Mycotic Keratitis—A Global Threat from the Filamentous Fungi
Abstract
1. Introduction
2. Epidemiology of Fungal Keratitis
2.1. Incidence
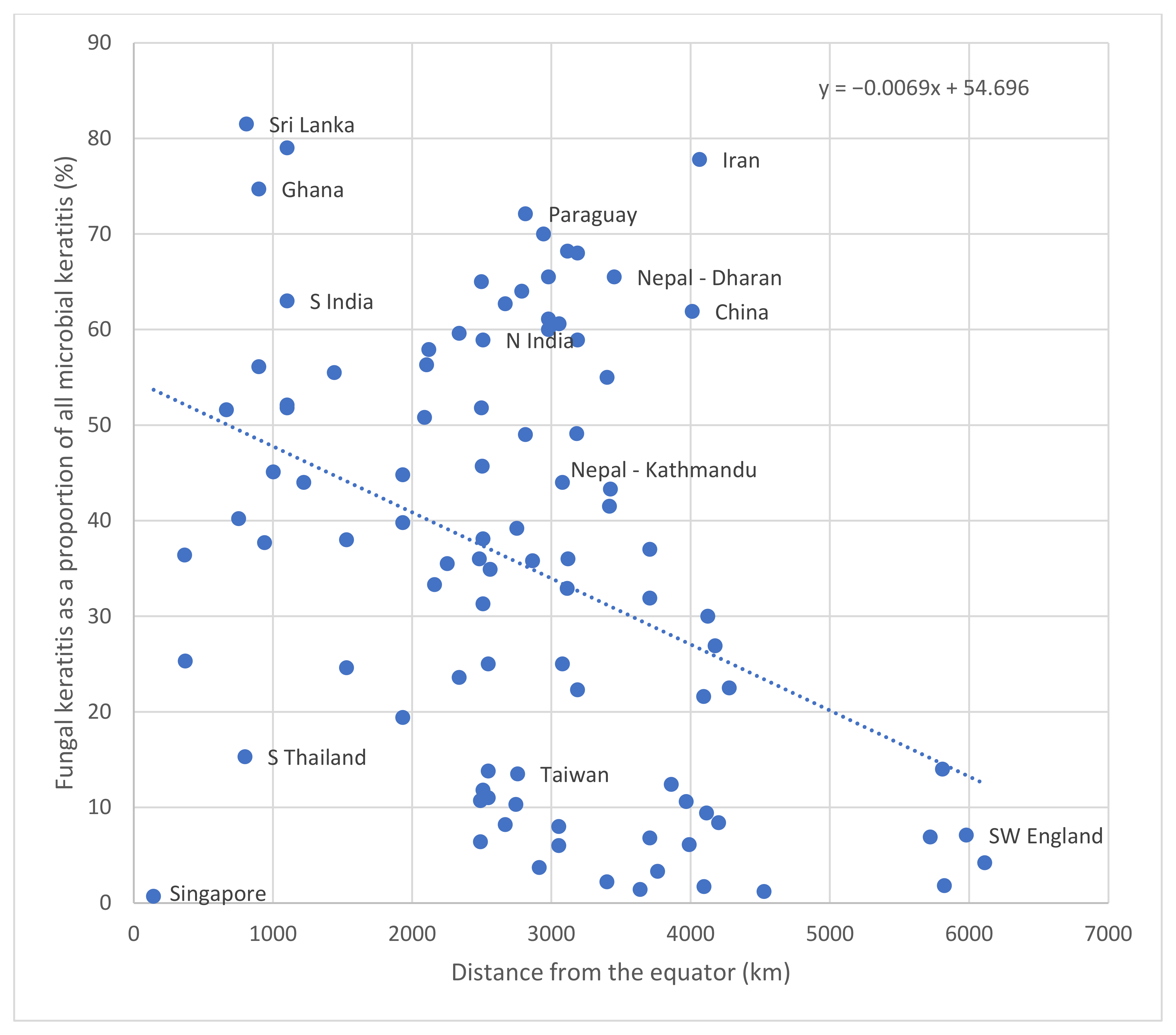
2.2. Geographical Distribution
| Country | Year | % FK # | % Culture Negative Cases ~ | Age (Mean) | % Male | % Trauma | % Steroid | % TEM | % CL | % OSD | % HIV | % DM | Distance from Equator (km) | N (All MK Cases) | Organism 1 (%) | Organism 2 (%) | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AFRICA | |||||||||||||||||
| Egypt (Zagazig) | 2012 | 55 | - | - | - | 63.6 | 6.1 | - | 12.1 | - | - | 18.2 | 3401 | 60 | Penicillium spp. (24.2) | Aspergillus spp. (21.2) | [37] |
| Egypt (Mansoura) | 2013–2015 | 65.5 | 55.5 | - | 66.1 | 51.4 | 5.3 | - | 2.4 | 4.5 | - | 15.1 | 3452 | 247 | Aspergillus (41.0) | - | [38] |
| Egypt (Tanta) | 2011–2013 | 43.3 | 15.5 | 49.2 | 65.9 | 58.4 | 32.7 | - | - | - | - | - | 3424 | 834 | Aspergillus flavus (29.1) | Aspergillus niger (16.1) | [39] |
| Ethiopia | 2014–2015 | 45.1 | - | - | 58.0 | 78.3 | 5.8 | - | - | - | - | 7.2 | 1003 | 153 | Fusarium spp. (27.6) | Aspergillus spp. (25.0) | [40] |
| Ghana | 1995 | 56.1 | 42.7 | 36.3 | 69.3 | - | - | - | - | - | - | - | 900 | 199 | Fusarium spp. (52.3) | Aspergillus spp. (15.3) | [41] |
| Ghana | 1999-2001 | 74.7 | 60.0 | - | - | - | - | - | - | - | - | - | 900 | 290 | Fusarium spp. (42.2) | Aspergillus spp. (17.4) | [7] |
| Libya | 2008–2010 | 32.9 | ^ | - | 60.7 | 78.5 | 3.6 | - | 21.4 | - | - | 17.8 | 3114 | 85 | Aspergillus spp. (50.0) | Fusarium spp. (39.3) | [42] |
| Sierra Leone | 2005–2006 | 37.7 | 5.5 | - | - | - | - | - | - | - | - | - | 941 | 73 | UFF (69.2) | Aspergillus spp. (15.4) | [35] |
| South Africa | 1982-1983 | 3.7 | - | - | - | 0 | 0 | - | 0 | - | 33.3 | 50.0 | 2913 | 164 | Curvularia spp. (33.3) | - | [43] |
| South Africa | 2013–2015 | 2.2 | - | - | - | - | - | - | - | - | - | - | 3399 | 46 | - | - | [44] |
| Tanzania | 2008–2010 | 51.6 | 45.6 | - | - | - | - | - | - | - | - | - | 667 | 170 | UFF (87.5) | Candida spp. (12.5) | [1] |
| Tanzania | 2013 | 40.2 | 8.9 | - | - | - | - | - | - | - | - | - | 755 | 202 | Candida spp. (60.8) | UFF (39.6) | [45] |
| Tunisia | 1995-2012 | 12.4 | 7 | 47.2 | 63.3 | 61.6 | 18.3 | 3.3 | 3.3 | 10.0 | - | 5 | 3862 | 483 | Fusarium spp. (49.0) | Aspergillus spp. (22.0) | [46] |
| Tunisia | 2010–2015 | 30.0 | 40 | 48.9 | 56.6 | 43.3 | 3.3 | - | 3.3 | - | - | 10 | 4124 | 30 | Fusarium spp. (50.0) | Aspergillus spp. (33.3) | [47] |
| Tunisia | 1996–2004 | 21.6 | 58 | - | - | 50.0 | - | - | - | 25 | - | - | 4094 | 100 | Fusarium spp. (87.5) | Acremonium spp. (12.5) | [48] |
| ASIA | |||||||||||||||||
| Bangladesh | 2008 | 39.2 | 5 | - | - | 49 | - | - | - | - | - | - | 2752 | 120 | - | - | [49] |
| Bangladesh | 1994 | 36 | 18.3 | - | - | - | - | - | - | - | - | - | 2483 | 142 | Aspergillus spp. (40.0) | Fusarium spp. (21.0) | [50] |
| China | 2009–2013 | 45.7 | 53.9 | - | - | - | - | - | - | - | - | - | 2504 | 2973 | Fusarium spp. (29.3) | Aspergillus spp. (24.1) | [51] |
| China | 1999-2004 | 61.9 | - | - | - | - | - | - | - | - | - | - | 4012 | 1054 | Fusarium spp. (73.3) | Aspergillus spp. (12.1) | [52] |
| China (Hong Kong) | 1997-1998 | 6.4 | 65.0 | - | - | 20 | 20 | - | - | - | - | - | 2491 | 223 | Fusarium spp. (60.0) | Penicillium spp. (20.0) | [53] |
| China (Hong Kong) | 2004–2013 | 10.7 | 67.7 | - | - | - | - | - | - | - | - | - | 2491 | 260 | Fusarium spp. (33.3) | Candida spp. (25.0) | [54] |
| China (Taiwan) | 1992-2001 | 13.5 | 51.0 | - | - | - | - | - | - | - | - | - | 2758 | 453 | Fusarium spp. (29.4) | Candida spp. (29.4) | [55] |
| China (Taiwan) | 2012–2014 | 8.2 | 69 | - | - | - | - | - | - | - | - | - | 2669 | 233 | - | - | [56] |
| India (West Bengal) | 2007–2011 | 58.9 | 27.0 | - | 61.7 | 88.7 | 16.3 | - | - | 6.0 | - | 11.8 | 2510 | 928 | Aspergillus spp. (37.8) | Fusarium spp. (20.3) | [57] |
| India (West Bengal) | 2008 | 38.1 | 32.7 | 53 | 65.0 | 48.0 | 16.0 | 16.0 | - | - | - | - | 2510 | 289 | Aspergillus spp. (55.4) | Fusarium spp. (10.8) | [58] |
| India (Odisha) | 2006–2009 | 35.5 | 18.6 | - | 70.0 | 40.2 | - | - | - | - | - | 2.2 | 2253 | 997 | Aspergillus spp. (27.9) | Fusarium spp. (23.2) | [59] |
| India (Assam) | 2007–2009 | 60.6 | - | - | 68.8 | 76.40 | - | - | - | 1.5 | - | 2.5 | 3056 | 310 | Fusarium spp. (25.0) | Aspergillus spp. (19.0) | [60] |
| India (Delhi) | 2010–2015 | 68 | 65 | - | 76 | 89.4 | - | - | - | 5.3 | - | 1.3 | 3188 | 400 | Aspergillus spp. (30.8) | Fusarium spp. (27.6) | [61] |
| India (Chandigarh) | 2005–2011 | Ψ | 49 | - | - | 66.5 | 2 | - | - | 11.7 | - | - | 3418 | 765 | Aspergillus spp. (47.6) | Dematiaceous fungi (21.9) | [62] |
| India (Rajasthan) | 2005–2012 | 68.2 | 45 | - | 71.7 | 62.8 | - | - | 3.9 | - | 1.1 | 8.9 | 3116 | 480 | Aspergillus spp. (63.3) | Alternaria spp. (8.3) | [63] |
| India (Chandigarh) | 1999-2003 | 41.5 | 46.9 | - | 80.5 | 43.8 | 7.8 | - | - | - | - | - | 3418 | 64 | Aspergillus spp. (41.2) | Fusarium spp. (23.5) | [64] |
| India (Delhi) | 2007–2011 | 58.9 | 27 | - | 61.7 | 88.7 | 16.3 | - | - | 19 | - | 11.8 | 3188 | 928 | Aspergillus spp. (37.8) | Dematiaceous fungi (23.8) | [65] |
| India (Delhi) | 2000–2004 | 22.3 | - | - | 77.9 | 32.4 | 16.2 | 2.7 | 0 | - | - | - | 3188 | 346 | Aspergillus spp. (55.9) | Dematiaceous fungi (7.8) | [66] |
| India (Madurai) | 2012–2013 | 79 | 14.5 | 50 | 64 | 70 | 9 | 19 | 8 | 1103 | 252 | Fusarium spp. (39.0) | Aspergillus spp. (18.0) | [67] | |||
| India (Madurai) | 1999–2002 | 52.1 | 29.4 | - | 65 | 92.1 | 1.2 | - | 0 | 6.7 | - | 15.7 | 1103 | 3183 | Fusarium spp. (41.9) | Dematiaceous fungi (26.9) | [68] |
| India (Madurai) | 1994 | 51.8 | 31.6 | - | 61.3 | - | - | - | - | - | - | - | 1103 | 434 | Fusarium spp. (47.1) | Aspergillus spp. (16.1) | [4] |
| India (Hyderabad) | 1991–2000 | 39.8 | ^ | 40.4 | 71.2 | 54.4 | 5.9 | - | - | 11.7 | - | 6.4 | 1933 | 3399 | Fusarium spp. (37.2) | Aspergillus spp. (30.7) | [69] |
| India (Hyderabad) | 1991–2001 | 44.8 | 39.6 | 30.9 | - | 81.9 | 2.4 | - | 0.3 | 18.2 | - | - | 1933 | 5897 | Fusarium spp. (35.6) | Aspergillus spp. (26.8) | [70] |
| India (Madurai) | 2006–2009 | 63 | 42 | - | - | - | - | - | - | - | - | - | 1103 | 6967 | Fusarium spp. (42.3) | - | [71] |
| India (Bangalore) | 2012–2014 | 55.5 | 62.5 | - | - | - | - | - | - | - | - | 1442 | 312 | Fusarium spp. (31.0) | Aspergillus spp. (11.0) | [72] | |
| India (Tamil Nadu) | 1999–2001 | 44 | 31 | - | - | - | - | - | - | - | - | - | 1223 | 800 | Aspergillus spp. (39.9) | Fusarium spp. (21.5) | [7] |
| India (Maharashtra) | 2004–2009 | 57.9 | 37 | - | - | - | - | - | - | - | - | - | 2120 | 852 | Fusarium spp. (35.0) | Aspergillus spp. (18.0) | [12] |
| India (Gujarat) | 2006–2008 | 65 | 60 | 54 | 73 | - | - | - | - | - | - | 2498 | 100 | Aspergillus spp. (70.0) | Fusarium spp. (12.0) | [73] | |
| India (Gujarat) | 2003–2005 | 51.8 | 45 | - | - | - | - | - | - | - | - | - | 2498 | 200 | Fusarium spp. (29.8) | Aspergillus spp. (21.1) | [74] |
| India (Gujarat) | 2007–2008 | 34.9 | 40.7 | - | - | - | - | - | - | - | - | - | 2561 | 150 | Aspergillus spp. (35.4) | Fusarium spp. (22.5) | [75] |
| India (West Bengal) | 2001–2003 | 62.7 | 32 | - | - | - | - | - | - | - | - | - | 2669 | 1198 | Aspergillus spp. (59.9) | Fusarium spp. (21.2) | [76] |
| India (Delhi) | 2005 | 49.1 | 43.2 | - | - | - | - | - | - | - | - | - | 3183 | 1000 | Aspergillus spp. (41.6) | Fusarium spp. (19.8) | [77] |
| India (Hyderabad) | 2002 | 19.4 | 33.5 | - | - | - | - | - | - | - | - | - | 1933 | 170 | Fusarium spp. (72.7) | - | [78] |
| Iran (Tehran) | 2011–2013 | Ψ | 94.4 | 79.3 | - | - | - | - | - | - | - | 3969 | 2180 | Fusarium spp. (49.6) | Aspergillus spp. (26.4) | [79] | |
| Iran (Sari) | 2004–2005 | 77.8 | 59.1 | 61.5 | 71.4 | 28.6 | 0 | - | 0 | 14.3 | - | 14.3 | 4065 | 22 | Fusarium spp. (50.0) | Aspergillus spp. (50.0) | [80] |
| Iraq | 2002–2005 | 31.9 | 41.4 | - | - | 90 | - | - | 0 | 6.8 | - | - | 3707 | 396 | Aspergillus spp. (56.8) | Fusarium spp. (27.0) | [81] |
| Iraq | 2013–2014 | 6.8 | 30.5 | - | - | - | - | - | - | - | - | - | 3707 | 105 | Aspergillus spp. (60.0) | Alternaria spp. (40.0) | [82] |
| Iraq | 2017–2018 | 37 | ^ | 73 | 61 | - | - | - | - | - | - | 41 | 3707 | 234 | Aspergillus spp. (70.0) | Penicillium spp. (13.0) | [83] |
| Japan | 1999–2003 | 6.1 | 41.5 | - | - | - | - | - | - | - | - | - | 3991 | 122 | Candida spp. (83.3) | - | [84] |
| Japan | 2003 | 10.6 | 56.7 | - | - | - | - | - | - | - | - | - | 3969 | 261 | - | - | [85] |
| Korea (RO) | 2003–2008 | 26.9 | 37.3 | - | - | - | - | - | - | - | - | - | 4177 | 83 | Candida spp. (57.0) | Aspergillus spp. (28.6) | [86] |
| Malaysia | 2007–2011 | 25.3 | 12.8 | - | 61.7 | 48.9 | 17.0 | - | 4.3 | 10.6 | - | 10.6 | 371 | 186 | Fusarium spp. (46.0) | Aspergillus spp. (9.8) | [87] |
| Malaysia | 2017 | 36.4 | 59.9 | - | - | - | - | - | - | - | - | - | 367 | 137 | Fusarium spp. (60.0) | - | [88] |
| Nepal (Dharan) | 2004–2008 | 61.1 | 20.8 | - | - | - | - | - | - | 2980 | 351 | Aspergillus spp. (33.3) | Fusarium spp. (12.7) | [89] | |||
| Nepal (Dharan) | 1998–1999 | 65.5 | 32.6 | - | - | - | - | - | - | - | - | - | 2980 | 86 | Aspergillus spp. (60.5) | Fusarium spp. (13.2) | [90] |
| Nepal (Nepalgunj) | 2011–2012 | 36 | ^ | - | 59.3 | 58 | 12 | - | - | 6 | - | - | 3120 | 1880 | Fusarium spp. (31.9) | Curvularia spp. (17.7) | [91] |
| Nepal (Dharan) | 2007–2008 | 60 | 54.5 | - | - | - | - | - | - | - | - | - | 2980 | 44 | Aspergillus spp. (66.6) | - | [92] |
| Nepal (Kathmandu) | 2014 | 44 | 55.4 | - | - | - | - | - | - | - | - | - | 3080 | 101 | Fusarium spp. (24.0) | Aspergillus spp. (20.0) | [93] |
| Nepal (Kathmandu) | 1981 | 25 | 50 | - | - | - | - | - | - | - | - | - | 3080 | 133 | - | - | [94] |
| Nepal (Biratnagar) | 2011 | 70 | - | - | - | - | - | - | - | - | - | 2944 | 1644 | No culture performed, microscopy only | [95] | ||
| Oman | 2004–2007 | 31.3 | 57.9 | - | 59.4 | 25 | 31.3 | 15.6 | - | 18.8 | - | 9.4 | 2510 | 242 | Fusarium spp. (50.0) | Aspergillus spp. (34.4) | [96] |
| Oman | 2000–2006 | 11.8 | 56.9 | - | - | - | - | - | - | - | - | - | 2510 | 188 | - | - | [97] |
| Pakistan | 2010 | 64 | 32.3 | - | - | - | - | - | - | - | - | - | 2788 | 133 | - | - | [98] |
| Saudi Arabia | 1984–2004 | 10.3 | 69.4 | 55 | 79 | 20.9 | 16.9 | - | 0.8 | 8.87 | - | 12 | 2746 | 1200 | Aspergillus spp. (37.0) | Trichophyton spp. (20.0) | [99] |
| Singapore | 1991–2005 | Ψ | ^ | 40 | 79.3 | 55 | 24 | - | 7 | 14 | - | - | 143 | 29 | Fusarium spp. (52.0) | Aspergillus spp. (17.0) | [100] |
| Singapore | 2012–2014 | 0.7 | - | - | - | - | - | - | - | - | - | - | 143 | 531 | - | - | [56] |
| Sri Lanka | 1976–1981 | 81.5 | 59.1 | - | - | - | - | - | - | - | - | - | 811 | 66 | UFF (63.6) | Aspergillus spp. (18.0) | [36] |
| Thailand (Central) | 1988–2000 | 24.6 | 52.7 | - | - | - | - | - | - | - | - | - | 1529 | 292 | Fusarium spp. (34.3) | Aspergillus spp. (20.0) | [101] |
| Thailand (South) | 1982–2003 | 15.3 | - | 46.4 | 72.3 | 66 | - | - | - | - | - | - | 800 | 556 | Fusarium spp. (64.5) | Aspergillus spp. (10.5) | [102] |
| Thailand (North) | 2003–2006 | 50.8 | 74.4 | - | - | - | - | - | - | - | - | - | 2090 | 305 | Fusarium spp. (58.1) | Aspergillus spp. (12.9) | [103] |
| Thailand (Central) | 2001–2004 | 38 | ^ | - | 67.7 | 77.5 | - | - | 0 | 9.68 | - | - | 1529 | 127 | Fusarium spp. (26.0) | Dematiaceous fungi (20.0) | [104] |
| Turkey (Adana) | 2014–2015 | 9.4 | - | 39.3 | 50 | 50 | - | - | 25 | - | - | - | 4115 | 64 | Aspergillus spp. (66.7) | Fusarium spp. (33.3) | [105] |
| Turkey (West Anatolia) | 1990–2005 | 22.5 | 63.8 | - | - | - | - | - | - | - | - | - | 4278 | 620 | Fusarium spp. (50.0) | Aspergillus spp. (20.0) | [106] |
| Vietnam (North) | 2008 | 59.6 | 47.2 | - | 44.1 | 83.8 | 1.4 | 1.4 | - | - | - | - | 2338 | 1153 | Fusarium spp. (40.7) | Aspergillus spp. (25.9) | [30] |
| Vietnam | 1974–1982 | 23.6 | - | - | - | - | - | - | - | - | - | - | 2338 | 1219 | - | - | [107] |
| EUROPE | |||||||||||||||||
| Netherlands | 2002–2004 | 1.8 | 42.0 | - | - | - | - | - | - | 50 | 50 | - | 5823 | 156 | Candida albicans (100) | - | [108] |
| Netherlands | 2014–2017 | 14.0 | 50 | - | - | - | - | - | - | - | - | - | 5809 | 185 | - | - | [34] |
| UK (SW England) | 2006–2017 | 6.9 | 61.9 | - | - | - | - | - | - | - | - | - | 5721 | 2116 | UFF (54.2) | Candida spp. (45.8) | [109] |
| UK (London) | 2007–2014 | - | 34.8 | 47.2 | 41.4 | 11.6 | 32.1 | - | 57.1 | 22.3 | - | - | 5727 | 112 | Fusarium spp. (41.8) | Candida spp. (38.0) | [28] |
| UK (NE England) | 2008–2017 | 4.2 | 55.5 | 55.3 | 65 | - | - | - | - | - | - | - | 6113 | 407 | UFF (50.0) | Candida spp. (50.0) | [110] |
| UK – (NW England) | 2004–2015 | 7.1 | 67.4 | - | - | - | - | - | - | - | - | - | 5980 | 4229 | Candida spp. (53.2) | Fusarium spp. (25.7) | [111] |
| LATIN AMERICA AND THE CARRIBEAN | |||||||||||||||||
| Brazil (São Paulo) | 1975–2007 | 11 | 51.4 | - | - | - | - | - | - | - | - | - | 2547 | 6804 | Fusarium spp. (51.9) | Candida spp. (17.6) | [112] |
| Brazil (Uberlandia) | 2001–2004 | 56.3 | 50.8 | - | - | 55.6 | - | - | 0 | 0 | - | - | 2104 | 65 | Fusarium spp. (61.1) | Aspergillus spp. (16.7) | [113] |
| Brazil (São Paulo) | 2000–2004 | 13.8 | 63.4 | 40.7 | 80.3 | - | - | - | - | - | - | - | 2547 | 478 | Fusarium spp. (66.7) | Aspergillus spp. (10.6) | [114] |
| Brazil (São Paulo) | 2003–2010 | 25 | 82.4 | 43 | 74 | 49.3 | - | - | - | - | - | - | 2547 | 599 | Fusarium spp. (83.3) | Aspergillus spp. (16.7) | [115] |
| Mexico | 2013–2014 | 33.3 | 47.1 | - | - | - | - | - | - | - | - | - | 2161 | 51 | Fusarium spp. (44.4) | Aspergillus spp. (22.2) | [116] |
| Paraguay | 1988–2001 | 49 | 21 | - | - | - | - | - | - | - | - | - | 2814 | 660 | Acremonium spp. (40.0) | Fusarium spp. (15.0) | [117] |
| Paraguay | 2009–2011 | 72.1 | 10.4 | - | 71 | - | - | - | - | - | - | - | 2814 | 48 | Fusarium spp. (34.0) | Aspergillus spp. (16.1) | [118] |
| NORTH AMERICA | |||||||||||||||||
| USA (N California) | 1976–1999 | 8.4 | 62 | - | - | - | - | - | - | - | - | - | 4201 | 1121 | Candida spp. (30.5) | - | [119] |
| USA (Florida) | 1968–1977 | 35.8 | 44.0 | - | - | - | - | - | - | - | - | - | 2865 | 663 | Fusarium spp. (62.0) | Candida spp. (7.5%) | [120] |
| USA (Florida) | 1999–2006 | - | 29.8 | 48 | 75 | 43 | 29 | - | 44 | 8.3 | - | 7.1 | 3298 | 84 | Fusarium spp. (41.0) | Candida spp. (14.0) | [121] |
| USA (S California) | 1998–2008 | 1.4 | ^ | 56.1 | 54 | 14 | - | - | 24 | 12.7 | 1.6 | 16 | 3638 | 4651 | UFF (64.0) | Candida spp. (32.0) | [122] |
| USA (New York) | 1987–2003 | 1.2 | ^ | 47 | 35 | 11 | 7 | - | 10 | 23 | 25 | 7 | 4528 | 5083 | Candida spp. (66.0) | Aspergillus spp. (12.0) | [33] |
| OCEANIA | |||||||||||||||||
| Australia (Brisbane) | 1999–2004 | 8 | 35 | - | - | - | - | - | - | - | - | - | 3054 | 231 | Fusarium spp. most commonly isolated | - | [123] |
| Australia (Queensland) | 1996–2016 | - | ^ | 48 | 65 | - | - | - | - | - | - | - | 3054 | 215 | Fusarium spp. (33.3) | Aspergillus spp. (13.0) | [124] |
| Australia (Sydney) | 2009–2017 | - | 6 | 60 | 65 | 24 | 54 | - | 26 | 34 | - | - | 3764 | 51 | Candida spp. (33.0) | Fusarium spp. (28.0) | [125] |
| Australia (Queensland) | 2005–2015 | 6 | ^ | - | - | - | - | - | - | - | - | - | 3054 | 3182 | UFF (75.9) | Candida spp. (24.1) | [126] |
| Australia (Sydney) | 2012–2016 | 3.3 | 31 | 63.5 | 67 | 25 | 46 | - | 28 | 25 | - | 8 | 3764 | 1052 | Candida spp. (30.4) | Fusarium spp. (21.7) | [127] |
| New Zealand | 2003–2007 | 1.7 | 34.4 | - | - | - | - | - | - | - | - | - | 4097 | 265 | Fusarium spp. (66.7) | Candida spp. (33.3) | [128] |
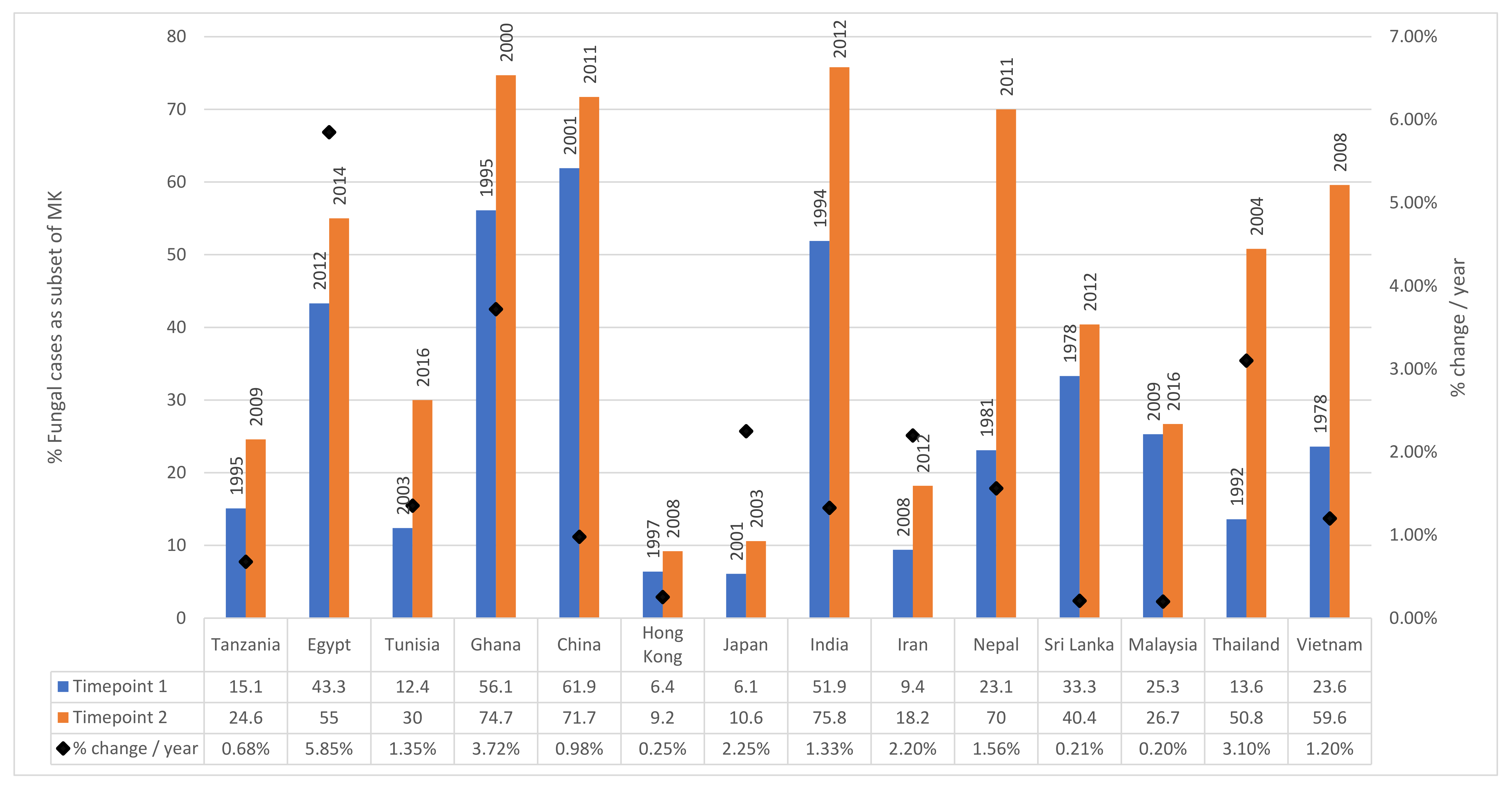
2.3. Changing Incidence over Time
2.4. Risk Factors
2.4.1. Age and Gender
2.4.2. Trauma
2.4.3. Occupation
2.4.4. Diabetes Mellitus
2.4.5. HIV
2.4.6. Traditional Eye Medicine
2.4.7. Topical Corticosteroids
2.4.8. Ocular Surface Disease
2.4.9. Contact Lens Usage
2.4.10. Previous Ocular Surgery
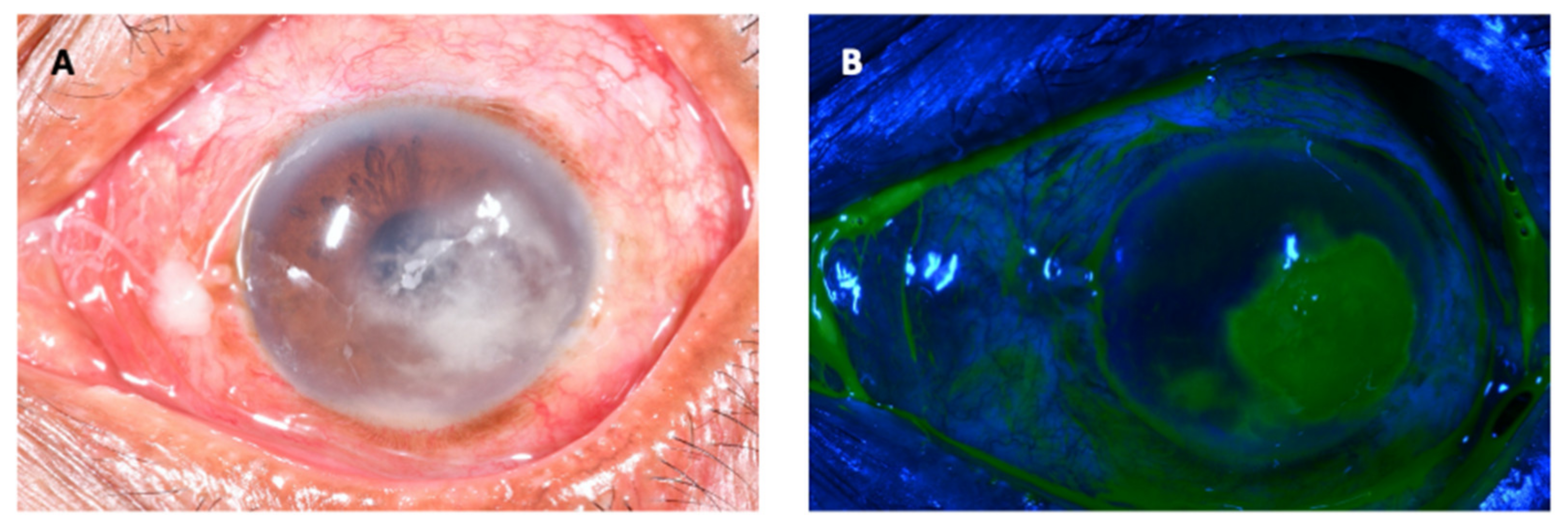
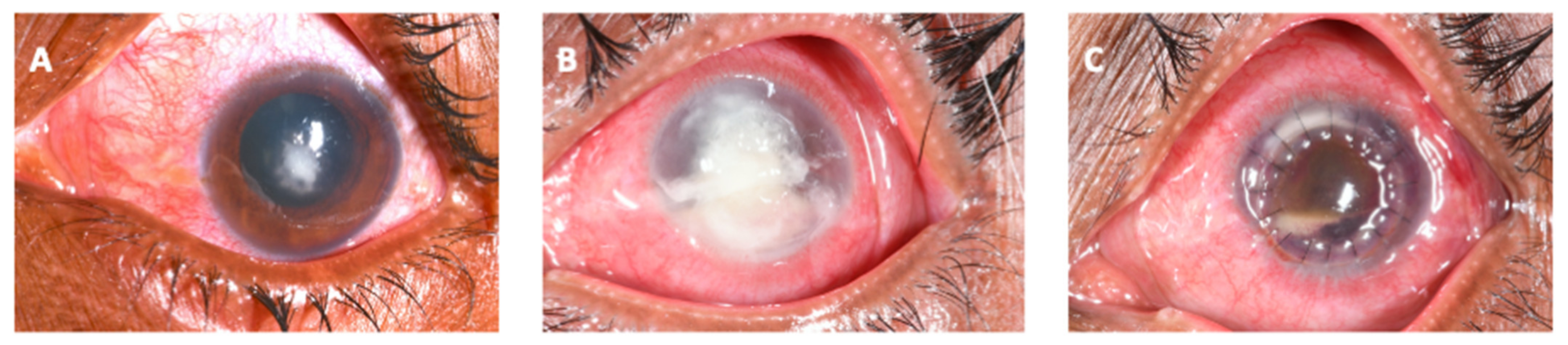
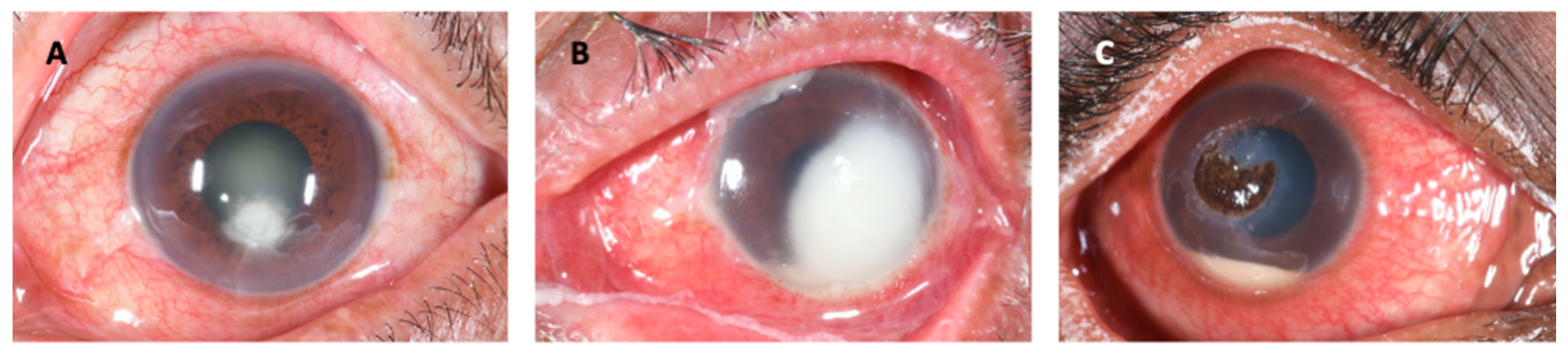
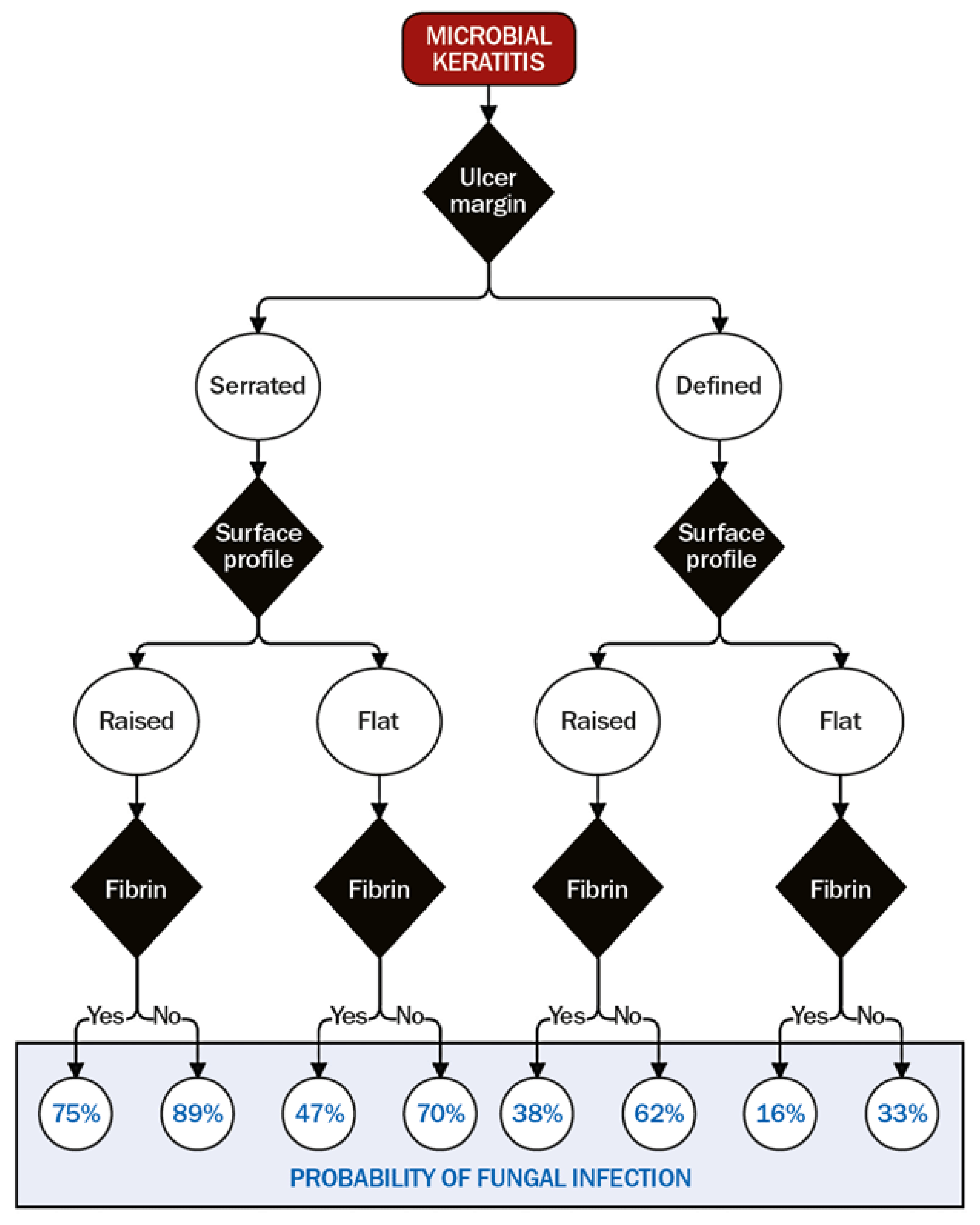
3. Clinical Features
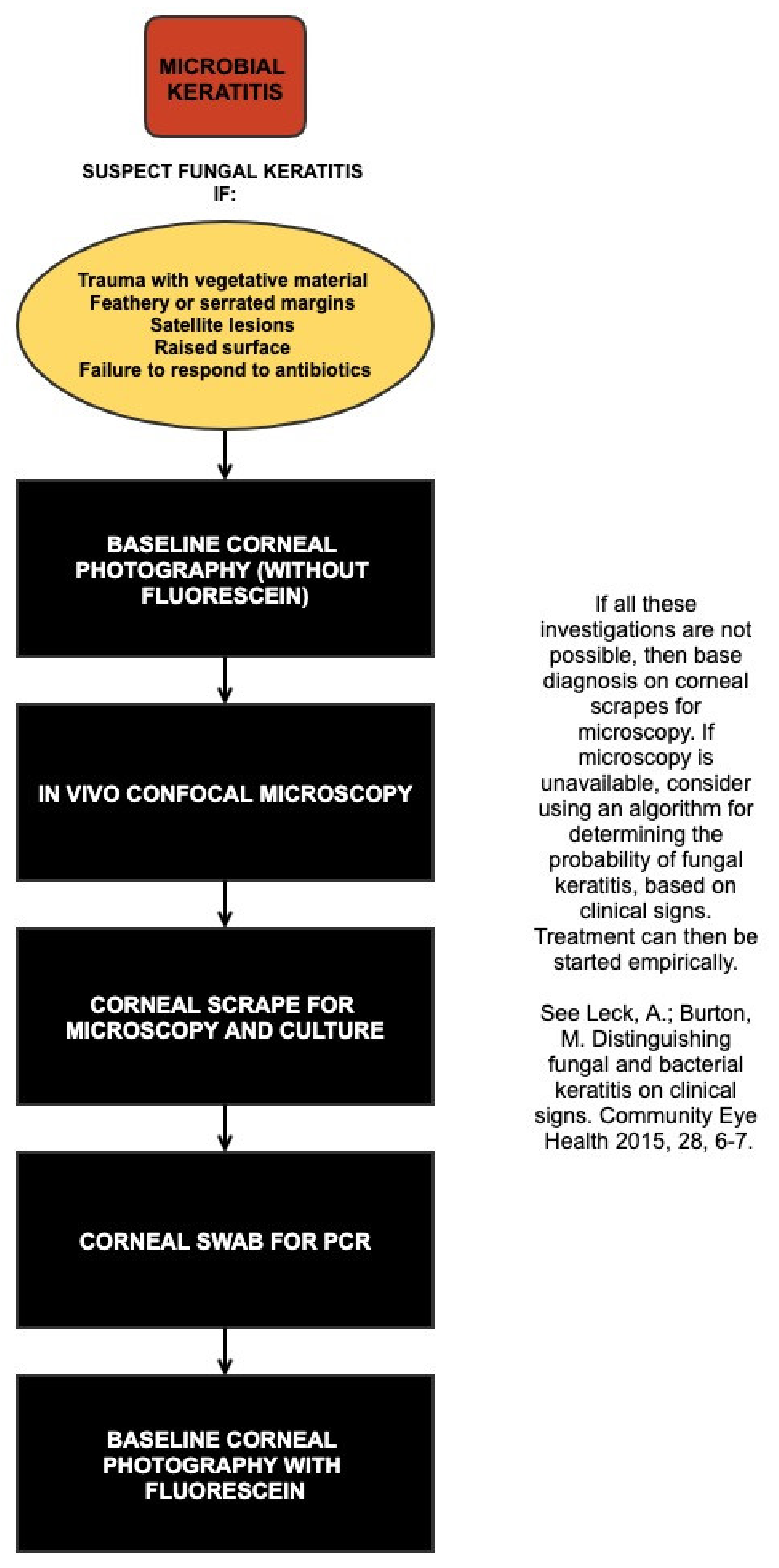
4. Making the Diagnosis
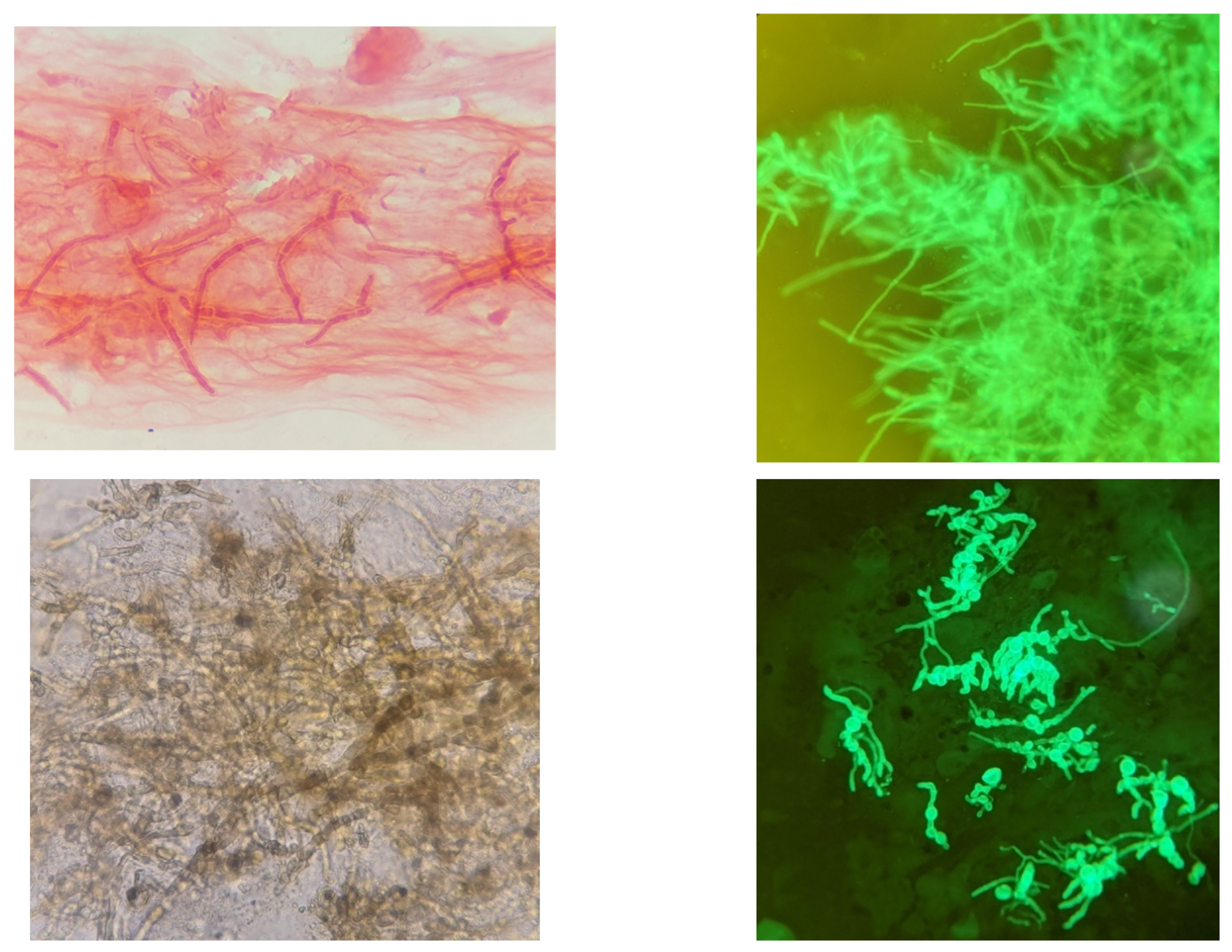
4.1. Laboratory
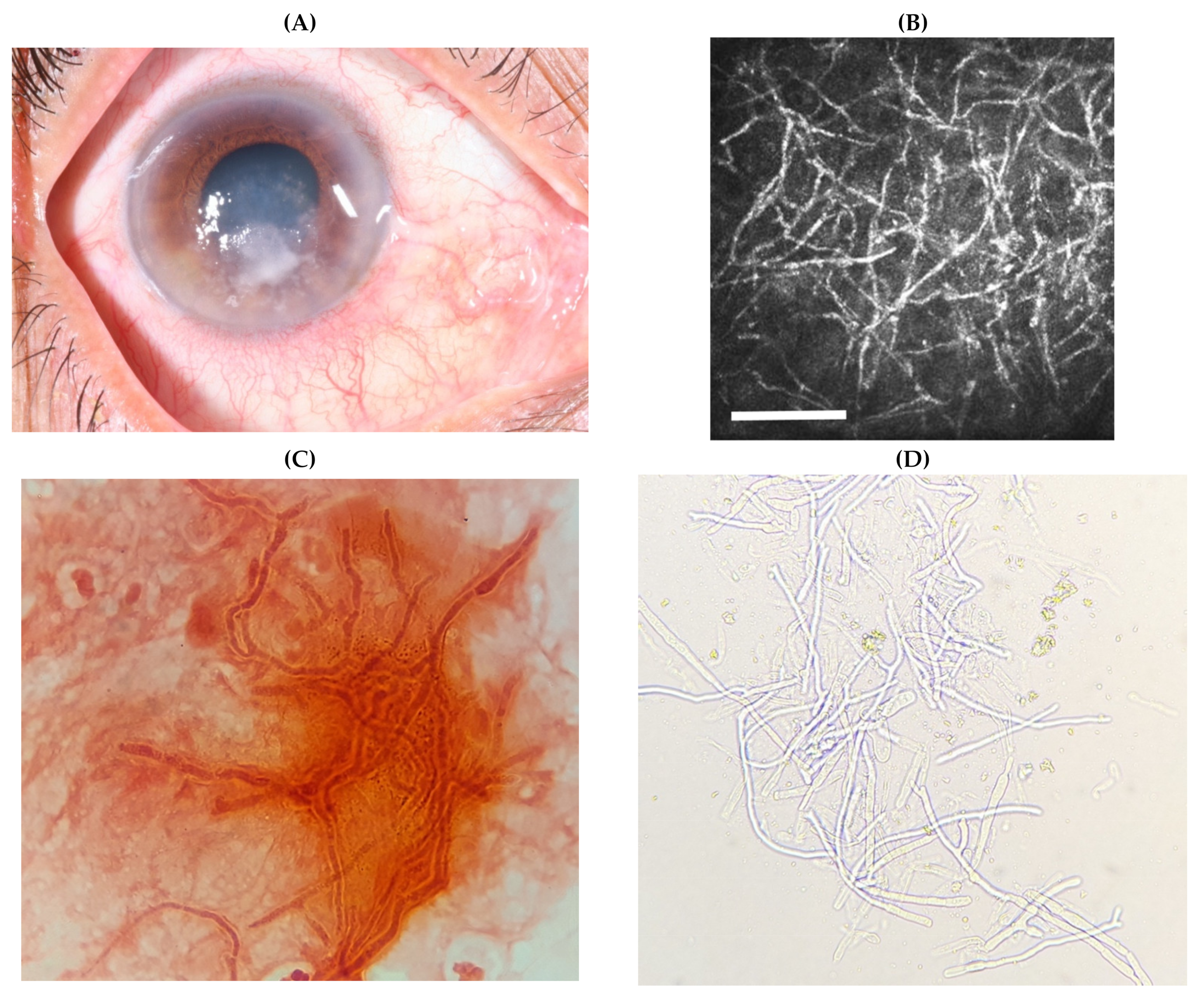
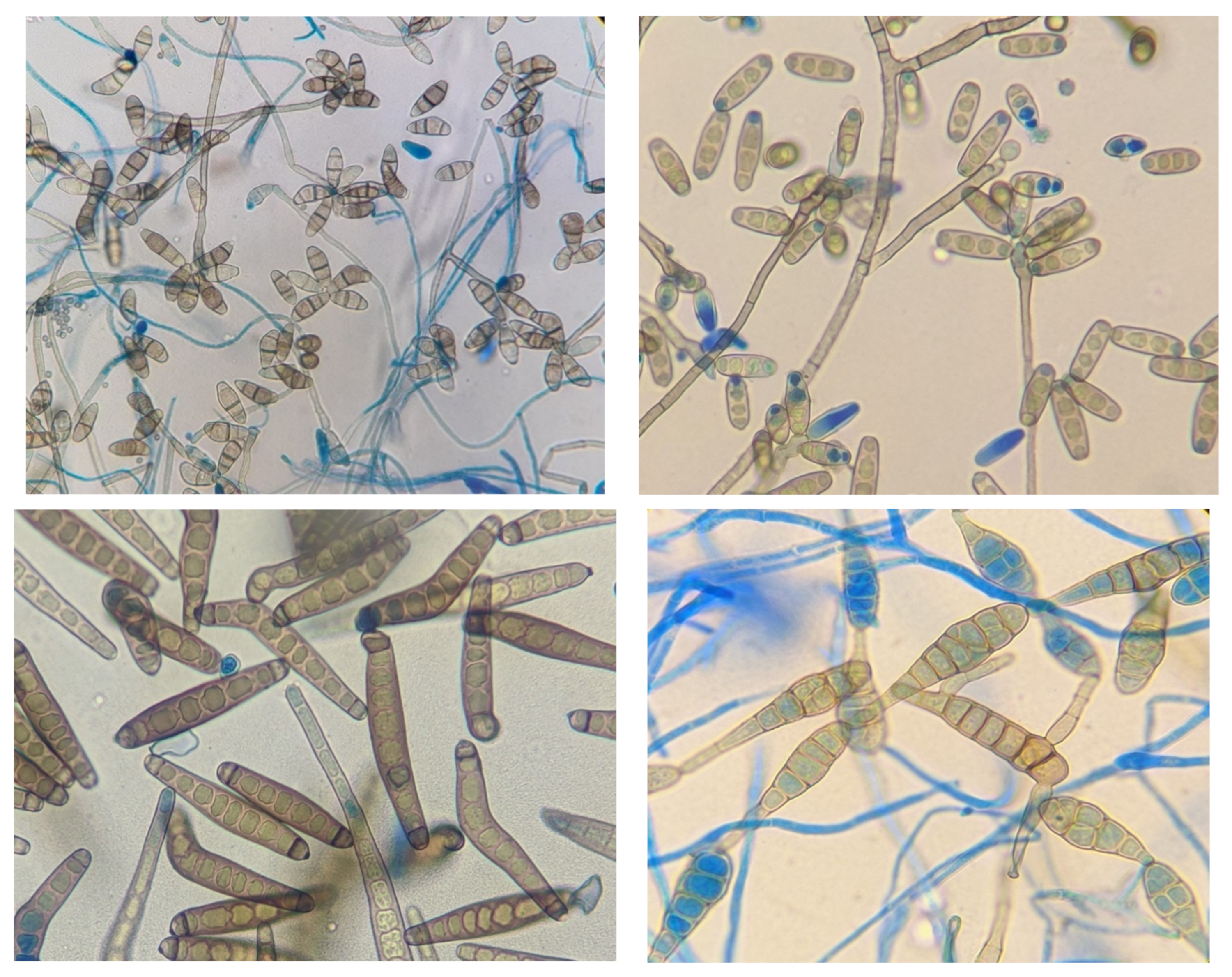
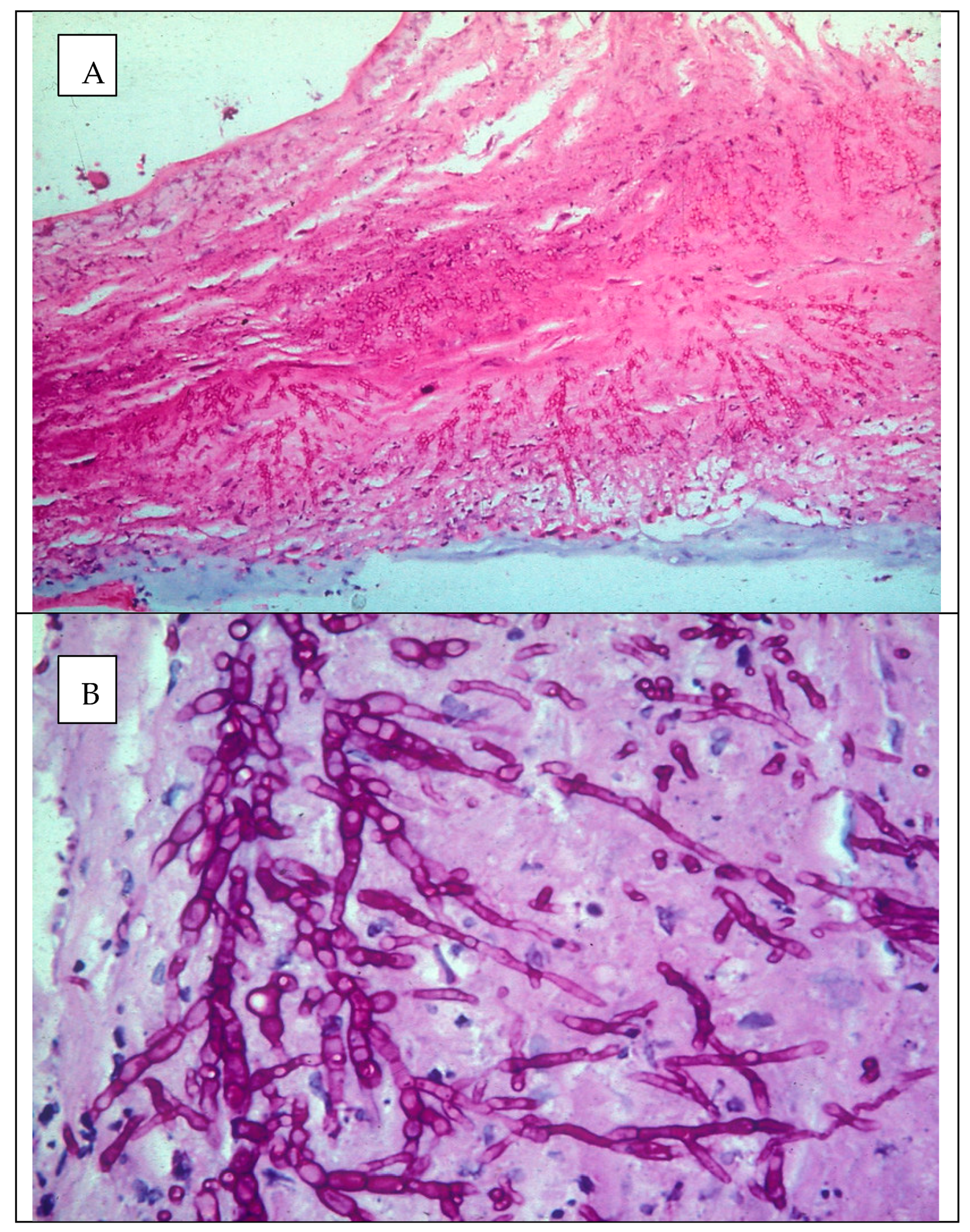
4.1.1. Microscopy and Culture
4.1.2. Molecular Techniques
4.1.3. In Vivo Confocal Microscopy
4.1.4. Systematic Approach to Making a Diagnosis
5. Management
6. Ocular Mycology
6.1. Fusarium spp.
Epidemiology
6.2. Aspergillus sp.
Epidemiology
6.3. Dematiaceous Fungi
Epidemiology
6.4. Other Filamentous Fungi
7. Unsolved Problems and Future Work
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Burton, M.J.; Pithuwa, J.; Okello, E.; Afwamba, I.; Onyango, J.J.; Oates, F.; Chevallier, C.; Hall, A.B. Microbial Keratitis in East Africa: Why are the Outcomes so Poor? Ophthalmic Epidemiol. 2011, 18, 158–163. [Google Scholar] [CrossRef]
- Thomas, P.A.; Leck, A.K.; Myatt, M. Characteristic clinical features as an aid to the diagnosis of suppurative keratitis caused by filamentous fungi. Br. J. Ophthalmol. 2005, 89, 1554–1558. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.; Leck, A.K.; Gichangi, M.; Burton, M.J.; Denning, D.W. The global incidence and diagnosis of fungal keratitis. Lancet Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Srinivasan, M.; Gonzales, C.A.; George, C.; Cevallos, V.; Mascarenhas, J.M.; Asokan, B.; Wilkins, J.; Smolin, G.; Whitcher, J.P. Epidemiology and aetiological diagnosis of corneal ulceration in Madurai, south India. Br. J. Ophthalmol. 1997, 81, 965–971. [Google Scholar] [CrossRef] [PubMed]
- Whitcher, J.P.; Srinivasan, M.; Upadhyay, M.P. Corneal blindness: A global perspective. Bull. World Health Organ. 2001, 79, 214–221. [Google Scholar]
- Bongomin, F.; Gago, S.; Oladele, R.O.; Denning, D.W. Global and Multi-National Prevalence of Fungal Diseases-Estimate Precision. J. Fungi 2017, 3, 57. [Google Scholar] [CrossRef]
- Leck, A.K.; Thomas, P.A.; Hagan, M.; Kaliamurthy, J.; Ackuaku, E.; John, M.; Newman, M.J.; Codjoe, F.S.; Opintan, J.A.; Kalavathy, C.M.; et al. Aetiology of suppurative corneal ulcers in Ghana and south India, and epidemiology of fungal keratitis. Br. J. Ophthalmol. 2002, 86, 1211–1215. [Google Scholar] [CrossRef] [PubMed]
- Qiao, G.L.; Ling, J.; Wong, T.; Yeung, S.N.; Iovieno, A. Candida Keratitis: Epidemiology, Management, and Clinical Outcomes. Cornea 2020, 39, 801–805. [Google Scholar] [CrossRef]
- Ahearn, D.G.; Zhang, S.; Stulting, R.D.; Schwam, B.L.; Simmons, R.B.; Ward, M.A.; Pierce, G.E.; Crow, S.A., Jr. Fusarium keratitis and contact lens wear: Facts and speculations. Med. Mycol. 2008, 46, 397–410. [Google Scholar] [CrossRef]
- Walther, G.; Stasch, S.; Kaerger, K.; Hamprecht, A.; Roth, M.; Cornely, O.A.; Geerling, G.; Mackenzie, C.R.; Kurzai, O.; von Lilienfeld-Toal, M. Fusarium Keratitis in Germany. J. Clin. Microbiol. 2017, 55, 2983–2995. [Google Scholar] [CrossRef] [PubMed]
- Oliveira Dos Santos, C.; Kolwijck, E.; van Rooij, J.; Stoutenbeek, R.; Visser, N.; Cheng, Y.Y.; Santana, N.T.Y.; Verweij, P.E.; Eggink, C.A. Epidemiology and Clinical Management of Fusarium keratitis in the Netherlands, 2005–2016. Front. Cell Infect. Microbiol. 2020, 10, 133. [Google Scholar] [CrossRef]
- Deorukhkar, S.; Katiyar, R.; Saini, S. Epidemiological features and laboratory results of bacterial and fungal keratitis: A five-year study at a rural tertiary-care hospital in western Maharashtra, India. Singap. Med. J. 2012, 53, 264–267. [Google Scholar]
- Thomas, P.A.; Kaliamurthy, J. Mycotic keratitis: Epidemiology, diagnosis and management. Clin. Microbiol. Infect. 2013, 19, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Manikandan, P.; Abdel-Hadi, A.; Randhir Babu Singh, Y.; Revathi, R.; Anita, R.; Banawas, S.; Bin Dukhyil, A.A.; Alshehri, B.; Shobana, C.S.; Panneer Selvam, K.; et al. Fungal Keratitis: Epidemiology, Rapid Detection, and Antifungal Susceptibilities of Fusarium and Aspergillus Isolates from Corneal Scrapings. Biomed. Res. Int. 2019, 2019, 6395840. [Google Scholar] [CrossRef] [PubMed]
- Garg, P.; Gopinathan, U.; Choudhary, K.; Rao, G.N. Keratomycosis: Clinical and microbiologic experience with dematiaceous fungi. Ophthalmology 2000, 107, 574–580. [Google Scholar] [CrossRef]
- Ghosh, A.; Kaur, H.; Gupta, A.; Singh, S.; Rudramurthy, S.M.; Gupta, S.; Chakrabarti, A. Emerging Dematiaceous and Hyaline Fungi Causing Keratitis in a Tertiary Care Centre From North India. Cornea 2020, 39, 868–876. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Khurana, A.; Sharma, M.; Chauhan, L. Causative fungi and treatment outcome of dematiaceous fungal keratitis in North India. Indian J. Ophthalmol. 2019, 67, 1048–1053. [Google Scholar] [CrossRef] [PubMed]
- Arunga, S.; Kintoki, G.M.; Gichuhi, S.; Onyango, J.; Newton, R.; Leck, A.; Macleod, D.; Hu, V.H.; Burton, M.J. Delay Along the Care Seeking Journey of Patients with Microbial Keratitis in Uganda. Ophthalmic Epidemiol. 2019, 26, 311–320. [Google Scholar] [CrossRef]
- Courtright, P.; Lewallen, S.; Kanjaloti, S.; Divala, D.J. Traditional eye medicine use among patients with corneal disease in rural Malawi. Br. J. Ophthalmol. 1994, 78, 810–812. [Google Scholar] [CrossRef]
- Yorston, D.; Foster, A. Traditional eye medicines and corneal ulceration in Tanzania. J. Trop. Med. Hyg. 1994, 97, 211–214. [Google Scholar]
- Burn, H.; Puri, L.; Roshan, A.; Singh, S.K.; Burton, M.J. Primary Eye Care in Eastern Nepal. Ophthalmic Epidemiol. 2019, 22, 1–12. [Google Scholar] [CrossRef]
- Prajna, N.V.; Krishnan, T.; Rajaraman, R.; Patel, S.; Srinivasan, M.; Das, M.; Ray, K.J.; O’Brien, K.S.; Oldenburg, C.E.; McLeod, S.D.; et al. Effect of Oral Voriconazole on Fungal Keratitis in the Mycotic Ulcer Treatment Trial II (MUTT II): A Randomized Clinical Trial. JAMA Ophthalmol. 2016, 134, 1365–1372. [Google Scholar] [CrossRef]
- Rahman, M.R.; Johnson, G.J.; Husain, R.; Howlader, S.A.; Minassian, D.C. Randomised trial of 0.2% chlorhexidine gluconate and 2.5% natamycin for fungal keratitis in Bangladesh. Br. J. Ophthalmol. 1998, 82, 919–925. [Google Scholar] [CrossRef]
- Prajna, N.V.; Krishnan, T.; Mascarenhas, J.; Rajaraman, R.; Prajna, L.; Srinivasan, M.; Raghavan, A.; Oldenburg, C.E.; Ray, K.J.; Zegans, M.E.; et al. The mycotic ulcer treatment trial: A randomized trial comparing natamycin vs voriconazole. JAMA Ophthalmol. 2013, 131, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.R.; Minassian, D.C.; Srinivasan, M.; Martin, M.J.; Johnson, G.J. Trial of chlorhexidine gluconate for fungal corneal ulcers. Ophthalmic Epidemiol. 1997, 4, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Prajna, N.V.; John, R.K.; Nirmalan, P.K.; Lalitha, P.; Srinivasan, M. A randomised clinical trial comparing 2% econazole and 5% natamycin for the treatment of fungal keratitis. Br. J. Ophthalmol. 2003, 87, 1235–1237. [Google Scholar] [CrossRef] [PubMed]
- Galarreta, D.J.; Tuft, S.J.; Ramsay, A.; Dart, J.K.G. Fungal keratitis in London: Microbiological and clinical evaluation. Cornea 2007, 26, 1082–1086. [Google Scholar] [CrossRef]
- Ong, H.S.; Fung, S.S.M.; Macleod, D.; Dart, J.K.G.; Tuft, S.J.; Burton, M.J. Altered Patterns of Fungal Keratitis at a London Ophthalmic Referral Hospital: An Eight-Year Retrospective Observational Study. Am. J. Ophthalmol. 2016, 168, 227–236. [Google Scholar] [CrossRef]
- Gordillo, M.A.; Cano, N.; Luquin, A.; Gutiérrez, C.; Verdú, E.; Cabrera, G.; Fierro, J.M.; Lamarca-Mateu, J.; España, J.; Marticorena-Álvarez, P.; et al. Queratitis secundaria a Fusarium spp. en España 2012–2014. Arch. Soc. Esp. Oftalmol. 2017, 93. [Google Scholar] [CrossRef]
- Nhung, P.T.; Thu, T.A.; Ngoc, L.H.; Ohkusu, K.; Ezaki, T. Epidemiology of Fungal Keratitis in North Vietnam. J. Clin. Exp. Ophthalmol. 2012, 3, 328. [Google Scholar] [CrossRef]
- Shah, A.; Sachdev, A.; Coggon, D.; Hossain, P. Geographic variations in microbial keratitis: An analysis of the peer-reviewed literature. Br. J. Ophthalmol. 2011, 95, 762–767. [Google Scholar] [CrossRef] [PubMed]
- Ung, L.; Bispo, P.J.M.; Shanbhag, S.S.; Gilmore, M.S.; Chodosh, J. The persistent dilemma of microbial keratitis: Global burden, diagnosis, and antimicrobial resistance. Surv. Ophthalmol. 2019, 64, 255–271. [Google Scholar] [CrossRef] [PubMed]
- Ritterband, D.C.; Seedor, J.A.; Shah, M.K.; Koplin, R.S.; McCormick, S.A. Fungal keratitis at the new york eye and ear infirmary. Cornea 2006, 25, 264–267. [Google Scholar] [CrossRef] [PubMed]
- Birker, I.C.Y.Y.; Luyten, G.P. Infectious corneal ulcers: A rising incidence in a Dutch referral centre. Acta Ophthalmol. 2018, 96, 3–49. [Google Scholar] [CrossRef]
- Capriotti, J.A.; Pelletier, J.S.; Shah, M.; Caivano, D.M.; Turay, P.; Ritterband, D.C. The etiology of infectious corneal ulceration in Sierra Leone. Int. Ophthalmol. 2010, 30, 637–640. [Google Scholar] [CrossRef]
- Gonawardena, S.A.; Ranasinghe, K.P.; Arseculeratne, S.N.; Seimon, C.R.; Ajello, L. Survey of mycotic and bacterial keratitis in Sri Lanka. Mycopathologia 1994, 127, 77–81. [Google Scholar] [CrossRef]
- Shabrawy, R.; El Badawy, N.; Harb, A. The incidence of fungal keratitis in Zagazig University Hospitals, Egypt and the value of direct microscopy and PCR technique in rapid diagnosis. J. Microbiol. Infect. Dis. 2013, 3, 186–191. [Google Scholar] [CrossRef][Green Version]
- Badawi, A.E.; Moemen, D.; El-Tantawy, N.L. Epidemiological, clinical and laboratory findings of infectious keratitis at Mansoura Ophthalmic Center, Egypt. Int. J. Ophthalmol. 2017, 10, 61–67. [Google Scholar] [CrossRef]
- Khater, M.M.; Shehab, N.S.; El-Badry, A.S. Comparison of mycotic keratitis with nonmycotic keratitis: An epidemiological study. J. Ophthalmol. 2014, 2014, 254302. [Google Scholar] [CrossRef]
- Kibret, T.; Bitew, A. Fungal keratitis in patients with corneal ulcer attending Minilik II Memorial Hospital, Addis Ababa, Ethiopia. BMC Ophthalmol. 2016, 16, 148. [Google Scholar] [CrossRef][Green Version]
- Hagan, M.; Wright, E.; Newman, M.; Dolin, P.; Johnson, G. Causes of suppurative keratitis in Ghana. Br. J. Ophthalmol. 1995, 79, 1024–1028. [Google Scholar] [CrossRef]
- Mehta, R.; Mehta, P.; Rao, M.; Acharya, Y.; Arja, S.B.; Sowmya, K. A Study of Fungal Keratitis in North Africa: Exploring Risk Factors and Microbiological Features. Int. J. Life-Sci. Sci. Res. 2016, 2, 579–582. [Google Scholar] [CrossRef]
- Carmichael, T.R.; Wolpert, M.; Koornhof, H.J. Corneal ulceration at an urban African hospital. Br. J. Ophthalmol. 1985, 69, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Schaftenaar, E.; Peters, R.P.; Baarsma, G.S.; Meenken, C.; Khosa, N.S.; Getu, S.; McIntyre, J.A.; Osterhaus, A.D.; Verjans, G.M. Clinical and corneal microbial profile of infectious keratitis in a high HIV prevalence setting in rural South Africa. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 1403–1409. [Google Scholar] [CrossRef] [PubMed]
- Mafwiri, M.M.; Kanyaro, N.D.; Padhan, D.H.; Sanyiwa, A.; Sangawe, J.L.F.; Kinabo, N.N. The microbial aetiology of corneal ulceration among patients attending a tertiary referral centre in Dar es Salaam. J. Ophthalmol. East. Cent. South. Afr. 2013, 16, 25–28. [Google Scholar]
- Cheikhrouhou, F.; Makni, F.; Neji, S.; Trigui, A.; Sellami, H.; Trabelsi, H.; Guidara, R.; Fki, J.; Ayadi, A. Epidemiological profile of fungal keratitis in Sfax (Tunisia). J. Mycol. Med. 2014, 24, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Zbiba, W.; Baba, A.; Bouayed, E.; Abdessalem, N.; Daldoul, A. A 5-year retrospective review of fungal keratitis in the region of Cap Bon. J. Fr. Ophtalmol. 2016, 39, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Limaiem, R.; Mghaieth, F.; Merdassi, A.; Mghaieth, K.; Aissaoui, A.; El Matri, L. Severe microbial keratitis: Report of 100 cases. J. Fr. Ophtalmol. 2007, 30, 374–379. [Google Scholar] [CrossRef]
- Talukder, A.K.; Halder, S.K.; Sultana, Z.; Bhuiyan, S.I. Epidemiology and outcome of non viral keratitis. Mymensingh Med. J. 2011, 20, 356–361. [Google Scholar]
- Dunlop, A.A.; Wright, E.D.; Howlader, S.A.; Nazrul, I.; Husain, R.; McClellan, K.; Billson, F.A. Suppurative corneal ulceration in Bangladesh. Aust. N. Z. J. Ophthalmol. 1994, 22, 105–110. [Google Scholar] [CrossRef]
- Lin, L.; Lan, W.; Lou, B.; Ke, H.; Yang, Y.; Lin, X.; Liang, L. Genus Distribution of Bacteria and Fungi Associated with Keratitis in a Large Eye Center Located in Southern China. Ophthalmic Epidemiol. 2017, 24, 90–96. [Google Scholar] [CrossRef]
- Zhong, W.X.; Sun, S.Y.; Zhao, J.; Shi, W.Y.; Xie, L.X. Retrospective study of suppurative keratitis in 1054 patients. Zhonghua Yan Ke Za Zhi 2007, 43, 245–250. [Google Scholar]
- Houang, E.; Lam, D.; Fan, D.; Seal, D. Microbial keratitis in Hong Kong: Relationship to climate, environment and contact-lens disinfection. Trans. R Soc. Trop. Med. Hyg. 2001, 95, 361–367. [Google Scholar] [CrossRef]
- Ng, A.L.; To, K.K.; Choi, C.C.; Yuen, L.H.; Yim, S.M.; Chan, K.S.; Lai, J.S.; Wong, I.Y. Predisposing Factors, Microbial Characteristics, and Clinical Outcome of Microbial Keratitis in a Tertiary Centre in Hong Kong: A 10-Year Experience. J. Ophthalmol. 2015, 2015, 769436. [Google Scholar] [CrossRef]
- Fong, C.F.; Tseng, C.H.; Hu, F.R.; Wang, I.J.; Chen, W.L.; Hou, Y.C. Clinical characteristics of microbial keratitis in a university hospital in Taiwan. Am. J. Ophthalmol. 2004, 137, 329–336. [Google Scholar] [CrossRef]
- Khor, W.-B.; Prajna, V.N.; Garg, P.; Mehta, J.S.; Xie, L.; Liu, Z.; Padilla, M.D.B.; Joo, C.-K.; Inoue, Y.; Goseyarakwong, P.; et al. The Asia Cornea Society Infectious Keratitis Study: A Prospective Multicenter Study of Infectious Keratitis in Asia. Am. J. Ophthalmol. 2018, 195, 161–170. [Google Scholar] [CrossRef]
- Bandyopadhyay, S.; Das, D.; Mondal, K.K.; Ghanta, A.K.; Purkrit, S.K.; Bhasrar, R. Epidemiology and laboratory diagnosis of fungal corneal ulcer in the Sundarban Region of West Bengal, eastern India. Nepal. J. Ophthalmol. 2012, 4, 29–36. [Google Scholar] [CrossRef]
- Saha, S.; Banerjee, D.; Khetan, A.; Sengupta, J. Epidemiological profile of fungal keratitis in urban population of West Bengal, India. Oman. J. Ophthalmol. 2009, 2, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Rautaraya, B.; Sharma, S.; Kar, S.; Das, S.; Sahu, S.K. Diagnosis and treatment outcome of mycotic keratitis at a tertiary eye care center in eastern India. BMC Ophthalmol. 2011, 11, 39. [Google Scholar] [CrossRef] [PubMed]
- Nath, R.; Baruah, S.; Saikia, L.; Devi, B.; Borthakur, A.K.; Mahanta, J. Mycotic corneal ulcers in upper Assam. Indian J. Ophthalmol. 2011, 59, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Roy, P.; Das, S.; Singh, N.P.; Saha, R.; Kajla, G.; Snehaa, K.; Gupta, V.P. Changing trends in fungal and bacterial profile of infectious keratitis at a tertiary care hospital: A six-year study. Clin. Epidemiol. Glob. Health 2017, 5, 40–45. [Google Scholar] [CrossRef]
- Ghosh, A.K.; Gupta, A.; Rudramurthy, S.M.; Paul, S.; Hallur, V.K.; Chakrabarti, A. Fungal Keratitis in North India: Spectrum of Agents, Risk Factors and Treatment. Mycopathologia 2016, 181, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Binnani, A.; Gupta, P.S.; Gupta, A. Epidemio-Clinico-Microbiological Study of Mycotic Keratitis in North-West Region of Rajasthan. Mycopathologia 2018, 183, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Chander, J.; Singla, N.; Agnihotri, N.; Arya, S.K.; Deep, A. Keratomycosis in and around Chandigarh: A five-year study from a north Indian tertiary care hospital. Indian J. Pathol. Microbiol. 2008, 51, 304–306. [Google Scholar] [CrossRef]
- Gupta, A.; Capoor, M.R.; Gupta, S.; Kochhar, S.; Tomer, A.; Gupta, V. Clinico-demographical profile of keratomycosis in Delhi, North India. Indian J. Med. Microbiol. 2014, 32, 310–314. [Google Scholar] [CrossRef] [PubMed]
- Saha, R.; Das, S. Mycological profile of infectious Keratitis from Delhi. Indian J. Med. Res. 2006, 123, 159–164. [Google Scholar]
- Chidambaram, J.D.; Venkatesh Prajna, N.; Srikanthi, P.; Lanjewar, S.; Shah, M.; Elakkiya, S.; Lalitha, P.; Burton, M.J. Epidemiology, risk factors, and clinical outcomes in severe microbial keratitis in South India. Ophthalmic Epidemiol. 2018, 25, 297–305. [Google Scholar] [CrossRef]
- Bharathi, M.J.; Ramakrishnan, R.; Meenakshi, R.; Padmavathy, S.; Shivakumar, C.; Srinivasan, M. Microbial Keratitis in South India: Influence of Risk Factors, Climate, and Geographical Variation. Ophthalmic Epidemiol. 2007, 14, 61–69. [Google Scholar] [CrossRef]
- Gopinathan, U.; Garg, P.; Fernandes, M.; Sharma, S.; Athmanathan, S.; Rao, G.N. The epidemiological features and laboratory results of fungal keratitis: A 10-year review at a referral eye care center in South India. Cornea 2002, 21, 555–559. [Google Scholar] [CrossRef]
- Gopinathan, U.; Sharma, S.; Garg, P.; Rao, G.N. Review of epidemiological features, microbiological diagnosis and treatment outcome of microbial keratitis: Experience of over a decade. Indian J. Ophthalmol. 2009, 57, 273–279. [Google Scholar] [CrossRef]
- Lin, C.C.; Lalitha, P.; Srinivasan, M.; Prajna, N.V.; McLeod, S.D.; Acharya, N.R.; Lietman, T.M.; Porco, T.C. Seasonal trends of microbial keratitis in South India. Cornea 2012, 31, 1123–1127. [Google Scholar] [CrossRef] [PubMed]
- Ranjini, C.Y.; Waddepally, V.V. Microbial Profile of Corneal Ulcers in a Tertiary Care Hospital in South India. J. Ophthalmic Vis. Res. 2016, 11, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Rajesh Somabhai, K.; Nilesh Dhanjibhai, P.; Mala, S. A Clinical Microbiological Study of Corneal Ulcer Patients at Western Gujarat, India. Acta Med. Iran. 2013, 51, 399–403. [Google Scholar]
- Kumar, A.; Pandya, S.; Kavathia, G.; Antala, S.; Madan, M.; Javdekar, T. Microbial keratitis in Gujarat, Western India: Findings from 200 cases. Pan. Afr. Med. J. 2011, 10, 48. [Google Scholar] [PubMed]
- Tewari, A.; Sood, N.; Vegad, M.M.; Mehta, D.C. Epidemiological and microbiological profile of infective keratitis in Ahmedabad. Indian J. Ophthalmol. 2012, 60, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Basak, S.K.; Basak, S.; Mohanta, A.; Bhowmick, A. Epidemiological and microbiological diagnosis of suppurative keratitis in Gangetic West Bengal, eastern India. Indian J. Ophthalmol. 2005, 53, 17–22. [Google Scholar] [CrossRef]
- Panda, A.; Satpathy, G.; Nayak, N.; Kumar, S.; Kumar, A. Demographic pattern, predisposing factors and management of ulcerative keratitis: Evaluation of one thousand unilateral cases at a tertiary care centre. Clin. Exp. Ophthalmol. 2007, 35, 44–50. [Google Scholar] [CrossRef]
- Sharma, S.; Taneja, M.; Gupta, R.; Upponi, A.; Gopinathan, U.; Nutheti, R.; Garg, P. Comparison of clinical and microbiological profiles in smear-positive and smear-negative cases of suspected microbial keratitis. Indian J. Ophthalmol. 2007, 55, 21–25. [Google Scholar] [CrossRef]
- Ebadollahi-Natanzi, A.; Arab-Rahmatipour, G.; Tabatabaei, S.A. Prevalence of Fungal Keratitis (FK) in Patients with Corneal Ulcers in Tehran, Iran. Asia Pac. J. Med. Toxicol. 2016, 5, 94–97. [Google Scholar] [CrossRef]
- Shokohi, T.; Nowroozpoor-Dailami, K.; Moaddel-Haghighi, T. Fungal Keratitis in Patients with Corneal Ulcer, in Sari, Northern Iran. Arch. Iran. Med. 2006, 9, 222–227. [Google Scholar]
- Al-Shakarchi, F. Initial therapy for suppurative microbial keratitis in Iraq. Br. J. Ophthalmol. 2007, 91, 1583–1587. [Google Scholar] [CrossRef][Green Version]
- Shakarchi, F.; Hussein, M.; Al-Shaibani, A. Profile of Microbial Keratitis at a Referral Center in Iraq. J. Al-Nahrain Univ. Sci. 2015, 18, 141–147. [Google Scholar] [CrossRef]
- Khalil, Z.; Hadi, A.; Kamil, S. Determination and Prevalence of Bacterial and Fungal Keratitis among Patients in Baghdad City. J. Pure Appl. Microbiol. 2018, 12, 1455–1463. [Google Scholar] [CrossRef]
- Toshida, H.; Kogure, N.; Inoue, N.; Murakami, A. Trends in microbial keratitis in Japan. Eye Contact Lens 2007, 33, 70–73. [Google Scholar] [CrossRef]
- National Surveillance of Infectious Keratitis in Japan. National Surveillance of Infectious Keratitis in Japan—Current status of isolates, patient background, and treatment. Nippon Ganka Gakkai Zasshi 2006, 110, 961–972. [Google Scholar]
- Han, S.B.; Lim, T.H.; Wee, W.R.; Lee, J.H.; Kim, M.K. Current characteristics of infectious keratitis at a tertiary referral center in South Korea. Jpn. J. Ophthalmol. 2009, 53, 549–551. [Google Scholar] [CrossRef]
- Mohd-Tahir, F.; Norhayati, A.; Siti-Raihan, I.; Ibrahim, M. A 5-Year Retrospective Review of Fungal Keratitis at Hospital Universiti Sains Malaysia. Interdiscip. Perspect. Infect. Dis. 2012, 2012, 851563. [Google Scholar] [CrossRef]
- Ratnalingam, V.; Umapathy, T.; Sumugam, K.; Hanafi, H.; Retnasabapathy, S. Microbial keratitis in West and East Malaysia. Int. Eye Sci. 2017, 17, 1989–1992. [Google Scholar] [CrossRef]
- Amatya, R.; Shrestha, S.; Khanal, B.; Gurung, R.; Poudel, N.; Bhattacharya, S.; Badu, P. Etiological agents of corneal ulcer: Five years prospective study in eastern Nepal. Nepal Med. Coll. J. NMCJ 2012, 14, 219–222. [Google Scholar] [PubMed]
- Khanal, B.; Kaini, K.R.; Deb, M.; Badhu, B.; Thakur, S.K. Microbial keratitis in eastern Nepal. Trop. Dr. 2001, 31, 168–169. [Google Scholar] [CrossRef] [PubMed]
- Ganguly, S.; Kansakar, I.; Sharma, M.; Bastola, P.; Pradhan, R. Pattern of fungal isolates in cases of corneal ulcer in the western periphery of Nepal. Nepal. J. Ophthalmol. 2011, 3, 118–122. [Google Scholar] [CrossRef]
- Lavaju, P.; Arya, S.; Khanal, B.; Amatya, R.; Patel, S. Demograhic pattern, clinical features and treatment outcome of patients with infective keratitis in the eastern region of Nepal. Nepal. J. Ophthalmol. 2010, 1, 101–106. [Google Scholar] [CrossRef][Green Version]
- Suwal, S.; Bhandari, D.; Thapa, P.; Shrestha, M.; Amatya, J. Microbiological profile of corneal ulcer cases diagnosed in a tertiary care ophthalmological institute in Nepal. BMC Ophthalmol. 2016, 16. [Google Scholar] [CrossRef]
- Upadhyay, M.; Rai, N.; Brandt, F.; Shrestha, R. Corneal ulcers in Nepal. Graefe’s Arch. Clin. Exp. Ophthalmol. 1982, 219, 55–59. [Google Scholar] [CrossRef]
- Sitoula, R.P.; Singh, S.; Mahaseth, V.; Sharma, A.; Labh, R. Epidemiology and etiological diagnosis of infective keratitis in eastern region of Nepal. Nepal. J. Ophthalmol. 2015, 7, 10–15. [Google Scholar] [CrossRef]
- Idiculla, T.; Zachariah, G.; Br, K.; Basu, S. A Retrospective Study of Fungal Corneal Ulcers in the South Sharqiyah Region in Oman. Sultan Qaboos Univ. Med. J. 2009, 9, 59–62. [Google Scholar]
- Keshav, B.Z.G.; Ideculla, T.; Bhat, V.; Joseph, M. Epidemiological characteristics of corneal ulcers in South sharqiya region. Oman Med. J. 2008, 23, 34–39. [Google Scholar]
- Riaz, Q.; Fawwad, U.; Bhatti, N.; Rehman, A.U.; Hasan, M.U. Epidemiology of Microbial Keratitis in a Tertiary Care Center in Karachi. Pak. J. Ophthalmol. 2013, 29, 94–99. [Google Scholar]
- Jastaneiah, S.; Al-Rajhi, A.; Abbott, D. Ocular mycosis at a referral center in Saudi Arabia: A 20-year study. Saudi J. Ophthalmol. 2011, 25, 231–238. [Google Scholar] [CrossRef]
- Wong, T.Y.; Fong, K.S.; Tan, D.T. Clinical and microbial spectrum of fungal keratitis in Singapore: A 5-year retrospective study. Int. Ophthalmol. 1997, 21, 127–130. [Google Scholar] [CrossRef]
- Boonpasart, S.; Kasetsuwan, N.; Puangsricharern, V.; Pariyakanok, L.; Jittpoonkusol, T. Infectious keratitis at King Chulalongkorn Memorial Hospital: A 12-year retrospective study of 391 cases. J. Med. Assoc. Thai 2002, 85 (Suppl. 1), S217–S230. [Google Scholar]
- Hirunpat, C.; Masae, N. Fungal keratitis in Songklanagarind Hospital. Songklanagarind Med. J. 2005, 23, 429–434. [Google Scholar]
- Tananuvat, N.; Punyakhum, O.; Ausayakhun, S.; Chaidaroon, W. Etiology and clinical outcomes of microbial keratitis at a tertiary eye-care center in northern Thailand. J. Med. Assoc. Thai 2012, 95, S8–S17. [Google Scholar]
- Sirikul, T.; Prabriputaloong, T.; Smathivat, A.; Chuck, R.S.; Vongthongsri, A. Predisposing Factors and Etiologic Diagnosis of Ulcerative Keratitis. Cornea 2008, 27, 283–287. [Google Scholar] [CrossRef]
- Erdem, E.; Yagmur, M.; Boral, H.; Ilkit, M.; Ersoz, R.; Seyedmousavi, S. Aspergillus flavus Keratitis: Experience of a Tertiary Eye Clinic in Turkey. Mycopathologia 2017, 182, 379–385. [Google Scholar] [CrossRef]
- Yilmaz, S.; Ozturk, I.; Maden, A. Microbial keratitis in West Anatolia, Turkey: A retrospective review. Int. Ophthalmol. 2007, 27, 261–268. [Google Scholar] [CrossRef]
- Nguyên, D.T.; Nguyên, H. Keratomycoses in Viet-Nam. Rev. Int. Trach. Pathol. Ocul. Trop. Subtrop. Sante Publique 1990, 67, 203–206. [Google Scholar]
- Van der Meulen, I.J.; van Rooij, J.; Nieuwendaal, C.P.; Van Cleijnenbreugel, H.; Geerards, A.J.; Remeijer, L. Age-related risk factors, culture outcomes, and prognosis in patients admitted with infectious keratitis to two Dutch tertiary referral centers. Cornea 2008, 27, 539–544. [Google Scholar] [CrossRef]
- Tavassoli, S.; Nayar, G.; Darcy, K.; Grzeda, M.; Luck, J.; Williams, O.M.; Tole, D. An 11-year analysis of microbial keratitis in the South West of England using brain–heart infusion broth. Eye 2019, 33, 1619–1625. [Google Scholar] [CrossRef]
- Ting, D.S.J.; Settle, C.; Morgan, S.J.; Baylis, O.; Ghosh, S. A 10-year analysis of microbiological profiles of microbial keratitis: The North East England Study. Eye 2018, 32, 1416–1417. [Google Scholar] [CrossRef]
- Tan, S.Z.; Walkden, A.; Au, L.; Fullwood, C.; Hamilton, A.; Qamruddin, A.; Armstrong, M.; Brahma, A.K.; Carley, F. Twelve-year analysis of microbial keratitis trends at a UK tertiary hospital. Eye 2017, 31, 1229–1236. [Google Scholar] [CrossRef]
- Cariello, A.; Passos, R.; Yu, M.; Hofling-lima, A.L. Microbial keratitis at a referral center in Brazil. Int. Ophthalmol. 2011, 31, 197–204. [Google Scholar] [CrossRef]
- Furlanetto, R.L.; Andreo, E.G.V.; Finotti, L.G.A.; Arcieri, E.S.; Ferreira, M.A.; Rocha, F.J. Epidemiology and Etiologic Diagnosis of Infectious Keratitis in Uberlandia, Brazil. Eur. J. Ophthalmol. 2010, 20, 498–503. [Google Scholar] [CrossRef]
- Ibrahim, M.M.; Vanini, R.; Ibrahim, F.M.; Fioriti, L.S.; Furlan, E.M.R.; Provinzano, L.M.A.; De Castro, R.S.; De Faria Esousa, S.J.; Rocha, E.M. Epidemiologic Aspects and Clinical Outcome of Fungal Keratitis in Southeastern Brazil. Eur. J. Ophthalmol. 2009, 19, 355–361. [Google Scholar] [CrossRef]
- Müller, G.G.; Kara-José, N.; Castro, R.S. Epidemiological profile of keratomycosis at the HC-UNICAMP. Arq. Bras. Oftalmol. 2012, 75, 247–250. [Google Scholar] [CrossRef]
- Parra-Rodríguez, D.S.; García-Carmona, K.P.; Vázquez-Maya, L.; Bonifaz, A. Incidencia de úlceras corneales microbianas en el Servicio de Oftalmología del Hospital General de México Dr. Eduardo Liceaga. Rev. Mex. Oftalmol. 2016, 90, 209–214. [Google Scholar] [CrossRef]
- Laspina, F.; Samudio, M.; Cibils, D.; Ta, C.N.; Fariña, N.; Sanabria, R.; Klauß, V.; Miño de Kaspar, H. Epidemiological characteristics of microbiological results on patients with infectious corneal ulcers: A 13-year survey in Paraguay. Graefe’s Arch. Clin. Exp. Ophthalmol. 2004, 242, 204–209. [Google Scholar] [CrossRef]
- Nentwich, M.M.; Bordón, M.; di Martino, D.S.; Campuzano, A.R.; Torres, W.M.; Laspina, F.; Lichi, S.; Samudio, M.; Farina, N.; Sanabria, R.R.; et al. Clinical and epidemiological characteristics of infectious keratitis in Paraguay. Int. Ophthalmol. 2015, 35, 341–346. [Google Scholar] [CrossRef]
- Varaprasathan, G.; Miller, K.; Lietman, T.; Whitcher, J.P.; Cevallos, V.; Okumoto, M.; Margolis, T.P.; Yinghui, M.; Cunningham, E.T.J. Trends in the Etiology of Infectious Corneal Ulcers at the F. I. Proctor Foundation. Cornea 2004, 23, 360–364. [Google Scholar] [CrossRef]
- Liesegang, T.J.; Forster, R.K. Spectrum of microbial keratitis in South Florida. Am. J. Ophthalmol. 1980, 90, 38–47. [Google Scholar] [CrossRef]
- Iyer, S.A.; Tuli, S.S.; Wagoner, R.C. Fungal Keratitis: Emerging Trends and Treatment Outcomes. Eye Contact Lens 2006, 32, 267–271. [Google Scholar] [CrossRef]
- Ho, J.W.; Fernandez, M.M.; Rebong, R.A.; Carlson, A.N.; Kim, T.; Afshari, N.A. Microbiological profiles of fungal keratitis: A 10-year study at a tertiary referral center. J. Ophthalmic Inflamm. Infect. 2016, 6, 5. [Google Scholar] [CrossRef]
- Green, M.; Apel, A.; Stapleton, F. A longitudinal study of trends in keratitis in Australia. Cornea 2008, 27, 33–39. [Google Scholar] [CrossRef]
- Chew, R.; Woods, M.L. Epidemiology of fungal keratitis in Queensland, Australia. Clin. Exp. Ophthalmol. 2019, 47, 26–32. [Google Scholar] [CrossRef]
- Watson, S.L.; Cabrera-Aguas, M.; Keay, L.; Khoo, P.; McCall, D.; Lahra, M.M. The clinical and microbiological features and outcomes of fungal keratitis over 9 years in Sydney, Australia. Mycoses 2020, 63, 43–51. [Google Scholar] [CrossRef]
- Green, M.; Carnt, N.; Apel, A.; Stapleton, F. Queensland Microbial Keratitis Database: 2005–2015. Br. J. Ophthalmol. 2019, 103, 1481–1486. [Google Scholar] [CrossRef]
- Khoo, P.; Cabrera-Aguas, M.P.; Nguyen, V.; Lahra, M.M.; Watson, S.L. Microbial keratitis in Sydney, Australia: Risk factors, patient outcomes, and seasonal variation. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 1745–1755. [Google Scholar] [CrossRef]
- Pandita, A.; Murphy, C. Microbial keratitis in Waikato, New Zealand. Clin. Exp. Ophthalmol. 2011, 39, 393–397. [Google Scholar] [CrossRef]
- Saad-Hussein, A.; El-Mofty, H.M.; Hassanien, M.A. Climate change and predicted trend of fungal keratitis in Egypt. East Mediterr. Health J. 2011, 17, 468–473. [Google Scholar] [CrossRef]
- Gower, E.W.; Keay, L.J.; Oechsler, R.A.; Iovieno, A.; Alfonso, E.C.; Jones, D.B.; Colby, K.; Tuli, S.S.; Patel, S.R.; Lee, S.M.; et al. Trends in fungal keratitis in the United States, 2001 to 2007. Ophthalmology 2010, 117, 2263–2267. [Google Scholar] [CrossRef]
- Bharathi, M.J.; Ramakrishnan, R.; Vasu, S.; Meenakshi, R.; Palaniappan, R. Epidemiological characteristics and laboratory diagnosis of fungal keratitis. A three-year study. Indian J. Ophthalmol. 2003, 51, 315–321. [Google Scholar] [PubMed]
- Bharathi, M.J.; Ramakrishnan, R.; Meenakshi, R.; Shivakumar, C.; Raj, D.L. Analysis of the risk factors predisposing to fungal, bacterial & Acanthamoeba keratitis in south India. Indian J. Med. Res. 2009, 130, 749–757. [Google Scholar] [PubMed]
- Sharma, S.; Das, S.; Virdi, A.; Fernandes, M.; Sahu, S.K.; Kumar Koday, N.; Ali, M.H.; Garg, P.; Motukupally, S.R. Re-appraisal of topical 1% voriconazole and 5% natamycin in the treatment of fungal keratitis in a randomised trial. Br. J. Ophthalmol. 2015, 99, 1190–1195. [Google Scholar] [CrossRef]
- Das, S.; Sharma, S.; Mahapatra, S.; Sahu, S.K. Fusarium keratitis at a tertiary eye care centre in India. Int. Ophthalmol. 2015, 35, 387–393. [Google Scholar] [CrossRef]
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pr. 2018, 138, 271–281. [Google Scholar] [CrossRef]
- Hine, J.L.; de Lusignan, S.; Burleigh, D.; Pathirannehelage, S.; McGovern, A.; Gatenby, P.; Jones, S.; Jiang, D.; Williams, J.; Elliot, A.J.; et al. Association between glycaemic control and common infections in people with Type 2 diabetes: A cohort study. Diabet. Med. 2017, 34, 551–557. [Google Scholar] [CrossRef]
- Dan, J.; Zhou, Q.; Zhai, H.; Cheng, J.; Wan, L.; Ge, C.; Xie, L. Clinical analysis of fungal keratitis in patients with and without diabetes. PLoS ONE 2018, 13, e0196741. [Google Scholar] [CrossRef]
- Arunga, S.; Kintoki, G.M.; Gichuhi, S.; Onyango, J.; Ayebazibwe, B.; Newton, R.; Leck, A.; Macleod, D.; Hu, V.H.; Burton, M.J. Risk Factors of Microbial Keratitis in Uganda: A Case Control Study. Ophthalmic Epidemiol. 2020, 27, 98–104. [Google Scholar] [CrossRef]
- Santos, C.; Parker, J.; Dawson, C.; Ostler, B. Bilateral fungal corneal ulcers in a patient with AIDS-related complex. Am. J. Ophthalmol. 1986, 102, 118–119. [Google Scholar] [CrossRef]
- Parrish, C.M.; O’Day, D.M.; Hoyle, T.C. Spontaneous fungal corneal ulcer as an ocular manifestation of AIDS. Am. J. Ophthalmol. 1987, 104, 302–303. [Google Scholar] [CrossRef]
- Mselle, J. Fungal keratitis as an indicator of HIV infection in Africa. Trop. Dr. 1999, 29, 133–135. [Google Scholar] [CrossRef] [PubMed]
- Arunga, S.; Kintoki, G.M.; Mwesigye, J.; Ayebazibwe, B.; Onyango, J.; Bazira, J.; Newton, R.; Gichuhi, S.; Leck, A.; Macleod, D.; et al. Epidemiology of Microbial Keratitis in Uganda: A Cohort Study. Ophthalmic Epidemiol. 2020, 27, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Anguria, P.; Ntuli, S.; Interewicz, B.; Carmichael, T. Traditional eye medication and pterygium occurrence in Limpopo Province. South Afr. Med. J. 2012, 102, 687–690. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bisika, T.; Courtright, P.; Geneau, R.; Kasote, A.; Chimombo, L.; Chirambo, M. Self treatment of eye diseases in Malawi. Afr. J. Tradit. Complement Altern. Med. 2008, 6, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Lionakis, M.S.; Kontoyiannis, D.P. Glucocorticoids and invasive fungal infections. Lancet 2003, 362, 1828–1838. [Google Scholar] [CrossRef]
- Nielsen, S.E.; Nielsen, E.; Julian, H.O.; Lindegaard, J.; Højgaard, K.; Ivarsen, A.; Hjortdal, J.; Heegaard, S. Incidence and clinical characteristics of fungal keratitis in a Danish population from 2000 to 2013. Acta Ophthalmol. 2015, 93, 54–58. [Google Scholar] [CrossRef]
- Cho, C.H.; Lee, S.B. Clinical analysis of microbiologically proven fungal keratitis according to prior topical steroid use: A retrospective study in South Korea. BMC Ophthalmol. 2019, 19, 207. [Google Scholar] [CrossRef]
- Keay, L.J.; Gower, E.W.; Iovieno, A.; Oechsler, R.A.; Alfonso, E.C.; Matoba, A.; Colby, K.; Tuli, S.S.; Hammersmith, K.; Cavanagh, D.; et al. Clinical and Microbiological Characteristics of Fungal Keratitis in the United States, 2001–2007: A Multicenter Study. Ophthalmology 2011, 118, 920–926. [Google Scholar] [CrossRef]
- Poole, T.R.G.; Hunter, D.L.; Maliwa, E.M.K.; Ramsay, A.R.C. Aetiology of microbial keratitis in northern Tanzania. Br. J. Ophthalmol. 2002, 86, 941–942. [Google Scholar] [CrossRef][Green Version]
- Bullock, J.D.; Warwar, R.E.; Elder, B.L.; Khamis, H.J. Microbiological Investigations of ReNu Plastic Bottles and the 2004 to 2006 ReNu With MoistureLoc-Related Worldwide Fusarium Keratitis Event. Eye Contact Lens 2016, 42, 147–152. [Google Scholar] [CrossRef]
- Buchta, V.; Feuermannová, A.; Váša, M.; Bašková, L.; Kutová, R.; Kubátová, A.; Vejsová, M. Outbreak of fungal endophthalmitis due to Fusarium oxysporum following cataract surgery. Mycopathologia 2014, 177, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Labiris, G.; Troeber, L.; Gatzioufas, Z.; Stavridis, E.; Seitz, B. Bilateral Fusarium oxysporum keratitis after laser in situ keratomileusis. J. Cataract Refract. Surg. 2012, 38, 2040–2044. [Google Scholar] [CrossRef]
- Jurkunas, U.; Behlau, I.; Colby, K. Fungal keratitis: Changing pathogens and risk factors. Cornea 2009, 28, 638–643. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.M.; Vanini, R.; Ibrahim, F.M.; Martins, W.d.P.; Carvalho, R.T.d.C.; Castro, R.S.d.; Rocha, E.M. Epidemiology and medical prediction of microbial keratitis in southeast Brazil. Arq. Bras. Oftalmol. 2011, 74, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Grzybowski, A.; Told, R.; Sacu, S.; Bandello, F.; Moisseiev, E.; Loewenstein, A.; Schmidt-Erfurth, U. 2018 Update on Intravitreal Injections: Euretina Expert Consensus Recommendations. Ophthalmologica 2018, 239, 181–193. [Google Scholar] [CrossRef]
- Luo, D.; Zhu, B.; Zheng, Z.; Zhou, H.; Sun, X.; Xu, X. Subtenon Vs Intravitreal Triamcinolone injection in Diabetic Macular Edema, A prospective study in Chinese population. Pak. J. Med. Sci. 2014, 30, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Weinberg, T.; Loewenstein, A. The role of steroids in treating diabetic macular oedema in the era of anti-VEGF. Eye 2020, 34, 1003–1005. [Google Scholar] [CrossRef] [PubMed]
- Durand, M.L. Bacterial and Fungal Endophthalmitis. Clin. Microbiol. Rev. 2017, 30, 597–613. [Google Scholar] [CrossRef] [PubMed]
- Galor, A.; Karp, C.L.; Forster, R.K.; Dubovy, S.R.; Gaunt, M.L.; Miller, D. Subconjunctival mycetoma after sub-Tenon’s corticosteroid injection. Cornea 2009, 28, 933–935. [Google Scholar] [CrossRef]
- Iwahashi, C.; Eguchi, H.; Hotta, F.; Uezumi, M.; Sawa, M.; Kimura, M.; Yaguchi, T.; Kusaka, S. Orbital abscess caused by Exophiala dermatitidis following posterior subtenon injection of triamcinolone acetonide: A case report and a review of literature related to Exophiala eye infections. BMC Infect. Dis. 2020, 20, 566. [Google Scholar] [CrossRef]
- Dahlgren, M.A.; Lingappan, A.; Wilhelmus, K.R. The Clinical Diagnosis of Microbial Keratitis. Am. J. Ophthalmol. 2007, 143, 940–944.e1. [Google Scholar] [CrossRef]
- Dalmon, C.; Porco, T.C.; Lietman, T.M.; Prajna, N.V.; Prajna, L.; Das, M.R.; Kumar, J.A.; Mascarenhas, J.; Margolis, T.P.; Whitcher, J.P.; et al. The Clinical Differentiation of Bacterial and Fungal Keratitis: A Photographic Survey. Investig. Opthalmol. Vis. Sci. 2012, 53, 1787–1791. [Google Scholar] [CrossRef]
- Leck, A.; Burton, M. Distinguishing fungal and bacterial keratitis on clinical signs. Community Eye Health 2015, 28, 6–7. [Google Scholar] [PubMed]
- Mascarenhas, J.; Lalitha, P.; Prajna, N.V.; Srinivasan, M.; Das, M.; D’Silva, S.S.; Oldenburg, C.E.; Borkar, D.S.; Esterberg, E.J.; Lietman, T.M.; et al. Acanthamoeba, Fungal, and Bacterial Keratitis: A Comparison of Risk Factors and Clinical Features. Am. J. Ophthalmol. 2014, 157, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Oldenburg, C.E.; Prajna, V.N.; Prajna, L.; Krishnan, T.; Mascarenhas, J.; Vaitilingam, C.M.; Srinivasan, M.; See, C.W.; Cevallos, V.; Zegans, M.E.; et al. Clinical signs in dematiaceous and hyaline fungal keratitis. Br. J. Ophthalmol. 2011, 95, 750–751. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Barron, B.A.; Gee, L.; Hauck, W.W.; Kurinij, N.; Dawson, C.R.; Jones, D.B.; Wilhelmus, K.R.; Kaufman, H.E.; Sugar, J.; Hyndiuk, R.A. Herpetic Eye Disease Study. A controlled trial of oral acyclovir for herpes simplex stromal keratitis. Ophthalmology 1994, 101, 1871–1882. [Google Scholar] [CrossRef]
- Mahmoudi, S.; Masoomi, A.; Ahmadikia, K.; Tabatabaei, S.A.; Soleimani, M.; Rezaie, S.; Ghahvechian, H.; Banafsheafshan, A. Fungal keratitis: An overview of clinical and laboratory aspects. Mycoses 2018, 61, 916–930. [Google Scholar] [CrossRef]
- Bhadange, Y.; Das, S.; Kasav, M.K.; Sahu, S.K.; Sharma, S. Comparison of culture-negative and culture-positive microbial keratitis: Cause of culture negativity, clinical features and final outcome. Br. J. Ophthalmol. 2015, 99, 1498–1502. [Google Scholar] [CrossRef]
- Ngo, J.; Khoo, P.; Watson, S. Improving the Efficiency and the Technique of the Corneal Scrape Procedure via an Evidence Based Instructional Video at a Quaternary Referral Eye Hospital. Curr. Eye Res. 2020, 45. [Google Scholar] [CrossRef]
- Vengayil, S.; Panda, A.; Satpathy, G.; Nayak, N.; Ghose, S.; Patanaik, D.; Khokhar, S. Polymerase chain reaction-guided diagnosis of mycotic keratitis: A prospective evaluation of its efficacy and limitations. Investig. Ophthalmol. Vis. Sci. 2009, 50, 152–156. [Google Scholar] [CrossRef]
- Thomas, P.A.; Theresa, P.A.; Theodore, J.; Geraldine, P. PCR for the molecular diagnosis of mycotic keratitis. Expert Rev. Mol. Diagn. 2012, 12, 703–718. [Google Scholar] [CrossRef] [PubMed]
- Tananuvat, N.; Salakthuantee, K.; Vanittanakom, N.; Pongpom, M.; Ausayakhun, S. Prospective comparison between conventional microbial work-up vs PCR in the diagnosis of fungal keratitis. Eye 2012, 26, 1337–1343. [Google Scholar] [CrossRef]
- Kim, E.; Chidambaram, J.D.; Srinivasan, M.; Lalitha, P.; Wee, D.; Lietman, T.M.; Whitcher, J.P.; Van Gelder, R.N. Prospective comparison of microbial culture and polymerase chain reaction in the diagnosis of corneal ulcer. Am. J. Ophthalmol. 2008, 146, 714–723.e1. [Google Scholar] [CrossRef]
- Ghosh, A.; Basu, S.; Datta, H.; Chattopadhyay, D. Evaluation of polymerase chain reaction-based ribosomal DNA sequencing technique for the diagnosis of mycotic keratitis. Am. J. Ophthalmol. 2007, 144, 396–403. [Google Scholar] [CrossRef]
- Ferrer, C.; Alio, J.L. Evaluation of molecular diagnosis in fungal keratitis. Ten years of experience. J. Ophthalmic Inflamm. Infect. 2011, 1, 15–22. [Google Scholar] [CrossRef]
- Homa, M.; Shobana, C.S.; Singh, Y.R.B.; Manikandan, P.; Selvam, K.P.; Kredics, L.; Narendran, V.; Vágvölgyi, C.; Galgóczy, L. Fusarium keratitis in South India: Causative agents, their antifungal susceptibilities and a rapid identification method for the Fusarium solani species complex. Mycoses 2013, 56, 501–511. [Google Scholar] [CrossRef] [PubMed]
- Oechsler, R.A.; Feilmeier, M.R.; Miller, D.; Shi, W.; Hofling-Lima, A.L.; Alfonso, E.C. Fusarium Keratitis: Genotyping, In Vitro Susceptibility and Clinical Outcomes. Cornea 2013, 32, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Dingle, T.C.; Butler-Wu, S.M. Maldi-tof mass spectrometry for microorganism identification. Clin. Lab. Med. 2013, 33, 589–609. [Google Scholar] [CrossRef] [PubMed]
- Atalay, A.; Koc, A.N.; Suel, A.; Sav, H.; Demir, G.; Elmali, F.; Cakir, N.; Seyedmousavi, S. Conventional Morphology Versus PCR Sequencing, rep-PCR, and MALDI-TOF-MS for Identification of Clinical Aspergillus Isolates Collected Over a 2-Year Period in a University Hospital at Kayseri, Turkey. J. Clin. Lab. Anal. 2016, 30, 745–750. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Yu, H.; Jiang, L.; Wu, J.; Yi, M. Fungal keratitis caused by a rare pathogen, Colletotrichum gloeosporioides, in an east coast city of China. J. Mycol. Med. 2020, 30, 100922. [Google Scholar] [CrossRef]
- Ting, D.S.J.; McKenna, M.; Sadiq, S.N.; Martin, J.; Mudhar, H.S.; Meeney, A.; Patel, T. Arthrographis kalrae Keratitis Complicated by Endophthalmitis: A Case Report With Literature Review. Eye Contact Lens 2020, 46, e59–e65. [Google Scholar] [CrossRef] [PubMed]
- Rohilla, R.; Meena, S.; Mohanty, A.; Gupta, N.; Kaistha, N.; Gupta, P.; Mangla, A.; Singh, A. Etiological spectrum of infectious keratitis in the era of MALDI-TOF-MS at a tertiary care hospital. J. Fam. Med. Prim. Care 2020, 9, 4576–4581. [Google Scholar] [CrossRef]
- Miqueleiz Zapatero, A.; Hernando, C.; Barba, J.; Buendía, B. First report of a case of fungal keratitis due to Curvularia hominis in Spain. Rev. Iberoam. Micol. 2018, 35, 155–158. [Google Scholar] [CrossRef]
- Cavallini, G.M.; Ducange, P.; Volante, V.; Benatti, C. Successful treatment of Fusarium keratitis after photo refractive keratectomy. Indian J. Ophthalmol. 2013, 61, 669–671. [Google Scholar] [CrossRef] [PubMed]
- Chidambaram, J.D.; Prajna, N.V.; Larke, N.L.; Palepu, S.; Lanjewar, S.; Shah, M.; Elakkiya, S.; Lalitha, P.; Carnt, N.; Vesaluoma, M.H.; et al. Prospective Study of the Diagnostic Accuracy of the In Vivo Laser Scanning Confocal Microscope for Severe Microbial Keratitis. Ophthalmology 2016, 123, 2285–2293. [Google Scholar] [CrossRef]
- Chidambaram, J.D.; Prajna, N.V.; Larke, N.; Macleod, D.; Srikanthi, P.; Lanjewar, S.; Shah, M.; Lalitha, P.; Elakkiya, S.; Burton, M.J. In vivo confocal microscopy appearance of Fusarium and Aspergillus species in fungal keratitis. Br. J. Ophthalmol. 2017, 101, 1119–1123. [Google Scholar] [CrossRef]
- Labbé, A.; Khammari, C.; Dupas, B.; Gabison, E.; Brasnu, E.; Labetoulle, M.; Baudouin, C. Contribution of in vivo confocal microscopy to the diagnosis and management of infectious keratitis. Ocul. Surf. 2009, 7, 41–52. [Google Scholar] [CrossRef]
- Chidambaram, J.D. Recent advances in the diagnosis and management of bacterial keratitis. Int. Ophthalmol. Clin. 2007, 47, 1–6. [Google Scholar] [CrossRef]
- Shi, W.; Li, S.; Liu, M.; Jin, H.; Xie, L. Antifungal chemotherapy for fungal keratitis guided by in vivo confocal microscopy. Graefe Arch. Clin. Exp. Ophthalmol. 2008, 246, 581–586. [Google Scholar] [CrossRef]
- Hau, S.C.; Dart, J.K.G.; Vesaluoma, M.; Parmar, D.N.; Claerhout, I.; Bibi, K.; Larkin, D.F.P. Diagnostic accuracy of microbial keratitis with in vivo scanning laser confocal microscopy. Br. J. Ophthalmol. 2010, 94, 982–987. [Google Scholar] [CrossRef]
- FlorCruz, N.V.; Evans, J.R. Medical interventions for fungal keratitis. Cochrane Database Syst. Rev. 2015, 4, CD004241. [Google Scholar] [CrossRef] [PubMed]
- Schein, O.D. Evidence-Based Treatment of Fungal Keratitis. JAMA Ophthalmol. 2016, 134, 1372–1373. [Google Scholar] [CrossRef] [PubMed]
- Parchand, S.; Gupta, A.; Ram, J.; Gupta, N.; Chakrabarty, A. Voriconazole for fungal corneal ulcers. Ophthalmology 2012, 119, 1083. [Google Scholar] [CrossRef] [PubMed]
- Prajna, N.V.; Mascarenhas, J.; Krishnan, T.; Reddy, P.R.; Prajna, L.; Srinivasan, M.; Vaitilingam, C.M.; Hong, K.C.; Lee, S.M.; McLeod, S.D.; et al. Comparison of natamycin and voriconazole for the treatment of fungal keratitis. Arch. Ophthalmol. 2010, 128, 672–678. [Google Scholar] [CrossRef]
- Martin, M.J.; Rahman, M.R.; Johnson, G.J.; Srinivasan, M.; Clayton, Y.M. Mycotic keratitis: Susceptibility to antiseptic agents. Int. Ophthalmol. 1995, 19, 299–302. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, J.J.; Yadav, R.; Das Sanyam, S.; Chaudhary, P.; Roshan, A.; Singh, S.K.; Arunga, S.; Matayan, E.; Macleod, D.; Weiss, H.A.; et al. Topical chlorhexidine 0.2% versus topical natamycin 5% for fungal keratitis in Nepal: Rationale and design of a randomised controlled non-inferiority trial. BMJ Open 2020, 10, e038066. [Google Scholar] [CrossRef]
- Sharma, N.; Sahay, P.; Maharana, P.K.; Singhal, D.; Saluja, G.; Bandivadekar, P.; Chako, J.; Agarwal, T.; Sinha, R.; Titiyal, J.S.; et al. Management Algorithm for Fungal Keratitis: The TST (Topical, Systemic, and Targeted Therapy) Protocol. Cornea 2019, 38, 141–145. [Google Scholar] [CrossRef]
- Sharma, N.; Singhal, D.; Maharana, P.K.; Sinha, R.; Agarwal, T.; Upadhyay, A.D.; Velpandian, T.; Satpathy, G.; Titiyal, J.S. Comparison of Oral Voriconazole Versus Oral Ketoconazole as an Adjunct to Topical Natamycin in Severe Fungal Keratitis: A Randomized Controlled Trial. Cornea 2017, 36, 1521–1527. [Google Scholar] [CrossRef]
- Zrenner, E.; Tomaszewski, K.; Hamlin, J.; Layton, G.; Wood, N. Effects of multiple doses of voriconazole on the vision of healthy volunteers: A double-blind, placebo-controlled study. Ophthalmic Res. 2014, 52, 43–52. [Google Scholar] [CrossRef]
- Prakash, G.; Sharma, N.; Goel, M.; Titiyal, J.S.; Vajpayee, R.B. Evaluation of intrastromal injection of voriconazole as a therapeutic adjunctive for the management of deep recalcitrant fungal keratitis. Am. J. Ophthalmol. 2008, 146, 56–59. [Google Scholar] [CrossRef]
- Sharma, N.; Agarwal, P.; Sinha, R.; Titiyal, J.S.; Velpandian, T.; Vajpayee, R.B. Evaluation of intrastromal voriconazole injection in recalcitrant deep fungal keratitis: Case series. Br. J. Ophthalmol. 2011, 95, 1735–1737. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Chacko, J.; Velpandian, T.; Titiyal, J.S.; Sinha, R.; Satpathy, G.; Tandon, R.; Vajpayee, R.B. Comparative evaluation of topical versus intrastromal voriconazole as an adjunct to natamycin in recalcitrant fungal keratitis. Ophthalmology 2013, 120, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Garg, P.; Das, S.; Roy, A. Collagen Cross-linking for Microbial Keratitis. Middle East Afr. J. Ophthalmol. 2017, 24, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Ting, D.S.J.; Henein, C.; Said, D.G.; Dua, H.S. Photoactivated chromophore for infectious keratitis—Corneal cross-linking (PACK-CXL): A systematic review and meta-analysis. Ocul. Surf. 2019, 17, 624–634. [Google Scholar] [CrossRef] [PubMed]
- Uddaraju, M.; Mascarenhas, J.; Das, M.R.; Radhakrishnan, N.; Keenan, J.D.; Prajna, L.; Prajna, V.N. Corneal Cross-linking as an Adjuvant Therapy in the Management of Recalcitrant Deep Stromal Fungal Keratitis: A Randomized Trial. Am. J. Ophthalmol. 2015, 160, 131–134.e5. [Google Scholar] [CrossRef] [PubMed]
- Prajna, N.V.; Radhakrishnan, N.; Lalitha, P.; Austin, A.; Ray, K.J.; Keenan, J.D.; Porco, T.C.; Lietman, T.M.; Rose-Nussbaumer, J. Cross-Linking-Assisted Infection Reduction: A Randomized Clinical Trial Evaluating the Effect of Adjuvant Cross-Linking on Outcomes in Fungal Keratitis. Ophthalmology 2020, 127, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Prajna, N.V.; Sangoi, K. Commentary: Timing of therapeutic keratoplasty. Indian J. Ophthalmol. 2019, 67, 1606. [Google Scholar] [CrossRef]
- Shi, W.; Wang, T.; Xie, L.; Li, S.; Gao, H.; Liu, J.; Li, H. Risk factors, clinical features, and outcomes of recurrent fungal keratitis after corneal transplantation. Ophthalmology 2010, 117, 890–896. [Google Scholar] [CrossRef]
- Mundra, J.; Dhakal, R.; Mohamed, A.; Jha, G.; Joseph, J.; Chaurasia, S.; Murthy, S. Outcomes of therapeutic penetrating keratoplasty in 198 eyes with fungal keratitis. Indian J. Ophthalmol. 2019, 67, 1599–1605. [Google Scholar] [CrossRef]
- Upadhyay, M.P.; Karmacharya, P.C.; Koirala, S.; Shah, D.N.; Shakya, S.; Shrestha, J.K.; Bajracharya, H.; Gurung, C.K.; Whitcher, J.P. The Bhaktapur eye study: Ocular trauma and antibiotic prophylaxis for the prevention of corneal ulceration in Nepal. Br. J. Ophthalmol. 2001, 85, 388–392. [Google Scholar] [CrossRef]
- Pflugfelder, S.C.; Flynn, H.W., Jr.; Zwickey, T.A.; Forster, R.K.; Tsiligianni, A.; Culbertson, W.W.; Mandelbaum, S. Exogenous fungal endophthalmitis. Ophthalmology 1988, 95, 19–30. [Google Scholar] [CrossRef]
- Lübke, J.; Auw-Hädrich, C.; Meyer-Ter-Vehn, T.; Emrani, E.; Reinhard, T. Fusarium keratitis with dramatic outcome. Ophthalmologe 2017, 114, 462–465. [Google Scholar] [CrossRef]
- Hu, S.; Fan, V.C.; Koonapareddy, C.; Du, T.T.; Asbell, P.A. Contact lens-related Fusarium infection: Case series experience in New York City and review of fungal keratitis. Eye Contact Lens 2007, 33, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.K.; So, K.; Chung, P.H.; Tsang, H.F.; Chuang, S.K. A multi-country outbreak of fungal keratitis associated with a brand of contact lens solution: The Hong Kong experience. Int. J. Infect. Dis. 2009, 13, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Khor, W.B.; Aung, T.; Saw, S.M.; Wong, T.Y.; Tambyah, P.A.; Tan, A.L.; Beuerman, R.; Lim, L.; Chan, W.K.; Heng, W.J.; et al. An outbreak of Fusarium keratitis associated with contact lens wear in Singapore. JAMA 2006, 295, 2867–2873. [Google Scholar] [CrossRef] [PubMed]
- Charm, J.; Cheung, S.W.; Cho, P. Practitioners’ analysis of contact lens practice in Hong Kong. Contact Lens Anterior Eye 2010, 33, 104–111. [Google Scholar] [CrossRef]
- Au, L.; Saha, K.; Fernando, B.; Ataullah, S.; Spencer, F. ‘Fast-track’ cataract services and diagnostic and treatment centre: Impact on surgical training. Eye 2008, 22, 55–59. [Google Scholar] [CrossRef][Green Version]
- Gaujoux, T.; Chatel, M.A.; Chaumeil, C.; Laroche, L.; Borderie, V.M. Outbreak of contact lens-related Fusarium keratitis in France. Cornea 2008, 27, 1018–1021. [Google Scholar] [CrossRef]
- Kaufmann, C.; Frueh, B.E.; Messerli, J.; Bernauer, W.; Thiel, M.A. Contact lens-associated fusarium keratitis in Switzerland. Klin. Monbl. Augenheilkd. 2008, 225, 418–421. [Google Scholar] [CrossRef]
- Daniel, C.S.; Rajan, M.S.; Saw, V.P.; Claerhout, I.; Kestelyn, P.; Dart, J.K. Contact lens-related Fusarium keratitis in London and Ghent. Eye 2009, 23, 484–485. [Google Scholar] [CrossRef][Green Version]
- Al-Hatmi, A.M.S.; Castro, M.A.; de Hoog, G.S.; Badali, H.; Alvarado, V.F.; Verweij, P.E.; Meis, J.F.; Zago, V.V. Epidemiology of Aspergillus species causing keratitis in Mexico. Mycoses 2019, 62, 144–151. [Google Scholar] [CrossRef]
- Venugopal, P.L.; Venugopal, T.L.; Gomathi, A.; Ramakrishna, E.S.; Ilavarasi, S. Mycotic keratitis in Madras. Indian J. Pathol. Microbiol. 1989, 32, 190–197. [Google Scholar]
- Panda, A.; Sharma, N.; Das, G.; Kumar, N.; Satpathy, G. Mycotic keratitis in children: Epidemiologic and microbiologic evaluation. Cornea 1997, 16, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Chongkae, S.; Nosanchuk, J.D.; Pruksaphon, K.; Laliam, A.; Pornsuwan, S.; Youngchim, S. Production of melanin pigments in saprophytic fungi in vitro and during infection. J. Basic Microbiol. 2019, 59, 1092–1104. [Google Scholar] [CrossRef]
- Revankar, S.G.; Sutton, D.A. Melanized fungi in human disease. Clin. Microbiol. Rev. 2010, 23, 884–928. [Google Scholar] [CrossRef] [PubMed]
- Guarner, J.; Brandt, M.E. Histopathologic Diagnosis of Fungal Infections in the 21st Century. Clin. Microbiol. Rev. 2011, 24, 247–280. [Google Scholar] [CrossRef]
- Sahay, P.; Goel, S.; Nagpal, R.; Maharana, P.K.; Sinha, R.; Agarwal, T.; Sharma, N.; Titiyal, J.S. Infectious Keratitis Caused by Rare and Emerging Micro-Organisms. Curr. Eye Res. 2020, 45, 761–773. [Google Scholar] [CrossRef]
- Yew, S.M.; Chan, C.L.; Lee, K.W.; Na, S.L.; Tan, R.; Hoh, C.C.; Yee, W.Y.; Ngeow, Y.F.; Ng, K.P. A five-year survey of dematiaceous fungi in a tropical hospital reveals potential opportunistic species. PLoS ONE 2014, 9, e104352. [Google Scholar] [CrossRef]
- Wilhelmus, K.R.; Jones, D.B. Curvularia keratitis. Trans. Am. Ophthalmol. Soc. 2001, 99, 111–130. [Google Scholar]
- Wilhelmus, K.R. Climatology of dematiaceous fungal keratitis. Am. J. Ophthalmol. 2005, 140, 1156–1157. [Google Scholar] [CrossRef]
- Satpathy, G.; Ahmed, N.H.; Nayak, N.; Tandon, R.; Sharma, N.; Agarwal, T.; Vanathi, M.; Titiyal, J.S. Spectrum of mycotic keratitis in north India: Sixteen years study from a tertiary care ophthalmic centre. J. Infect. Public Health 2019, 12, 367–371. [Google Scholar] [CrossRef]
- Chowdhary, A.; Singh, K. Spectrum of fungal keratitis in North India. Cornea 2005, 24, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Ung, L.; Acharya, N.R.; Agarwal, T.; Alfonso, E.C.; Bagga, B.; Bispo, P.J.; Burton, M.J.; Dart, J.K.; Doan, T.; Fleiszig, S.M.; et al. Infectious corneal ulceration: A proposal for neglected tropical disease status. Bull. World Health Organ. 2019, 97, 854–856. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Upadhyay, M.P.; Priyadarsini, B.; Mahalakshmi, R.; Whitcher, J.P. Corneal ulceration in south-east Asia III: Prevention of fungal keratitis at the village level in south India using topical antibiotics. Br. J. Ophthalmol. 2006, 90, 1472–1475. [Google Scholar] [CrossRef] [PubMed]
- Maung, N.; Thant, C.C.; Srinivasan, M.; Upadhyay, M.P.; Priyadarsini, B.; Mahalakshmi, R.; Whitcher, J.P. Corneal ulceration in South East Asia. II: A strategy for the prevention of fungal keratitis at the village level in Burma. Br. J. Ophthalmol. 2006, 90, 968–970. [Google Scholar] [CrossRef] [PubMed]
- Getshen, K.; Srinivasan, M.; Upadhyay, M.; Priyadarsini, B.; Mahalaksmi, R.; Whitcher, J. Corneal ulceration in South East Asia. I: A model for the prevention of bacterial ulcers at the village level in rural Bhutan. Br. J. Ophthalmol. 2006, 90, 276–278. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoffman, J.J.; Burton, M.J.; Leck, A. Mycotic Keratitis—A Global Threat from the Filamentous Fungi. J. Fungi 2021, 7, 273. https://doi.org/10.3390/jof7040273
Hoffman JJ, Burton MJ, Leck A. Mycotic Keratitis—A Global Threat from the Filamentous Fungi. Journal of Fungi. 2021; 7(4):273. https://doi.org/10.3390/jof7040273
Chicago/Turabian StyleHoffman, Jeremy J., Matthew J. Burton, and Astrid Leck. 2021. "Mycotic Keratitis—A Global Threat from the Filamentous Fungi" Journal of Fungi 7, no. 4: 273. https://doi.org/10.3390/jof7040273
APA StyleHoffman, J. J., Burton, M. J., & Leck, A. (2021). Mycotic Keratitis—A Global Threat from the Filamentous Fungi. Journal of Fungi, 7(4), 273. https://doi.org/10.3390/jof7040273






