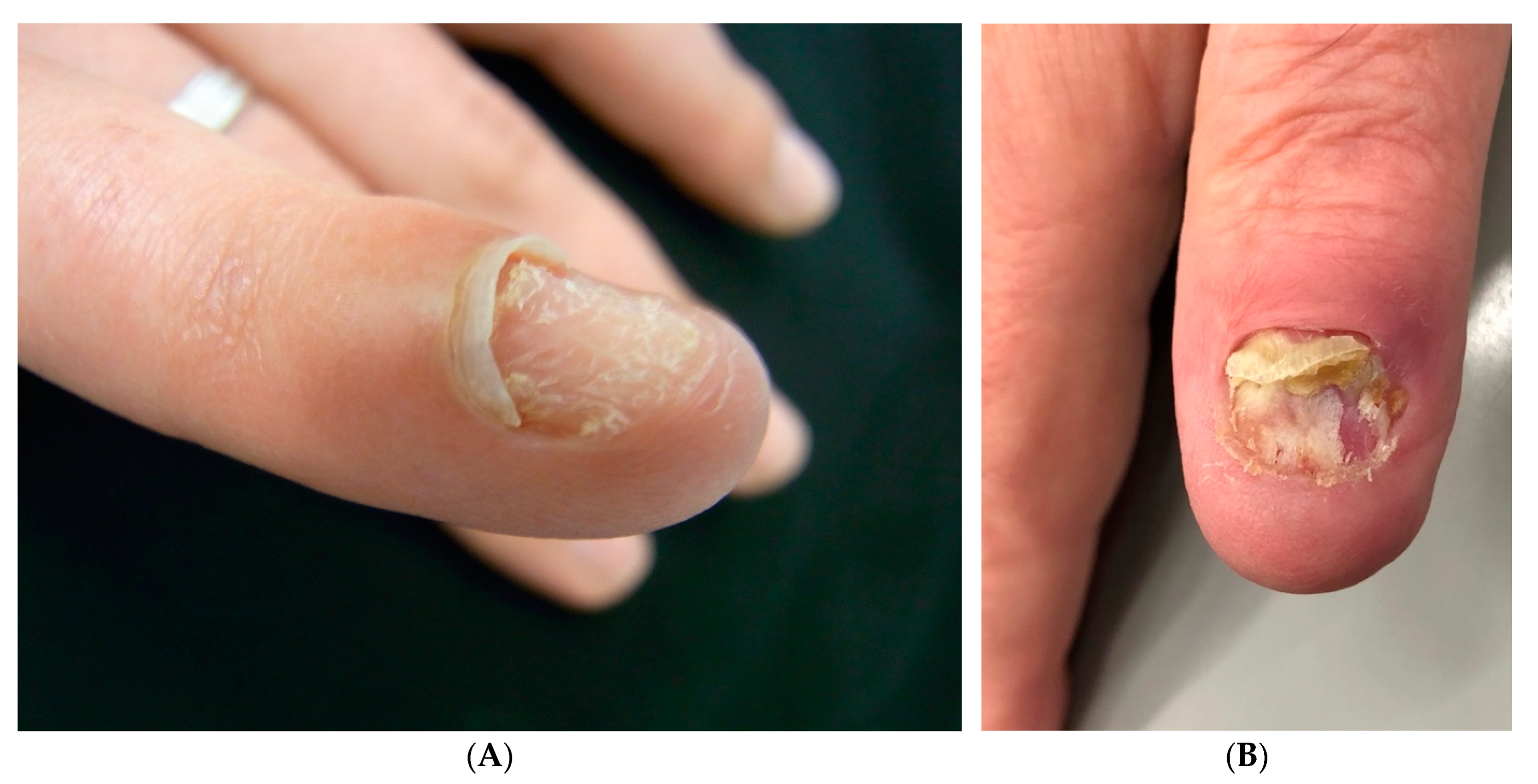
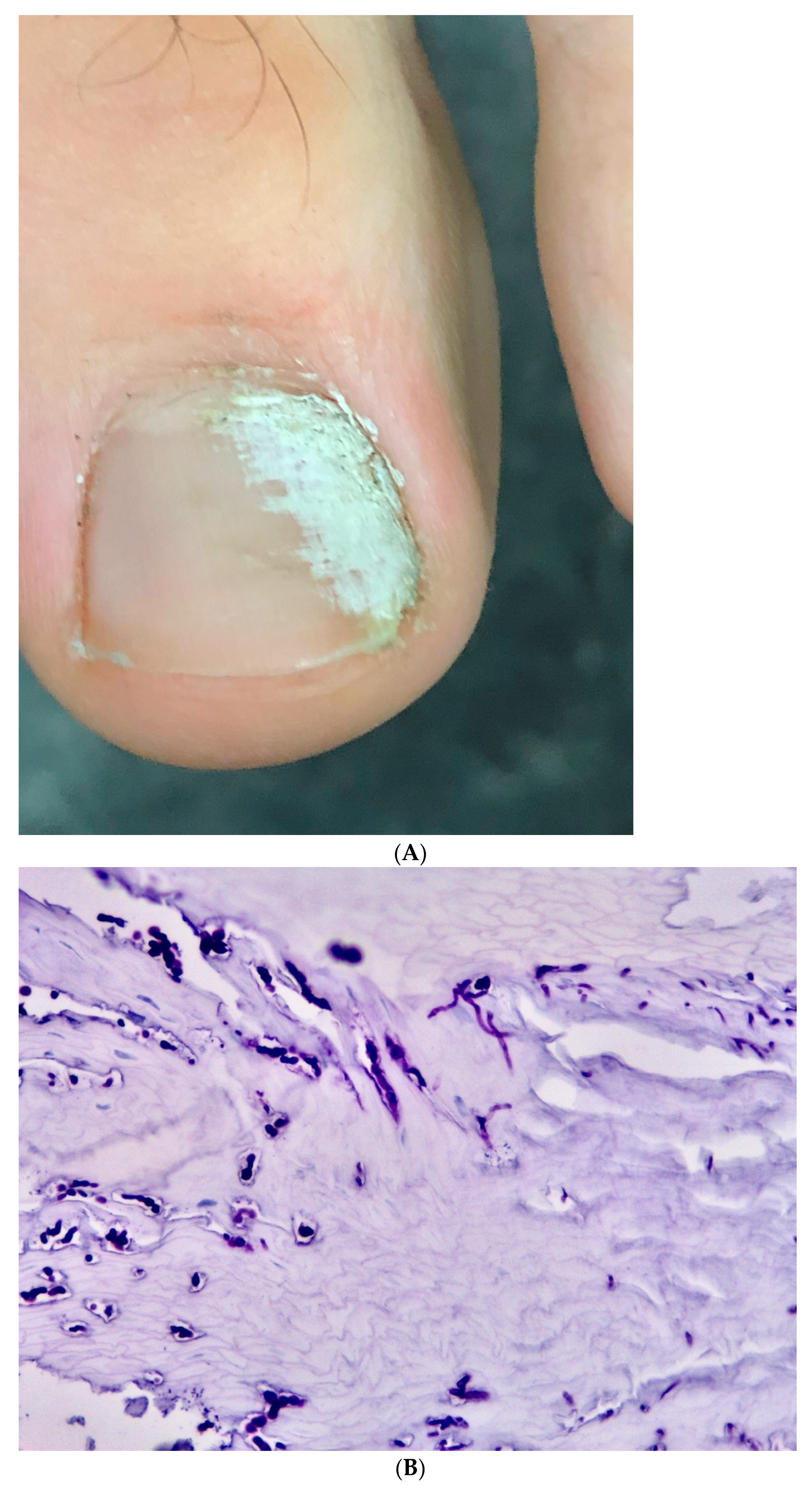
Post-Traumatic Single-Digit Onychomycosis
Abstract
1. Introduction
2. Patients and Methods
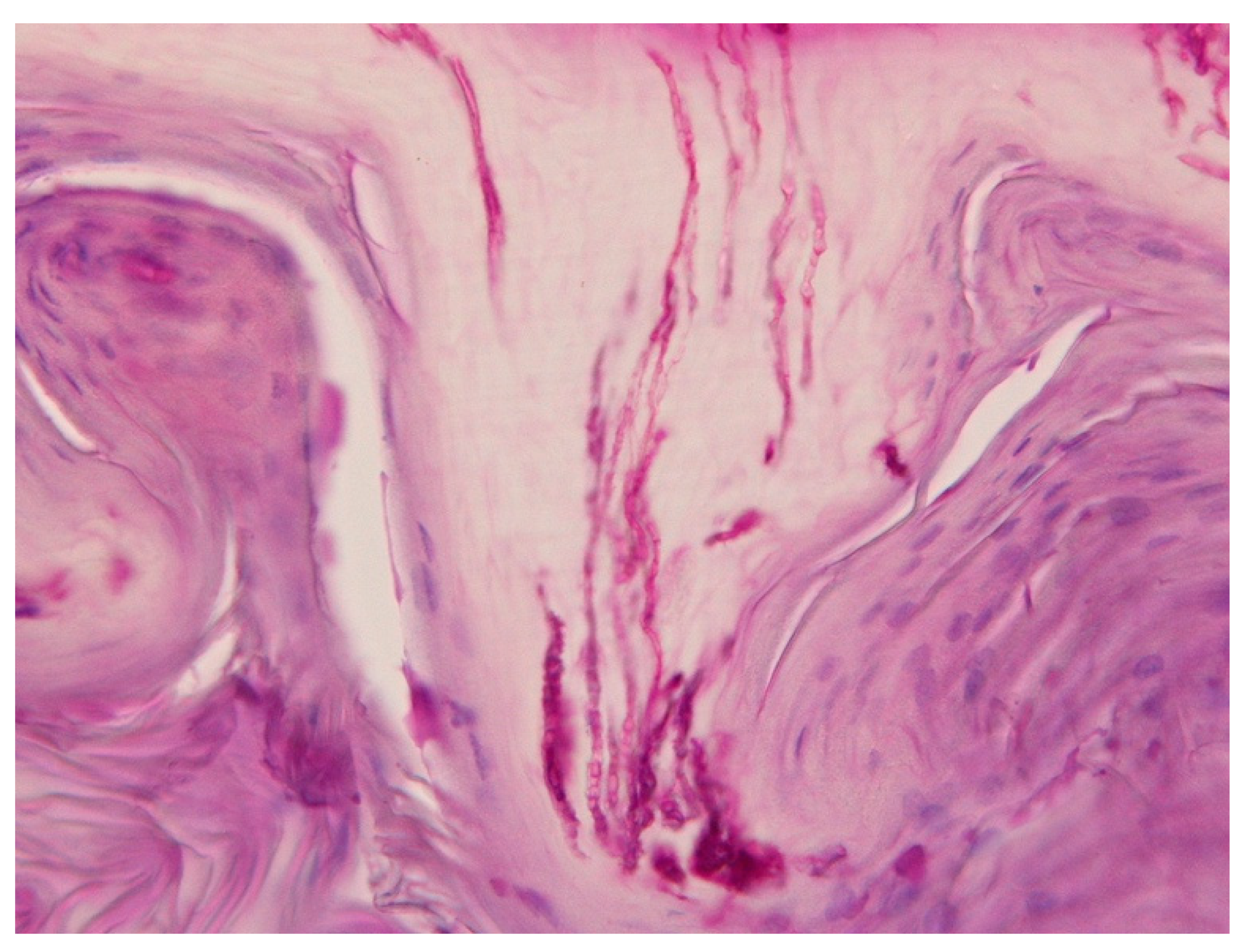
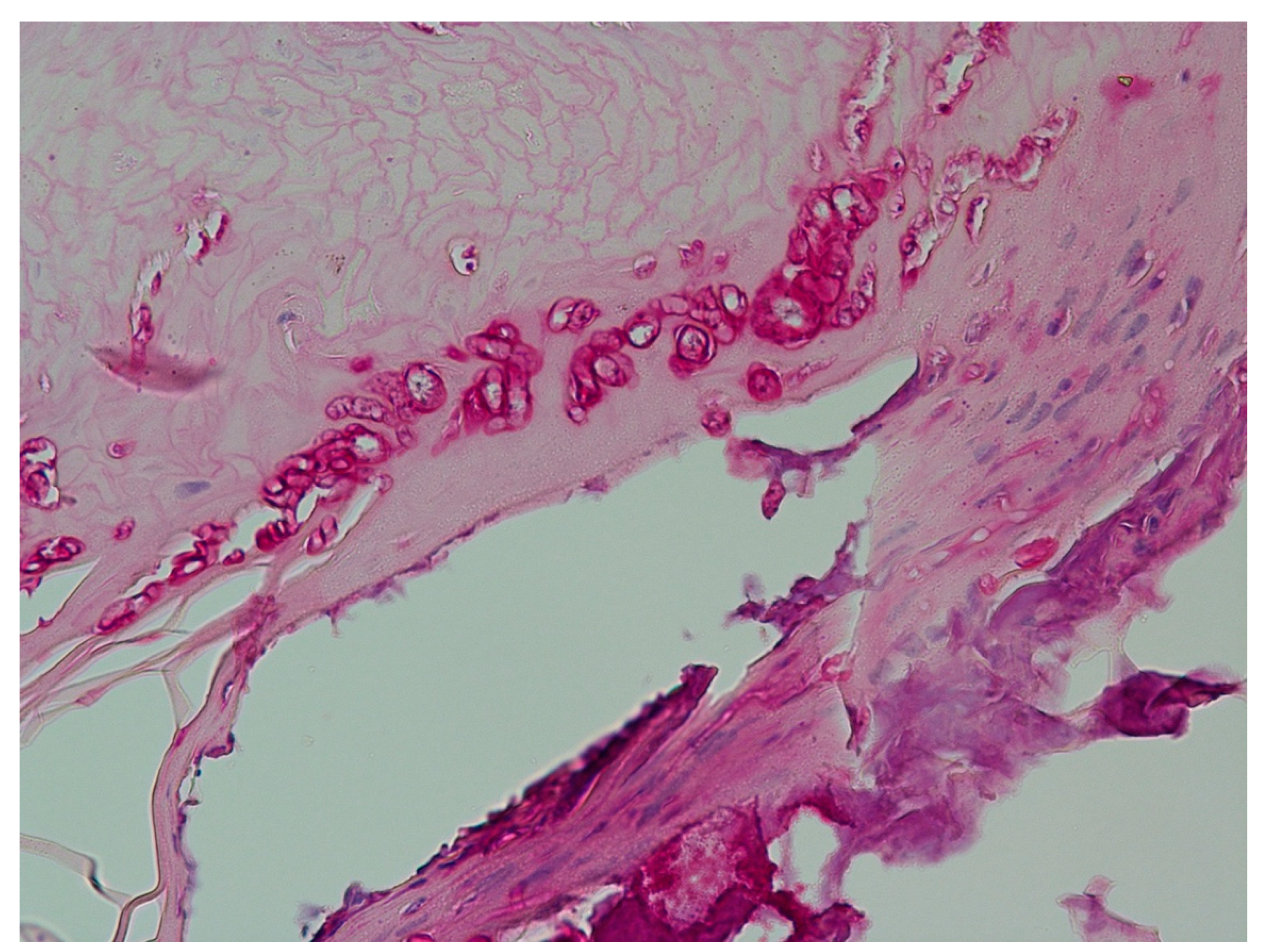
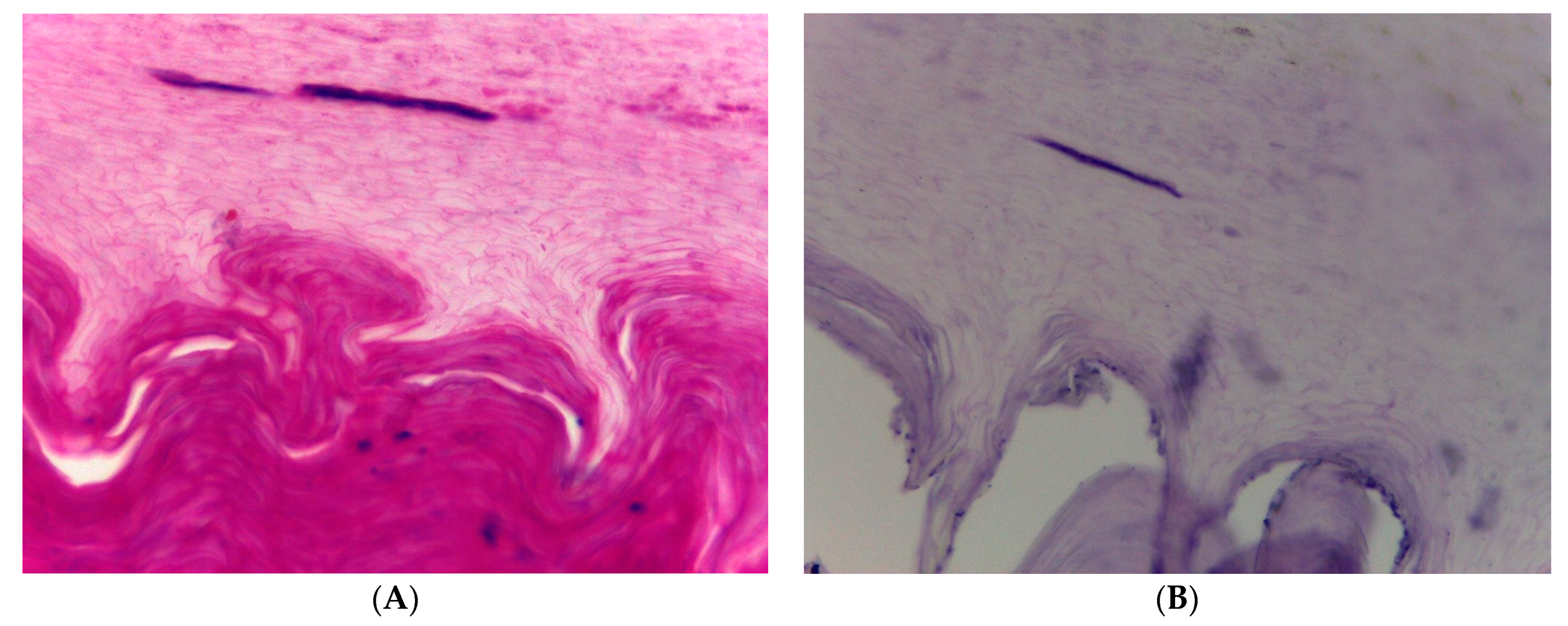
3. Results
4. Discussion
- Difficulties in making the correct clinical diagnosis;
- Problems with confirming the diagnosis by laboratory methods;
- Efficacious treatment of onychomycoses;
- Particular therapeutic challenges of post-traumatic single-digit onychomycoses.
5. Conclusions
6. Take-Home Message
- ▪
- Alterations of a single nail raise the suspicion of either a tumor or a trauma. The latter is usually remembered by the patient as this is commonly a painful event;
- ▪
- Involvement by a fungal infection of a single nail may have been triggered by a trauma that has long been forgotten;
- ▪
- The patient should be specifically asked for a previous trauma and mycologic examinations should be performed, as they may remain negative, the routine direct microscopy and culture should be complemented with histopathology or, if available, fungal PCR;
- ▪
- The pre-damaged nail may pose a considerable therapeutic challenge.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zaias, N.; Escovar, S.; Rebell, G. Opportunistic toenail onychomycosis. The fungal colonization of an available nail unit space by non-dermatophytes is produced by the trauma of the closed shoe by an asymmetric gait or other trauma. A plausible theory. J. Eur. Acad. Dermatol. Venereol. 2014, 28, 1002–1006. [Google Scholar] [CrossRef]
- Zaias, N.; Tosti, A.; Rebell, G.; Morelli, R.; Bardazzi, F.; Bieley, H.; Zaiac, M.; Glick, B.; Paley, B.; Allevato, M.; et al. Autosomal dominant pattern of distal subungual onychomycosis caused by Trichophyton rubrum. J. Am. Acad. Dermatol. 1996, 34, 302–304. [Google Scholar] [CrossRef] [PubMed]
- Daggett, C.; Brodell, R.T.; Daniel, C.R.; Jackson, J. Onychomycosis in athletes. Am. J. Clin. Dermatol. 2019, 20, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.R.; Algu, L.; Kamran, R.; Leveille, C.F.; Abid, K.; Rae, C.; Lipner, S.R. Effect of onychomycosis and treatment on patient-reported quality-of-life outcomes: A systematic review. J. Am. Acad. Dermatol. 2021, 85, 1227–1239. [Google Scholar] [CrossRef] [PubMed]
- Haneke, E. The potential risks of not treating onychomycosis. In Proceedings of the Second International Symposium on Onychomycosis; Gardiner Caldwell Comm Ltd.: Macclesfield, UK, 1996. [Google Scholar]
- Haneke, E.; Roseeuw, D. The scope of onychomycosis: Epidemiology and clinical features. Int. J. Dermatol. 1999, 38, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, A.A.; Friedman, A.J. Complex regional pain syndrome: What the dermatologist should know. J. Drugs Dermatol. 2018, 17, 532–536. [Google Scholar]
- Abeck, D.; Haneke, E.; Nolting, S.; Reinel, D.; Seebacher, C. Onychomykose: Aktuelle Daten zu Epidemiologie, Erregerspektrum, Risikofaktoren sowie Beeinflussung der Lebensqualität. Dtsch Ärztebl. 2000, 97, 1984–1986. [Google Scholar]
- Haneke, E. Pathogenesis of onychomycoses. Dermatology 1998, 197, 200–201. [Google Scholar]
- Baran, R.; Hay, R.J.; Tosti, A.; Haneke, E. A new classification of onychomycoses. Br. J. Dermatol. 1998, 139, 567–571. [Google Scholar] [CrossRef]
- Baran, R.; Hay, R.; Haneke, E.; Tosti, A. Onychomycosis, 2nd ed.; Taylor & Francis: Oxon, UK, 2006. [Google Scholar]
- Haneke, E. Nail biopsies in onychomycosis. Mykosen 1985, 28, 473–480. [Google Scholar] [CrossRef]
- Haneke, E. Bedeutung der Nagelhistologie für die Diagnostik und Therapie der Onychomykosen. Ärztl Kosmetol. 1988, 18, 248–254. [Google Scholar]
- Lawry, M.; Haneke, E.; Storbeck, K.; Martin, S.; Zimmer, B.; Romano, P. Methods for diagnosing onychomycosis: A comparative study and review of the literature. Arch. Dermatol. 2000, 136, 1112–1126. [Google Scholar] [CrossRef] [PubMed]
- Rammlmair, A.; Mühlethaler, K.; Haneke, E. Fusarium onychomycoses in Switzerland—A mycological and histopathological study. Mycoses 2019, 62, 928–931. [Google Scholar] [CrossRef] [PubMed]
- Trevisan, F.; Veasey, J.V.; Werner, B. Nail clipping with PAS stain and correlation with fungi isolated in culture: A valuable exchange in the diagnosis of onychomycosis. Skin Appendage Disord. 2022, 8, 399–405. [Google Scholar] [CrossRef]
- Piérard, G.E.; Quatresooz, P.; Arrese, J.E. Spotlight on nail histomycology. Dermatol. Clin. 2006, 24, 371–374. [Google Scholar] [CrossRef] [PubMed]
- Tsunemi, Y.; Hiruma, M. Clinical study of Dermatophyte Test Strip, an immunochromatographic method, to detect tinea unguium dermatophytes. J. Dermatol. 2016, 43, 1417–1423. [Google Scholar] [CrossRef] [PubMed]
- Ortner, V.K.; Franco, W.; Haedersdal, M.; Philipsen, P.A. Noninvasive assessment of mycotic nail tissue using an ultraviolet fluorescence excitation imaging system. Lasers Surg. Med. 2021, 53, 245–251. [Google Scholar] [CrossRef]
- Gupta, A.K.; Hall, D.C.; Cooper, E.A.; Ghannoum, M.A. Diagnosing onychomycosis: What‘s new? J. Fungi 2022, 8, 464. [Google Scholar] [CrossRef]
- Tsuboi, R.; Mochizuki, T.; Ito, H.; Kawano, S.; Suzuki, Y.; Naka, W.; Hata, Y.; Hamaguchi, T.; Maruyama, R. Validation of a lateral flow immunochromatographic assay for tinea unguium diagnosis. J. Dermatol. 2021, 48, 633–637. [Google Scholar] [CrossRef]
- Haneke, E. Nail surgery. Clin. Dermatol. 2013, 31, 516–525. [Google Scholar] [CrossRef]
- Grover, C.; Bansal, S.; Nanda, S.; Reddy, B.; Kumar, V. Combination of surgical avulsion and topical therapy for single nail onychomycosis: A randomized controlled trial. Br. J. Dermatol. 2007, 157, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Rocha, B.P.; Verardino, G.; Leverone, A.; D’Almeida, L.F.V.; Azulay, V.; Haneke, E.; Nakamura, R.C. Histopathological analysis of chronic paronychia. Int. J. Dermatol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Haneke, E. Toenails: Where orthopedics and onychology meet. In Advances in Nail Disease and Management; Updates in Clinical Dermatology; Baran, R., Ed.; Springer Nature: Cham, Switzerland, 2021; pp. 71–85. [Google Scholar]
- Haneke, E. Differential diagnosis of nail psoriasis and onychomycoses: A report based on 40 years of specialised nail consultations. EMJ Dermatol. 2020. [Google Scholar] [CrossRef]
- Haneke, E. The role of surgery in the treatment of onychomycosis. Z ästhet oper Dermatol. 2002, 3, 6–10. [Google Scholar]
- Gupta, A.K.; De Doncker, P.; Haneke, E. Itraconazole pulse therapy for the treatment of Candida onychomycosis. J. Eur. Acad. Dermatol. Venereol. 2001, 15, 112–115. [Google Scholar] [CrossRef]
- Gupta, A.K.; Renaud, H.J.; Quinlan, E.M.; Shear, N.H.; Piguet, V. The growing problem of antifungal resistance in onychomycosis and other superficial mycoses. Am. J. Clin. Dermatol. 2021, 22, 149–157. [Google Scholar] [CrossRef]
- Gupta, A.K.; Talukder, M.; Msc, M.V. Review of the alternative therapies for onychomycosis and superficial fungal infections: Posaconazole, fosravuconazole, voriconazole, oteseconazole. Int. J. Dermatol. 2022, 61, 1431–1441. [Google Scholar] [CrossRef]
- Shemer, A.; Eshel, Y.; Gupta, A.K.; Farhi, R.; Haneke, E.; Daniel, C.R.; Foley, K.; Quinlan, E.M. Once weekly application of urea 40% and bifonazole 1% leads to earlier nail removal in onychomycosis. Skin. Appendage Disord. 2020, 6, 304–308. [Google Scholar] [CrossRef]
- Haneke, E. Important malignant and new nail tumors. JDDG J. Dtsch. Dermatol. Ges. 2017, 15, 367–386. [Google Scholar] [CrossRef]



| p Value | ||
|---|---|---|
| Gender | F 30, M 14, total 44 | ns (0.9987) |
| Age range | 22–68 years | |
| Affected nail | Finger 39, toe 5 | p = 0.00116 |
| Previous mycologic cultures | Negative 40 (90.9%) Trichophyton rubrum 2 (4.5%) Non-dermatophyte mold 2 (4.5%) | p < 0.001 |
| Previous antifungal treatment | 34 with no substantial improvement (77.2%) | |
| Current diagnosis confirmed | 44 by histopathology (100%) 30 by culture (68.2%): 14 T. rubrum (31.8%) 1 T. mentagrophytes complex (2.3%) 15 non-dermatophyte molds (34.1%) | p < 0.0001 p = 0.006363 |
|
|
|
|
|
|
|
| Method | Advantage | Disadvantage |
|---|---|---|
| KOH without or with Parker ink or blancophore | Easy, rapid, cheap. | Relatively non specific, requires expertise. Blancophore requires fluorescence microscope. |
| Culture | Identification of fungus. | No differentiation between pathogen and colonizer. High percentage of biologically false negatives. |
| Histopathology (PAS, Grocott) | Differentiation of type of fungal infection, high yield of positives, differentiation between invasive onychomycosis and colonization, differential diagnoses possible. | No species identification. |
| Immunohistochemistry | Fungus identification? | Difficult on nail sections, few antibodies available. |
| Polymerase chain reaction | Identification of fungus, rapid. | No differentiation between pathogen and colonizer, expensive. |
| Immunochromatography | Easy to perform. Useful supplement for KOH. | Only for dermatophytes (T rubrum). |
| In situ hybridization | Localization of infection and pathogen identification (?). | No routine primers available. |
| MALDI-ToF mass spectroscopy | Species identification possible after culture. | Requires previous culture. Depends on fungal protein library. |
| Optical coherence tomography | Fungi may be detected. | Expensive. No species identification. |
| Confocal laser scanning microscopy | Fungi can be identified. | Expensive. No species identification. |
| Ultraviolet fluorescence excitation imaging | Immediate diagnosis of fungus infected nails possible. | Not yet available. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haneke, E.; Stovbyr, G. Post-Traumatic Single-Digit Onychomycosis. J. Fungi 2023, 9, 313. https://doi.org/10.3390/jof9030313
Haneke E, Stovbyr G. Post-Traumatic Single-Digit Onychomycosis. Journal of Fungi. 2023; 9(3):313. https://doi.org/10.3390/jof9030313
Chicago/Turabian StyleHaneke, Eckart, and Ganna Stovbyr. 2023. "Post-Traumatic Single-Digit Onychomycosis" Journal of Fungi 9, no. 3: 313. https://doi.org/10.3390/jof9030313
APA StyleHaneke, E., & Stovbyr, G. (2023). Post-Traumatic Single-Digit Onychomycosis. Journal of Fungi, 9(3), 313. https://doi.org/10.3390/jof9030313





