Low-Cost Pseudo-Anthropomorphic PVA-C and Cellulose Lung Phantom for Ultrasound-Guided Interventions
Abstract
1. Introduction
2. Materials and Methods
3. Results and Discussion
3.1. Ultrasound Characterization
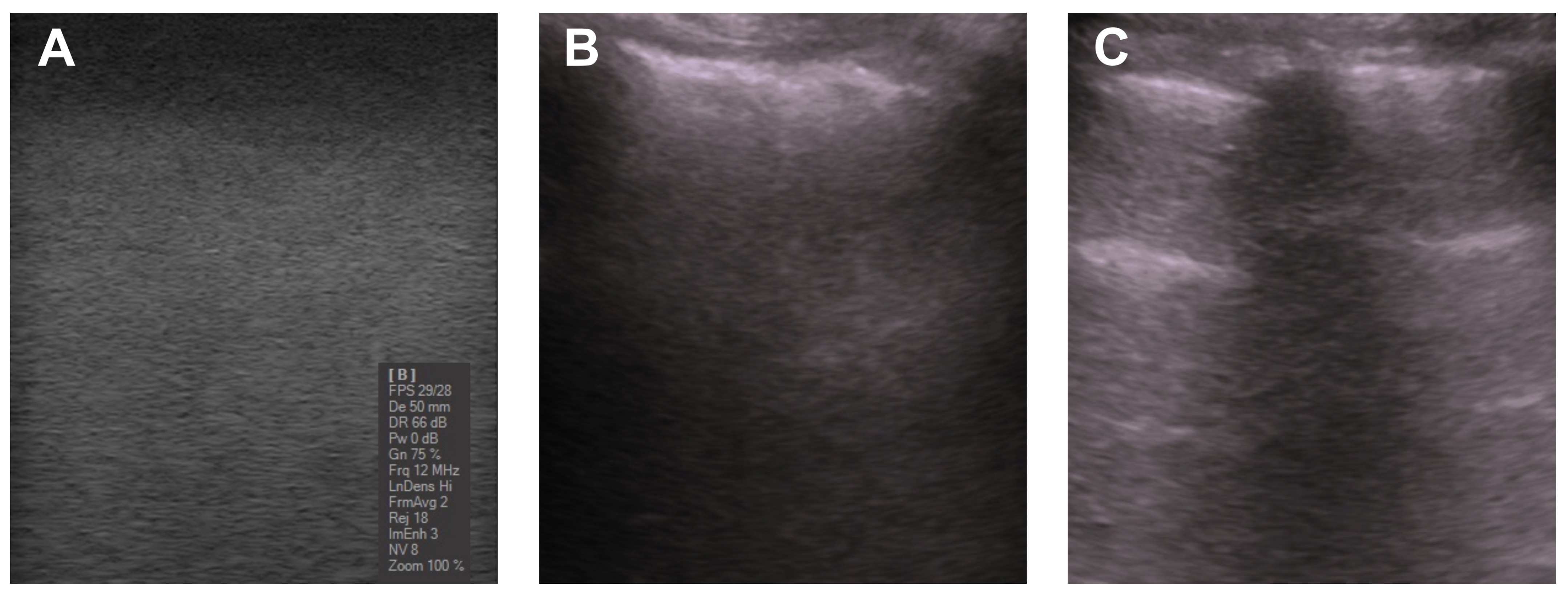
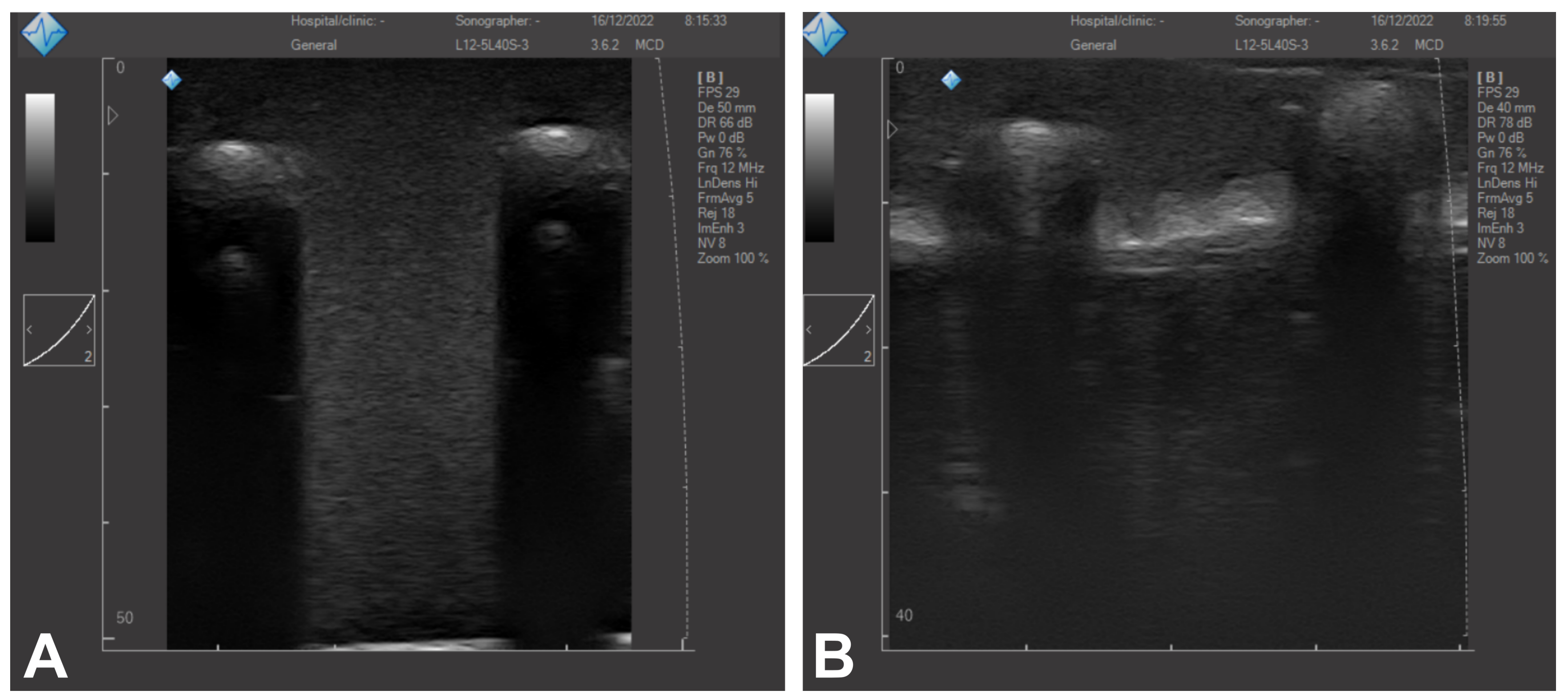
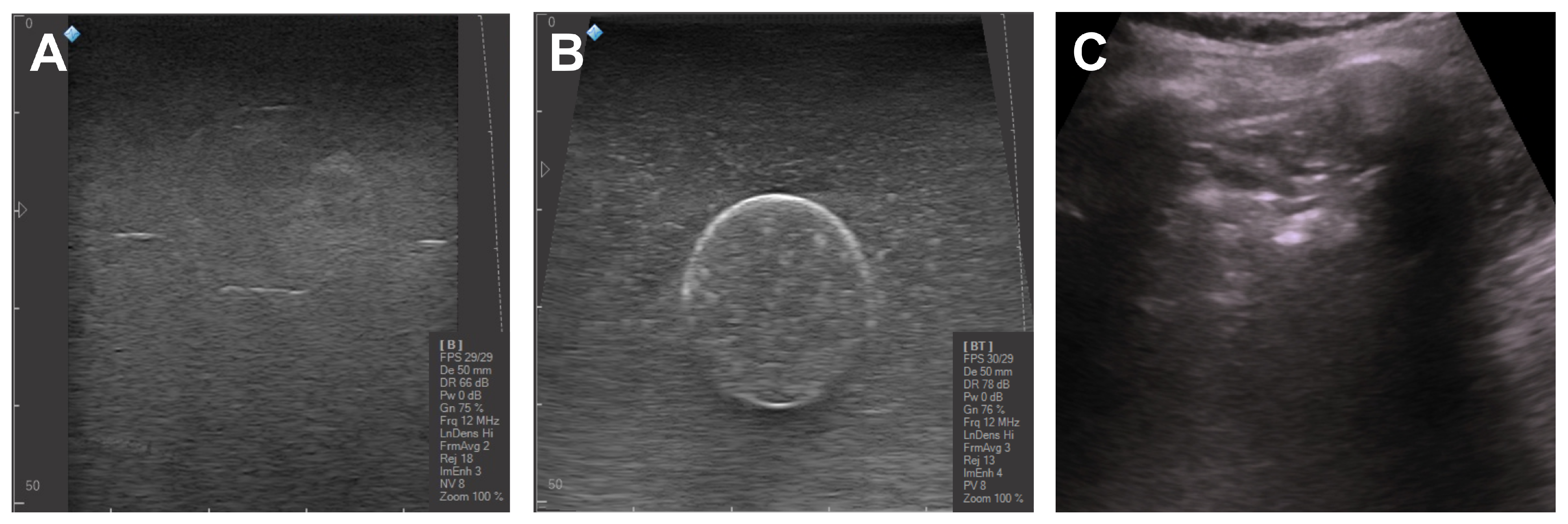
3.2. Ultrasound Imaging
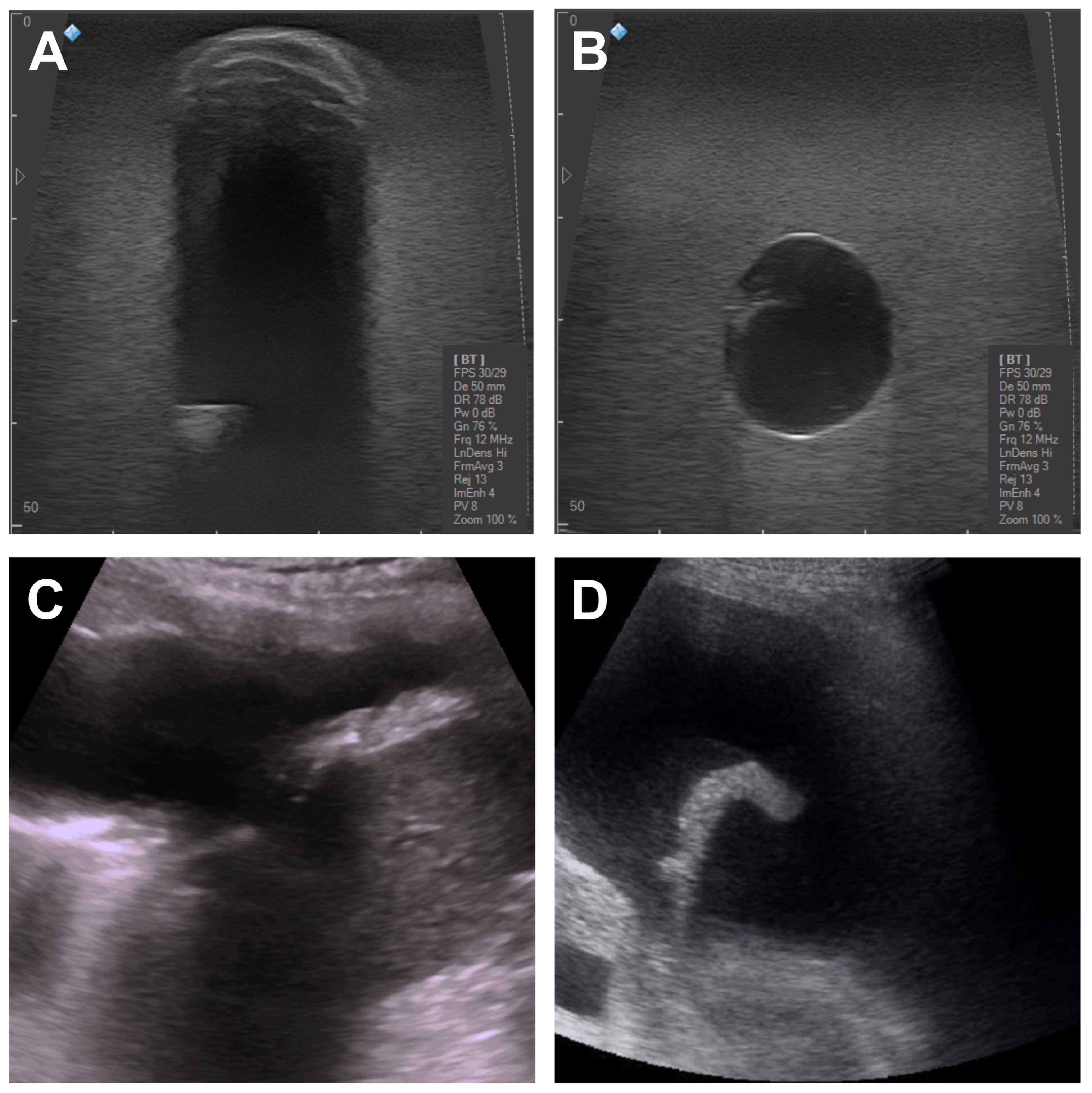
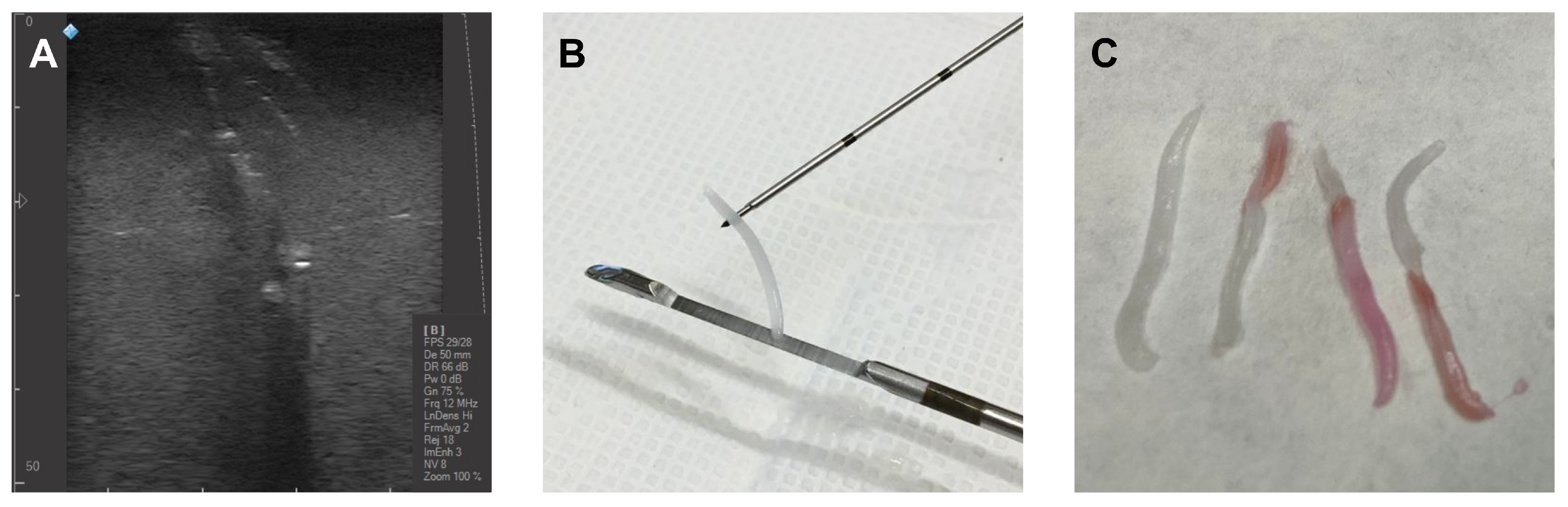
3.3. Invasive Surgical Procedures
3.4. Comparison to Commercial Phantoms
3.5. Comparison to Custom-Made Low-Cost Phantoms
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhou, J.; Zhang, X. A lung phantom model to study pulmonary edema using lung ultrasound surface wave elastography. Ultrasound Med. Biol. 2018, 44, 2400–2405. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Osborn, T.; Zhou, B.; Meixner, D.; Kinnick, R.R.; Bartholmai, B.; Greenleaf, J.F.; Kalra, S. Lung ultrasound surface wave elastography: A pilot clinical study. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2017, 64, 1298–1304. [Google Scholar] [CrossRef] [PubMed]
- Mongodi, S.; Orlando, A.; Arisi, E.; Tavazzi, G.; Santangelo, E.; Caneva, L.; Pozzi, M.; Pariani, E.; Bettini, G.; Maggio, G.; et al. Lung ultrasound in patients with acute respiratory failure reduces conventional imaging and health care provider exposure to COVID-19. Ultrasound Med. Biol. 2020, 46, 2090–2093. [Google Scholar] [CrossRef] [PubMed]
- Nikitichev, D.I.; Barburas, A.; McPherson, K.; Mari, J.M.; West, S.J.; Desjardins, A.E. Construction of 3-dimensional printed ultrasound phantoms with wall-less vessels. J. Ultrasound Med. 2016, 35, 1333–1339. [Google Scholar] [CrossRef]
- Troianos, C.A.; Hartman, G.S.; Glas, K.E.; Skubas, N.J.; Eberhardt, R.T.; Walker, J.D.; Reeves, S.T.; Councils on Intraoperative Echocardiography and Vascular Ultrasound of the American Society of Echocardiography; Society of Cardiovascular Anesthesiologists. Special articles: Guidelines for performing ultrasound guided vascular cannulation: Recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Anesth. Analg. 2012, 114, 46–72. [Google Scholar] [CrossRef]
- Davidson, I.J.; Yoo, M.C.; Biasucci, D.G.; Browne, P.; Dees, C.; Dolmatch, B.; Gallieni, M.; La Greca, A.; Korndorffer, J.R.; Nolen, B.; et al. Simulation training for vascular access interventions. J. Vasc. Access 2010, 11, 181–190. [Google Scholar] [CrossRef]
- Davidson, I.J.; Lok, C.; Dolmatch, B.; Gallieni, M.; Nolen, B.; Pittiruti, M.; Ross, J.; Slakey, D. Virtual reality: Emerging role of simulation training in vascular access. Proc. Semin. Nephrol. 2012, 32, 572–581. [Google Scholar] [CrossRef]
- Evans, L.V.; Dodge, K.L.; Shah, T.D.; Kaplan, L.J.; Siegel, M.D.; Moore, C.L.; Hamann, C.J.; Lin, Z.; D’onofrio, G. Simulation training in central venous catheter insertion: Improved performance in clinical practice. Acad. Med. 2010, 85, 1462–1469. [Google Scholar] [CrossRef]
- Sultan, S.F.; Shorten, G.; Iohom, G. Simulators for training in ultrasound guided procedures. Med. Ultrason. 2013, 15, 125–131. [Google Scholar] [CrossRef]
- Madsen, E.L.; Zagzebski, J.A.; Banjavie, R.A.; Jutila, R.E. Tissue mimicking materials for ultrasound phantoms. Med. Phys. 1978, 5, 391–394. [Google Scholar] [CrossRef]
- Ultrasound CIRS, Inc. Available online: https://www.cirsinc.com/product-category/ultrasound/ (accessed on 15 December 2022).
- CAE Healthcare. Available online: https://www.caehealthcare.com (accessed on 15 December 2022).
- Kyoto Kagaku Co., Ltd. Available online: https://www.kyotokagaku.com/en/ (accessed on 15 December 2022).
- Shin, D.S.; Kang, S.H.; Kim, K.H.; Kim, T.H.; Kim, D.S.; Chung, J.B.; Lucero, S.A.; Suh, T.S.; Yamamoto, T. Development of a deformable lung phantom with 3D-printed flexible airways. Med. Phys. 2020, 47, 898–908. [Google Scholar] [CrossRef] [PubMed]
- Nioutsikou, E.; Symonds-Tayler, J.R.N.; Bedford, J.L.; Webb, S. Quantifying the effect of respiratory motion on lung tumour dosimetry with the aid of a breathing phantom with deforming lungs. Phys. Med. Biol. 2006, 51, 3359. [Google Scholar] [CrossRef] [PubMed]
- Serban, M.; Heath, E.; Stroian, G.; Collins, D.L.; Seuntjens, J. A deformable phantom for 4D radiotherapy verification: Design and image registration evaluation. Med. Phys. 2008, 35, 1094–1102. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.; Suh, T.S.; Lee, D.S. Development of a deformable lung phantom for the evaluation of deformable registration. J. Appl. Clin. Med. Phys. 2010, 11, 281–286. [Google Scholar] [CrossRef]
- Hong, D.; Lee, S.; Kim, G.B.; Lee, S.M.; Kim, N.; Seo, J.B. Development of a CT imaging phantom of anthromorphic lung using fused deposition modeling 3D printing. Medicine 2020, 99, e18617. [Google Scholar] [CrossRef]
- Gholampourkashi, S.; Cygler, J.E.; Lavigne, B.; Heath, E. Development of a deformable phantom for experimental verification of 4D Monte Carlo simulations in a deforming anatomy. Phys. Med. 2018, 51, 81–90. [Google Scholar] [CrossRef]
- Mirbeik-Sabzevari, A.; Tavassolian, N. Ultrawideband, stable normal and cancer skin tissue phantoms for millimeter-wave skin cancer imaging. IEEE Trans. Biomed. Eng. 2018, 66, 176–186. [Google Scholar] [CrossRef]
- Filippou, V.; Tsoumpas, C. Recent advances on the development of phantoms using 3D printing for imaging with CT, MRI, PET, SPECT, and ultrasound. Med. Phys. 2018, 45, e740–e760. [Google Scholar] [CrossRef]
- Maneas, E.; Xia, W.; Nikitichev, D.I.; Daher, B.; Manimaran, M.; Wong, R.Y.J.; Chang, C.W.; Rahmani, B.; Capelli, C.; Schievano, S.; et al. Anatomically realistic ultrasound phantoms using gel wax with 3D printed moulds. Phys. Med. Biol. 2018, 63, 015033. [Google Scholar] [CrossRef]
- Pacioni, A.; Carbone, M.; Freschi, C.; Viglialoro, R.; Ferrari, V.; Ferrari, M. Patient-specific ultrasound liver phantom: Materials and fabrication method. Int. J. Comput. Assist. Radiol. Surg. 2015, 10, 1065–1075. [Google Scholar] [CrossRef]
- Blüthgen, C.; Sanabria, S.; Frauenfelder, T.; Klingmüller, V.; Rominger, M. Economical sponge phantom for teaching, understanding, and researching A-and B-line reverberation artifacts in lung ultrasound. J. Ultrasound Med. 2017, 36, 2133–2142. [Google Scholar] [CrossRef]
- Molinari, F.; Madhuranthakam, A.J.; Lenkinski, R.; Bankier, A.A. Ultrashort echo time MRI of pulmonary water content: Assessment in a sponge phantom at 1.5 and 3.0 Tesla. Diagn. Interv. Radiol. 2014, 20, 34. [Google Scholar] [CrossRef] [PubMed]
- Laing, J.; Moore, J.T.; Vassallo, R.; Bainbridge, D.; Drangova, M.; Peters, T.M. Patient-specific cardiac phantom for clinical training and preprocedure surgical planning. J. Med. Imaging 2018, 5, 021222. [Google Scholar] [CrossRef] [PubMed]
- Alves, N.; Kim, A.; Tan, J.; Hwang, G.; Javed, T.; Neagu, B.; Courtney, B.K. Cardiac tissue-mimicking ballistic gel phantom for ultrasound imaging in clinical and research applications. Ultrasound Med. Biol. 2020, 46, 2057–2069. [Google Scholar] [CrossRef]
- Selame, L.A.; Risler, Z.; Zakaria, S.J.; Hughes, L.P.; Lewiss, R.E.; Kehm, K.; Goodsell, K.; Kalwani, R.; Mirsch, D.; Kluger, S.B.; et al. A comparison of homemade vascular access ultrasound phantom models for peripheral intravenous catheter insertion. J. Vasc. Access 2021, 22, 891–897. [Google Scholar] [CrossRef]
- Adams, F.; Qiu, T.; Mark, A.; Fritz, B.; Kramer, L.; Schlager, D.; Wetterauer, U.; Miernik, A.; Fischer, P. Soft 3D-printed phantom of the human kidney with collecting system. Ann. Biomed. Eng. 2017, 45, 963–972. [Google Scholar] [CrossRef]
- Suga, M.; Usumura, M.; Kishimoto, R.; Mizoguchi, T.; Yamaguchi, T.; Obata, T. Development of a viscoelastic phantom for ultrasound and MR elastography satisfying the QIBA acoustic specifications. In Proceedings of the 2020 IEEE International Ultrasonics Symposium (IUS), Las Vegas, NV, USA, 7–11 September 2020; pp. 1–3. [Google Scholar]
- Fromageau, J.; Gennisson, J.L.; Schmitt, C.; Maurice, R.L.; Mongrain, R.; Cloutier, G. Estimation of polyvinyl alcohol cryogel mechanical properties with four ultrasound elastography methods and comparison with gold standard testings. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2007, 54, 498–509. [Google Scholar] [CrossRef] [PubMed]
- Elvira, L.; Durán, C.; Higuti, R.T.; Tiago, M.M.; Ibáñez, A.; Parrilla, M.; Valverde, E.; Jiménez, J.; Bassat, Q. Development and characterization of medical phantoms for ultrasound imaging based on customizable and mouldable polyvinyl alcohol Cryogel–Based materials and 3-D printing: Application to high-frequency cranial ultrasonography in infants. Ultrasound Med. Biol. 2019, 45, 2226–2241. [Google Scholar] [CrossRef]
- Surry, K.; Austin, H.; Fenster, A.; Peters, T. Poly (vinyl alcohol) cryogel phantoms for use in ultrasound and MR imaging. Phys. Med. Biol. 2004, 49, 5529. [Google Scholar] [CrossRef]
- Wan, W.; Bannerman, A.D.; Yang, L.; Mak, H. Poly (vinyl alcohol) cryogels for biomedical applications. Polym. Cryogels 2014, 263, 283–321. [Google Scholar]
- Villa, E.; Arteaga-Marrero, N.; González-Fernández, J.; Ruiz-Alzola, J. Bimodal microwave and ultrasound phantoms for non-invasive clinical imaging. Sci. Rep. 2020, 10, 20401. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Li, G.Y.; Zhang, X.; Liu, Y.L. Tissue-mimicking materials for elastography phantoms: A review. Extrem. Mech. Lett. 2017, 17, 62–70. [Google Scholar] [CrossRef]
- Chen, A.I.; Balter, M.L.; Chen, M.I.; Gross, D.; Alam, S.K.; Maguire, T.J.; Yarmush, M.L. Multilayered tissue mimicking skin and vessel phantoms with tunable mechanical, optical, and acoustic properties. Med. Phys. 2016, 43, 3117–3131. [Google Scholar] [CrossRef] [PubMed]
- Culjat, M.O.; Goldenberg, D.; Tewari, P.; Singh, R.S. A review of tissue substitutes for ultrasound imaging. Ultrasound Med. Biol. 2010, 36, 861–873. [Google Scholar] [CrossRef] [PubMed]
- King, D.M.; Hangiandreou, N.J.; Tradup, D.J.; Stekel, S.F. Evaluation of a low-cost liquid ultrasound test object for detection of transducer artefacts. Phys. Med. Biol. 2010, 55, N557. [Google Scholar] [CrossRef] [PubMed]
- Bhaladhare, S.; Das, D. Cellulose: A fascinating biopolymer for hydrogel synthesis. J. Mater. Chem. B 2022, 10, 1923–1945. [Google Scholar] [CrossRef]
- Liu, Y.; Ahmed, S.; Sameen, D.E.; Wang, Y.; Lu, R.; Dai, J.; Li, S.; Qin, W. A review of cellulose and its derivatives in biopolymer-based for food packaging application. Trends Food Sci. Technol. 2021, 112, 532–546. [Google Scholar] [CrossRef]
- Arteaga-Marrero, N.; Villa, E.; González-Fernández, J.; Martín, Y.; Ruiz-Alzola, J. Polyvinyl alcohol cryogel phantoms of biological tissues for wideband operation at microwave frequencies. PLoS ONE 2019, 14, e0219997. [Google Scholar] [CrossRef]
- Clegg, A.J. Precision Casting Processes; Pergamon Press: Oxford, UK, 1991. [Google Scholar]
- Cook, J.R.; Bouchard, R.R.; Emelianov, S.Y. Tissue-mimicking phantoms for photoacoustic and ultrasonic imaging. Biomed. Opt. Express 2011, 2, 3193–3206. [Google Scholar] [CrossRef]
- Zell, K.; Sperl, J.I.; Vogel, M.W.; Niessner, R.; Haisch, C. Acoustical properties of selected tissue phantom materials for ultrasound imaging. Phys. Med. Biol. 2007, 52, N475. [Google Scholar] [CrossRef]
- Sachse, W.; Pao, Y.H. On the determination of phase and group velocities of dispersive waves in solids. J. Appl. Phys. 1978, 49, 4320–4327. [Google Scholar] [CrossRef]
- Wang, H.; Cao, W. Improved ultrasonic spectroscopy methods for characterization of dispersive materials. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2001, 48, 1060–1065. [Google Scholar] [CrossRef] [PubMed]
- Marsh, J.N.; Hall, C.S.; Hughes, M.S.; Mobley, J.; Miller, J.G.; Brandenburger, G.H. Broadband through-transmission signal loss measurements of Albunex® suspensions at concentrations approaching in vivo doses. J. Acoust. Soc. Am. 1997, 101, 1155–1161. [Google Scholar] [CrossRef]
- Kharine, A.; Manohar, S.; Seeton, R.; Kolkman, R.G.; Bolt, R.A.; Steenbergen, W.; de Mul, F.F. Poly (vinyl alcohol) gels for use as tissue phantoms in photoacoustic mammography. Phys. Med. Biol. 2003, 48, 357. [Google Scholar] [CrossRef] [PubMed]
- Born, J.; Wiedemann, N.; Cossio, M.; Buhre, C.; Brändle, G.; Leidermann, K.; Goulet, J.; Aujayeb, A.; Moor, M.; Rieck, B.; et al. Accelerating detection of lung pathologies with explainable ultrasound image analysis. Appl. Sci. 2021, 11, 672. [Google Scholar] [CrossRef]
- Automatic Detection of COVID-19 from Ultrasound Data. Available online: https://github.com/BorgwardtLab/covid19_ultrasound (accessed on 24 October 2022).
- Liu, J.; Chen, S.W.; Liu, F.; Wang, Y.; Kong, X.Y.; Li, Q.P.; Huang, J.J. BPD, not BPD, or iatrogenic BPD: Findings of lung ultrasound examinations. Medicine 2014, 93, e133. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Yang, W.; Zhang, H.; Xu, Q.; Yan, K. The role of contrast-enhanced ultrasound in selection indication and improveing diagnosis for transthoracic biopsy in peripheral pulmonary and mediastinal lesions. BioMed Res. Int. 2015, 2015, 231782. [Google Scholar] [CrossRef]
- Karabinis, A.; Saranteas, T.; Karakitsos, D.; Lichtenstein, D.; Poularas, J.; Yang, C.; Stefanadis, C. The ’cardiac-lung mass’ artifact: An echocardiographic sign of lung atelectasis and/or pleural effusion. Crit. Care 2008, 12, R122. [Google Scholar] [CrossRef]
- Brogi, E.; Gargani, L.; Bignami, E.; Barbariol, F.; Marra, A.; Forfori, F.; Vetrugno, L. Thoracic ultrasound for pleural effusion in the intensive care unit: A narrative review from diagnosis to treatment. Crit. Care 2017, 21, 325. [Google Scholar] [CrossRef]
- Efremov, S.M.; Kuzkov, V.V.; Fot, E.V.; Kirov, M.Y.; Ponomarev, D.N.; Lakhin, R.E.; Kokarev, E.A. Lung ultrasonography and cardiac surgery: A narrative review. J. Cardiothorac. Vasc. Anesth. 2020, 34, 3113–3124. [Google Scholar] [CrossRef]
- Rippey, J.; Gawthrope, I. Creating thoracic phantoms for diagnostic and procedural ultrasound training. Australas. J. Ultrasound Med. 2012, 15, 43–54. [Google Scholar] [CrossRef] [PubMed]
- CAE Blue Phantom (Vascular Access). Available online: https://medicalskillstrainers.cae.com/139/vascular-access?initialMap=139&initialQuery=139&map=productClusterIds,specialty (accessed on 15 December 2022).
- Image-Guided Abdominal Biopsy Phantom. Available online: http://www.cirsinc.com/wp-content/uploads/2019/04/071B-DS-120418.pdf (accessed on 24 October 2022).
- Lumbar Puncture Simulator IIA. Available online: https://www.kyotokagaku.com/en/products_data/m43b_en/ (accessed on 15 December 2022).
- Ultrasound Examination Training Phantom “ABDFAN”. Available online: https://www.kyotokagaku.com/products_data/us1b_catalog_en.pdf (accessed on 24 October 2022).
- Kendall, J.L.; Faragher, J.P. Ultrasound-guided central venous access: A homemade phantom for simulation. Can. J. Emerg. Med. 2007, 9, 371–373. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, R.; Crofton, M. Training phantom for ultrasound guided biopsy. Br. J. Radiol. 1997, 70, 192–194. [Google Scholar] [CrossRef]
- Amato, A.C.M.; Freitas, S.L.D.; Veloso, P.M.; Correia, T.C.V.; Santos, R.V.D.; Amato, S.J.D.T.A. Gelatin model for training ultrasound-guided puncture. J. Vasc. Bras. 2015, 14, 200–204. [Google Scholar] [CrossRef]
- Sanchez-de Toledo, J.; Villaverde, I. Advanced low-cost ultrasound-guided vascular access simulation: The chicken breast model. Pediatr. Emerg. Care 2017, 33, e43–e45. [Google Scholar] [CrossRef]
- Rippey, J.C.; Blanco, P.; Carr, P.J. An affordable and easily constructed model for training in ultrasound-guided vascular access. J. Vasc. Access 2015, 16, 422–427. [Google Scholar] [CrossRef]
- Fredfeldt, K. An easily made ultrasound biopsy phantom. J. Ultrasound Med. 1986, 5, 295–297. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arteaga-Marrero, N.; Villa, E.; Llanos González, A.B.; Gómez Gil, M.E.; Fernández, O.A.; Ruiz-Alzola, J.; González-Fernández, J. Low-Cost Pseudo-Anthropomorphic PVA-C and Cellulose Lung Phantom for Ultrasound-Guided Interventions. Gels 2023, 9, 74. https://doi.org/10.3390/gels9020074
Arteaga-Marrero N, Villa E, Llanos González AB, Gómez Gil ME, Fernández OA, Ruiz-Alzola J, González-Fernández J. Low-Cost Pseudo-Anthropomorphic PVA-C and Cellulose Lung Phantom for Ultrasound-Guided Interventions. Gels. 2023; 9(2):74. https://doi.org/10.3390/gels9020074
Chicago/Turabian StyleArteaga-Marrero, Natalia, Enrique Villa, Ana Belén Llanos González, Marta Elena Gómez Gil, Orlando Acosta Fernández, Juan Ruiz-Alzola, and Javier González-Fernández. 2023. "Low-Cost Pseudo-Anthropomorphic PVA-C and Cellulose Lung Phantom for Ultrasound-Guided Interventions" Gels 9, no. 2: 74. https://doi.org/10.3390/gels9020074
APA StyleArteaga-Marrero, N., Villa, E., Llanos González, A. B., Gómez Gil, M. E., Fernández, O. A., Ruiz-Alzola, J., & González-Fernández, J. (2023). Low-Cost Pseudo-Anthropomorphic PVA-C and Cellulose Lung Phantom for Ultrasound-Guided Interventions. Gels, 9(2), 74. https://doi.org/10.3390/gels9020074





