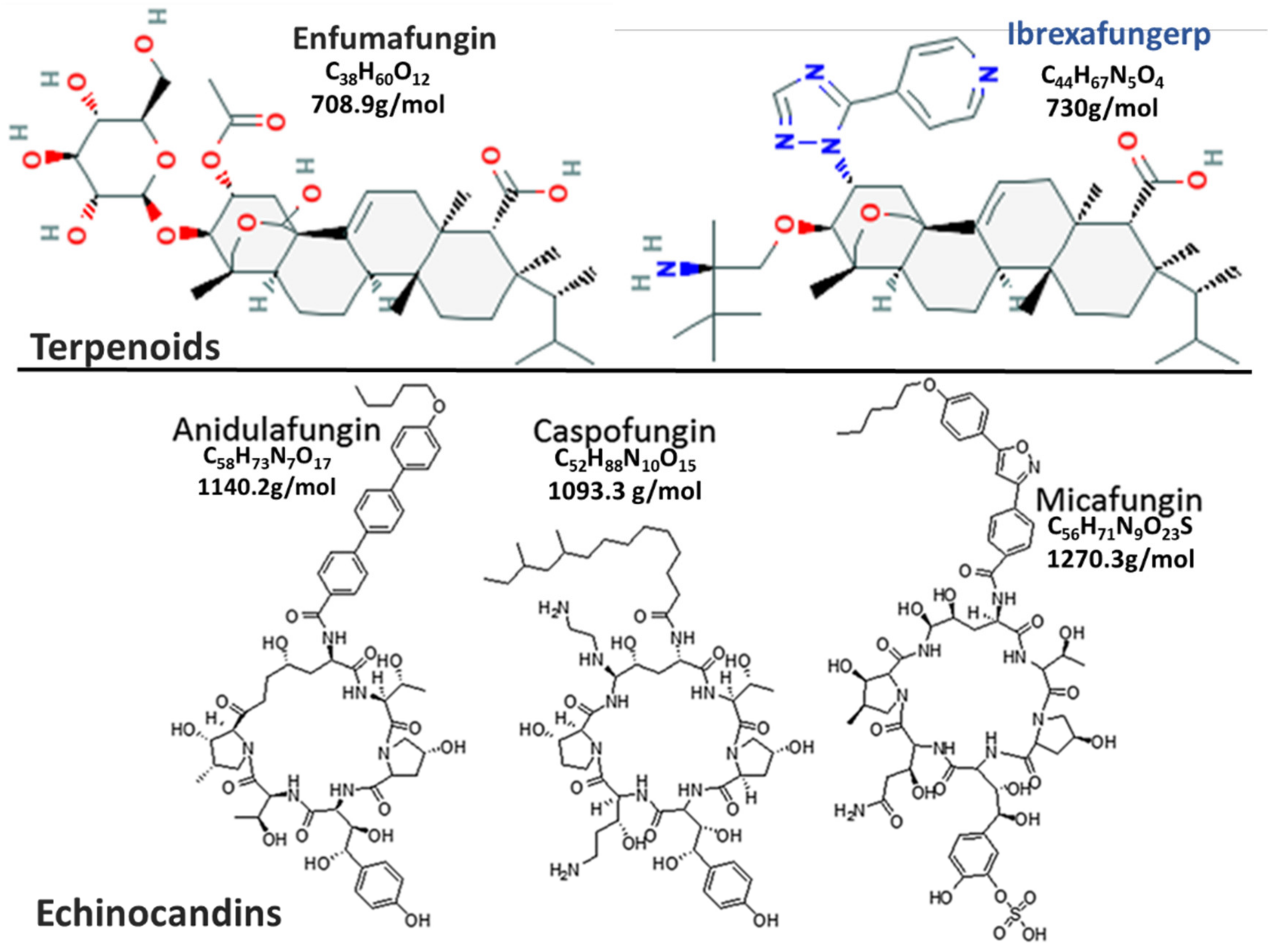
Ibrexafungerp: A First-in-Class Oral Triterpenoid Glucan Synthase Inhibitor
Abstract
1. Introduction
2. Mechanism of Action and Resistance
3. Important Pathogenic Fungi and Antifungal Spectrum
4. In Vitro Activity
5. In Vivo Data from Animal Models
6. Clinical Efficacy
7. Pharmacokinetics/Pharmacodynamics
8. Indications and Usage
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Douglas, C.M. Fungal beta(1,3)-D-glucan synthesis. Med. Mycol. 2001, 39 (Suppl. S1), 55–66. [Google Scholar] [CrossRef]
- Mikamo, H.; Sato, Y.; Tamaya, T. In vitro antifungal activity of FK463, a new water-soluble echinocandin-like lipopeptide. J. Antimicrob. Chemother. 2000, 46, 485–487. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Denning, D.W. Echinocandin antifungal drugs. Lancet 2003, 362, 1142–1151. [Google Scholar] [CrossRef]
- Merck Research Laboratories. Cancidas (Caspofungin Acetate) Injection. Application No.: 21-227. Approval Date: 26 January 2001. Food and Drug Administration, Center for Drug Evaluation and Research, Division of Special Pathogen and Immunologic Drug Products. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2001/21227_Cancidas.cfm (accessed on 29 December 2020).
- Feldmesser, M.; Kress, Y.; Mednick, A.; Casadevall, A. The effect of the echinocandin analogue caspofungin on cell wall glucan synthesis by Cryptococcus neoformans. J. Infect. Dis. 2000, 182, 1791–1795. [Google Scholar] [CrossRef]
- Kurtz, M.B.; Rex, J.H. Glucan synthase inhibitors as antifungal agents. Adv. Protein Chem. 2001, 56, 423–475. [Google Scholar] [CrossRef]
- Chandrasekar, P.H.; Sobel, J.D. Micafungin: A new echinocandin. Clin. Infect. Dis. 2006, 42, 1171–1178. [Google Scholar] [CrossRef] [PubMed]
- Vazquez, J.A.; Sobel, J.D. Anidulafungin: A novel echinocandin. Clin. Infect. Dis. 2006, 43, 215–222. [Google Scholar] [CrossRef]
- Pelaez, F.; Cabello, A.; Platas, G.; Diez, M.T.; Gonzalez del Val, A.; Basilio, A.; Martan, I.; Vicente, F.; Bills, G.E.; Giacobbe, R.A.; et al. The discovery of enfumafungin, a novel antifungal compound produced by an endophytic Hormonema species biological activity and taxonomy of the producing organisms. Syst. Appl. Microbiol. 2000, 23, 333–343. [Google Scholar] [CrossRef]
- PubChem [Internet]. Bethesda (MD): National Library of Medicine (US), National Center for Biotechnology Information; 2004-.PubChem Compound Summary. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/ (accessed on 30 December 2020).
- Coad, B.R.; Lamont-Friedrich, S.J.; Gwynne, L.; Jasieniak, M.; Griesser, S.S.; Traven, A.; Peleg, A.Y.; Griesser, H.J. Surface coatings with covalently attached caspofungin are effective in eliminating fungal pathogens. J. Mater. Chem. B 2015, 3, 8469–8476. [Google Scholar] [CrossRef] [PubMed]
- Onishi, J.; Meinz, M.; Thompson, J.; Curotto, J.; Dreikorn, S.; Rosenbach, M.; Douglas, C.; Abruzzo, G.; Flattery, A.; Kong, L.; et al. Discovery of novel antifungal (1,3)-beta-D-glucan synthase inhibitors. Antimicrob. Agents Chemother. 2000, 44, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.R.; Donnelley, M.A.; Thompson, G.R. Ibrexafungerp: A novel oral glucan synthase inhibitor. Med. Mycol. 2020, 58, 579–592. [Google Scholar] [CrossRef]
- Azie, N. A Phase 2b, Dose Finding Study Evaluating Oral Ibrexafungerp in Moderate to Severe Acute Vulvovaginal Candidiasis (DOVE). In Proceedings of the 3rd ISIDOG Congress, Porto, Portugal, 31 Octorber–3 November 2019; Available online: https://www.scynexis.com/science/publications-and-presentations/posters-and-presentations?page=2 (accessed on 29 December 2020).
- Apgar, J.M.; Wilkening, R.R.; Parker, D.L., Jr.; Meng, D.; Wildonger, K.J.; Sperbeck, D.; Greenlee, M.L.; Balkovec, J.M.; Flattery, A.M.; Abruzzo, G.K.; et al. Ibrexafungerp: An orally active beta-1,3-glucan synthesis inhibitor. Bioorg. Med. Chem. Lett. 2020. [Google Scholar] [CrossRef]
- Scynexis. The World Health Organization Recognizes New Antifungal Class by Granting “ibrexafungerp” to SCYNEXIS as the International Non-Proprietary Name for SCY-078. SCYNEXIS, Inc. Press Release Online. 2018. Available online: https://ir.scynexis.com/press-releases/detail/156/the-world-health-organization-recognizes-new-antifungal (accessed on 29 December 2020).
- Garcia-Rubio, R.; de Oliveira, H.C.; Rivera, J.; Trevijano-Contador, N. The Fungal Cell Wall: Candida, Cryptococcus, and Aspergillus Species. Front. Microbiol. 2019, 10, 2993. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Herrera, J.; Ortiz-Castellanos, L. Cell wall glucans of fungi. A review. Cell Surf. 2019, 5, 100022. [Google Scholar] [CrossRef] [PubMed]
- Fleet, G.H. Composition and structure of yeast cell walls. Curr. Top Med. Mycol. 1985, 1, 24–56. [Google Scholar] [CrossRef] [PubMed]
- Deresinski, S.C.; Stevens, D.A. Caspofungin. Clin. Infect. Dis. 2003, 36, 1445–1457. [Google Scholar] [CrossRef]
- Latge, J.P. The cell wall: A carbohydrate armour for the fungal cell. Mol. Microbiol. 2007, 66, 279–290. [Google Scholar] [CrossRef]
- Mazur, P.; Morin, N.; Baginsky, W.; el-Sherbeini, M.; Clemas, J.A.; Nielsen, J.B.; Foor, F. Differential expression and function of two homologous subunits of yeast 1,3-beta-D-glucan synthase. Mol. Cell Biol. 1995, 15, 5671–5681. [Google Scholar] [CrossRef] [PubMed]
- Dijkgraaf, G.J.; Abe, M.; Ohya, Y.; Bussey, H. Mutations in Fks1p affect the cell wall content of beta-1,3- and beta-1,6-glucan in Saccharomyces cerevisiae. Yeast 2002, 19, 671–690. [Google Scholar] [CrossRef] [PubMed]
- Kondoh, O.; Tachibana, Y.; Ohya, Y.; Arisawa, M.; Watanabe, T. Cloning of the RHO1 gene from Candida albicans and its regulation of beta-1,3-glucan synthesis. J. Bacteriol. 1997, 179, 7734–7741. [Google Scholar] [CrossRef]
- Shematek, E.M.; Braatz, J.A.; Cabib, E. Biosynthesis of the yeast cell wall. I. Preparation and properties of beta-(1 leads to 3) glucan synthetase. J. Biol. Chem. 1980, 255, 888–894. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Messer, S.A.; Motyl, M.R.; Jones, R.N.; Castanheira, M. In vitro activity of a new oral glucan synthase inhibitor (MK-3118) tested against Aspergillus spp. by CLSI and EUCAST broth microdilution methods. Antimicrob. Agents Chemother. 2013, 57, 1065–1068. [Google Scholar] [CrossRef]
- Walker, S.S.; Xu, Y.; Triantafyllou, I.; Waldman, M.F.; Mendrick, C.; Brown, N.; Mann, P.; Chau, A.; Patel, R.; Bauman, N.; et al. Discovery of a novel class of orally active antifungal beta-1,3-D-glucan synthase inhibitors. Antimicrob. Agents Chemother. 2011, 55, 5099–5106. [Google Scholar] [CrossRef]
- Scorneaux, B.; Angulo, D.; Borroto-Esoda, K.; Ghannoum, M.; Peel, M.; Wring, S. SCY-078 Is Fungicidal against Candida Species in Time-Kill Studies. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef]
- Bowman, J.C.; Hicks, P.S.; Kurtz, M.B.; Rosen, H.; Schmatz, D.M.; Liberator, P.A.; Douglas, C.M. The antifungal echinocandin caspofungin acetate kills growing cells of Aspergillus fumigatus in vitro. Antimicrob. Agents Chemother. 2002, 46, 3001–3012. [Google Scholar] [CrossRef]
- Ghannoum, M.; Long, L.; Larkin, E.L.; Isham, N.; Sherif, R.; Borroto-Esoda, K.; Barat, S.; Angulo, D. Evaluation of the Antifungal Activity of the Novel Oral Glucan Synthase Inhibitor SCY-078, Singly and in Combination, for the Treatment of Invasive Aspergillosis. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef] [PubMed]
- Jimenez-Ortigosa, C.; Perez, W.B.; Angulo, D.; Borroto-Esoda, K.; Perlin, D.S. De Novo Acquisition of Resistance to SCY-078 in Candida glabrata Involves FKS Mutations That both Overlap and Are Distinct from Those Conferring Echinocandin Resistance. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef]
- Perlin, D.S. Resistance to echinocandin-class antifungal drugs. Drug Resist. Updat. 2007, 10, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Effron, G.; Lee, S.; Park, S.; Cleary, J.D.; Perlin, D.S. Effect of Candida glabrata FKS1 and FKS2 mutations on echinocandin sensitivity and kinetics of 1,3-beta-D-glucan synthase: Implication for the existing susceptibility breakpoint. Antimicrob. Agents Chemother. 2009, 53, 3690–3699. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Kelly, R.; Kahn, J.N.; Robles, J.; Hsu, M.J.; Register, E.; Li, W.; Vyas, V.; Fan, H.; Abruzzo, G.; et al. Specific substitutions in the echinocandin target Fks1p account for reduced susceptibility of rare laboratory and clinical Candida sp. isolates. Antimicrob. Agents Chemother. 2005, 49, 3264–3273. [Google Scholar] [CrossRef]
- Ben-Ami, R.; Garcia-Effron, G.; Lewis, R.E.; Gamarra, S.; Leventakos, K.; Perlin, D.S.; Kontoyiannis, D.P. Fitness and virulence costs of Candida albicans FKS1 hot spot mutations associated with echinocandin resistance. J. Infect. Dis. 2011, 204, 626–635. [Google Scholar] [CrossRef] [PubMed]
- Alexander, B.D.; Johnson, M.D.; Pfeiffer, C.D.; Jimenez-Ortigosa, C.; Catania, J.; Booker, R.; Castanheira, M.; Messer, S.A.; Perlin, D.S.; Pfaller, M.A. Increasing echinocandin resistance in Candida glabrata: Clinical failure correlates with presence of FKS mutations and elevated minimum inhibitory concentrations. Clin. Infect. Dis. 2013, 56, 1724–1732. [Google Scholar] [CrossRef]
- Pham, C.D.; Iqbal, N.; Bolden, C.B.; Kuykendall, R.J.; Harrison, L.H.; Farley, M.M.; Schaffner, W.; Beldavs, Z.G.; Chiller, T.M.; Park, B.J.; et al. Role of FKS Mutations in Candida glabrata: MIC values, echinocandin resistance, and multidrug resistance. Antimicrob. Agents Chemother. 2014, 58, 4690–4696. [Google Scholar] [CrossRef] [PubMed]
- Chowdhary, A.; Prakash, A.; Sharma, C.; Kordalewska, M.; Kumar, A.; Sarma, S.; Tarai, B.; Singh, A.; Upadhyaya, G.; Upadhyay, S.; et al. A multicentre study of antifungal susceptibility patterns among 350 Candida auris isolates (2009-17) in India: Role of the ERG11 and FKS1 genes in azole and echinocandin resistance. J. Antimicrob. Chemother. 2018, 73, 891–899. [Google Scholar] [CrossRef]
- Kordalewska, M.; Lee, A.; Park, S.; Berrio, I.; Chowdhary, A.; Zhao, Y.; Perlin, D.S. Understanding Echinocandin Resistance in the Emerging Pathogen Candida auris. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef] [PubMed]
- Naicker, S.D.; Magobo, R.E.; Zulu, T.G.; Maphanga, T.G.; Luthuli, N.; Lowman, W.; Govender, N.P. Two echinocandin-resistant Candida glabrata FKS mutants from South Africa. Med. Mycol. Case Rep. 2016, 11, 24–26. [Google Scholar] [CrossRef]
- Nunnally, N.S.; Etienne, K.A.; Angulo, D.; Lockhart, S.R.; Berkow, E.L. In Vitro Activity of Ibrexafungerp, a Novel Glucan Synthase Inhibitor against Candida glabrata Isolates with FKS Mutations. Antimicrob. Agents Chemother. 2019, 63. [Google Scholar] [CrossRef] [PubMed]
- Perfect, J.R. The antifungal pipeline: A reality check. Nat. Rev. Drug Discov. 2017, 16, 603–616. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Pappas, P.G.; Wingard, J.R. Invasive Fungal Pathogens: Current Epidemiological Trends. Clin. Infect. Dis. 2006, 43, S3–S14. [Google Scholar] [CrossRef]
- Brown, G.D.; Denning, D.W.; Gow, N.A.; Levitz, S.M.; Netea, M.G.; White, T.C. Hidden killers: Human fungal infections. Sci. Transl. Med. 2012, 4, 165rv113. [Google Scholar] [CrossRef]
- WHO. Antimicrobial Resistance: Global Report on Surveillance; WHO (World Health Organization): Geneva, Switzerland, 2014; Available online: https://www.who.int/drugresistance/documents/surveillancereport/en/ (accessed on 5 January 2021).
- Arendrup, M.C. Update on antifungal resistance in Aspergillus and Candida. Clin. Microbiol. Infect. 2014, 20 (Suppl. S6), 42–48. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Diekema, D.J. Rare and emerging opportunistic fungal pathogens: Concern for resistance beyond Candida albicans and Aspergillus fumigatus. J. Clin. Microbiol. 2004, 42, 4419–4431. [Google Scholar] [CrossRef] [PubMed]
- Wickes, B.L. Analysis of a Candida auris Outbreak Provides New Insights into an Emerging Pathogen. J. Clin. Microbiol. 2020, 58. [Google Scholar] [CrossRef] [PubMed]
- Van Schalkwyk, E.; Mpembe, R.S.; Thomas, J.; Shuping, L.; Ismail, H.; Lowman, W.; Karstaedt, A.S.; Chibabhai, V.; Wadula, J.; Avenant, T.; et al. Epidemiologic Shift in Candidemia Driven by Candida auris, South Africa, 2016–2017(1). Emerg. Infect. Dis. 2019, 25, 1698–1707. [Google Scholar] [CrossRef] [PubMed]
- Govender, N.P.; Patel, J.; Magobo, R.E.; Naicker, S.; Wadula, J.; Whitelaw, A.; Coovadia, Y.; Kularatne, R.; Govind, C.; Lockhart, S.R.; et al. Emergence of azole-resistant Candida parapsilosis causing bloodstream infection: Results from laboratory-based sentinel surveillance in South Africa. J. Antimicrob. Chemother. 2016, 71, 1994–2004. [Google Scholar] [CrossRef]
- Fridkin, S.K.; Jarvis, W.R. Epidemiology of nosocomial fungal infections. Clin. Microbiol. Rev. 1996, 9, 499–511. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Messer, S.A.; Moet, G.J.; Jones, R.N.; Castanheira, M. Candida bloodstream infections: Comparison of species distribution and resistance to echinocandin and azole antifungal agents in Intensive Care Unit (ICU) and non-ICU settings in the SENTRY Antimicrobial Surveillance Program (2008–2009). Int. J. Antimicrob. Agents 2011, 38, 65–69. [Google Scholar] [CrossRef]
- Chowdhary, A.; Sharma, C.; Duggal, S.; Agarwal, K.; Prakash, A.; Singh, P.K.; Jain, S.; Kathuria, S.; Randhawa, H.S.; Hagen, F.; et al. New clonal strain of Candida auris, Delhi, India. Emerg. Infect. Dis. 2013, 19, 1670–1673. [Google Scholar] [CrossRef]
- Chowdhary, A.; Kumar, V.A.; Sharma, C.; Prakash, A.; Agarwal, K.; Babu, R.; Dinesh, K.R.; Karim, S.; Singh, S.K.; Hagen, F.; et al. Multidrug-resistant endemic clonal strain of Candida auris in India. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 919–926. [Google Scholar] [CrossRef] [PubMed]
- Lockhart, S.R.; Etienne, K.A.; Vallabhaneni, S.; Farooqi, J.; Chowdhary, A.; Govender, N.P.; Colombo, A.L.; Calvo, B.; Cuomo, C.A.; Desjardins, C.A.; et al. Simultaneous Emergence of Multidrug-Resistant Candida auris on 3 Continents Confirmed by Whole-Genome Sequencing and Epidemiological Analyses. Clin. Infect. Dis. 2017, 64, 134–140. [Google Scholar] [CrossRef]
- Lockhart, S.R.; Jackson, B.R.; Vallabhaneni, S.; Ostrosky-Zeichner, L.; Pappas, P.G.; Chiller, T. Thinking beyond the Common Candida Species: Need for Species-Level Identification of Candida Due to the Emergence of Multidrug-Resistant Candida auris. J. Clin. Microbiol. 2017, 55, 3324–3327. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.C.; Barat, S.A.; Borroto-Esoda, K.; Angulo, D.; Chaturvedi, S.; Chaturvedi, V. Pan-resistant Candida auris isolates from the outbreak in New York are susceptible to ibrexafungerp (a glucan synthase inhibitor). Int. J. Antimicrob. Agents 2020, 55, 105922. [Google Scholar] [CrossRef]
- Ostrowsky, B.; Greenko, J.; Adams, E.; Quinn, M.; O’Brien, B.; Chaturvedi, V.; Berkow, E.; Vallabhaneni, S.; Forsberg, K.; Chaturvedi, S.; et al. Candida auris Isolates Resistant to Three Classes of Antifungal Medications-New York, 2019. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Osei Sekyere, J. Candida auris: A systematic review and meta-analysis of current updates on an emerging multidrug-resistant pathogen. Microbiologyopen 2018, 7, e00578. [Google Scholar] [CrossRef]
- Sabino, R.; Verissimo, C.; Pereira, A.A.; Antunes, F. Candida auris, an Agent of Hospital-Associated Outbreaks: Which Challenging Issues Do We Need to Have in Mind? Microorganisms 2020, 8, 181. [Google Scholar] [CrossRef]
- Chaabane, F.; Graf, A.; Jequier, L.; Coste, A.T. Review on Antifungal Resistance Mechanisms in the Emerging Pathogen Candida auris. Front Microbiol. 2019, 10, 2788. [Google Scholar] [CrossRef]
- Forsberg, K.; Woodworth, K.; Walters, M.; Berkow, E.L.; Jackson, B.; Chiller, T.; Vallabhaneni, S. Candida auris: The recent emergence of a multidrug-resistant fungal pathogen. Med. Mycol. 2019, 57, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Govender, N.P.; Magobo, R.E.; Mpembe, R.; Mhlanga, M.; Matlapeng, P.; Corcoran, C.; Govind, C.; Lowman, W.; Senekal, M.; Thomas, J. Candida auris in South Africa, 2012–2016. Emerg. Infect. Dis. 2018, 24, 2036–2040. [Google Scholar] [CrossRef] [PubMed]
- Magobo, R.E.; Corcoran, C.; Seetharam, S.; Govender, N.P. Candida auris-associated candidemia, South Africa. Emerg. Infect. Dis. 2014, 20, 1250–1251. [Google Scholar] [CrossRef] [PubMed]
- Patterson, T.F.; Kirkpatrick, W.R.; White, M.; Hiemenz, J.W.; Wingard, J.R.; Dupont, B.; Rinaldi, M.G.; Stevens, D.A.; Graybill, J.R. Invasive aspergillosis. Disease spectrum, treatment practices, and outcomes. I3 Aspergillus Study Group. Medicine 2000, 79, 250–260. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.J.; Schranz, J.; Teutsch, S.M. Aspergillosis case-fatality rate: Systematic review of the literature. Clin. Infect. Dis. 2001, 32, 358–366. [Google Scholar] [CrossRef]
- Vermeulen, E.; Maertens, J.; de Bel, A.; Nulens, E.; Boelens, J.; Surmont, I.; Mertens, A.; Boel, A.; Lagrou, K. Nationwide Surveillance of Azole Resistance in Aspergillus Diseases. Antimicrob. Agents Chemother. 2015, 59, 4569–4576. [Google Scholar] [CrossRef]
- Snelders, E.; van der Lee, H.A.; Kuijpers, J.; Rijs, A.J.; Varga, J.; Samson, R.A.; Mellado, E.; Donders, A.R.; Melchers, W.J.; Verweij, P.E. Emergence of azole resistance in Aspergillus fumigatus and spread of a single resistance mechanism. PLoS Med. 2008, 5, e219. [Google Scholar] [CrossRef] [PubMed]
- Snelders, E.; Huis In ‘t Veld, R.A.; Rijs, A.J.; Kema, G.H.; Melchers, W.J.; Verweij, P.E. Possible environmental origin of resistance of Aspergillus fumigatus to medical triazoles. Appl. Environ. Microbiol. 2009, 75, 4053–4057. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, T.G.; Perfect, J.R. Cryptococcosis in the era of AIDS–100 years after the discovery of Cryptococcus neoformans. Clin. Microbiol. Rev. 1995, 8, 515–548. [Google Scholar] [CrossRef] [PubMed]
- Walzer, P.D.; Evans, H.E.; Copas, A.J.; Edwards, S.G.; Grant, A.D.; Miller, R.F. Early predictors of mortality from Pneumocystis jirovecii pneumonia in HIV-infected patients: 1985-2006. Clin. Infect. Dis. 2008, 46, 625–633. [Google Scholar] [CrossRef]
- Duncan, R.A.; von Reyn, C.F.; Alliegro, G.M.; Toossi, Z.; Sugar, A.M.; Levitz, S.M. Idiopathic CD4+ T-lymphocytopenia--four patients with opportunistic infections and no evidence of HIV infection. N. Engl. J. Med. 1993, 328, 393–398. [Google Scholar] [CrossRef]
- Reid, A.B.; Chen, S.C.; Worth, L.J. Pneumocystis jirovecii pneumonia in non-HIV-infected patients: New risks and diagnostic tools. Curr. Opin. Infect. Dis. 2011, 24, 534–544. [Google Scholar] [CrossRef]
- Porollo, A.; Meller, J.; Joshi, Y.; Jaiswal, V.; Smulian, A.G.; Cushion, M.T. Analysis of current antifungal agents and their targets within the Pneumocystis carinii genome. Curr. Drug Targets 2012, 13, 1575–1585. [Google Scholar] [CrossRef] [PubMed]
- Kaneshiro, E.S.; Ellis, J.E.; Jayasimhulu, K.; Beach, D.H. Evidence for the presence of “metabolic sterols” in Pneumocystis: Identification and initial characterization of Pneumocystis carinii sterols. J. Eukaryot Microbiol. 1994, 41, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Malamba, S.; Sandison, T.; Lule, J.; Reingold, A.; Walker, J.; Dorsey, G.; Mermin, J. Plasmodium falciparum dihydrofolate reductase and dihyropteroate synthase mutations and the use of trimethoprim-sulfamethoxazole prophylaxis among persons infected with human immunodeficiency virus. Am. J. Trop. Med. Hyg. 2010, 82, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.C.; Slavin, M.A.; Sorrell, T.C. Echinocandin antifungal drugs in fungal infections: A comparison. Drugs 2011, 71, 11–41. [Google Scholar] [CrossRef] [PubMed]
- Eschenauer, G.; Depestel, D.D.; Carver, P.L. Comparison of echinocandin antifungals. Ther. Clin. Risk Manag. 2007, 3, 71–97. [Google Scholar] [CrossRef]
- De la Torre, P.; Meyer, D.K.; Reboli, A.C. Anidulafungin: A novel echinocandin for candida infections. Future Microbiol. 2008, 3, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Jimenez-Ortigosa, C.; Paderu, P.; Motyl, M.R.; Perlin, D.S. Enfumafungin derivative MK-3118 shows increased in vitro potency against clinical echinocandin-resistant Candida Species and Aspergillus species isolates. Antimicrob. Agents Chemother. 2014, 58, 1248–1251. [Google Scholar] [CrossRef]
- Cushion, M.; Ashbaugh, A.; Borroto-Esoda, K.; Barat, S.A.; Angulo, D. SCY-078 demonstrates antifungal activity against pneumocystis in a prophylactic murine model of pneumocystis pneumonia. ASM Microbe Online 2018. [Google Scholar] [CrossRef]
- Espinel-Ingroff, A. Comparison of In vitro activities of the new triazole SCH56592 and the echinocandins MK-0991 (L-743,872) and LY303366 against opportunistic filamentous and dimorphic fungi and yeasts. J. Clin. Microbiol. 1998, 36, 2950–2956. [Google Scholar] [CrossRef] [PubMed]
- Maligie, M.A.; Selitrennikoff, C.P. Cryptococcus neoformans resistance to echinocandins: (1,3)beta-glucan synthase activity is sensitive to echinocandins. Antimicrob. Agents Chemother. 2005, 49, 2851–2856. [Google Scholar] [CrossRef] [PubMed]
- Marcos-Zambrano, L.J.; Gomez-Perosanz, M.; Escribano, P.; Bouza, E.; Guinea, J. The novel oral glucan synthase inhibitor SCY-078 shows in vitro activity against sessile and planktonic Candida spp. J. Antimicrob. Chemother. 2017, 72, 1969–1976. [Google Scholar] [CrossRef]
- Larkin, E.; Hager, C.; Chandra, J.; Mukherjee, P.K.; Retuerto, M.; Salem, I.; Long, L.; Isham, N.; Kovanda, L.; Borroto-Esoda, K.; et al. The Emerging Pathogen Candida auris: Growth Phenotype, Virulence Factors, Activity of Antifungals, and Effect of SCY-078, a Novel Glucan Synthesis Inhibitor, on Growth Morphology and Biofilm Formation. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Messer, S.A.; Rhomberg, P.R.; Borroto-Esoda, K.; Castanheira, M. Differential Activity of the Oral Glucan Synthase Inhibitor SCY-078 against Wild-Type and Echinocandin-Resistant Strains of Candida Species. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef]
- Schell, W.A.; Jones, A.M.; Borroto-Esoda, K.; Alexander, B.D. Antifungal Activity of SCY-078 and Standard Antifungal Agents against 178 Clinical Isolates of Resistant and Susceptible Candida Species. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef]
- Berkow, E.L.; Angulo, D.; Lockhart, S.R. In Vitro Activity of a Novel Glucan Synthase Inhibitor, SCY-078, against Clinical Isolates of Candida auris. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef]
- Ghannoum, M.; Long, L.; Isham, N.; Hager, C.; Wilson, R.; Borroto-Esoda, K.; Barat, S.; Angulo, D. Activity of a novel 1,3-beta-D-glucan Synthase Inhibitor, Ibrexafungerp (formerly SCY-078), Against Candida glabrata. Antimicrob. Agents Chemother. 2019. [Google Scholar] [CrossRef] [PubMed]
- Arendrup, M.C.; Jorgensen, K.M.; Hare, R.K.; Chowdhary, A. In Vitro Activity of Ibrexafungerp (SCY-078) against Candida auris Isolates as Determined by EUCAST Methodology and Comparison with Activity against C. albicans and C. glabrata and with the Activities of Six Comparator Agents. Antimicrob. Agents Chemother. 2020, 64. [Google Scholar] [CrossRef]
- Zhu, Y.C.; Barat, S.A.; Borroto-Esoda, K.; Angulo, D.; Chaturvedi, S.; Chaturvedi, V. In vitro Efficacy of Novel Glucan Synthase Inhibitor, Ibrexafungerp (SCY-078), Against Multidrug- and Pan-resistant Candida auris Isolates from the Outbreak in New York. BioRxiv 2020. [Google Scholar] [CrossRef]
- Chandra, J.; Mukherjee, P.K.; Leidich, S.D.; Faddoul, F.F.; Hoyer, L.L.; Douglas, L.J.; Ghannoum, M.A. Antifungal resistance of candidal biofilms formed on denture acrylic in vitro. J. Dent. Res. 2001, 80, 903–908. [Google Scholar] [CrossRef] [PubMed]
- Cowen, L.E.; Sanglard, D.; Howard, S.J.; Rogers, P.D.; Perlin, D.S. Mechanisms of Antifungal Drug Resistance. Cold Spring Harb. Perspect Med. 2014, 5, a019752. [Google Scholar] [CrossRef]
- Ghannoum, M.; Long, L.; Sherif, R.; Abidi, F.Z.; Borroto-Esoda, K.; Barat, S.; Angulo, D.; Wiederhold, N. Determination of Antifungal Activity of SCY-078, a Novel Glucan Synthase Inhibitor, Against a broad panel of Rare Pathogenic Fungi. ASM Microbe Online 2020. [Google Scholar] [CrossRef]
- Larkin, E.L.; Long, L.; Isham, N.; Borroto-Esoda, K.; Barat, S.; Angulo, D.; Wring, S.; Ghannoum, M. A Novel 1,3-Beta-d-Glucan Inhibitor, Ibrexafungerp (Formerly SCY-078), Shows Potent Activity in the Lower pH Environment of Vulvovaginitis. Antimicrob. Agents Chemother. 2019, 63. [Google Scholar] [CrossRef]
- Odds, F.C.; Brown, A.J.; Gow, N.A. Antifungal agents: Mechanisms of action. Trends Microbiol. 2003, 11, 272–279. [Google Scholar] [CrossRef]
- Rocha, E.M.; Garcia-Effron, G.; Park, S.; Perlin, D.S. A Ser678Pro substitution in Fks1p confers resistance to echinocandin drugs in Aspergillus fumigatus. Antimicrob. Agents Chemother. 2007, 51, 4174–4176. [Google Scholar] [CrossRef]
- Lamoth, F.; Alexander, B.D. Antifungal activities of SCY-078 (MK-3118) and standard antifungal agents against clinical non-Aspergillus mold isolates. Antimicrob. Agents Chemother. 2015, 59, 4308–4311. [Google Scholar] [CrossRef]
- Wiederhold, N.P.; Najvar, L.K.; Jaramillo, R.; Olivo, M.; Pizzini, J.; Catano, G.; Patterson, T.F. Oral glucan synthase inhibitor SCY-078 is effective in an experimental murine model of invasive candidiasis caused by WT and echinocandin-resistant Candida glabrata. J. Antimicrob. Chemother. 2018, 73, 448–451. [Google Scholar] [CrossRef]
- Lepak, A.J.; Marchillo, K.; Andes, D.R. Pharmacodynamic target evaluation of a novel oral glucan synthase inhibitor, SCY-078 (MK-3118), using an in vivo murine invasive candidiasis model. Antimicrob. Agents Chemother. 2015, 59, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Wring, S.A.; Randolph, R.; Park, S.; Abruzzo, G.; Chen, Q.; Flattery, A.; Garrett, G.; Peel, M.; Outcalt, R.; Powell, K.; et al. Preclinical Pharmacokinetics and Pharmacodynamic Target of SCY-078, a First-in-Class Orally Active Antifungal Glucan Synthesis Inhibitor, in Murine Models of Disseminated Candidiasis. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef] [PubMed]
- Ghannoum, M.; Isham, N.; Angulo, D.; Borroto-Esoda, K.; Barat, S.; Long, L. Efficacy of Ibrexafungerp (SCY-078) against Candida auris in an In Vivo Guinea Pig Cutaneous Infection Model. Antimicrob. Agents Chemother. 2020, 64. [Google Scholar] [CrossRef]
- Vergidis, P.; Clancy, C.J.; Shields, R.K.; Park, S.Y.; Wildfeuer, B.N.; Simmons, R.L.; Nguyen, M.H. Intra-Abdominal Candidiasis: The Importance of Early Source Control and Antifungal Treatment. PLoS ONE 2016, 11, e0153247. [Google Scholar] [CrossRef]
- Lee, A.; Prideaux, B.; Zimmerman, M.; Carter, C.; Barat, S.; Angulo, D.; Dartois, V.; Perlin, D.S.; Zhao, Y. Penetration of Ibrexafungerp (Formerly SCY-078) at the Site of Infection in an Intra-abdominal Candidiasis Mouse Model. Antimicrob. Agents Chemother. 2020, 64. [Google Scholar] [CrossRef]
- Borroto-Esoda, K.; Barat, S.; Angulo, D.; Holden, K.; Warn, P. SCY-078 Demonstrates Significant Antifungal Activity in a Murine Model of Invasive Aspergillosis. Open Forum Infect. Dis. 2017, 4, S472. [Google Scholar] [CrossRef]
- Petraitis, V.; Petraitiene, R.; Katragkou, A.; Maung, B.B.W.; Naing, E.; Kavaliauskas, P.; Barat, S.; Borroto-Esoda, K.; Azie, N.; Angulo, D.; et al. Combination Therapy with Ibrexafungerp (Formerly SCY-078), a First-in-Class Triterpenoid Inhibitor of (1-->3)-beta-d-Glucan Synthesis, and Isavuconazole for Treatment of Experimental Invasive Pulmonary Aspergillosis. Antimicrob. Agents Chemother. 2020, 64. [Google Scholar] [CrossRef] [PubMed]
- Barat, S.A.; Borroto-Esoda, K.; Angulo, D.; Ashbaugh, A.; Cushion, M. Efficacy of Ibrexafungerp (formerly SCY-078) in a Murine Treatment Model of Pneumocystis Pneumonia. ASM Microbe Online. 2019. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwjftpvlt4TvAhWzQEEAHTPRAjUQFjAAegQIAhAD&url=https%3A%2F%2Fd1io3yog0oux5.cloudfront.net%2F_b4b7034c330a452751c9d7c806d956ea%2Fscynexis%2Fdb%2F385%2F2952%2Fpdf%2FBARAT%2BASM2019%2BPneumocystis_final.pdf&usg=AOvVaw3kok9W_OsTJ6m6dJlFXIG_ (accessed on 5 January 2021).
- Spec, A.; Pullman, J.; Thompson, G.R.; Powderly, W.G.; Tobin, E.H.; Vazquez, J.; Wring, S.A.; Angulo, D.; Helou, S.; Pappas, P.G.; et al. MSG-10: A Phase 2 study of oral ibrexafungerp (SCY-078) following initial echinocandin therapy in non-neutropenic patients with invasive candidiasis. J. Antimicrob. Chemother. 2019, 74, 3056–3062. [Google Scholar] [CrossRef] [PubMed]
- Wring, S.; Murphy, G.; Atiee, G.; Corr, C.; Hyman, M.; Willett, M.; Angulo, D. Lack of Impact by SCY-078, a First-in-Class Oral Fungicidal Glucan Synthase Inhibitor, on the Pharmacokinetics of Rosiglitazone, a Substrate for CYP450 2C8, Supports the Low Risk for Clinically Relevant Metabolic Drug-Drug Interactions. J. Clin. Pharmacol. 2018, 58, 1305–1313. [Google Scholar] [CrossRef] [PubMed]
- Wring, S.; Murphy, G.; Atiee, G.; Corr, C.; Hyman, M.; Willett, M.; Angulo, D. Clinical Pharmacokinetics and Drug-Drug Interaction Potential for Coadministered SCY-078, an Oral Fungicidal Glucan Synthase Inhibitor, and Tacrolimus. Clin. Pharmacol. Drug Dev. 2019, 8, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Azie, N.; Angulo, D.; Dehn, B.; Sobel, J.D. Oral Ibrexafungerp: An investigational agent for the treatment of vulvovaginal candidiasis. Expert Opin. Investig. Drugs 2020, 29, 893–900. [Google Scholar] [CrossRef] [PubMed]
- Juneja, D.; Singh, O.; Tarai, B.; Angulo, D. Successful Treatment of Two Patients with Candida auris Candidemia with the Investigational Agent, Oral Ibrexafungerp (formerly SCY-078) from the CARES Study. In Proceedings of the 29th ECCMID Congress, Amsterdam, The Netherlands, 13–16 April 2019. [Google Scholar]
- Cadet, R.; Tufa, M.; Angulo, D.; Nyirjesy, P. A Phase 2b, Dose-Finding Study Evaluating Oral Ibrexafungerp vs Fluconazole in Vulvovaginal Candidiasis (DOVE). Obstet. Gynecol. 2019, 133, 113S–114S. [Google Scholar] [CrossRef]
- Schwebke, J.R.; Sorkin-Wells, V.; Azie, N.; Angulo, D.; Sobel, J. Oral ibrexafungerp efficacy and safety in the treatment of vulvovaginal candidiasis: A phase 3, randomized, blinded, study vs. placebo (VANISH-303). IDSOG Oral Present. 2020, 223, 964–965. [Google Scholar] [CrossRef]
- Scynexis. SCYNEXIS Announces Positive Top-Line Results from Its Second Pivotal Phase 3 Study (VANISH-306) of Oral Ibrexafungerp for the Treatment of Vulvovaginal Candidiasis (Vaginal Yeast Infection). SCYNEXIS, Inc. Press Release Online. 2020. Available online: https://www.globenewswire.com/news-release/2020/04/21/2019183/0/en/SCYNEXIS-Announces-Positive-Top-Line-Results-from-its-Second-Pivotal-Phase-3-Study-VANISH-306-of-Oral-Ibrexafungerp-for-the-Treatment-of-Vulvovaginal-Candidiasis-Vaginal-Yeast-Infe.html (accessed on 29 December 2020).
- Scynexis. SCYNEXIS Completes Patient Enrollment Ahead of Schedule in the Second Pivotal Phase 3 Study (VANISH-306) of Oral Ibrexafungerp for the Treatment of Vulvovaginal Candidiasis (Vaginal Yeast Infection). SCYNEXIS, Inc. Press Release Online. 2020. Available online: https://www.scynexis.com/news-media/press-releases/detail/201/scynexis-completes-patient-enrollment-ahead-of-schedule-in (accessed on 29 December 2020).
- Alexander, B.D.; Cornely, O.A.; Pappas, P.G.; Miller, R.; Johnson, M.; Vazquez, J.; Ostrosky-Zeichner, L.; Spec, A.; Rautemaa-Richardson, R.; Krause, R.; et al. Efficacy and Safety of Oral Ibrexafungerpin 41 Patients with Refractory Fungal Diseases, Interim Analysis of a Phase 3 Open-label Study (FURI). Poster Presented at ID Week 2020 Online. 2019. Available online: https://www.scynexis.com/science/publications-and-presentations/posters-and-presentations (accessed on 29 December 2020).
- Wring, S.; Borroto-Esoda, K.; Solon, E.; Angulo, D. SCY-078, a Novel Fungicidal Agent, Demonstrates Distribution to Tissues Associated with Fungal Infections during Mass Balance Studies with Intravenous and Oral [(14)C]SCY-078 in Albino and Pigmented Rats. Antimicrob. Agents Chemother. 2019, 63. [Google Scholar] [CrossRef] [PubMed]
- Murphy, G.; Hyman, M.; Willett, M.; Angulo, D. CYP-mediated Drug Interaction Profile of SCY-078, a novel Glucan Synthase Inhibitor (GSI). Poster Presentation, ASM Microbe Online. 2017. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwi75vS8uYTvAhWEi1wKHcfgDTwQFjABegQIARAD&url=https%3A%2F%2Fd1io3yog0oux5.cloudfront.net%2F_55b477ff244a9c3da81d223259d3ec5d%2Fscynexis%2Fdb%2F385%2F2578%2Fpdf%2FPOSTER_CYP-mediated%2BDrug%2BInteraction%2BProfile%2Bof%2BSCY-078%2Ba%2Bnovel%2BGlucan%2BSynthase%2BInhibitor%2B%2528GSI%2529_ASM%2BMicrobe%2B2017.pdf&usg=AOvVaw2CGBLOrIAWaPSRo1h4F1sJ (accessed on 5 January 2021).
- Lecointre, K.; Furlan, V.; Taburet, A.M. In vitro effects of tacrolimus on human cytochrome P450. Fundam Clin. Pharmacol. 2002, 16, 455–460. [Google Scholar] [CrossRef]
- Scynexis. SCYNEXIS Announces FDA Acceptance and Priority Review of New Drug Application for Oral Ibrexafungerp for the Treatment of Vaginal Yeast Infections. SCYNEXIS, Inc. Press Release Online. 2020. Available online: https://ir.scynexis.com/press-releases/detail/225/scynexis-announces-fda-acceptance-and-priority-review-of (accessed on 29 December 2020).
- Scynexis. SCYNEXIS Announces Interim Results from Phase 2 Study of Oral SCY-078 in Patients with Invasive Candidiasis. scyNEXIS, Inc. Press Release Online. 2016. Available online: https://www.scynexis.com/news-media/press-releases/detail/79/scynexis-announces-interim-results-from-phase-2-study-of (accessed on 29 December 2020).
- Scynexis. Ibrexafungerp: First Representative of a Novel Oral/IV Antifungal Family (vF_SCYX Corporate Presentation-Dec.2020.pdf). Corporate Presentation—Dec. 2020 Online. 2020. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwjtg9GAuYTvAhVfQUEAHTwIBcsQFjAAegQIAhAD&url=https%3A%2F%2Fd1io3yog0oux5.cloudfront.net%2F_3e9cb56306763226218d943b224cb4f9%2Fscynexis%2Fdb%2F334%2F2840%2Fpdf%2FvF_SCYX%2BCorporate%2BPresentation%2B-%2BDec.2020.pdf&usg=AOvVaw2QYCiPbuPvtHgLjRPxjULt (accessed on 29 December 2020).
- Kneale, M.; Bartholomew, J.S.; Davies, E.; Denning, D.W. Global access to antifungal therapy and its variable cost. J. Antimicrob. Chemother. 2016, 71, 3599–3606. [Google Scholar] [CrossRef]
- Mycamine (Micafungin Sodium) Injection. Fujisawa Healthcare, Inc. Application No.: 021506. Approval Date: 16 March 2005. Food and Drug Administration, Center for Drug Evaluation and Research, Division of Special Pathogen and Immunologic Drug Products. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2005/21-506_Mycamine.cfm (accessed on 29 December 2020).
- Eraxis (Anidulafungin) Injection. Vicuron Pharmaceuticals Inc. Application No.: 021632 & 021948, 17 February 2006. Food and Drug Administration, Center for Drug Evaluation and Research, Division of Special Pathogen and Immunologic Drug Products. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2006/021632_021948_EraxisTOC.cfm (accessed on 29 December 2020).
- SAHPRA. South African Health Products Regulatory Authority Registered Health Products. 2021. Available online: https://www.sahpra.org.za/registered-health-products/ (accessed on 17 January 2021).

| Phase | NCT Number | Acronym | Title | Conditions | Drugs | Outcome Measures | Age (yrs) | # | Start Date | End Date |
|---|---|---|---|---|---|---|---|---|---|---|
| Phase 1 | NCT04307082 | ADME | ADME Study of [14C]-Ibrexafungerp in Healthy Male Subjects | Fungal Infection | [14C]-Ibrexafungerp (IBX) | Mass balance|Routes & rates of elimination of [14C]-IBX |Number of subjects with treatment-emergent adverse events | 30–65 | 6 | 5 December 2019 | 30 June 2020 |
| Phase 1 | NCT04092751 | Study to Evaluate the Effect of SCY-078 (Ibrexafungerp) on the PK of Pravastatin in Healthy Subjects | Pharmacokinetics | PRA| SCY-078 plus PRA | Pharmacokinetics of PRA + SCY-078: AUC, Cmax, Tmax, Half-life |Safety & tolerability of the oral combination PRA + SCY-078 | 18–55 | 28 | 22 November 2019 | 20 December 2019 | |
| Phase 1 | NCT04092725 | Study to Evaluate the Effect of SCY-078 on the PK of Dabigatran in Healthy Subjects | Pharmacokinetics | DAB|SCY-078 plus DAB | Pharmacokinetics of DAB + SCY-078: AUC, Cmax, Tmax, Half-life |Safety & tolerability of the oral combination DAB + SCY-078 | 18–55 | 36 | 9 September 2019 | 3 January 2020 | |
| Phase 2 | NCT02244606 | Oral Ibrexafungerp (SCY-078) vs Standard-of-Care Following IV Echinocandin in the Treatment of Invasive Candidiasis | Mycoses, Candidiasis, Invasive, Candidemia | SCY-078|Fluconazole| Micafungin | Safety & tolerability, assessed by adverse events, clinical laboratory results, physical examination findings, ECG results, & vital sign measurements|Dose of SCY-078 that achieves the target exposure (AUC)|Global response| Clinical response| Microbiological response|Relapse | 18–80 | 27 | 1 September 2014 | August 2016 | |
| Phase 2 | NCT02679456 | Safety and Efficacy of Oral Ibrexafungerp (SCY-078) vs. Oral Fluconazole in Subjects With Vulvovaginal Candidiasis | Vulvovaginal Candidiasis | SCY-078|Fluconazole | % of subjects achieving therapeutic cure at TOC visit (Day 24 +/-3)|% of subjects with recurrence of VVC during the observation period | 18–65 | 96 | 1 November 2015 | 5 August 2016 | |
| Phase 2 | NCT03253094 | DOVE | An Active-Controlled, Dose-Finding Study of Oral IBX vs. Oral Fluconazole in Subjects With Acute Vulvovaginal Candidiasis | Candida Vulvovaginitis | Fluconazole|SCY-078 | Clinical cure (complete resolution of signs & symptoms)|Co-occurrence of clinical & mycological cure | 18–100 | 186 | 1 August 2017 | 4 May 2018 |
| Phase 2 | NCT03672292 | SCYNERGIA | Study to Evaluate the Safety and Efficacy of the Coadministration of Ibrexafungerp (SCY-078) With Voriconazole in Patients With Invasive Pulmonary Aspergillosis | Invasive Pulmonary Aspergillosis | SCY-078|Voriconazole| Oral Placebo Tablets | Adverse events; discontinuation due to AE; death|Composite clinical, radiological & mycological response (global response)| Death| Change in serum GMI|Study & comparator plasma concentrations | ≥18 | 60 | 22 January 2019 | 7 June 2021 |
| Phase 3 | NCT03987620 | Vanish 306 | Efficacy and Safety of Oral Ibrexafungerp (SCY-078) vs. Placebo in Subjects With Acute Vulvovaginal Candidiasis | Candida Vulvovaginitis | Ibrexafungerp|Placebo | Clinical cure (complete resolution of signs & symptoms)|Mycological eradication (negative culture for growth of yeast)|Clinical cure & mycological eradication (responder outcome)|Complete resolution of signs 7 symptoms at follow-up|Safety & tolerability of IBX | ≥12 | 366 | 7 June 2019 | 29 April 2020 |
| Phase 3 | NCT03734991 | Vanish 303 | Efficacy and Safety of Oral Ibrexafungerp (SCY-078) vs. Placebo in Subjects With Acute Vulvovaginal Candidiasis (VANISH 303) | Candida Vulvovaginitis | Ibrexafungerp|Placebo | Clinical cure (complete resolution of signs & symptoms) | Mycological eradication (negative culture for yeast growth) |Clinical cure & mycological eradication (responder outcome) |Complete resolution of signs & symptoms at follow-up| subjects with treatment-related adverse events | ≥12 | 376 | 4 January 2019 | 4 September 2019 |
| Phase 3 | NCT03059992 | FURI | Study to Evaluate the Efficacy and Safety of Ibrexafungerp in Patients With Fungal Diseases That Are Refractory to or Intolerant of Standard Antifungal Treatment | Candidiasis (Invasive, Mucocutaneous, Recurrent Vulvovaginal)| Coccidioido- mycosis| Histoplasmosis| Blastomycosis |Aspergillosis (Chronic & Invasive Pulmonary, Allergic Bronchopulmonary |Other Emerging Fungi | Ibrexafungerp | Assessment of Global Response|Assessment of Recurrence of Baseline Fungal Infection|Assessment of survival | ≥12 | 200 | 1 April 2017 | 5 December 2021 |
| Phase 3 | NCT04029116 | CANDLE | Phase 3 Study of Oral Ibrexafungerp (SCY-078) Vs. Placebo in Subjects With Recurrent Vulvovaginal Candidiasis (VVC) | Recurrent Vulvovaginal Candidiasis | Fluconazole Tablet| IBX| Placebo oral tablet | Clinical Success|The percentage of subjects with no Mycologically Proven Recurrence|Safety & tolerability | ≥12 | 320 | 23 September 2019 | September, 2021 |
| Phase 3 | NCT03363841 | CARES | Open-Label Study to Evaluate the Efficacy and Safety of Oral Ibrexafungerp (SCY-078) in Patients With Candidiasis Caused by Candida Auris (CARES) | Candidiasis, Invasive Candidemia | SCY-078 | Efficacy as measured by % of subjects with global success at end of treatment|Participants with treatment-related Adverse Events |Participants with Discontinuations due to Adverse Events |Recurrence of Baseline Fungal Infection| Survival | ≥18 | 30 | 15 November 2017 | 15 May 2021 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jallow, S.; Govender, N.P. Ibrexafungerp: A First-in-Class Oral Triterpenoid Glucan Synthase Inhibitor. J. Fungi 2021, 7, 163. https://doi.org/10.3390/jof7030163
Jallow S, Govender NP. Ibrexafungerp: A First-in-Class Oral Triterpenoid Glucan Synthase Inhibitor. Journal of Fungi. 2021; 7(3):163. https://doi.org/10.3390/jof7030163
Chicago/Turabian StyleJallow, Sabelle, and Nelesh P. Govender. 2021. "Ibrexafungerp: A First-in-Class Oral Triterpenoid Glucan Synthase Inhibitor" Journal of Fungi 7, no. 3: 163. https://doi.org/10.3390/jof7030163
APA StyleJallow, S., & Govender, N. P. (2021). Ibrexafungerp: A First-in-Class Oral Triterpenoid Glucan Synthase Inhibitor. Journal of Fungi, 7(3), 163. https://doi.org/10.3390/jof7030163







