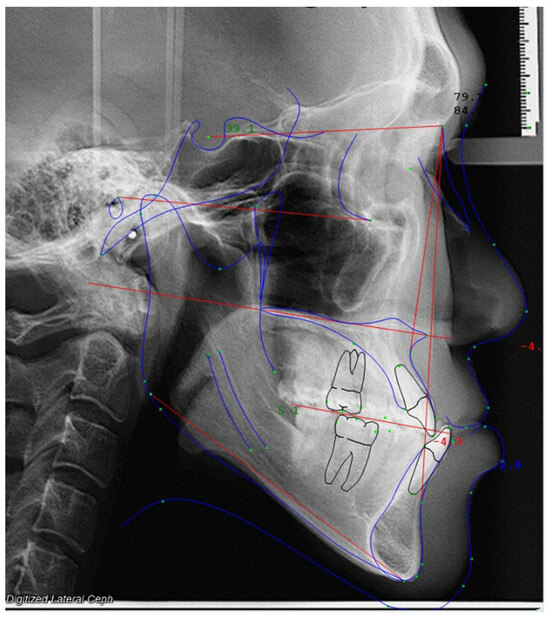
Figure 1.
Cephalometric analysis in Dolphin Imaging software.
The post-treatment values were input into the treatment simulation module of the Dolphin Imaging software, which subsequently generated a predicted treatment outcome. The values of soft tissue changes for both the actual post-treatment and the predicted treatment outcomes were automatically assessed by the Dolphin measurement function.
A total of 22 cephalometric landmarks, which included 12 hard tissue and 10 soft tissue landmarks, were selected for both linear and angular measurements (Figure 2 and Table 2). Cephalometric analysis was conducted in accordance with Steiner’s analysis [14], McNamara analysis [15], Holdaway soft tissue analysis [16], and a study by Nuntasukkasame et al. [17] (Table 3). The values of soft tissue changes in the actual post-treatment and predicted treatment outcomes were automatically documented using the measurement function in the Dolphin Imaging software. The differences between the predicted and actual soft tissue changes were calculated by subtracting the predicted values from the actual values. Positive values indicated that the actual values exceeded the predicted values, whereas negative values indicated the opposite.
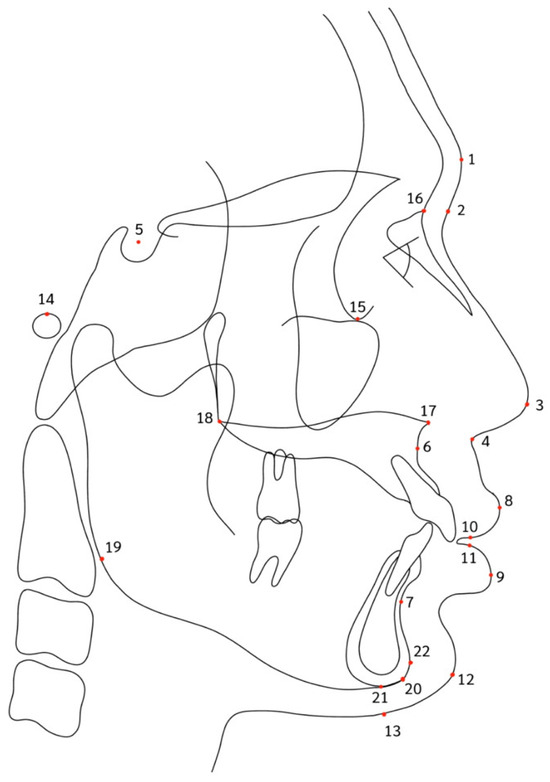
Figure 2.
Cephalometric landmarks in this study.

Table 2.
Cephalometric landmarks.

Table 3.
Soft tissue parameters.
2.3. Statistical Analysis
Statistical analysis of the data was conducted utilizing SPSS statistical software, version 26 (IBM Corp., Armonk, NY, USA). The distribution of data was evaluated using the Shapiro–Wilk test, which confirmed a normal distribution for all variables examined in this study. A paired t-test was employed to evaluate the statistical differences between the predicted and actual treatment outcomes for the parameters under investigation. A significance level of 0.05 was established to determine the statistical significance.
2.4. Quality Control
All measurements were conducted in a blinded manner, wherein the examiner remained unaware of the treatment group associated with the lateral cephalograms. Intraoperative reliability was evaluated using the intraclass correlation coefficient based on a randomly selected sample of 25 lateral cephalograms obtained after a 2-week interval. Upon comparison of the initial and subsequent measurements using an independent t-test, no statistically significant differences were observed between the two sets (p < 0.05). Furthermore, the intraclass correlation coefficient, which exceeded 0.92, indicated excellent reliability. Notably, no systematic error was detected for any variable in the paired t-test (p > 0.05). Random errors were assessed using the Dahlberg formula, which revealed a range of 0.10–0.13 mm for linear cephalometric measurements. These random errors were deemed acceptable.
3. Results
3.1. Non-Extraction Group
Comparisons between the actual and predicted values in the non-extraction group are shown in Table 4. The facial and upper lip parameters were not significantly different. However, significant differences were found in three parameters of the lower lip: the lower lip sulcus depth (−0.43 mm, p = 0.025), the lower lip to the E-plane (−0.44 mm, p = 0.001), and the lower lip to the H-line (−0.31 mm, p = 0.003), whereas the lower lip length showed no significant differences. The negative values indicated that the soft tissue prediction from the Dolphin Imaging software presented a more anterior position of the lower lip than the actual condition.

Table 4.
Comparisons of the soft tissue parameters between actual values and predicted values in non-extraction.
3.2. Extraction Group
The results of the extraction group are shown in Table 5. Significant differences between the actual and predicted values were found in both the upper and lower lip parameters. The four upper lip parameters included the upper lip sulcus depth (−0.36 mm, p = 0.001), the upper lip to the E-plane (−0.39 mm, p = 0.001), the upper lip thickness at the A-point (0.97 mm, p = 0.002), and the upper lip thickness at the vermillion border (1.01 mm, p = 0.004). These indicated that the upper lip prediction from Dolphin Imaging software presented more protrusion and thinner lip thickness at both the A-point and the vermillion border than the actual condition. Three lower lip parameters included the lower lip sulcus depth (−0.35 mm, p = 0.017), the lower lip to the E-plane (−0.58 mm, p < 0.001), and the lower lip to the H-line (−0.50 mm, p = 0.001). These indicated that the lower lip prediction from Dolphin Imaging software presented more protrusion than the actual condition. However, the upper and lower lip lengths, as well as facial parameters, were not significantly different.

Table 5.
Comparisons of the soft tissue parameters between actual values and predicted values in extraction.
3.3. Orthodontic Treatment Combined with Orthognathic Surgery
In the orthognathic surgery group, significant differences between the actual and predicted values were found in all parameter categories that included the facial soft tissue and the upper and lower lips (Table 6). The two facial parameters included the facial contour angle (0.95 mm, p = 0.002) and chin thickness (0.60 mm, p = 0.004). These indicated that the facial soft tissue prediction from Dolphin Imaging software presented more concavity and thinner chin thickness than the actual condition. Two upper lip parameters included the upper lip sulcus depth (−0.55 mm, p = 0.039) and the upper lip to the E-plane (−0.51 mm, p = 0.002). These indicated that the upper lip prediction from the Dolphin Imaging software presented more protrusion than the actual condition. Three lower lip parameters included the lower lip sulcus depth (0.55 mm, p = 0.048), the lower lip to the E-plane (0.68 mm, p < 0.001), and the lower lip to the H-line (0.63 mm, p < 0.001). These indicated that the lower lip prediction from the Dolphin Imaging software presented more retrusion than the actual condition. However, there were no significant differences in the facial heights and lip lengths.

Table 6.
Comparisons of the soft tissue parameters between actual values and predicted values in orthodontic treatment combined with orthognathic surgery.
4. Discussion
Orthodontists commonly encounter inquiries concerning potential alterations to the facial profile that result from a specific treatment plan. Consequently, it is essential to ensure accuracy in predicting the treatment results of soft tissue changes. This accuracy assists orthodontists in formulating optimal treatment plans and providing insights into the final appearance of patients, thereby enhancing patient understanding and satisfaction. Nevertheless, discrepancies between the predicted soft tissue response after orthodontic treatment and the actual outcome are a notable concern. Hence, this study assessed the accuracy of digital software in predicting soft tissue changes following orthodontic interventions among patients who underwent treatments that included non-extraction, extraction, and orthodontic treatment combined with orthognathic surgery.
The accuracy of digital software predictions emerges as a crucial determinant in evaluating and predicting a post-treatment soft tissue profile when formulating an effective treatment plan. In this study, the non-extraction group showed that the lower lip position was simulated to be 0.3–0.4 mm more anteriorly than the actual outcome. This finding contradicted a previous study [12], in which only the vertical placement of the lower lip was simulated to appear more inferiorly (about 1.2 mm) than its actual position. The inconsistent results may be attributed to the presence of lower incisor crowding observed in non-extraction cases in our study, which was corrected through the proclination of the lower incisors. A previous study reported that a slight increase in lower lip thickness and protrusion was observed in correlation with an increase in incisal inclination [18]. In addition, the low accuracy in predicting the lower lip could be attributed to several factors, including the flexibility and susceptibility of the lower lip to the impact of incisor position and angulations. Other factors include soft tissue thickness and tonicity, as well as perioral musculature and underlying muscle attachments [19,20].
In the extraction group, orthodontic treatments possess the ability to influence the facial profile and aesthetic aspects of a patient, especially in scenarios involving extractions and substantial anterior retraction [21,22]. The extraction of premolars may potentially lead to increased lip retrusion compared to treatments in non-extraction cases [23]. Differences in the accuracy of lip position prediction were found between the investigations. This study revealed that the upper and lower lip responses after extraction were notably less (0.3–0.5 mm) than the digitally predicted responses when the incisors underwent retraction. Consistent with a previous study [12], the extraction cases predicted a significantly more protruded horizontal position of both lips than what was observed, while the vertical position of the lip remained unchanged. In contrast, the study conducted by Zhang et al. [10] reported more protrusion and inferior positioning of the lips than depicted in real images. This variation can be attributed to distinctions in the populations studied, as Zhang et al. focused on cases of bimaxillary dentoalveolar protrusion. It was observed that cases with bimaxillary protrusion exhibited a slightly greater degree of soft tissue change compared to patients with maxillary protrusion [24]. This suggested that the vertical position of the lips in patients with bimaxillary dentoalveolar protrusion can be influenced by extraction [25]. However, minimal alterations were noted in our study due to the inclusion of borderline extraction cases [26]. Additionally, there was a robust correlation observed between the movement of incisors and both upper and lower lips [27]. The extent of lower lip movement increased proportionally with the degree of maxillary protrusion [24].
Due to the variability and challenges associated with predicting soft tissue changes post-surgically, it is imperative to assess the accuracy of the Dolphin program. This study revealed significant differences between the actual treatment outcomes and the predicted values within the surgery group. The actual values of chin thickness, facial contour angle, and lower lip parameters exceeded the predicted values by 0.5–1.0 mm. However, the actual post-surgical results of the upper lip exhibited more retrusive positions (about 0.5 mm) than the treatment simulation. This aligns with previous studies that indicated that the lips and chin were the most inaccurately predicted landmarks following orthognathic treatment [7,11,28]. Specifically, upper lip landmarks were more likely to be underestimated, while those surrounding the lower lip and chin area tended to be overestimated in the horizontal plane [8]. The poor accuracy of predicting soft tissue changes in the lip and chin regions may be attributed to factors such as soft tissue thickness, tonicity, perioral musculature, and underlying muscle attachments [2,29]. Additionally, the unstable trait of soft tissue thickness in the chin region is associated with the individual’s body mass index [30]. Consequently, these critical considerations were not integrated into the prediction process, which potentially compromised the overall accuracy and comprehensiveness of the prognostic outcomes.
While the utilization of Dolphin Imaging software has enhanced the capacity of clinicians to anticipate soft tissue profiles following orthodontic treatment, there are certain errors in predicting treatment outcomes with some degree of inaccuracy in specific directions. Numerous studies that compared the software-generated predictions with the actual treatment outcomes revealed noteworthy disparities in the measurements [31,32]. This study demonstrated that the mean differences between the predicted and actual postoperative images were confined within a range of less than 2 mm across various subject groups. Despite the presence of statistically significant differences between the simulated and actual positions of specific points, the majority of these differences were of insufficient magnitude to attain clinical significance [8]. Therefore, the Dolphin Imaging software could be considered an alternative tool to predict soft tissue responses in orthodontic treatment with clinically acceptable accuracy.
This study has some limitations. First, it was conducted using two-dimensional analysis, which limited the measurement of changes in projections or variations in lip length along a fixed plane. To enhance the capability of soft tissue analysis, 3D construction from cone beam computed tomography and a 3D facial scanner is recommended for further study. The incorporation of this advancement into future studies has the potential to significantly enhance the understanding and accuracy of the analyses, which would offer a more comprehensive perspective on orthodontic and surgical planning. Second, the Dolphin software generates a prediction based on a fixed ratio of movement between the soft and hard tissues to simulate changes following treatment. Unfortunately, the changes that occur after treatment are not limited to hard tissue movement alone. Numerous additional factors exert an impact on soft tissue modifications that include thickness, tension, dentofacial morphology, and the measurement technology employed [13,24,33]. Consequently, it is essential to take these factors into account during the prediction process to prevent unrealistic expectations and patient dissatisfaction. Finally, this was a retrospective study. The subjects were not perfectly homogeneous due to different types and magnitudes of dental and skeletal discrepancies. Additional studies are needed to investigate the subtypes of orthognathic surgery for different skeletal discrepancies or facial profiles.
5. Conclusions
Soft tissue prediction presented errors that ranged from 0.3 to 1.0 mm for all interventions. The prediction errors in the non-extraction group presented more protrusion of the lower lip than the final actual outcome, while the extraction group presented more protrusion of both the upper and lower lips than the actual outcome. In the orthognathic surgery group, prediction errors were observed in chin thickness, facial contour angle, and in both the upper and lower lip parameters.
Author Contributions
Conceptualization, P.C.; methodology, P.C. and T.N.; software, P.C. and T.N.; validation, P.C. and T.N.; formal analysis, P.C. and T.N.; investigation, P.C. and T.N.; resources, P.C.; data curation, P.C. and T.N.; writing—original draft preparation, P.C. and T.N.; writing—review and editing, P.C. and T.N.; visualization, P.C. and T.N.; supervision, P.C.; project administration, P.C. and T.N.; funding acquisition, P.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Faculty of Dentistry and Prince of Songkla University.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Faculty of Dentistry, Prince of Songkla University. (Protocol EC6502-005, Date of approval 28 February 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
Data are available upon request.
Acknowledgments
We would like to thank Chaithanathat Traiyansiri, Ketkarn Limprasertsiri, and Ployngam Cheevarungnapakul for their kind assistance.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Sundareswaran, S.; Ramakrishnan, R. The facial aesthetic index: An additional tool for assessing treatment need. J. Orthod. Sci. 2016, 5, 57–63. [Google Scholar] [CrossRef]
- Maetevorakul, S.; Viteporn, S. Factors influencing soft tissue profile changes following orthodontic treatment in patients with Class II division 1 malocclusion. Prog. Orthod. 2016, 17, 13. [Google Scholar] [CrossRef] [PubMed]
- Tng, T.T.H.; Chan, T.C.K.; Hägg, U.; Cooke, M.S. Validity of cephalometric landmarks: An experimental study on human skulls. Eur. J. Orthod. 1994, 16, 110–120. [Google Scholar] [CrossRef]
- Prabhakar, R.; Rajakumar, P.; Karthikeyan, M.K.; Saravanan, R.; Vikram, N.R.; Reddy, A. A hard tissue cephalometric comparative study between hand tracing and computerized tracing. J. Pharm. Bioallied Sci. 2014, 6, S101–S106. [Google Scholar] [CrossRef]
- Farooq, M.U.; Khan, M.A.; Imran, S.; Sameera, A.; Qureshi, A.; Ahmed, S.A.; Kumar, S.; Rahman, M.A.U. Assessing the reliability of digitalized cephalometric analysis in comparison with manual cephalometric analysis. J. Clin. Diagn. Res. 2016, 10, ZC20–ZC23. [Google Scholar] [CrossRef] [PubMed]
- Gossett, C.B.; Preston, C.B.; Dunford, R.; Lampasso, J. Prediction accuracy of computer-assisted surgical visual treatment objectives as compared with conventional visual treatment objectives. J. Oral Maxillofac. Surg. 2005, 63, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Nadjmi, N.; Tehranchi, A.; Azami, N.; Saedi, B.; Mollemans, W. Comparison of soft-tissue profiles in Le Fort I osteotomy patients with Dolphin and Maxilim softwares. Am. J. Orthod. Dentofacial Orthop. 2013, 144, 654–662. [Google Scholar] [CrossRef]
- Peterman, R.J.; Jiang, S.; Johe, R.; Mukherjee, P.M. Accuracy of Dolphin visual treatment objective (VTO) prediction software on class III patients treated with maxillary advancement and mandibular setback. Prog. Orthod. 2016, 17, 19. [Google Scholar] [CrossRef]
- Jacobson, R.; Sarver, D.M. The predictability of maxillary repositioning in LeFort I orthognathic surgery. Am. J. Orthod. Dentofacial Orthop. 2002, 122, 142–154. [Google Scholar] [CrossRef]
- Zhang, X.; Mei, L.; Yan, X.; Wei, J.; Li, Y.; Li, H.; Li, Z.; Zheng, W.; Li, Y. Accuracy of computer-aided prediction in soft tissue changes after orthodontic treatment. Am. J. Orthod. Dentofacial Orthop. 2019, 156, 823–831. [Google Scholar] [CrossRef]
- Pektas, Z.Ö.; Kircelli, B.H.; Cilasun, Ü.; Uckan, S. The accuracy of computer-assisted surgical planning in soft tissue prediction following orthognathic surgery. Int. J. Med. Robot. Comput. Assist. Surg. 2007, 3, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Soheilifar, S.; Soheilifar, S.; Afrasiabi, Z.; Soheilifar, S.; Tapak, L.; Naghdi, N. Prediction accuracy of Dolphin software for soft-tissue profile in Class I patients undergoing fixed orthodontic treatment. J. World. Fed. Orthod. 2022, 11, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.; Mohamed, A.M.A.; He, Y.; Dong, W.; Yaosen, C.; Yang, Y. Extraction vs. nonextraction on soft-tissue profile change in patients with malocclusion: A systematic review and meta-analysis. Biomed Res. Int. 2021, 2021, 7751516. [Google Scholar] [CrossRef] [PubMed]
- Steiner, C.C. The use of cephalometrics as an aid to planning and assessing orthodontic treatment: Report of a case. Am. J. Orthod. 1960, 46, 721–735. [Google Scholar] [CrossRef]
- McNamara, J.A., Jr. A method of cephalometric evaluation. Am. J. Orthod. 1984, 86, 449–469. [Google Scholar] [CrossRef] [PubMed]
- Harvold, E.P.; Vargervik, K. Morphogenetic response to activator treatment. Am. J. Orthod. 1971, 60, 478–490. [Google Scholar] [CrossRef] [PubMed]
- Nuntasukkasame, A.; Suntornlohanakul, S.; Charoemratrote, C. Natural head position: The role in lateral cephalometric analysis. O. J. Thai Assoc. Orthod. 2012, 2, 10–16. [Google Scholar]
- Khan, M.; Fida, M. Soft tissue profile response in extraction versus non-extraction orthodontic treatment. J. Coll. Physicians Surg. Pak. 2010, 20, 454–459. [Google Scholar]
- Oliver, B.M. The influence of lip thickness and strain on upper lip response to incisor retraction. Am. J. Orthod. 1982, 82, 141–149. [Google Scholar] [CrossRef]
- Qadeer, T.A.; Jawaid, M.; Fahim, M.F.; Habib, M.; Khan, E.B. Effect of lip thickness and competency on soft-tissue changes. Am. J. Orthod. Dentofacial Orthop. 2022, 162, 483–490. [Google Scholar] [CrossRef]
- Caplan, M.J.; Shivapuja, P.K. The effect of premolar extractions on the soft-tissue profile in adult African American females. Angle Orthod. 1997, 67, 129–136. [Google Scholar] [PubMed]
- Bishara, S.E.; Cummins, D.M.; Jakobsen, J.R. The morphologic basis for the extraction decision in Class II, division 1 malocclusions: A comparative study. Am. J. Orthod. Dentofacial Orthop. 1995, 107, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Kocadereli, İ. Changes in soft tissue profile after orthodontic treatment with and without extractions. Am. J. Orthod. Dentofacial Orthop. 2002, 122, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Yogosawa, F. Predicting soft tissue profile changes concurrent with orthodontic treatment. Angle Orthod. 1990, 60, 199–206. [Google Scholar] [PubMed]
- Yasutomi, H.; Ioi, H.; Nakata, S.; Nakasima, A.; Counts, A.L. Effects of retraction of anterior teeth on horizontal and vertical lip positions in Japanese adults with the bimaxillary dentoalveolar protrusion. Orthod. Waves 2006, 65, 141–147. [Google Scholar] [CrossRef]
- Soheilifar, S.; Soheilifar, S.; Ataei, H.; Mollabashi, V.; Amini, P.; Bakhshaei, A.; Naghdi, N. Extraction versus non-extraction orthodontic treatment: Soft tissue profile changes in borderline class I patients. Dent. Med. Probl. 2020, 57, 275–283. [Google Scholar] [PubMed]
- Shirvani, A.; Sadeghian, S.; Abbasi, S. Prediction of lip response to orthodontic treatment using a multivariable regression model. Dent. Res. J. 2016, 13, 38–45. [Google Scholar]
- Ahmad Akhoundi, M.S.; Shirani, G.; Arshad, M.; Heidar, H.; Sodagar, A. Comparison of an imaging software and manual prediction of soft tissue changes after orthognathic surgery. J. Dent. 2012, 9, 178–187. [Google Scholar]
- Stella, J.P.; Streater, M.R.; Epker, B.N.; Sinn, D.P. Predictability of upper lip soft tissue changes with maxillary advancement. J. Oral Maxillofac. Surg. 1989, 47, 697–703. [Google Scholar] [CrossRef]
- Karsli, N.; Tuhan Kutlu, E. Effect of body mass index on soft tissues in adolescents with skeletal class I and normal facial height. PeerJ 2023, 11, e16196. [Google Scholar] [CrossRef]
- De Lira, A.d.L.S.; de Moura, W.L.; de Barros Vieira, J.M.; Nojima, M.G.; Nojima, L.I. Surgical prediction of skeletal and soft tissue changes in Class III treatment. J. Oral Maxillofac. Surg. 2012, 70, e290–e297. [Google Scholar] [CrossRef] [PubMed]
- Power, G.; Breckon, J.; Sherriff, M.; McDonald, F. Dolphin Imaging Software: An analysis of the accuracy of cephalometric digitization and orthognathic prediction. Int. J. Oral Maxillofac. Surg. 2005, 34, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Kolokitha, O.-E.; Chatzistavrou, E. Factors influencing the accuracy of cephalometric prediction of soft tissue profile changes following orthognathic surgery. J. Maxillofac. Oral Surg. 2012, 11, 82–90. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).