A Systematic Review on Organ-on-a-Chip in PDMS or Hydrogel in Dentistry: An Update of the Literature
Abstract
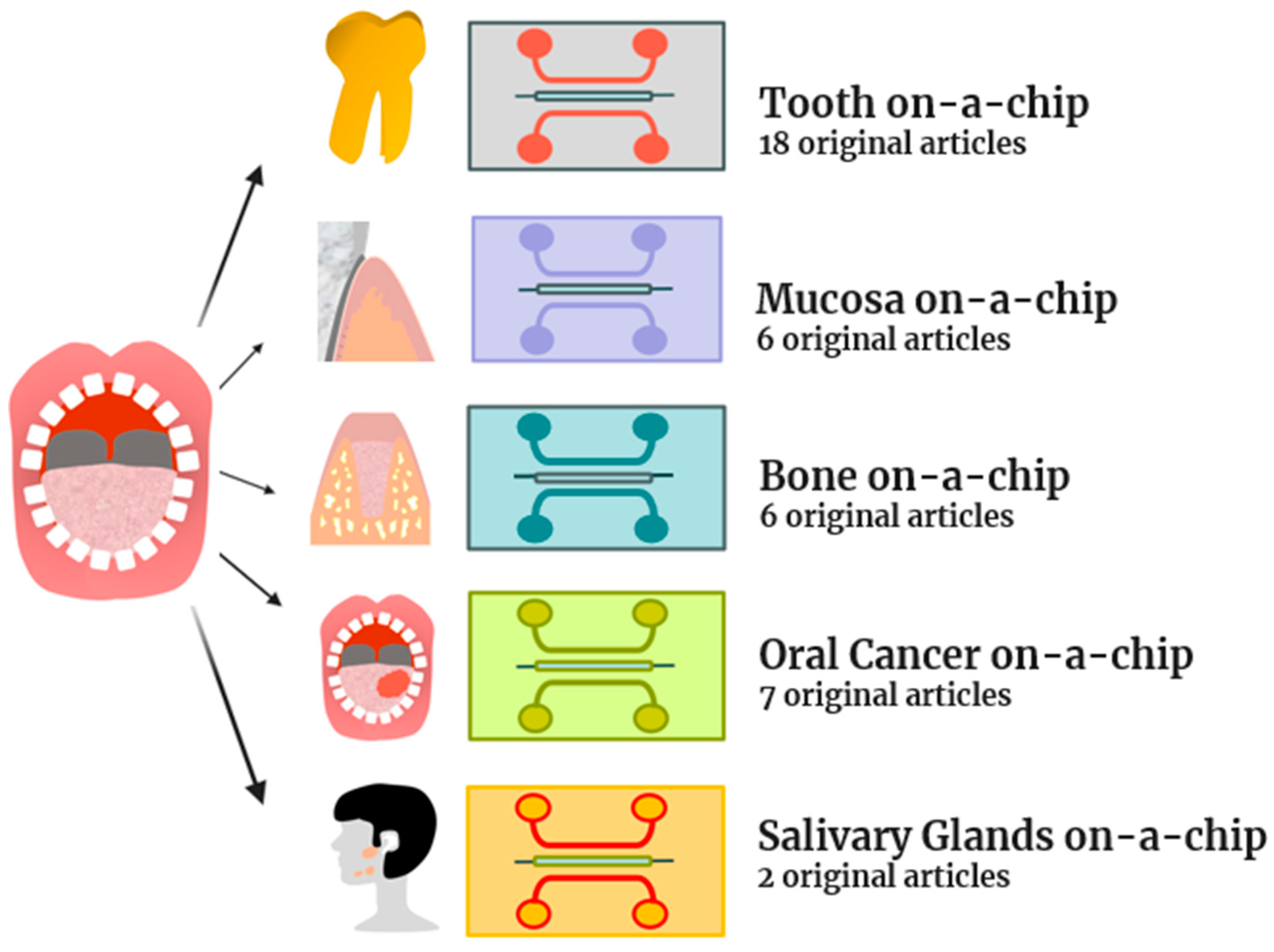
1. Introduction
2. Results and Discussion
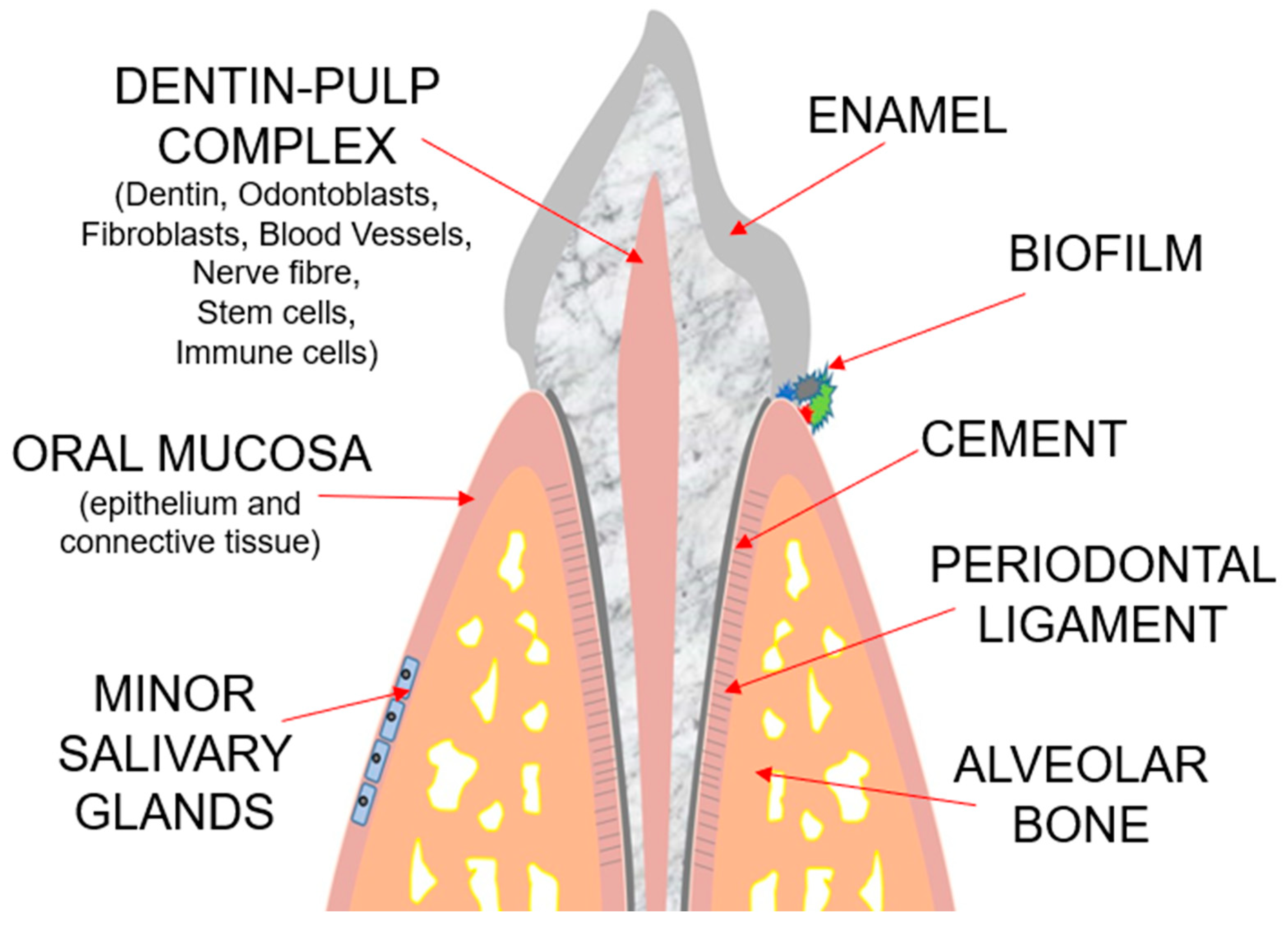
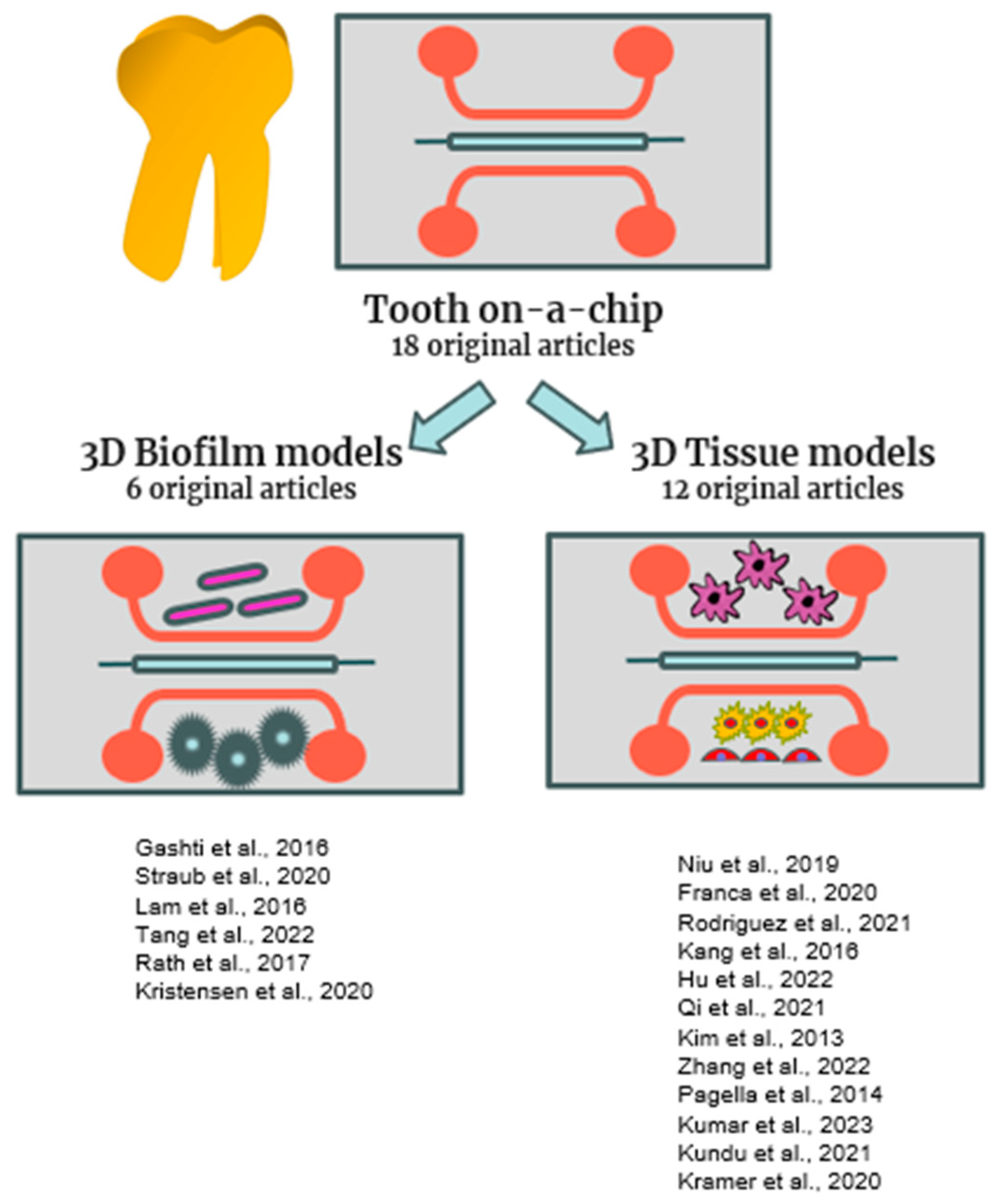
2.1. Tooth-on-a-Chip
2.1.1. Tooth-on-a-Chip Designs and Materials
2.1.2. Tooth-on-a-Chip 3D Tissue Models
2.1.3. Tooth-on-a-Chip 3D Biofilm Models
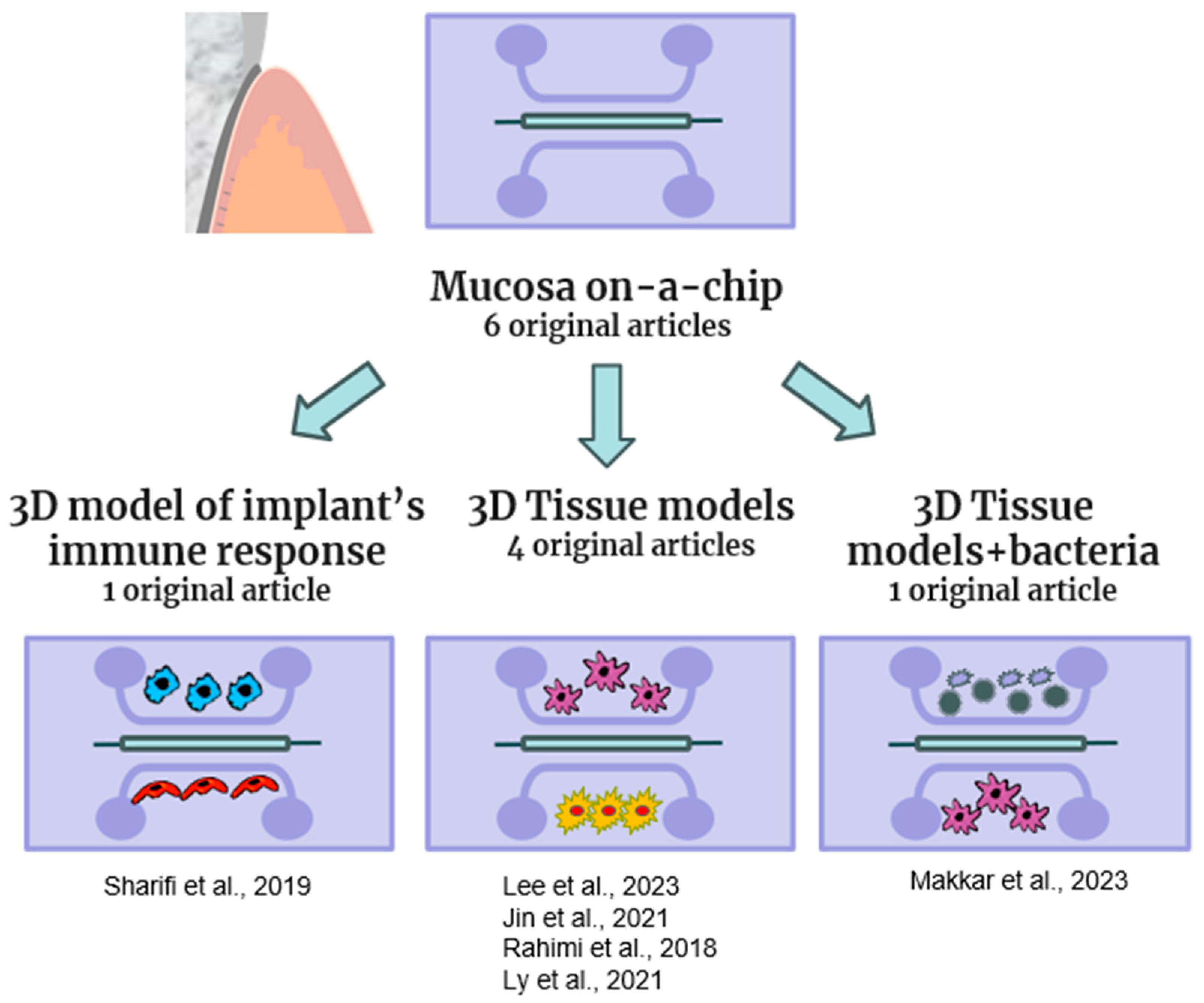
2.2. Mucosa-on-a-Chip
2.3. Bone-on-a-Chip
2.4. Oral Cancer-on-a-Chip
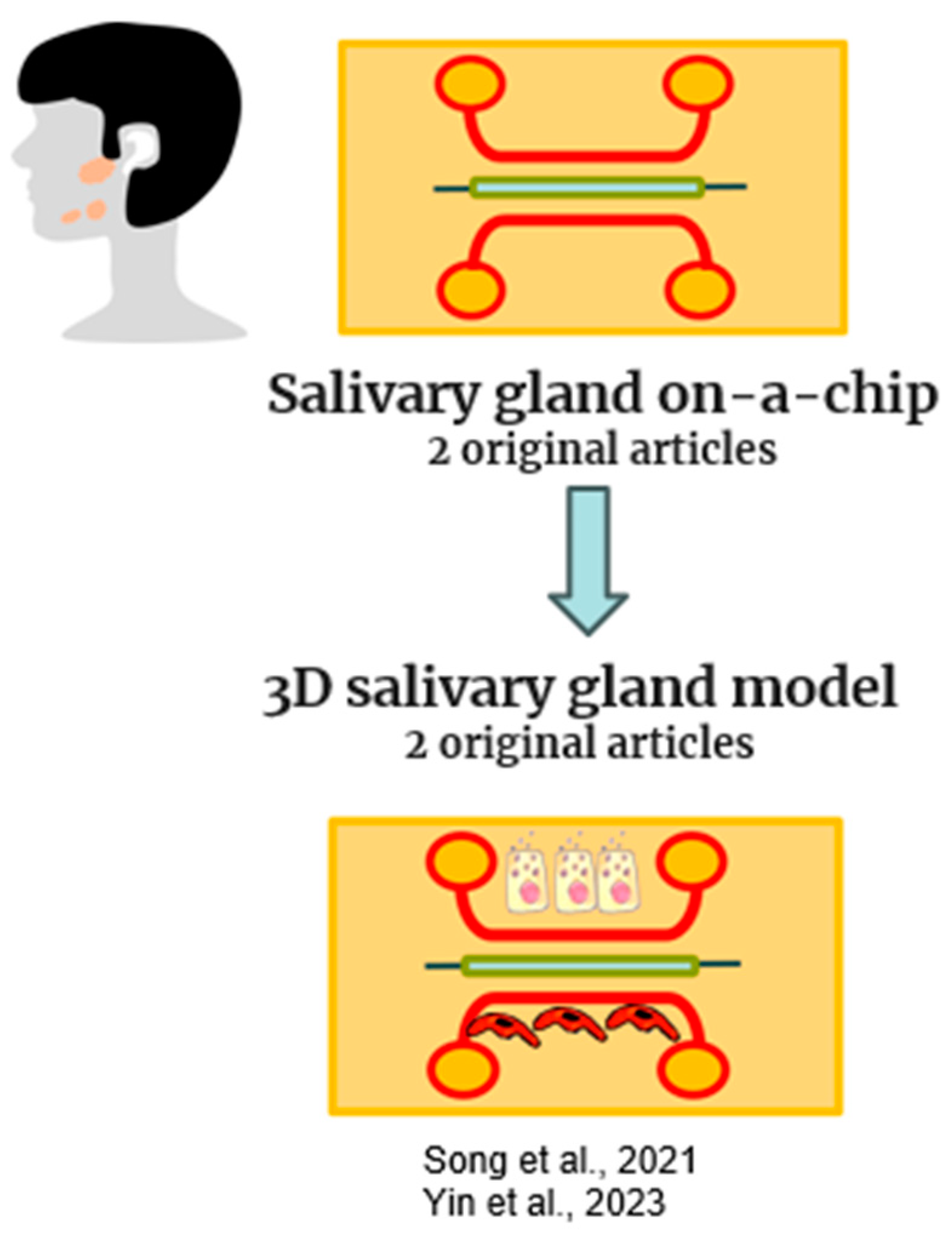
2.5. Salivary Glands-on-a-Chip
2.6. Future Trends
3. Conclusions
4. Materials and Methods
4.1. Inclusion Criteria
- Why are OoCs potentially important for dental clinical practice?
- What are the OoCs’ current and future applications in dentistry?
4.2. Selection of the Manuscripts
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kapałczyńska, M.; Kolenda, T.; Przybyła, W.; Zajączkowska, M.; Teresiak, A.; Filas, V.; Ibbs, M.; Bliźniak, R.; Łuczewski, Ł.; Lamperska, K. 2D and 3D Cell Cultures—A Comparison of Different Types of Cancer Cell Cultures. Arch. Med. Sci. 2016, 14, 910–919. [Google Scholar] [CrossRef]
- Ehlers, H.; Nicolas, A.; Schavemaker, F.; Heijmans, J.P.M.; Bulst, M.; Trietsch, S.J.; van den Broek, L.J. Vascular Inflammation on a Chip: A Scalable Platform for Trans-Endothelial Electrical Resistance and Immune Cell Migration. Front. Immunol. 2023, 14, 1118624. [Google Scholar] [CrossRef]
- Dudás, J.; Ladányi, A.; Ingruber, J.; Steinbichler, T.B.; Riechelmann, H. Epithelial to Mesenchymal Transition: A Mechanism That Fuels Cancer Radio/Chemoresistance. Cells 2020, 9, 428. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Zhang, Z.; Zhou, C.; Liu, L.; Huang, C. Epithelial–Mesenchymal Transition: The History, Regulatory Mechanism, and Cancer Therapeutic Opportunities. MedComm 2022, 3, e144. [Google Scholar] [CrossRef]
- Si, L.; Bai, H.; Rodas, M.; Cao, W.; Oh, C.Y.; Jiang, A.; Moller, R.; Hoagland, D.; Oishi, K.; Horiuchi, S.; et al. A Human-Airway-on-a-Chip for the Rapid Identification of Candidate Antiviral Therapeutics and Prophylactics. Nat. Biomed. Eng. 2021, 5, 815–829. [Google Scholar] [CrossRef] [PubMed]
- Benam, K.H.; Villenave, R.; Lucchesi, C.; Varone, A.; Hubeau, C.; Lee, H.-H.; Alves, S.E.; Salmon, M.; Ferrante, T.C.; Weaver, J.C.; et al. Small Airway-on-a-Chip Enables Analysis of Human Lung Inflammation and Drug Responses in Vitro. Nat. Methods 2016, 13, 151–157. [Google Scholar] [CrossRef]
- Bai, H.; Si, L.; Jiang, A.; Belgur, C.; Zhai, Y.; Plebani, R.; Oh, C.Y.; Rodas, M.; Patil, A.; Nurani, A.; et al. Mechanical Control of Innate Immune Responses against Viral Infection Revealed in a Human Lung Alveolus Chip. Nat. Commun. 2022, 13, 1928. [Google Scholar] [CrossRef]
- Kasendra, M.; Tovaglieri, A.; Sontheimer-Phelps, A.; Jalili-Firoozinezhad, S.; Bein, A.; Chalkiadaki, A.; Scholl, W.; Zhang, C.; Rickner, H.; Richmond, C.A.; et al. Development of a Primary Human Small Intestine-on-a-Chip Using Biopsy-Derived Organoids. Sci. Rep. 2018, 8, 2871. [Google Scholar] [CrossRef]
- Goyal, G.; Prabhala, P.; Mahajan, G.; Bausk, B.; Gilboa, T.; Xie, L.; Zhai, Y.; Lazarovits, R.; Mansour, A.; Kim, M.S.; et al. Ectopic Lymphoid Follicle Formation and Human Seasonal Influenza Vaccination Responses Recapitulated in an Organ-on-a-Chip. Adv. Sci. 2022, 9, e2103241. [Google Scholar] [CrossRef] [PubMed]
- Ewart, L.; Apostolou, A.; Briggs, S.A.; Carman, C.V.; Chaff, J.T.; Heng, A.R.; Jadalannagari, S.; Janardhanan, J.; Jang, K.-J.; Joshipura, S.R.; et al. Performance Assessment and Economic Analysis of a Human Liver-Chip for Predictive Toxicology. Commun. Med. 2022, 2, 154. [Google Scholar] [CrossRef]
- Mahajan, G.; Doherty, E.; To, T.; Sutherland, A.; Grant, J.; Junaid, A.; Gulati, A.; LoGrande, N.; Izadifar, Z.; Timilsina, S.S.; et al. Vaginal Microbiome-Host Interactions Modeled in a Human Vagina-on-a-Chip. Microbiome 2022, 10, 201. [Google Scholar] [CrossRef]
- Plebani, R.; Potla, R.; Soong, M.; Bai, H.; Izadifar, Z.; Jiang, A.; Travis, R.N.; Belgur, C.; Dinis, A.; Cartwright, M.J.; et al. Modeling Pulmonary Cystic Fibrosis in a Human Lung Airway-on-a-Chip. J. Cyst. Fibros. 2022, 21, 606–615. [Google Scholar] [CrossRef] [PubMed]
- Bein, A.; Fadel, C.W.; Swenor, B.; Cao, W.; Powers, R.K.; Camacho, D.M.; Naziripour, A.; Parsons, A.; LoGrande, N.; Sharma, S.; et al. Nutritional Deficiency in an Intestine-on-a-Chip Recapitulates Injury Hallmarks Associated with Environmental Enteric Dysfunction. Nat. Biomed. Eng. 2022, 6, 1236–1247. [Google Scholar] [CrossRef] [PubMed]
- Hassell, J.M.; Begon, M.; Ward, M.J.; Fèvre, E.M. Urbanization and Disease Emergence: Dynamics at the Wildlife–Livestock–Human Interface. Trends Ecol. Evol. 2017, 32, 55–67. [Google Scholar] [CrossRef]
- Kang, K.-J.; Ju, S.M.; Jang, Y.-J.; Kim, J. Indirect Co-Culture of Stem Cells from Human Exfoliated Deciduous Teeth and Oral Cells in a Microfluidic Platform. Tissue Eng. Regen. Med. 2016, 13, 428–436. [Google Scholar] [CrossRef]
- Lam, R.H.W.; Cui, X.; Guo, W.; Thorsen, T. High-Throughput Dental Biofilm Growth Analysis for Multiparametric Microenvironmental Biochemical Conditions Using Microfluidics. Lab. Chip 2016, 16, 1652–1662. [Google Scholar] [CrossRef]
- Gashti, M.P.; Asselin, J.; Barbeau, J.; Boudreau, D.; Greener, J. A Microfluidic Platform with PH Imaging for Chemical and Hydrodynamic Stimulation of Intact Oral Biofilms. Lab. Chip 2016, 16, 1412–1419. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y.; Vázquez-Rosado, E.J.; Wu, D.; Viswananthan, V.; Farach, A.; Farach-Carson, M.C.; Harrington, D.A. Microfluidic Coaxial 3D Bioprinting of Cell-Laden Microfibers and Microtubes for Salivary Gland Tissue Engineering. Biomater. Adv. 2023, 154, 213588. [Google Scholar] [CrossRef]
- Makkar, H.; Zhou, Y.; Tan, K.S.; Lim, C.T.; Sriram, G. Modeling Crevicular Fluid Flow and Host-Oral Microbiome Interactions in a Gingival Crevice-on-Chip. Adv. Healthc. Mater. 2023, 12, e2202376. [Google Scholar] [CrossRef]
- Liu, L.; Xie, Z.; Zhang, W.; Fang, S.; Kong, J.; Jin, D.; Li, J.; Li, X.; Yang, X.; Luo, Y.; et al. Biomimetic Tumor-Induced Angiogenesis and Anti-Angiogenic Therapy in a Microfluidic Model. RSC Adv. 2016, 6, 35248–35256. [Google Scholar] [CrossRef]
- Rath, H.; Stumpp, S.N.; Stiesch, M. Development of a Flow Chamber System for the Reproducible in Vitro Analysis of Biofilm Formation on Implant Materials. PLoS ONE 2017, 12, e0172095. [Google Scholar] [CrossRef]
- Jalali, F.; Ellett, F.; Balani, P.; Duncan, M.J.; Dewhirst, F.E.; Borisy, G.G.; Irimia, D. No Man’s Land: Species-specific Formation of Exclusion Zones Bordering Actinomyces Graevenitzii Microcolonies in Nanoliter Cultures. Microbiologyopen 2021, 10, e1137. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, C.; Rahimi, B.; Padova, D.; Rooholghodos, S.A.; Bienek, D.R.; Luo, X.; Kaufman, G.; Raub, C.B. Oral Mucosa-on-a-Chip to Assess Layer-Specific Responses to Bacteria and Dental Materials. Biomicrofluidics 2018, 12, 054106. [Google Scholar] [CrossRef] [PubMed]
- Koning, J.J.; Rodrigues Neves, C.T.; Schimek, K.; Thon, M.; Spiekstra, S.W.; Waaijman, T.; de Gruijl, T.D.; Gibbs, S. A Multi-Organ-on-Chip Approach to Investigate How Oral Exposure to Metals Can Cause Systemic Toxicity Leading to Langerhans Cell Activation in Skin. Front. Toxicol. 2022, 3, 82482. [Google Scholar] [CrossRef] [PubMed]
- Tiozzo-Lyon, P.; Andrade, M.; Leiva-Sabadini, C.; Morales, J.; Olivares, A.; Ravasio, A.; Aguayo, S. Microfabrication Approaches for Oral Research and Clinical Dentistry. Front. Dent. Med. 2023, 4, 1120394. [Google Scholar] [CrossRef]
- Morris, A.L.; Tadi, P. Anatomy, Head and Neck, Teeth; StatPearls Publishing: St. Petersburg, FL, USA, 2023. [Google Scholar]
- Li, J.; Parada, C.; Chai, Y. Cellular and Molecular Mechanisms of Tooth Root Development. Development 2017, 144, 374–384. [Google Scholar] [CrossRef]
- Straub, H.; Eberl, L.; Zinn, M.; Rossi, R.M.; Maniura-Weber, K.; Ren, Q. A Microfluidic Platform for in Situ Investigation of Biofilm Formation and Its Treatment under Controlled Conditions. J. Nanobiotechnology 2020, 18, 166. [Google Scholar] [CrossRef] [PubMed]
- Tang, P.-C.; Eriksson, O.; Sjögren, J.; Fatsis-Kavalopoulos, N.; Kreuger, J.; Andersson, D.I. A Microfluidic Chip for Studies of the Dynamics of Antibiotic Resistance Selection in Bacterial Biofilms. Front. Cell Infect. Microbiol. 2022, 12, 896149. [Google Scholar] [CrossRef]
- Kristensen, M.F.; Leonhardt, D.; Neland, M.L.B.; Schlafer, S. A 3D Printed Microfluidic Flow-Cell for Microscopy Analysis of in Situ-Grown Biofilms. J. Microbiol. Methods 2020, 171, 105876. [Google Scholar] [CrossRef]
- Niu, L.; Zhang, H.; Liu, Y.; Wang, Y.; Li, A.; Liu, R.; Zou, R.; Yang, Q. Microfluidic Chip for Odontoblasts in vitro. ACS Biomater. Sci. Eng. 2019, 5, 4844–4851. [Google Scholar] [CrossRef]
- França, C.M.; Tahayeri, A.; Rodrigues, N.S.; Ferdosian, S.; Puppin Rontani, R.M.; Sereda, G.; Ferracane, J.L.; Bertassoni, L.E. The Tooth On-a-Chip: A Microphysiologic Model System Mimicking the Biologic Interface of the Tooth with Biomaterials. Lab. Chip 2020, 20, 405–413. [Google Scholar] [CrossRef]
- Rodrigues, N.S.; França, C.M.; Tahayeri, A.; Ren, Z.; Saboia, V.P.A.; Smith, A.J.; Ferracane, J.L.; Koo, H.; Bertassoni, L.E. Biomaterial and Biofilm Interactions with the Pulp-Dentin Complex-on-a-Chip. J. Dent. Res. 2021, 100, 1136–1143. [Google Scholar] [CrossRef]
- Hu, S.; Muniraj, G.; Mishra, A.; Hong, K.; Lum, J.L.; Hong, C.H.L.; Rosa, V.; Sriram, G. Characterization of Silver Diamine Fluoride Cytotoxicity Using Microfluidic Tooth-on-a-Chip and Gingival Equivalents. Dent. Mater. 2022, 38, 1385–1394. [Google Scholar] [CrossRef]
- Qi, Y.; Zou, T.; Dissanayaka, W.L.; Wong, H.M.; Bertassoni, L.E.; Zhang, C. Fabrication of Tapered Fluidic Microchannels Conducive to Angiogenic Sprouting within Gelatin Methacryloyl Hydrogels. J. Endod. 2021, 47, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Lee, H.; Chung, M.; Jeon, N.L. Engineering of Functional, Perfusable 3D Microvascular Networks on a Chip. Lab. Chip 2013, 13, 1489. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Han, Y.; Chen, Q.; Dissanayaka, W.L. Sema4D–Plexin-B1 Signaling in Recruiting Dental Stem Cells for Vascular Stabilization on a Microfluidic Platform. Lab. Chip 2022, 22, 4632–4644. [Google Scholar] [CrossRef] [PubMed]
- Pagella, P.; Neto, E.; Jiménez-Rojo, L.; Lamghari, M.; Mitsiadis, T.A. Microfluidics Co-Culture Systems for Studying Tooth Innervation. Front. Physiol. 2014, 5, 326. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Kingsley, D.; Madhurakkat Perikamana, S.; Mogha, P.; Goodwin, C.R.; Varghese, S. Self-Assembled Innervated Vasculature-on-a-Chip to Study Nociception. Biofabrication 2023, 15, 035008. [Google Scholar] [CrossRef] [PubMed]
- Kundu, A.; McCoy, L.; Azim, N.; Nguyen, H.; Didier, C.M.; Ausaf, T.; Sharma, A.D.; Curley, J.L.; Moore, M.J.; Rajaraman, S. Fabrication and Characterization of 3D Printed, 3D Microelectrode Arrays for Interfacing with a Peripheral Nerve-on-a-Chip. ACS Biomater. Sci. Eng. 2021, 7, 3018–3029. [Google Scholar] [CrossRef] [PubMed]
- Kramer, L. Modeling Chemotherapy-Induced Peripheral Neuropathy Using a Nerve-on-a-Chip Microphysiological System. Altex 2020, 37, 350–364. [Google Scholar] [CrossRef]
- Pagella, P.; Cordiale, A.; Marconi, G.D.; Trubiani, O.; Rasponi, M.; Mitsiadis, T.A. Bioengineered Tooth Emulation Systems for Regenerative and Pharmacological Purposes. Eur. Cell Mater. 2021, 41, 502–516. [Google Scholar] [CrossRef] [PubMed]
- Franca, C.M.; de Souza Balbinot, G.; Cunha, D.; Saboia, V.d.P.A.; Ferracane, J.; Bertassoni, L.E. In-Vitro Models of Biocompatibility Testing for Restorative Dental Materials: From 2D Cultures to Organs on-a-Chip. Acta Biomater. 2022, 150, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Bertassoni, L.E. Progress and Challenges in Microengineering the Dental Pulp Vascular Microenvironment. J. Endod. 2020, 46, S90–S100. [Google Scholar] [CrossRef] [PubMed]
- Vrana, N.E.; Lavalle, P.; Dokmeci, M.R.; Dehghani, F.; Ghaemmaghami, A.M.; Khademhosseini, A. Engineering Functional Epithelium for Regenerative Medicine and In Vitro Organ Models: A Review. Tissue Eng. Part. B Rev. 2013, 19, 529–543. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Sanaei, F.; Verdurmen, W.P.R.; Yang, F.; Ji, W.; Walboomers, X.F. The Application of Organs-on-a-Chip in Dental, Oral, and Craniofacial Research. J. Dent. Res. 2023, 102, 364–375. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, F.; Htwe, S.S.; Righi, M.; Liu, H.; Pietralunga, A.; Yesil-Celiktas, O.; Maharjan, S.; Cha, B.; Shin, S.R.; Dokmeci, M.R.; et al. A Foreign Body Response-on-a-Chip Platform. Adv. Healthc. Mater. 2019, 8, e1801425. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.-J.; Kim, Y.; Salipante, P.; Kotula, A.P.; Lipshutz, S.; Graves, D.T.; Alimperti, S. Mechanical Regulation of Oral Epithelial Barrier Function. Bioengineering 2023, 10, 517. [Google Scholar] [CrossRef]
- Jin, L.; Tian, T.; Liu, D.; Mao, H.; Liu, H. ·Reconstituting Organ-Level Periodontal Soft Tissue on a Chip. In Proceedings of the 2021 21st International Conference on Solid-State Sensors, Actuators and Microsystems (Transducers), Orlando, FL, USA, 20–24 June 2021; IEEE: Piscataway, NJ, USA, 2021; pp. 707–710. [Google Scholar]
- Ly, K.L.; Rooholghodos, S.A.; Rahimi, C.; Rahimi, B.; Bienek, D.R.; Kaufman, G.; Raub, C.B.; Luo, X. An Oral-Mucosa-on-a-Chip Sensitively Evaluates Cell Responses to Dental Monomers. Biomed. Microdevices 2021, 23, 7. [Google Scholar] [CrossRef]
- Jeon, J.S.; Bersini, S.; Whisler, J.A.; Chen, M.B.; Dubini, G.; Charest, J.L.; Moretti, M.; Kamm, R.D. Generation of 3D Functional Microvascular Networks with Human Mesenchymal Stem Cells in Microfluidic Systems. Integr. Biol. 2014, 6, 555–563. [Google Scholar] [CrossRef]
- Perottoni, S.; Neto, N.G.B.; Di Nitto, C.; Dmitriev, R.I.; Raimondi, M.T.; Monaghan, M.G. Intracellular Label-Free Detection of Mesenchymal Stem Cell Metabolism within a Perivascular Niche-on-a-Chip. Lab. Chip 2021, 21, 1395–1408. [Google Scholar] [CrossRef]
- Vurat, M.T.; Şeker, Ş.; Lalegül-Ülker, Ö.; Parmaksiz, M.; Elçin, A.E.; Elçin, Y.M. Development of a Multicellular 3D-Bioprinted Microtissue Model of Human Periodontal Ligament-Alveolar Bone Biointerface: Towards a Pre-Clinical Model of Periodontal Diseases and Personalized Periodontal Tissue Engineering. Genes. Dis. 2022, 9, 1008–1023. [Google Scholar] [CrossRef]
- Nasello, G.; Alamán-Díez, P.; Schiavi, J.; Pérez, M.Á.; McNamara, L.; García-Aznar, J.M. Primary Human Osteoblasts Cultured in a 3D Microenvironment Create a Unique Representative Model of Their Differentiation Into Osteocytes. Front. Bioeng. Biotechnol. 2020, 8, 336. [Google Scholar] [CrossRef]
- Atif, A.R.; Pujari-Palmer, M.; Tenje, M.; Mestres, G. A Microfluidics-Based Method for Culturing Osteoblasts on Biomimetic Hydroxyapatite. Acta Biomater. 2021, 127, 327–337. [Google Scholar] [CrossRef]
- Middleton, K.; Al-Dujaili, S.; Mei, X.; Günther, A.; You, L. Microfluidic Co-Culture Platform for Investigating Osteocyte-Osteoclast Signalling during Fluid Shear Stress Mechanostimulation. J. Biomech. 2017, 59, 35–42. [Google Scholar] [CrossRef]
- Chi, A.C.; Day, T.A.; Neville, B.W. Oral Cavity and Oropharyngeal Squamous Cell Carcinoma—An Update. CA Cancer J. Clin. 2015, 65, 401–421. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Regmi, S.; Poudel, C.; Adhikari, R.; Luo, K.Q. Applications of Microfluidics and Organ-on-a-Chip in Cancer Research. Biosensors 2022, 12, 459. [Google Scholar] [CrossRef]
- Nguyen, H.Q.; Seo, T.S. A 3D Printed Size-Tunable Flow-Focusing Droplet Microdevice to Produce Cell-Laden Hydrogel Microspheres. Anal. Chim. Acta 2022, 1192, 339344. [Google Scholar] [CrossRef] [PubMed]
- Zoupanou, S.; Volpe, A.; Primiceri, E.; Gaudiuso, C.; Ancona, A.; Ferrara, F.; Chiriacò, M.S. SMILE Platform: An Innovative Microfluidic Approach for On-Chip Sample Manipulation and Analysis in Oral Cancer Diagnosis. Micromachines 2021, 12, 885. [Google Scholar] [CrossRef] [PubMed]
- Pagella, P.; Catón, J.; Meisel, C.T.; Mitsiadis, T.A. Ameloblastomas Exhibit Stem Cell Potential, Possess Neurotrophic Properties, and Establish Connections with Trigeminal Neurons. Cells 2020, 9, 644. [Google Scholar] [CrossRef]
- Kong, J.; Luo, Y.; Jin, D.; An, F.; Zhang, W.; Liu, L.; Li, J.; Fang, S.; Li, X.; Yang, X.; et al. A Novel Microfluidic Model Can Mimic Organ-Specific Metastasis of Circulating Tumor Cells. Oncotarget 2016, 7, 78421–78432. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Jia, Z.; Kong, J.; Zhang, F.; Fang, S.; Li, X.; Li, W.; Yang, X.; Luo, Y.; Lin, B.; et al. Carcinoma-Associated Fibroblasts Lead the Invasion of Salivary Gland Adenoid Cystic Carcinoma Cells by Creating an Invasive Track. PLoS ONE 2016, 11, e0150247. [Google Scholar] [CrossRef]
- Al-Samadi, A.; Poor, B.; Tuomainen, K.; Liu, V.; Hyytiäinen, A.; Suleymanova, I.; Mesimaki, K.; Wilkman, T.; Mäkitie, A.; Saavalainen, P.; et al. In Vitro Humanized 3D Microfluidic Chip for Testing Personalized Immunotherapeutics for Head and Neck Cancer Patients. Exp. Cell Res. 2019, 383, 111508. [Google Scholar] [CrossRef]
- Ozdemir, T.; Srinivasan, P.P.; Zakheim, D.R.; Harrington, D.A.; Witt, R.L.; Farach-Carson, M.C.; Jia, X.; Pradhan-Bhatt, S. Bottom-up Assembly of Salivary Gland Microtissues for Assessing Myoepithelial Cell Function. Biomaterials 2017, 142, 124–135. [Google Scholar] [CrossRef]
- Maria, O.M.; Maria, O.; Liu, Y.; Komarova, S.V.; Tran, S.D. Matrigel Improves Functional Properties of Human Submandibular Salivary Gland Cell Line. Int. J. Biochem. Cell Biol. 2011, 43, 622–631. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.S.; An, H.Y.; Choi, J.S.; Kim, H.J.; Lim, J.Y. Organotypic Spheroid Culture to Mimic Radiation-Induced Salivary Hypofunction. J. Dent. Res. 2017, 96, 396–405. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.-S.; Lee, S.; Hong, H.J.; Lim, Y.C.; Koh, W.-G.; Lim, J.-Y. Stem Cell Properties of Human Clonal Salivary Gland Stem Cells Are Enhanced by Three-Dimensional Priming Culture in Nanofibrous Microwells. Stem Cell Res. Ther. 2018, 9, 74. [Google Scholar] [CrossRef]
- Song, Y.; Uchida, H.; Sharipol, A.; Piraino, L.; Mereness, J.A.; Ingalls, M.H.; Rebhahn, J.; Newlands, S.D.; DeLouise, L.A.; Ovitt, C.E.; et al. Development of a Functional Salivary Gland Tissue Chip with Potential for High-Content Drug Screening. Commun. Biol. 2021, 4, 361. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Adelfio, M.; Ghezzi, C.E. Long-Term In Vitro Culture Systems to Study Human Microbiome. ACS Biomater. Sci. Eng. 2022, 8, 4613–4617. [Google Scholar] [CrossRef] [PubMed]
- Rawas-Qalaji, M.; Cagliani, R.; Al-Hashimi, N.; Al-Dabbagh, R.; Al-Dabbagh, A.; Hussain, Z. Microfluidics in Drug Delivery: Review of Methods and Applications. Pharm. Dev. Technol. 2023, 28, 61–77. [Google Scholar] [CrossRef] [PubMed]
- Soares, D.G.; Bordini, E.A.F.; Swanson, W.B.; de Souza Costa, C.A.; Bottino, M.C. Platform Technologies for Regenerative Endodontics from Multifunctional Biomaterials to Tooth-on-a-Chip Strategies. Clin. Oral. Investig. 2021, 25, 4749–4779. [Google Scholar] [CrossRef] [PubMed]
- Nashimoto, Y.; Hori, T.; Ostrovidov, S.; Katagiri, S.; Kaji, H. Engineering Oral Microenvironments Using Microphysiological Systems. Sens. Mater. 2023, 35, 1293. [Google Scholar] [CrossRef]
- Farshidfar, N.; Assar, S.; Amiri, M.A.; Sahmeddini, S.; Hamedani, S.; Zarei, M.; Tayebi, L. The Feasible Application of Microfluidic Tissue/Organ-on-a-Chip as an Impersonator of Oral Tissues and Organs: A Direction for Future Research. Biodes. Manuf. 2023, 6, 478–506. [Google Scholar] [CrossRef]



| Reference | Organ-on-a-Chip | Aim | Chip Design | Material | Cell Type | Applied Methods | Future Applications |
|---|---|---|---|---|---|---|---|
| Gashti et al. (2016) [17] | Microfluidic platform of oral biofilm | To study oral biofilm under different conditions | One chamber | PDMS | S. salivarius | pH measurements, and confocal fluorescence (CLSM) | To test localized acidification in the oral biofilm |
| Straub et al. (2020) [28] | Microfluidic platform of oral biofilm | To obtain real-time observation of bacterial adhesion and biofilm formation | Parallel | PDMS | E. coli | Single-cell tracking analysis | To study bacterial and surface interactions. To establish a tool for studying the in situ activity of antimicrobial agents against surface-associated bacteria and cells in a biofilm. |
| Lam et al. (2016) [16] | Artificial teeth | To study the bacterial growth under a matrix of different combinations of microenvironmental factors | Multi-array | PDMS | Streptococci species, F. nucleatum | CLSM, live dead, bacterial assay | To perform biofilm analysis and to test anti-biofilm agents |
| Tang et al. (2022) [29] | Microfluidic platform of oral biofilm | To develop a model for studying the antibiotic resistance dynamics | Multi-array | PDMS | E. coli | In situ staining, determination of MIC | Applications of this device in many areas of microbiology where biofilms are common |
| Rath et al. (2017) [21] | Microfluidic platform of oral biofilm | To study biofilm formation on titanium surfaces | One chamber | Polyaryletherketone (PAEK) + titanium | S. gordonii, S. salivarius, S. oralis, P. gingivalis, A. actinomycetemcomitans | Live dead | To optimize the study of the formation of oral multispecies biofilms. To investigate the influence of different flow velocities, nutrient concentrations, and substrata on the biofilm formation |
| Kristensen et al. (2020) [30] | Microfluidic platform of oral biofilm | To develop a flow cell model for bacterial studies | One chamber | Resin by 3D printing | Biofilm from healthy volunteers | pH, CLSM | To study the effect of different flow rates on pH in biofilms of different age in a larger subject group to understand the caries process |
| Niu et al. (2019) [31] | Microstructures of dentin tubules-on-a-chip | To study the physiology of dental pulp | Parallel | PDMS + collagen | Odontoblast cells; Mouse Dental Papilla Cell (MDPC-23) | CLSM | A tool for investigating the mechanisms of dental diseases and developing effective treatments |
| França et al. (2020) [32] | Tooth-on-a-chip | Dentine/pulp model for Cell testing of HEMA, phosphoric acid, scotch bond | parallel | PDMS + dentin | Stem Cells From the Apical Papilla (SCAP) | Live dead, cytotoxicity, gelatinolytic activity assay, metabolic activity assay | To test pulp response to biomaterials |
| Rodrigues et al. (2021) [33] | Dental pulp-on-a-chip | Dentine/pulp model for testing calcium silicate cements | parallel | PDMS + Dentin + Collagen 1 | Human dental pulp stem cells (hDPSC), S. mutans | CLSM, ELISA, pH, Live dead | To test pulp response to biomaterials and to bacteria |
| Kang et al. (2016) [15] | Tooth-on-a-chip | To investigate the mineralization of SHED cells in an oral cell niche | parallel | PDMS | human gingival fibroblasts (hGFs), periodontal ligament stem cells (hPDLSCs), human exfoliated deciduous teeth (SHED) | Alizarin Red Staining (ARS), RT-PCR | A model to examine the effects of ecretory factors from various oral cells on pulp stem cells |
| Hu et al. (2022) [34] | Tooth-on-a-chip | Dentine/pulp model for testing silver diamine fluoride | one chamber | Polymethyl methacrylate (PMMA) + Dentin | DPSCs (dental pulp cells), hGFs, human keratinocytes (OKF6/TERT1) | MTT, mucosal corrosion test | To test pulp response to biomaterials |
| Qi et al. (2021) [35] | Endothelized Fluidic microchannels | To test angiogenic sprouting | one chamber | Gelatin metacryloyl (GelMa) hydrogel | SCAP, Human umbelical vein endothelial cells (HUVECss) | CLSM | Root canal model for endodontic regeneration |
| Kim S et al. (2013) [36] | Microvascular networks-on-a-chip | To form perfusable and functional microvascular networks in 3D ECM constructs. | parallel | PDMS + fibrin matrix + collagen I | HUVEC, normal human lung fibroblast, Human promyelocytic leukemia cells, Human glioblastoma multiforme cells | CLSM, Measurement of vessel permeability, Fluid perfusion experiments, analysis of endothelial NO synthesis | A versatile in vitro model for the fundamental study of vascular biology and vascularized micro-organs or human disease models for drug discovery |
| Zhang et al. (2022) [37] | Vascularized dental pulp-on-a-chip | To study the SHED cell recruitment during angiogenesis | parallel | Chip from AIM Biotech + fibrin gel | HUVEC, SHED | CLSM, Western Blot (WB), Optical microscope (OP), ELISA, RT-PCR, Vessel permeability assay | A model to study vascular development |
| Pagella et al. (2014) [38] | Dental pulp nervous system-on-a-chip | To study whether trigeminal ganglia and teeth can survive for long periods of time in microfluidic devices | parallel | PDMS + poly-D-lysine and laminin | Trigeminal ganglia, Incisor tooth germs | Immunohistochemistry (IHC), CLSM | To study tooth germ formation kinetics |
| Kumar et al. (2023) [39] | Innervated Vasculature-on-a-chip | To develop a microfluidic model of innervated vasculature to study the interface between sensory neurons and vasculature | one chamber | PDMS + Poly-D-Lysine | HUVEC, murin and human primary dorsal root ganglion neurons (DRGs) | CLSM | To develop innervated micro-physiological models. |
| Kundu et al. (2021) [40] | Nerve-on-a-chip | To design a 3D microelectrode to obtain a nerve-on-a-chip | multi-arrays | Photopolymer clear resin (3D printed) layer of SiO2 | DRG | OP, scanning electron microscopy (SEM), Fourier-transform infrared spectroscopy (FTIR), propidium iodide and calcein for viability | To simulate “disease in a dish” |
| Kramer et al. (2020) [41] | Nerve-on-a-chip | To develop a rat nerve-on-a-chip to demonstrate its potential as a preclinical assay for screening for drug-induced nerve dysfunction | one chamber | Polymerized hydrogel | DRG | Compound action potentials (CAPs), Nerve conduction velocity (NCV), LDH Cytotoxicity Assay, Cell Counting Kit-8 (CCK-8), Light microscopy (LM), transmission electron microscopy (TEM), Mitochondrial membrane potential assay, IHC | To develop an effective tool for screening potentially harmful drugs and other neuropathy-inducing agents |
| Reference | Organ-on-a-Chip | Aim | Chip Design | Material | Cell Type | Applied Methods | Future Applications |
|---|---|---|---|---|---|---|---|
| Lee et al. (2023) [48] | 3D Oral Epi-mucosa platform | To investigate the epithelial barrier function in conditions of mechanical stress | one chamber | PDMS + collagen gel | Human immortalized gingival keratinocyte (hIGK) cells | Scanning Electron Microscope, Mechanical Testing, Epithelial Permeability Measurement, CLSM, Staining, RT-PCR and RT-qPCR Analysis | A model to elucidate new pathways involved in oral diseases |
| Sharifi et al. (2020) [47] | Foreign Body Response-on-a-chip (FBROC) | To investigate the response of circulating immune cells to the implants | one chamber | PDMS + PMMA + GelMA | HUVEC, human monocytes THP-1 (human leukemia monocytic cell line) | 3D conducted computational fluid dynamics (CFD) simulations, ELISA, CLSM | A model to interrogate the response to biomaterials |
| Makkar et al. (2023) [19] | Gingival crevice-on-chip | To study host–microbial interaction in periodontal disease | parallel | PDMS + fibrin gel | Gingival fibroblasts (hGFs), S. oralis, F. nucleatum | Cytotoxicity, Live dead, ELISA, CLSM | In vitro model of periodontal pocket including more oral cells |
| Jin et al. (2021) [49] | Periodontal soft tissue-on-a-chip | To develop a model of epithelial–capillary interface | parallel | PDMS + PETE membrane | Huvec, Gingival epithelial cells (hGEs) | CLSM | In vitro model of periodontal pocket to study diseases related to periodontitis |
| Rahimi et al. (2018) [23] | Oral mucosa-on-a-chip | To investigate the response to bacteria and dental materials (HEMA) | parallel | PDMS + collagen I | Human gingival Keratinocytes (hGKs), hGFs, S. mutans | CLSM, Live dead, impedance spectrometer | For testing the response to biomaterials and bacteria by incorporating the patient’s immune cells |
| Ly et al. (2021) [50] | Oral mucosa-on-a-chip | To study the response of gingiva to dental biomaterials (HEMA at different concentrations) | parallel | PDMS + collagen I | Human gingival Keratinocytes (hGKs), hGFs | CLSM, Live dead | Evaluation of tissue response to various biomaterials |
| Reference | Organ-on-a-Chip | Aim | Chip Design | Material | Cell Type | Applied Methods | Future Applications |
|---|---|---|---|---|---|---|---|
| Vurat et al. (2020) [53] | Periodontal ligament–alveolar bone 3D bioprinted | To develop a multicellular 3D-bioprinted microtissue model of human periodontal ligament–alveolar bone bio-interface | one chamber | PDMS + Methacrylated gelatin (Gel-MA) + hydroxyapatite–magnetic iron oxide nanoparticles | Human periondal ligament fibroblasts (hPDLFs), osteoblasts (hOBs) | Rheology, ATR-FTIR analysis, Thermogravimetric analysis, Mechanical analysis, SEM, Swelling testing, Alamar blue assay, Live/dead cell staining, CSLM, histochemical staining (PAS) | In vitro model to study the potential effects of drugs |
| Perottoni et al. (2021) [52] | Perivascular niche-on-a-chip | To develop and validate a miniaturized platform for profiling stem cell metabolism in a niche-on-a-chip | parallel | Oxygen-impermeable polycarbonate (PC) | Bone marrow-derived human MSCs (h-MSCs) | Computational fluid dynamic (CFD) analysis, Multiphoton quantitative intracellular oxygen imaging, Two-photon fluorescence lifetime imaging microscopy (2P-FLIM) | To provide a reliable tool for disease modelling and drug screening |
| Nasello et al. (2020) [54] | Bone-on-a-chip | To develop a bone-on-a-chip device to study the osteoblast differentiation into osteocytes | parallel | PDMS + hydrogel | hOB | CSLM, inverted brightfield microscope, calcein green staining, extracellular ALP activity. | To develop patient-specific bone models to study the individual osteogenic potential and the effect of alternative therapies |
| Jeon et al. (2014) [51] | Microvascular network-on-chip | To generate a functional, perfusable 3D human microvascular network | parallel | PDMS + hydrogel | Endothelial stem cells (ECs), bone marrow-derived human mesenchymal stem cells (BM-hMSCs) | CSLM, Vessel permeability | To test diffusion and effects of therapeutics in complex microenvironments |
| Atif et al. (2021) [55] | Hydroxyapatite (HA)-on-chip | To integrate HA in a microfluidic platform and to assess the behavior of pre-osteoblast | parallel | PDMS + biomimetic hydroxyapatite | Mouse osteoblasts (MC3T3-E1) | Cell viability, LDH, ALP assay | A tool to evaluate the biological properties of biomaterials |
| Middleton et al. (2017) [56] | Bone-on-a-chip | To study the cross-talk between bone cells under different flow conditions | parallel | Not specified | Osteoclast precursors (RAW264.7), osteocytes (MLO-Y4) | CSLM | A tool for investigating bone response to different stimuli |
| Reference | Organ-on-a-Chip | Aim | Chip Design | Material | Cell Type | Applied Methods | Future Applications |
|---|---|---|---|---|---|---|---|
| Pagella et al. (2020) [62] | Innervated ameloblastoma-on-a-chip | To study the interaction between ameloblastoma cells and trigeminal ganglia cells | Parallel | PDMS + laminin | ameloblastoma cells, Trigeminal Ganglia cells from mouse | CLSM | In vitro model to study the invasiveness of cancer cells |
| Kong et al. (2016) [63] | Organ metastasis of circulating tumor cells-on-a-chip | To assess the potential of breast and salivary gland cancer cells to metastasize to the lung | parallel | PDMS + collagen I | HUVEC, MCF-7, and MBA-MD-231 (breast cancer cells), salivary gland adenoid cystic carcinoma cell line (ACC-M), Primary murine pulmonary cells, Primary murine hepatocytes | ELISA, CLSM, and Flow cytometry | An in vitro model to predict the metastatic capabilities of tumor circulating cells, and to rapidly screen possible anti-metastatic drugs. |
| Liu et al. (2016) [20] | Tumor-induced angiogenesis-on-a-chip | To investigate metastasis and invasiveness processes in oral cancer | Parallel | PDMS | HUVEC, oral squamous cell carcinoma (UM-SCC6), Salivary gland adenoid cystic carcinoma (ACC-M) | CLSM, | An in vitro model to test future anti-cancer and antiangiogenic drugs |
| Zoupanou et al. (2021) [61] | Plug-and-play device | To develop a device for early screening of oral squamous cell carcinoma | Serpentine | PMMA functionalized with O2 plasma | Jurkart cells (t-cell leukemia), human oral cavity squamous cell carcinoma (OECM-1) | Tests to distinguish cancer cells from blood cells | Early diagnosis of oral carcinoma |
| Li et al. (2016) [64] | Adenoid cystic carcinoma (ACC) platform | To study the role of Carcinoma-associated fibroblasts (CAFs) in the progression of adenoid cystic carcinoma (ACC) | Parallel | PDMS | CAF from (ACC) patients, human salivary adenoid cystic carcinoma cell line (SACC83), metastatic lung cells (LM) | Optical microscope, cell invasion and migration assay, wound healing, CLSM | A model to study ACC progression |
| Nguyen et al. (2022) [60] | A 3D-printed size-tunable flow-focusing droplet microdevice | To develop a droplet device that permits the generation under control, Ca-alginate microspheres containing tumor cells | Resin by 3D printing | A549 adenocarcinomic human alveolar basal epithelial cells | CLSM | A tool for tumor spheroid production | |
| Al-Samadi et al. (2019) [65] | Tongue cancer-on-a-chip | To test the efficacy of immunotherapy | parallel | PDMS + myogelfibrin | tongue cancer cell line (HSC-3), and monocytes (hMNC) | CLSM | A 3D model to study novel therapies for tongue cancer |
| Reference | Organ-on-a-Chip | Aim | Chip Design | Material | Cell Type | Applied Methods | Future Applications |
|---|---|---|---|---|---|---|---|
| Song et al. (2021) [70] | Salivary gland model | To develop functional tissue mimetics for mouse and human salivary glands | multi-arrays | PDMS + Hydrogel | Mouse acinar cell clusters and intercalated ducts (AIDUCs) | LIVE/DEAD, RT-PCR, CMLS, Calcium signalling assay, amylase activity | To provide a tool for mechanistic studies and for clinically predictive screening assays |
| Yin et al. (2023) [18] | Salivary gland model | To produce with a 3D printer a Microfluidic device cell-laden microfibers and microtubes for salivary gland tissue engineering | multi-arrays | Alginate hydrogel | human Salivary Stem progenitor cells (hS/PCs) | LIVE/DEAD, calcein, Ethidium Homodimer-III, different imaging techniques, Immunochemistry | To produce a model that mimics salivary glands |
| 1 | Huang C, Sanaei F, Verdurmen WPR, Yang F, Ji W, Walboomers XF. The Application of Organs-on-a-Chip in Dental, Oral, and Craniofacial Research. J Dent Res. 2023 Apr;102(4):364–375. https://doi.org/10.1177/00220345221145555. Epub 2023 Feb 1. PMID: 36726271; PMCID: PMC10031637. [46] | Review |
| 2 | Tiozzo-Lyon P, Andrade M, Leiva-Sabadini C, Morales J, Olivares A, Ravasio A, Aguayo S. Microfabrication approaches for oral research and clinical dentistry Front. Dent. Med, 09 March 2023 Sec. Dental Materials. Volume 4—2023 | https://doi.org/10.3389/fdmed.2023.1120394 [25] | Review |
| 3 | Adelfio M, Ghezzi CE. Long-Term In Vitro Culture Systems to Study Human Microbiome. ACS Biomater Sci Eng. 2022 Nov 14;8(11):4613–4617. https://doi.org/10.1021/acsbiomaterials.1c01380. Epub 2022 Mar 24. PMID: 35324141; PMCID: PMC9508280. [73] | Review |
| 4 | Franca CM, Balbinot GS, Cunha D, Saboia VPA, Ferracane J, Bertassoni LE. In-vitro models of biocompatibility testing for restorative dental materials: From 2D cultures to organs on-a-chip. Acta Biomater. 2022 Sep 15;150:58–66. https://doi.org/10.1016/j.actbio.2022.07.060. Epub 2022 Aug 3. PMID: 35933103; PMCID: PMC9814917. [43] | Review |
| 5 | Regmi S, Poudel C, Adhikari R, Luo KQ. Applications of Microfluidics and Organ-on-a-Chip in Cancer Research. Biosensors (Basel). 2022 Jun 27;12(7):459. https://doi.org/10.3390/bios12070459. PMID: 35884262; PMCID: PMC9313151. [59] | Review |
| 6 | Rawas-Qalaji M, Cagliani R, Al-Hashimi N, Al-Dabbagh R, Al-Dabbagh A, Hussain Z. Microfluidics in drug delivery: review of methods and applications. Pharm Dev Technol. 2023 Jan;28(1):61–77. https://doi.org/10.1080/10837450.2022.2162543. Epub 2023 Jan 2. PMID: 36592376. [74] | Review |
| 7 | Soares DG, Bordini EAF, Swanson WB, de Souza Costa CA, Bottino MC. Platform technologies for regenerative endodontics from multifunctional biomaterials to tooth-on-a-chip strategies. Clin Oral Investig. 2021 Aug;25(8):4749–4779. https://doi.org/10.1007/s00784-021-04013-4. Epub 2021 Jun 28. PMID: 34181097; PMCID: PMC8546585. [75] | Review |
| 8 | Pagella P, Cordiale A, Marconi GD, Trubiani O, Rasponi M, Mitsiadis TA. Bioengineered tooth emulation systems for regenerative and pharmacological purposes. Eur Cell Mater. 2021 May 10;41:502–516. https://doi.org/10.22203/eCM.v041a32. PMID: 33970477. [42] | Review |
| 9 | Bertassoni LE. Progress and Challenges in Microengineering the Dental Pulp Vascular Microenvironment. J Endod. 2020 Sep;46(9S):S90-S100. https://doi.org/10.1016/j.joen.2020.06.033. PMID: 32950200; PMCID: PMC9924144. [44] | Review |
| 10 | Nashimoto Y, Hori T, Ostrovidov S, Katagiri S, Kaji H. Engineering Oral Microenvironments Using Microphysiological Systems. Sensors and Materials, Vol. 35, No. 4 (2023) 1293–1299 1293. https://doi.org/10.18494/SAM4164 [76] | Review |
| 11 | Farshidfar, N., Assar, S., Amiri, M.A. et al. The feasible application of microfluidic tissue/organ-on-a-chip as an impersonator of oral tissues and organs: a direction for future research. Bio-des. Manuf. 6, 478–506 (2023). https://doi.org/10.1007/s42242-023-00235-5 [77] | Review |
| Nr. | Reference | Topic |
|---|---|---|
| 1 | Kundu A, McCoy L, Azim N, Nguyen H, Didier CM, Ausaf T, Sharma AD, Curley JL, Moore MJ, Rajaraman S. Fabrication and Characterization of 3D Printed, 3D Microelectrode Arrays for Interfacing with a Peripheral Nerve-on-a-Chip. ACS Biomater Sci Eng. 2021 Jul 12;7(7):3018-3029. https://doi.org/10.1021/acsbiomaterials.0c01184. Epub 2020 Dec 10. PMID: 34275292. [40] | Tooth |
| 2 | França CM, Tahayeri A, Rodrigues NS, Ferdosian S, Puppin Rontani RM, Sereda G, Ferracane JL, Bertassoni LE. The tooth on-a-chip: a microphysiologic model system mimicking the biologic interface of the tooth with biomaterials. Lab Chip. 2020 Jan 21;20(2):405-413. https://doi.org/10.1039/c9lc00915a. Epub 2019 Dec 19. PMID: 31854401; PMCID: PMC7395925. [32] | Tooth |
| 3 | Hu S, Muniraj G, Mishra A, Hong K, Lum JL, Hong CHL, Rosa V, Sriram G. Characterization of silver diamine fluoride cytotoxicity using microfluidic tooth-on-a-chip and gingival equivalents. Dent Mater. 2022 Aug;38(8):1385-1394. https://doi.org/10.1016/j.dental.2022.06.025. Epub 2022 Jun 29. PMID: 35778310. [34] | Tooth |
| 4 | Rodrigues NS, França CM, Tahayeri A, Ren Z, Saboia VPA, Smith AJ, Ferracane JL, Koo H, Bertassoni LE. Biomaterial and Biofilm Interactions with the Pulp-Dentin Complex-on-a-Chip. J Dent Res. 2021 Sep;100(10):1136-1143. https://doi.org/10.1177/00220345211016429. Epub 2021 May 26. PMID: 34036838; PMCID: PMC8504857. [33] | Tooth |
| 5 | Kumar V, Kingsley D, Madhurakkat Perikamana S, Mogha P, Goodwin CR, Varghese S. Self-assembled innervated vasculature-on-a-chip to study nociception. Biofabrication. 2023 Apr 13;15(3):10.1088/1758-5090/acc904. https://doi.org/10.1088/1758-5090/acc904. PMID: 36996841; PMCID: PMC10152403. [39] | Tooth |
| 6 | Kramer L, Nguyen HT, Jacobs E, McCoy L, Curley JL, Sharma AD, Moore MJ. Modeling chemotherapy-induced peripheral neuropathy using a Nerve-on-a-chip microphysiological system. ALTEX. 2020;37(3):350-364. https://doi.org/10.14573/altex.2001181. Epub 2020 May 7. PMID: 32388569. [41] | Tooth |
| 7 | Pagella P, Neto E, Jiménez-Rojo L, Lamghari M, Mitsiadis TA. Microfluidics co-culture systems for studying tooth innervation. Front Physiol. 2014 Aug 25;5:326. https://doi.org/10.3389/fphys.2014.00326. [38] | Tooth |
| 8 | Zhang L, Han Y, Chen Q, Dissanayaka WL. Sema4D-plexin-B1 signaling in recruiting dental stem cells for vascular stabilization on a microfluidic platform. Lab Chip. 2022 Nov 22;22(23):4632-4644. https://doi.org/10.1039/d2lc00632d. PMID: 36331411. [37] | Tooth |
| 9 | Kim S, Lee H, Chung M, Jeon NL. Engineering of functional, perfusable 3D microvascular networks-on-a-chip. Lab Chip. 2013 Apr 21;13(8):1489-500. https://doi.org/10.1039/c3lc41320a. Erratum in: Lab Chip. 2013 Dec 21;13(24):4891. PMID: 23440068. [36] | Tooth |
| 10 | Qi Y, Zou T, Dissanayaka WL, Wong HM, Bertassoni LE, Zhang C. Fabrication of Tapered Fluidic Microchannels Conducive to Angiogenic Sprouting within Gelatin Methacryloyl Hydrogels. J Endod. 2021 Jan;47(1):52-61. https://doi.org/10.1016/j.joen.2020.08.026. Epub 2020 Oct 9. PMID: 33045266. [35] | Tooth |
| 11 | Niu L, Zhang H, Liu Y, Wang Y, Li A, Liu R, Zou R, Yang Q. Microfluidic Chip for Odontoblasts in Vitro. ACS Biomater Sci Eng. 2019 Sep 9;5(9):4844-4851. https://doi.org/10.1021/acsbiomaterials.9b00743. Epub 2019 Aug 1. PMID: 33448827. [31] | Tooth |
| 12 | Kang, KJ., Ju, S.M., Jang, YJ. et al. Indirect co-culture of stem cells from human exfoliated deciduous teeth and oral cells in a microfluidic platform. Tissue Eng Regen Med 13, 428–436 (2016). https://doi.org/10.1007/s13770-016-0005-2 [15] | Tooth |
| 13 | Tang PC, Eriksson O, Sjögren J, Fatsis-Kavalopoulos N, Kreuger J, Andersson DI. A Microfluidic Chip for Studies of the Dynamics of Antibiotic Resistance Selection in Bacterial Biofilms. Front Cell Infect Microbiol. 2022 May 10;12:896149. https://doi.org/10.3389/fcimb.2022.896149. PMID: 35619647; PMCID: PMC9128571. [29] | Tooth |
| 14 | Kristensen MF, Leonhardt D, Neland MLB, Schlafer S. A 3D printed microfluidic flow-cell for microscopy analysis of in situ-grown biofilms. J Microbiol Methods. 2020 Apr;171:105876. https://doi.org/10.1016/j.mimet.2020.105876. Epub 2020 Feb 19. PMID: 32087186. [30] | Tooth |
| 15 | Rath H, Stumpp SN, Stiesch M. Development of a flow chamber system for the reproducible in vitro analysis of biofilm formation on implant materials. PLoS One. 2017 Feb 10;12(2):e0172095. https://doi.org/10.1371/journal.pone.0172095. PMID: 28187188; PMCID: PMC5302373. [21] | Tooth |
| 16 | Lam RH, Cui X, Guo W, Thorsen T. High-throughput dental biofilm growth analysis for multiparametric microenvironmental biochemical conditions using microfluidics. Lab Chip. 2016 Apr 26;16(9):1652-62. https://doi.org/10.1039/c6lc00072j. PMID: 27045372. [16] | Tooth |
| 17 | Straub H, Eberl L, Zinn M, Rossi RM, Maniura-Weber K, Ren Q. A microfluidic platform for in situ investigation of biofilm formation and its treatment under controlled conditions. J Nanobiotechnology. 2020 Nov 11;18(1):166. https://doi.org/10.1186/s12951-020-00724-0. PMID: 33176791; PMCID: PMC7661213. [28] | Tooth |
| 18 | Gashti MP, Asselin J, Barbeau J, Boudreau D, Greener J. A microfluidic platform with pH imaging for chemical and hydrodynamic stimulation of intact oral biofilms. Lab Chip. 2016 Apr 21;16(8):1412-9. https://doi.org/10.1039/c5lc01540e. PMID: 26956837. [17] | Tooth |
| 19 | L. Jin, T. Tian, D. Liu, H. Mao and H. Liu, “·Reconstituting Organ-Level Periodontal Soft Tissue-on-a-chip,” 2021 21st International Conference on Solid-State Sensors, Actuators and Microsystems (Transducers), Orlando, FL, USA, 2021, pp. 707-710, https://doi.org/10.1109/Transducers50396.2021.9495506. [49] | Mucosa |
| 20 | Lee EJ, Kim Y, Salipante P, Kotula AP, Lipshutz S, Graves DT, Alimperti S. Mechanical Regulation of Oral Epithelial Barrier Function. Bioengineering (Basel). 2023 Apr 25;10(5):517. https://doi.org/10.3390/bioengineering10050517. PMID: 37237587; PMCID: PMC10215350. [48] | Mucosa |
| 21 | Makkar H, Zhou Y, Tan KS, Lim CT, Sriram G. Modeling Crevicular Fluid Flow and Host-Oral Microbiome Interactions in a Gingival Crevice-on-Chip. Adv Healthc Mater. 2023 Jan;12(6):e2202376. https://doi.org/10.1002/adhm.202202376. Epub 2022 Nov 28. PMID: 36398428. [19] | Mucosa |
| 22 | Sharifi F, Htwe SS, Righi M, Liu H, Pietralunga A, Yesil-Celiktas O, Maharjan S, Cha BH, Shin SR, Dokmeci MR, Vrana NE, Ghaemmaghami AM, Khademhosseini A, Zhang YS. A Foreign Body Response-on-a-Chip Platform. Adv Healthc Mater. 2019 Feb;8(4):e1801425. https://doi.org/10.1002/adhm.201801425. Epub 2019 Jan 29. PMID: 30694616; PMCID: PMC6398437. [47] | Mucosa |
| 23 | Rahimi C, Rahimi B, Padova D, Rooholghodos SA, Bienek DR, Luo X, Kaufman G, Raub CB. Oral mucosa-on-a-chip to assess layer-specific responses to bacteria and dental materials. Biomicrofluidics. 2018 Sep 26;12(5):054106. https://doi.org/10.1063/1.5048938. PMID: 30310527; PMCID: PMC6158033. [23] | Mucosa |
| 24 | Ly KL, Rooholghodos SA, Rahimi C, Rahimi B, Bienek DR, Kaufman G, Raub CB, Luo X. An Oral-mucosa-on-a-chip sensitively evaluates cell responses to dental monomers. Biomed Microdevices. 2021 Jan 11;23(1):7. https://doi.org/10.1007/s10544-021-00543-6. PMID: 33426594; PMCID: PMC8344876. [50] | Mucosa |
| 25 | Vurat MT, Şeker Ş, Lalegül-Ülker Ö, Parmaksiz M, Elçin AE, Elçin YM. Development of a multicellular 3D-bioprinted microtissue model of human periodontal ligament-alveolar bone biointerface: Towards a pre-clinical model of periodontal diseases and personalized periodontal tissue engineering. Genes Dis. 2020 Nov 28;9(4):1008-1023. https://doi.org/10.1016/j.gendis.2020.11.011. PMID: 35685479; PMCID: PMC9170773. [53] | Bone |
| 26 | Nasello G, Alamán-Díez P, Schiavi J, Pérez MÁ, McNamara L, García-Aznar JM. Primary Human Osteoblasts Cultured in a 3D Microenvironment Create a Unique Representative Model of Their Differentiation Into Osteocytes. Front Bioeng Biotechnol. 2020 Apr 24;8:336. https://doi.org/10.3389/fbioe.2020.00336. PMID: 32391343; PMCID: PMC7193048. [54] | Bone |
| 27 | Perottoni S, Neto NGB, Di Nitto C, Dmitriev RI, Raimondi MT, Monaghan MG. Intracellular label-free detection of mesenchymal stem cell metabolism within a perivascular niche-on-a-chip. Lab Chip. 2021 Apr 7;21(7):1395-1408. https://doi.org/10.1039/d0lc01034k. Epub 2021 Feb 19. PMID: 33605282. [52] | Bone |
| 28 | Jeon JS, Bersini S, Whisler JA, Chen MB, Dubini G, Charest JL, Moretti M, Kamm RD. Generation of 3D functional microvascular networks with human mesenchymal stem cells in microfluidic systems. Integr Biol (Camb). 2014 May;6(5):555-63. https://doi.org/10.1039/c3ib40267c. PMID: 24676392; PMCID: PMC4307755. [51] | Bone |
| 29 | Atif AR, Pujari-Palmer M, Tenje M, Mestres G. A microfluidics-based method for culturing osteoblasts on biomimetic hydroxyapatite. Acta Biomater. 2021 Jun;127:327-337. https://doi.org/10.1016/j.actbio.2021.03.046. Epub 2021 Mar 27. PMID: 33785452. [55] | Bone |
| 30 | Middleton K, Al-Dujaili S, Mei X, Günther A, You L. Microfluidic co-culture platform for investigating osteocyte-osteoclast signalling during fluid shear stress mechanostimulation. J Biomech. 2017 Jul 5;59:35-42. https://doi.org/10.1016/j.jbiomech.2017.05.012. Epub 2017 May 18. PMID: 28552413. [56] | Bone |
| 31 | Song Y, Uchida H, Sharipol A, Piraino L, Mereness JA, Ingalls MH, Rebhahn J, Newlands SD, DeLouise LA, Ovitt CE, Benoit DSW. Development of a functional salivary gland tissue chip with potential for high-content drug screening. Commun Biol. 2021 Mar 19;4(1):361. https://doi.org/10.1038/s42003-021-01876-x. Erratum in: Commun Biol. 2021 Apr 30;4(1):533. Erratum in: Commun Biol. 2022 Mar 30;5(1):315. PMID: 33742114; PMCID: PMC7979686. [70] | Salivary Glands |
| 32 | Yin Y, Vázquez-Rosado EJ, Wu D, Viswananthan V, Farach A, Farach-Carson MC, Harrington DA. Microfluidic coaxial 3D bioprinting of cell-laden microfibers and microtubes for salivary gland tissue engineering. Biomater Adv. 2023 Aug 14;154:213588. https://doi.org/10.1016/j.bioadv.2023.213588. Epub ahead of print. PMID: 37634337. [18] | Salivary Glands |
| 33 | Nguyen HQ, Seo TS. A 3D printed size-tunable flow-focusing droplet microdevice to produce cell-laden hydrogel microspheres. Anal Chim Acta. 2022 Feb 1;1192:339344. https://doi.org/10.1016/j.aca.2021.339344. Epub 2021 Dec 7. PMID: 35057943. [60] | Carcinoma |
| 34 | Pagella P, Catón J, Meisel CT, Mitsiadis TA. Ameloblastomas Exhibit Stem Cell Potential, Possess Neurotrophic Properties, and Establish Connections with Trigeminal Neurons. Cells. 2020 Mar 6;9(3):644. https://doi.org/10.3390/cells9030644. PMID: 32155948; PMCID: PMC7140461. [62] | Carcinoma |
| 35 | Kong J, Luo Y, Jin D, An F, Zhang W, Liu L, Li J, Fang S, Li X, Yang X, Lin B, Liu T. A novel microfluidic model can mimic organ-specific metastasis of circulating tumor cells. Oncotarget. 2016 Nov 29;7(48):78421-78432. https://doi.org/10.18632/oncotarget.9382. PMID: 27191997; PMCID: PMC5346650. [63] | Carcinoma |
| 36 | Liu, Lilu and Xie, Zhaorong and Zhang, Wenyuan and Fang, Shimeng and Kong, Jing and Jin, Dong and Li, Jiao and Li, Xiaojie and Yang, Xuesong and Luo, Yong and Lin, Bingcheng and Liu, Tingjiao. Biomimetic tumor-induced angiogenesis and anti-angiogenic therapy in a microfluidic model”, RSC Adv. 2016”, 6, 42, 35248-35256”, doi ==“10.1039/C6RA05645H” [20] | Carcinoma |
| 37 | Zoupanou S, Volpe A, Primiceri E, Gaudiuso C, Ancona A, Ferrara F, Chiriacò MS. SMILE Platform: An Innovative Microfluidic Approach for On-Chip Sample Manipulation and Analysis in Oral Cancer Diagnosis. Micromachines (Basel). 2021 Jul 27;12(8):885. https://doi.org/10.3390/mi12080885. PMID: 34442507; PMCID: PMC8401059. [61] | Carcinoma |
| 38 | Li J, Jia Z, Kong J, Zhang F, Fang S, Li X, Li W, Yang X, Luo Y, Lin B, Liu T. Carcinoma-Associated Fibroblasts Lead the Invasion of Salivary Gland Adenoid Cystic Carcinoma Cells by Creating an Invasive Track. PLoS One. 2016 Mar 8;11(3):e0150247. https://doi.org/10.1371/journal.pone.0150247. PMID: 26954362; PMCID: PMC4782997. [64] | Carcinoma |
| 39 | Al-Samadi A, Poor B, Tuomainen K, Liu V, Hyytiäinen A, Suleymanova I, Mesimaki K, Wilkman T, Mäkitie A, Saavalainen P, Salo T. In vitro humanized 3D microfluidic chip for testing personalized immunotherapeutics for head and neck cancer patients. Exp Cell Res. 2019 Oct 15;383(2):111508. https://doi.org/10.1016/j.yexcr.2019.111508. Epub 2019 Jul 26. PMID: 31356815. [65] | Carcinoma |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pierfelice, T.V.; D’Amico, E.; Petrini, M.; Romano, M.; D’Arcangelo, C.; Sbordone, L.; Barone, A.; Plebani, R.; Iezzi, G. A Systematic Review on Organ-on-a-Chip in PDMS or Hydrogel in Dentistry: An Update of the Literature. Gels 2024, 10, 102. https://doi.org/10.3390/gels10020102
Pierfelice TV, D’Amico E, Petrini M, Romano M, D’Arcangelo C, Sbordone L, Barone A, Plebani R, Iezzi G. A Systematic Review on Organ-on-a-Chip in PDMS or Hydrogel in Dentistry: An Update of the Literature. Gels. 2024; 10(2):102. https://doi.org/10.3390/gels10020102
Chicago/Turabian StylePierfelice, Tania Vanessa, Emira D’Amico, Morena Petrini, Mario Romano, Camillo D’Arcangelo, Ludovico Sbordone, Antonio Barone, Roberto Plebani, and Giovanna Iezzi. 2024. "A Systematic Review on Organ-on-a-Chip in PDMS or Hydrogel in Dentistry: An Update of the Literature" Gels 10, no. 2: 102. https://doi.org/10.3390/gels10020102
APA StylePierfelice, T. V., D’Amico, E., Petrini, M., Romano, M., D’Arcangelo, C., Sbordone, L., Barone, A., Plebani, R., & Iezzi, G. (2024). A Systematic Review on Organ-on-a-Chip in PDMS or Hydrogel in Dentistry: An Update of the Literature. Gels, 10(2), 102. https://doi.org/10.3390/gels10020102










