Candida albicans—The Virulence Factors and Clinical Manifestations of Infection
Abstract
1. Introduction
1.1. Fungal Infection
1.2. Candida Albicans
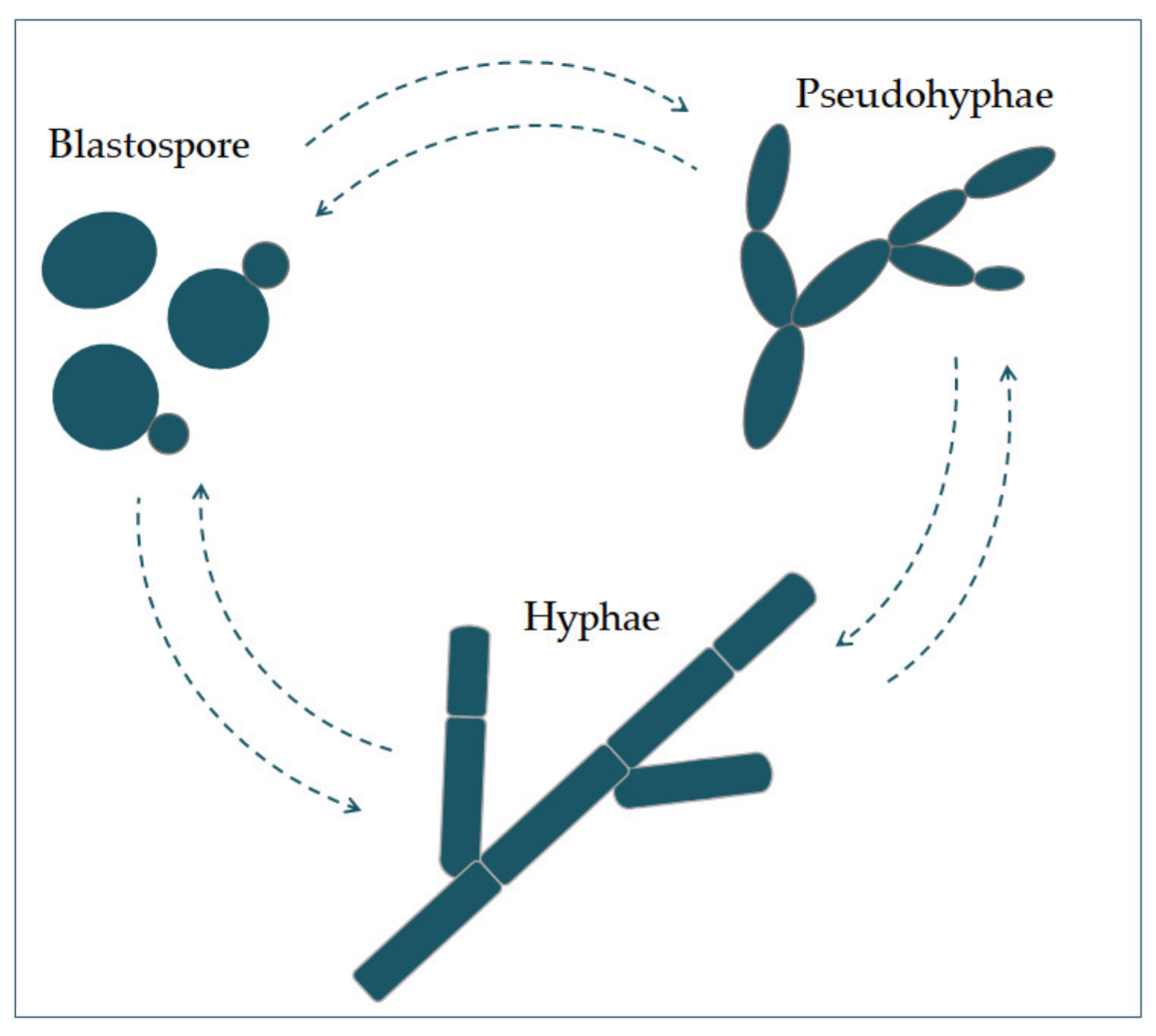
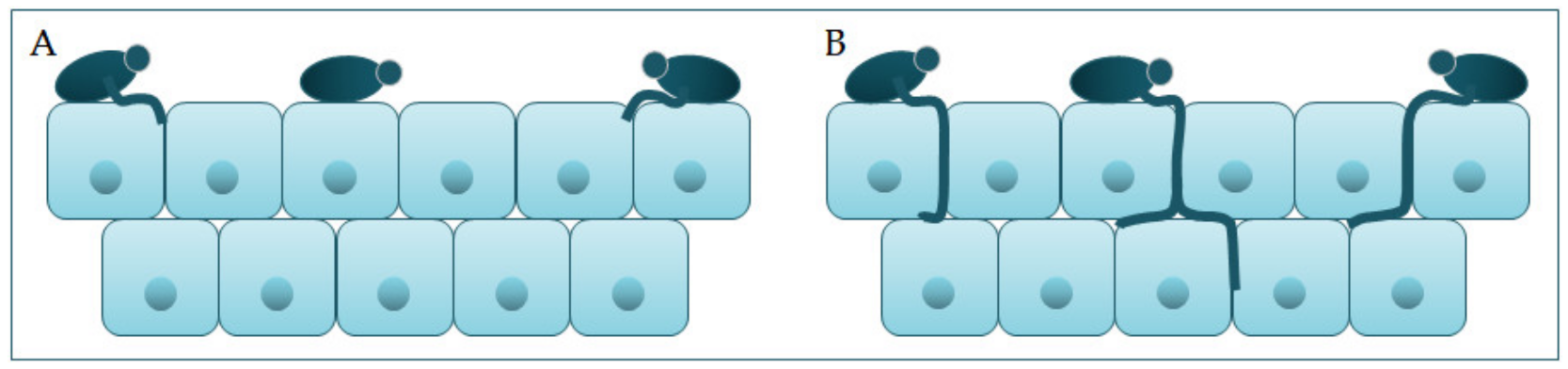
2. Virulence Factors of Candida albicans
3. Clinical Manifestations of Candidiasis
3.1. Candida albicans in the Oral Cavity
3.2. Candida albicans in Gastroenterology
3.3. Candida albicans in Dermatovenerology
3.4. Invasive Candida albicans Infections
4. Conclusions
Authors Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Mukaremera, L.; Lee, K.K.; Mora-Montes, H.M.; Gow, N.A.R. Candida albicans yeast, pseudohyphal, and hyphal morphogenesis differentially affects immune recognition. Front. Immunol. 2017, 8, 1. [Google Scholar] [CrossRef] [PubMed]
- Morad, H.O.J.; Wild, A.-M.; Wiehr, S.; Davies, G.; Maurer, A.; Pichler, B.J.; Thornton, C.R. Pre-clinical Imaging of Invasive Candidiasis Using ImmunoPET/MR. Front. Microbiol. 2018, 9, 1996. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Zhou, X.; Ren, B.; Cheng, L. The regulation of hyphae growth in Candida albicans. Virulence 2020, 11, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Basmaciyan, L.; Bon, F.; Paradis, T.; Lapaquette, P.; Dalle, F. Candida Albicans Interactions with The Host: Crossing The Intestinal Epithelial Barrier. Tissue Barriers 2019, 7, 1612661. [Google Scholar] [CrossRef]
- Walker, G.M.; White, N.A. Introduction to Fungal Physiology. In Fungi: Biology and Applications; Kavanagh, K., Ed.; Wiley-Blackwell: Chichester, UK, 2017; p. 4. ISBN 978-1-119-37432-9. [Google Scholar]
- Molero, G.; Díez-Orejas, R.; Navarro-García, F.; Monteoliva, L.; Pla, J.; Gil, C.; Sánchez-Pérez, M.; Nombela, C. Candida albicans: Genetics, dimorphism and pathogenicity. Int. Microbiol. 1998, 1, 95–106. [Google Scholar]
- Kornitzer, D. Regulation of candida albicans hyphal morphogenesis by endogenous signals. J. Fungi 2019, 5. [Google Scholar] [CrossRef]
- Basso, V.; d’Enfert, C.; Znaidi, S.; Bachellier-Bassi, S. From genes to networks: The regulatory circuitry controlling candida albicans morphogenesis. In Fungal Physiology and Immunopathogenesis: Current Topics in Microbiology and Immunology; Rodrigues, M., Ed.; Springer: Berlin/Heidelberg, Germany, 2019; Volume 422, pp. 61–99. [Google Scholar]
- Garcia-Rubio, R.; de Oliveira, H.C.; Rivera, J.; Trevijano-Contador, N. The Fungal Cell Wall: Candida, Cryptococcus, and Aspergillus Species. Front. Microbiol. 2020, 10, 2993. [Google Scholar] [CrossRef]
- Höfs, S.; Mogavero, S.; Hube, B. Interaction of Candida albicans with host cells: Virulence factors, host defense, escape strategies, and the microbiota. J. Microbiol. 2016, 54, 149–169. [Google Scholar] [CrossRef]
- Reyna-Beltrán, E.; Isaac Bazán Méndez, C.; Iranzo, M.; Mormeneo, S.; Pedro Luna-Arias, J. The Cell Wall of Candida albicans: A Proteomics View. In Candida Albicans; Sandai, D., Ed.; IntechOpen: London, UK, 2019. [Google Scholar]
- Ciurea, C.N.; Kosovski, I.-B.; Mare, A.D.; Toma, F.; Pintea-Simon, I.A.; Man, A. Candida and Candidiasis—Opportunism Versus Pathogenicity: A Review of the Virulence Traits. Microorganisms 2020, 8, 857. [Google Scholar] [CrossRef]
- Hall, R.A. Dressed to impress: Impact of environmental adaptation on the Candida albicans cell wall. Mol. Microbiol. 2015, 97, 7–17. [Google Scholar] [CrossRef]
- Jordá, T.; Puig, S. Regulation of Ergosterol Biosynthesis in Saccharomyces cerevisiae. Genes 2020, 11, 795. [Google Scholar] [CrossRef] [PubMed]
- Cho, I.; Jackson, M.R.; Swift, J. Roles of Cross-Membrane Transport and Signaling in the Maintenance of Cellular Homeostasis. Cell. Mol. Bioeng. 2016, 9, 234–246. [Google Scholar] [CrossRef] [PubMed]
- Viana, R.; Dias, O.; Lagoa, D.; Galocha, M.; Rocha, I.; Teixeira, M.C. Genome-Scale Metabolic Model of the Human Pathogen Candida albicans: A Promising Platform for Drug Target Prediction. J. Fungi 2020, 6, 171. [Google Scholar] [CrossRef] [PubMed]
- Deorukhkar, S.C. Virulence Traits Contributing to Pathogenicity of Candida Species. J. Microbiol. Exp. 2017, 5. [Google Scholar] [CrossRef]
- Noble, S.M.; Gianetti, B.A.; Witchley, J.N. Candida albicans cell-type switching and functional plasticity in the mammalian host. Nat. Rev. Microbiol. 2017, 15, 96–108. [Google Scholar] [CrossRef]
- Hanaoka, M.; Domae, E. IL-1α released from oral epithelial cells upon candidalysin exposure initiates an early innate epithelial response. Int. Immunol. 2020. [Google Scholar] [CrossRef]
- Gale, C.; Gerami-Nejad, M.; McClellan, M.; Vandoninck, S.; Longtine, M.S.; Berman, J. Candida albicans Int1p Interacts with the Septin Ring in Yeast and Hyphal Cells. Mol. Biol. Cell 2001, 12, 3538–3549. [Google Scholar] [CrossRef]
- Sudbery, P.E. Growth of Candida albicans hyphae. Nat. Rev. Microbiol. 2011, 9, 737–748. [Google Scholar] [CrossRef]
- Mayer, F.L.; Wilson, D.; Hube, B. Candida albicans pathogenicity mechanisms. Virulence 2013, 4, 119–128. [Google Scholar] [CrossRef]
- Tsui, C.; Kong, E.F.; Jabra-Rizk, M.A. Pathogenesis of Candida albicans biofilm. Pathog. Dis. 2016, 74, ftw018. [Google Scholar] [CrossRef]
- Maza, P.K.; Bonfim-Melo, A.; Padovan, A.C.B.; Mortara, R.A.; Orikaza, C.M.; Ramos, L.M.D.; Moura, T.R.; Soriani, F.M.; Almeida, R.S.; Suzuki, E.; et al. Candida albicans: The ability to invade epithelial cells and survive under oxidative stress is unlinked to hyphal length. Front. Microbiol. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Galocha, M.; Pais, P.; Cavalheiro, M.; Pereira, D.; Viana, R.; Teixeira, M.C. Divergent approaches to virulence in C. Albicans and C. Glabrata: Two sides of the same coin. Int. J. Mol. Sci. 2019, 20, 2345. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.J.; Chen, Y.L. Conserved and divergent functions of the CAMP/PKA signaling pathway in candida albicans and candida tropicalis. J. Fungi 2018, 4, 68. [Google Scholar] [CrossRef] [PubMed]
- Moyes, D.L.; Wilson, D.; Richardson, J.P.; Mogavero, S.; Tang, S.X.; Wernecke, J.; Höfs, S.; Gratacap, R.L.; Robbins, J.; Runglall, M.; et al. Candidalysin is a fungal peptide toxin critical for mucosal infection. Nature 2016, 532, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Naglik, J.R.; Gaffen, S.L.; Hube, B. Candidalysin: Discovery and function in Candida albicans infections. Curr. Opin. Microbiol. 2019, 52, 100–109. [Google Scholar] [CrossRef]
- Kasper, L.; König, A.; Koenig, P.A.; Gresnigt, M.S.; Westman, J.; Drummond, R.A.; Lionakis, M.S.; Groß, O.; Ruland, J.; Naglik, J.R.; et al. The fungal peptide toxin Candidalysin activates the NLRP3 inflammasome and causes cytolysis in mononuclear phagocytes. Nat. Commun. 2018, 9, 1–20. [Google Scholar] [CrossRef]
- König, A.; Hube, B.; Kasper, L. The Dual Function of the Fungal Toxin Candidalysin during Candida albicans—Macrophage Interaction and Virulence. Toxins 2020, 12, 469. [Google Scholar] [CrossRef]
- Priya, A.; Pandian, S.K. Piperine Impedes Biofilm Formation and Hyphal Morphogenesis of Candida albicans. Front. Microbiol. 2020, 11. [Google Scholar] [CrossRef]
- Talapko, J.; Škrlec, I. The Principles, Mechanisms, and Benefits of Unconventional Agents in the Treatment of Biofilm Infection. Pharmaceuticals 2020, 13, 299. [Google Scholar] [CrossRef]
- McCall, A.D.; Pathirana, R.U.; Prabhakar, A.; Cullen, P.J.; Edgerton, M. Candida albicans biofilm development is governed by cooperative attachment and adhesion maintenance proteins. NPJ Biofilms Microbiomes 2019, 5, 1–12. [Google Scholar] [CrossRef]
- Cavalheiro, M.; Teixeira, M.C. Candida Biofilms: Threats, challenges, and promising strategies. Front. Med. 2018, 5, 28. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Wang, J.J.; Qian, H.; Tan, L.; Zhang, Z.; Liu, H.; Pan, Y.; Zhao, Y. Insights into the Role of Extracellular DNA and Extracellular Proteins in Biofilm Formation of Vibrio parahaemolyticus. Front. Microbiol. 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Karygianni, L.; Ren, Z.; Koo, H.; Thurnheer, T. Biofilm Matrixome: Extracellular Components in Structured Microbial Communities. Trends Microbiol. 2020, 28, 668–681. [Google Scholar] [CrossRef] [PubMed]
- Nett, J.E.; Andes, D.R. Contributions of the biofilm matrix to candida pathogenesis. J. Fungi 2020, 6, 21. [Google Scholar] [CrossRef]
- Paluch, E.; Rewak-Soroczyńska, J.; Jędrusik, I.; Mazurkiewicz, E.; Jermakow, K. Prevention of biofilm formation by quorum quenching. Appl. Microbiol. Biotechnol. 2020, 104, 1871–1881. [Google Scholar] [CrossRef]
- Perry, A.M.; Hernday, A.D.; Nobile, C.J. Unraveling How Candida albicans Forms Sexual Biofilms. J. Fungi 2020, 6, 14. [Google Scholar] [CrossRef]
- Glazier, V.E.; Murante, T.; Murante, D.; Koselny, K.; Liu, Y.; Kim, D.; Koo, H.; Krysan, D.J. Genetic analysis of the Candida albicans biofilm transcription factor network using simple and complex haploinsufficiency. PLoS Genet. 2017, 13, e1006948. [Google Scholar] [CrossRef]
- Rodríguez-Cerdeira, C.; Martínez-Herrera, E.; Carnero-Gregorio, M.; López-Barcenas, A.; Fabbrocini, G.; Fida, M.; El-Samahy, M.; González-Cespón, J.L. Pathogenesis and Clinical Relevance of Candida Biofilms in Vulvovaginal Candidiasis. Front. Microbiol. 2020, 11, 2884. [Google Scholar] [CrossRef]
- Bartnicka, D.; Karkowska-Kuleta, J.; Zawrotniak, M.; Satała, D.; Michalik, K.; Zielinska, G.; Bochenska, O.; Kozik, A.; Ciaston, I.; Koziel, J.; et al. Adhesive protein-mediated cross-talk between Candida albicans and Porphyromonas gingivalis in dual species biofilm protects the anaerobic bacterium in unfavorable oxic environment. Sci. Rep. 2019, 9. [Google Scholar] [CrossRef]
- Ganguly, S.; Mitchell, A.P. Mucosal biofilms of Candida albicans. Curr. Opin. Microbiol. 2011, 14, 380–385. [Google Scholar] [CrossRef]
- Murillo, L.A.; Newport, G.; Lan, C.Y.; Habelitz, S.; Dungan, J.; Agabian, N.M. Genome-wide transcription profiling of the early phase of biofilm formation by Candida albicans. Eukaryot. Cell 2005, 4, 1562–1573. [Google Scholar] [CrossRef] [PubMed]
- Bonhomme, J.; d’Enfert, C. Candida albicans biofilms: Building a heterogeneous, drug-tolerant environment. Curr. Opin. Microbiol. 2013, 16, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Mallick, E.M.; Bergeron, A.C.; Jones, S.K.; Newman, Z.R.; Brothers, K.M.; Creton, R.; Wheeler, R.T.; Bennett, R.J. Phenotypic Plasticity Regulates Candida albicans Interactions and Virulence in the Vertebrate Host. Front. Microbiol. 2016, 7, 780. [Google Scholar] [CrossRef] [PubMed]
- Brimacombe, C.A.; Sierocinski, T.; Dahabieh, M.S. A white-to-opaque-like phenotypic switch in the yeast Torulaspora microellipsoides. Commun. Biol. 2020, 3, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Wibawa, T. The role of virulence factors in Candida albicans pathogenicity. J. Med. Sci. 2016, 48, 58–68. [Google Scholar] [CrossRef]
- Nobile, C.J.; Johnson, A.D. Candida albicans Biofilms and Human Disease. Annu. Rev. Microbiol. 2015, 69, 71–92. [Google Scholar] [CrossRef]
- Naglik, J.R.; Challacombe, S.J.; Hube, B. Candida albicans Secreted Aspartyl Proteinases in Virulence and Pathogenesis. Microbiol. Mol. Biol. Rev. 2003, 67, 400–428. [Google Scholar] [CrossRef]
- Lewis, M.A.O.; Williams, D.W. Diagnosis and management of oral candidosis. Br. Dent. J. 2017, 223, 675–681. [Google Scholar] [CrossRef]
- Peters, B.A.; Wu, J.; Hayes, R.B.; Ahn, J. The oral fungal mycobiome: Characteristics and relation to periodontitis in a pilot study. BMC Microbiol. 2017, 17, 157. [Google Scholar] [CrossRef]
- Sav, H.; Altinbas, R.; Bestepe Dursun, Z. Fungal profile and antifungal susceptibility pattern in patients with oral candidiasis. Infez. Med. 2020, 28, 392–396. [Google Scholar]
- Aslani, N.; Janbabaei, G.; Abastabar, M.; Meis, J.F.; Babaeian, M.; Khodavaisy, S.; Boekhout, T.; Badali, H. Identification of uncommon oral yeasts from cancer patients by MALDI-TOF mass spectrometry. BMC Infect. Dis. 2018, 18, 24. [Google Scholar] [CrossRef] [PubMed]
- Rafiq, N.B. Candidiasis. StatPearls 2020, 1261–1267. [Google Scholar] [CrossRef]
- Zdanavičienė, E.; Sakalauskienė, J.; Gleiznys, A.; Gleiznys, D.; Žilinskas, J. Host responses to Candida albicans. A review. Stomatologija 2017, 19, 109–123. [Google Scholar] [PubMed]
- Baumgardner, D.J. Oral Fungal Microbiota: To Thrush and Beyond. J. Patient-Cent. Res. Rev. 2019, 6, 252–261. [Google Scholar] [CrossRef]
- Serrano, J.; López-Pintor, R.M.; Ramírez, L.; Fernández-Castro, M.; Sanz, M.; Melchor, S.; Peiteado, D.; Hernández, G. Risk factors related to oral candidiasis in patients with primary Sjögren’s syndrome. Med. Oral Patol. Oral Cir. Bucal 2020, 25, e700–e705. [Google Scholar] [CrossRef]
- Suryana, K.; Suharsono, H.; Antara, I.G.P.J. Factors associated with oral candidiasis in people living with HIV/AIDS: A case control study. HIV/AIDS Res. Palliat. Care 2020, 12, 33–39. [Google Scholar] [CrossRef]
- Du, X.; Xiong, H.; Yang, Y.; Yan, J.; Zhu, S.; Chen, F. Dynamic study of oral Candida infection and immune status in HIV infected patients during HAART. Arch. Oral Biol. 2020, 115, 104741. [Google Scholar] [CrossRef]
- Hellstein, J.W.; Marek, C.L. Candidiasis: Red and White Manifestations in the Oral Cavity. Head Neck Pathol. 2019, 13, 25–32. [Google Scholar] [CrossRef]
- Millsop, J.W.; Fazel, N. Oral candidiasis. Clin. Dermatol. 2016, 34, 487–494. [Google Scholar] [CrossRef]
- O’Donnell, L.E.; Millhouse, E.; Sherry, L.; Kean, R.; Malcolm, J.; Nile, C.J.; Ramage, G. Polymicrobial Candida biofilms: Friends and foe in the oral cavity. FEMS Yeast Res. 2015, 15. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M. Current perspectives and the future of candida albicans-associated denture stomatitis treatment. Dent. Med. Probl. 2020, 57, 95–102. [Google Scholar] [CrossRef]
- Kirkpatrick, C.H.; Hill, H.R. Chronic mucocutaneous candidiasis. Pediatr. Infect. Dis. J. 2001, 20, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Sanghvi, R.; Siddik, D.; Hullah, E.; Shah, T.; Carey, B. Chronic mucocutaneous candidiasis: A rare diagnosis in paediatric dentistry. Br. J. Oral Maxillofac. Surg. 2020, 58, 708–710. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Zhang, L.; Xu, Z.; Zhang, J.; Jiang, Y.Y.; Cao, Y.; Yan, T. Innate immune cell response upon Candida albicans infection. Virulence 2016, 7, 512–526. [Google Scholar] [CrossRef] [PubMed]
- Richardson, J.P.; Moyes, D.L. Adaptive immune responses to Candida albicans infection. Virulence 2015, 6, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Kumamoto, C.A. Inflammation and gastrointestinal Candida colonization. Curr. Opin. Microbiol. 2011, 14, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Cassone, A. Vulvovaginal Candida albicans infections: Pathogenesis, immunity and vaccine prospects. BJOG Int. J. Obstet. Gynaecol. 2015, 122, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Kashem, S.W.; Kaplan, D.H. Skin Immunity to Candida albicans. Trends Immunol. 2016, 37, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Ng, W.F.; Von Delwig, A.; Carmichael, A.J.; Arkwright, P.D.; Abinun, M.; Cant, A.J.; Jolles, S.; Lilic, D. Impaired TH17 responses in patients with chronic mucocutaneous candidiasis with and without autoimmune polyendocrinopathy-candidiasis- ectodermal dystrophy. J. Allergy Clin. Immunol. 2010, 126. [Google Scholar] [CrossRef]
- Soltész, B.; Tóth, B.; Sarkadi, A.K.; Erdos, M.; Maródi, L. The evolving view of IL-17-mediated immunity in defense against mucocutaneous candidiasis in humans. Int. Rev. Immunol. 2015, 34, 348–363. [Google Scholar] [CrossRef]
- Bolognia, J.; Schaffer, J.; Cerroni, L. Dermatology, 4th ed.; Elsevier: Amsterdam, The Netherlands, 2018; Volume 2, ISBN 978-0-7020-6275-9. [Google Scholar]
- Chevalier, M.; Ranque, S.; Prêcheur, I. Oral fungal-bacterial biofilm models in vitro: A review. Med. Mycol. 2018, 56, 653–667. [Google Scholar] [CrossRef]
- Salehi, B.; Kregiel, D.; Mahady, G.; Sharifi-Rad, J.; Martins, N.; Rodrigues, C.F. Management of Streptococcus mutans-Candida spp. Oral Biofilms’ Infections: Paving the Way for Effective Clinical Interventions. J. Clin. Med. 2020, 9, 517. [Google Scholar] [CrossRef]
- Pereira, D.F.A.; Seneviratne, C.J.; Koga-Ito, C.Y.; Samaranayake, L.P. Is the oral fungal pathogen Candida albicans a cariogen? Oral Dis. 2018, 24, 518–526. [Google Scholar] [CrossRef]
- Yoo, H.J.; Jwa, S.K. Inhibitory effects of β-caryophyllene on Streptococcus mutans biofilm. Arch. Oral Biol. 2018, 88, 42–46. [Google Scholar] [CrossRef]
- Sampaio, A.A.; Souza, S.E.; Ricomini-Filho, A.P.; Del Bel Cury, A.A.; Cavalcanti, Y.W.; Cury, J.A. Candida albicans Increases Dentine Demineralization Provoked by Streptococcus mutans Biofilm. Caries Res. 2019, 53, 322–331. [Google Scholar] [CrossRef]
- Abrantes, P.M.D.S.; Africa, C.W.J. Measuring Streptococcus mutans, Streptococcus sanguinis and Candida albicans biofilm formation using a real-time impedance-based system. J. Microbiol. Methods 2020, 169. [Google Scholar] [CrossRef]
- Diaz, P.I.; Valm, A.M. Microbial Interactions in Oral Communities Mediate Emergent Biofilm Properties. J. Dent. Res. 2020, 99, 18–25. [Google Scholar] [CrossRef]
- Sztukowska, M.N.; Dutton, L.C.; Delaney, C.; Ramsdale, M.; Ramage, G.; Jenkinson, H.F.; Nobbs, A.H.; Lamont, R.J. Community development between Porphyromonas gingivalis and Candida albicans mediated by inIJ and Als3. MBio 2018, 9. [Google Scholar] [CrossRef]
- Bartnicka, D.; Gonzalez-Gonzalez, M.; Sykut, J.; Koziel, J.; Ciaston, I.; Adamowicz, K.; Bras, G.; Zawrotniak, M.; Karkowska-Kuleta, J.; Satala, D.; et al. Candida albicans shields the periodontal killer porphyromonas gingivalis from recognition by the host immune system and supports the bacterial infection of gingival tissue. Int. J. Mol. Sci. 2020, 21, 1984. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention Candida Infections of the Mouth, Throat, and Esophagus. Available online: https://www.cdc.gov/fungal/diseases/candidiasis/thrush/index.html (accessed on 4 January 2021).
- Faith, J.J.; Guruge, J.L.; Charbonneau, M.; Subramanian, S.; Seedorf, H.; Goodman, A.L.; Clemente, J.C.; Knight, R.; Heath, A.C.; Leibel, R.L.; et al. The long-term stability of the human gut microbiota. Science 2013, 341, 1237439. [Google Scholar] [CrossRef]
- Sekirov, I.; Russell, S.L.; Caetano, M.; Antunes, L.; Finlay, B.B. Gut microbiota in health and disease. Physiol. Rev. 2010, 90, 859–904. [Google Scholar] [CrossRef]
- Jeziorek, M.; Frej-Mądrzak, M.; Choroszy-Król, I. The influence of diet on gastrointestinal Candida spp. colonization and the susceptibility of Candida spp. to antifungal drugs. Rocz. Panstw. Zakl. Hig. 2019, 70, 195–200. [Google Scholar] [CrossRef]
- Mishra, A.A.; Koh, A.Y. Adaptation of Candida albicans During Gastrointestinal Tract Colonization. Curr. Clin. Microbiol. Rep. 2018, 5, 165–172. [Google Scholar] [CrossRef]
- Tong, Y.; Tang, J. Candida albicans infection and intestinal immunity. Microbiol. Res. 2017, 198, 27–35. [Google Scholar] [CrossRef]
- Zhu, W.; Filler, S.G. Interactions of Candida albicans with epithelial cells. Cell. Microbiol. 2010, 12, 273–282. [Google Scholar] [CrossRef]
- Allert, S.; Förster, T.M.; Svensson, C.M.; Richardson, J.P.; Pawlik, T.; Hebecker, B.; Rudolphi, S.; Juraschitz, M.; Schaller, M.; Blagojevic, M.; et al. Candida albicans-induced epithelial damage mediates translocation through intestinal barriers. MBio 2018, 9. [Google Scholar] [CrossRef]
- Robertson, K.D.; Nagra, N.; Mehta, D. Esophageal Candidiasis. StatPearls 2013, 1, 64–65. [Google Scholar] [CrossRef][Green Version]
- Mohamed, A.A.; Lu, X.L.; Mounmin, F.A. Diagnosis and Treatment of Esophageal Candidiasis: Current Updates. Can. J. Gastroenterol. Hepatol. 2019, 2019. [Google Scholar] [CrossRef]
- Rosołowski, M.; Kierzkiewicz, M. Etiology, diagnosis and treatment of infectious esophagitis. Prz. Gastroenterol. 2013, 8, 333–337. [Google Scholar] [CrossRef]
- Alsomali, M.I.; Arnold, M.A.; Frankel, W.L.; Graham, R.P.; Hart, P.A.; Lam-Himlin, D.M.; Naini, B.V.; Voltaggio, L.; Arnold, C.A. Challenges to “classic” esophageal candidiasis: Looks are usually deceiving. Am. J. Clin. Pathol. 2017, 147, 33–42. [Google Scholar] [CrossRef]
- Hoversten, P.; Otaki, F.; Katzka, D.A. Course of Esophageal Candidiasis and Outcomes of Patients at a Single Center. Clin. Gastroenterol. Hepatol. 2019, 17, 200–202.e1. [Google Scholar] [CrossRef]
- Mushi, M.F.; Ngeta, N.; Mirambo, M.M.; Mshana, S.E. Predictors of esophageal candidiasis among patients attending endoscopy unit in a tertiary hospital, Tanzania: A retrospective cross-sectional study. Afr. Health Sci. 2018, 18, 66–71. [Google Scholar] [CrossRef]
- Hoversten, P.; Kamboj, A.K.; Katzka, D.A. Infections of the esophagus: An update on risk factors, diagnosis, and management. Dis. Esophagus 2018, 31. [Google Scholar] [CrossRef]
- Castelo Branco, S.; Ferreira, A.T.; Saraiva, S.; Silva, M.J.; Garcia, T. Fungal Gastroduodenitis. Eur. J. Case Rep. Intern. Med. 2017, 2. [Google Scholar] [CrossRef]
- Stamatiades, G.A.; Ioannou, P.; Petrikkos, G.; Tsioutis, C. Fungal infections in patients with inflammatory bowel disease: A systematic review. Mycoses 2018, 61, 366–376. [Google Scholar] [CrossRef]
- Moyes, D.L.; Richardson, J.P.; Naglik, J.R. Candida albicans-epithelial interactions and pathogenicity mechanisms: Scratching the surface. Virulence 2015, 6, 338–346. [Google Scholar] [CrossRef]
- Naglik, J.R.; König, A.; Hube, B.; Gaffen, S.L. Candida albicans–epithelial interactions and induction of mucosal innate immunity. Curr. Opin. Microbiol. 2017, 40, 104–112. [Google Scholar] [CrossRef]
- Richardson, J.P.; Ho, J.; Naglik, J.R. Candida–epithelial interactions. J. Fungi 2018, 4, 22. [Google Scholar] [CrossRef]
- Gil-Bona, A.; Amador-García, A.; Gil, C.; Monteoliva, L. The external face of Candida albicans: A proteomic view of the cell surface and the extracellular environment. J. Proteom. 2018, 180, 70–79. [Google Scholar] [CrossRef]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2015, 62, e1–e50. [Google Scholar] [CrossRef]
- Metin, A.; Dilek, N.; Bilgili, S.G. Recurrent candidal intertrigo: Challenges and solutions. Clin. Cosmet. Investig. Dermatol. 2018, 11, 175–185. [Google Scholar] [CrossRef]
- Leggit, J.C. Acute and Chronic Paronychia. Am. Fam. Physician 2017, 96, 44–51. [Google Scholar]
- Schlager, E.; Ashack, K.; Khachemoune, A. Erosio interdigitalis blastomycetica: A review of interdigital candidiasis. Dermatol. Online J. 2018, 24, 13030. [Google Scholar]
- Spinillo, A.; Pizzoli, G.; Colonna, L.; Nicola, S.; De Seta, F.; Guaschino, S. Epidemiologic characteristics of women with idiopathic recurrent vulvovaginal candidiasis. Obs. Gynecol. 1993, 5, 721–727. [Google Scholar] [CrossRef]
- Swamiappan, M. Anogenital pruritus—An overview. J. Clin. Diagn. Res. 2016, 10, WE01–WE03. [Google Scholar] [CrossRef]
- Visscher, M.O.; Adam, R.; Brink, S.; Odio, M. Newborn infant skin: Physiology, development, and care. Clin. Dermatol. 2015, 33, 271–280. [Google Scholar] [CrossRef]
- Darmstadt, G.L.; Dinulos, J.G.; Miller, Z. Congenital cutaneous candidiasis: Clinical presentation, pathogenesis, and management guidelines. Pediatrics 2000, 105, 438–444. [Google Scholar] [CrossRef]
- Greenberg, R.G.; Benjamin, D.K. Neonatal candidiasis: Diagnosis, prevention, and treatment. J. Infect. 2014, 69, S19–S22. [Google Scholar] [CrossRef]
- Grimbacher, B.; Holland, S.M.; Gallin, J.I.; Greenberg, F.; Hill, S.C.; Malech, H.L.; Miller, J.A.; O’Connell, A.C.; Dent, B.; Puck, J.M. Hyper-IgE syndrome with recurrent infections—An autosomal dominant multisystem disorder. N. Engl. J. Med. 1999, 340, 692–702. [Google Scholar] [CrossRef]
- Mogensen, T.H. Primary Immunodeficiencies with Elevated IgE. Int. Rev. Immunol. 2016, 35, 39–56. [Google Scholar] [CrossRef]
- Milner, J.D.; Brenchley, J.M.; Laurence, A.; Freeman, A.F.; Hill, B.J.; Elias, K.M.; Kanno, Y.; Spalding, C.; Elloumi, H.Z.; Paulson, M.L.; et al. Impaired TH17 cell differentiation in subjects with autosomal dominant hyper-IgE syndrome. Nature 2008, 452, 773–776. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; Tsai, I.C.; Lin, C.; Hsieh, W.P.; Lan, C.Y.; Chuang, Y.J.; Chen, B. Sen Essential functional modules for pathogenic and defensive mechanisms in candida albicans infections. Biomed. Res. Int. 2014, 2014, 136130–136130. [Google Scholar] [CrossRef] [PubMed]
- de Leon, E.M.; Jacober, S.J.; Sobel, J.D.; Foxman, B. Prevalence and risk factors for vaginal Candida colonization in women with type 1 and type 2 diabetes. BMC Infect. Dis. 2002, 2, 1. [Google Scholar] [CrossRef] [PubMed]
- Dorko, E.; Baranová, Z.; Jenča, A.; Kizek, P.; Pilipčinec, E.; Tkáčiková, L. Diabetes mellitus and candidiases. Folia Microbiol. 2005, 50, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Dicle, O.; Parmaksizoglu, B.; Gurkan, A.; Tuncer, M.; Demirbas, A.; Yilmaz, E. Skin infections in 401 renal transplant recipients in southern Turkey—PubMed. Exp. Clin. Transpl. 2009, 7, 133–136. [Google Scholar]
- Bassetti, M.; Righi, E.; Costa, A.; Fasce, R.; Molinari, M.P.; Rosso, R.; Pallavicini, F.B.; Viscoli, C. Epidemiological trends in nosocomial candidemia in intensive care. BMC Infect. Dis. 2006, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Schwartz, K.; Bartoces, M.; Monsur, J.; Severson, R.K.; Sobel, J.D. Effect of antibiotics on vulvovaginal candidiasis: A metronet study. J. Am. Board Fam. Med. 2008, 21, 261–268. [Google Scholar] [CrossRef]
- Seelig, M.S. The role of antibiotics in the pathogenesis of Candida infections. Am. J. Med. 1966, 40, 887–917. [Google Scholar] [CrossRef]
- Baker, K.F.; Isaacs, J.D. Novel therapies for immune-mediated inflammatory diseases: What can we learn from their use in rheumatoid arthritis, spondyloarthritis, systemic lupus erythematosus, psoriasis, Crohn’s disease and ulcerative colitis? Ann. Rheum. Dis. 2018, 77, 175–187. [Google Scholar] [CrossRef]
- Kuwabara, T.; Ishikawa, F.; Kondo, M.; Kakiuchi, T. The Role of IL-17 and Related Cytokines in Inflammatory Autoimmune Diseases. Mediat. Inflamm. 2017, 2017. [Google Scholar] [CrossRef]
- Beringer, A.; Noack, M.; Miossec, P. IL-17 in Chronic Inflammation: From Discovery to Targeting. Trends Mol. Med. 2016, 22, 230–241. [Google Scholar] [CrossRef] [PubMed]
- Conti, H.R.; Gaffen, S.L. IL-17–Mediated Immunity to the Opportunistic Fungal Pathogen Candida albicans. J. Immunol. 2015, 195, 780–788. [Google Scholar] [CrossRef] [PubMed]
- Lesher, J. Oral therapy of common superficial fungal infections of the skin. J. Am. Acad. Dermatol. 1999, 40, S31–S34. [Google Scholar] [CrossRef]
- Costa, C.; Dias, P.J.; Sá-Correia, I.; Teixeira, M.C. MFS multidrug transporters in pathogenic fungi: Do they have real clinical impact? Front. Physiol. 2014, 5, 197. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Sae-Tia, S.; Fries, B.C. Candidiasis and mechanisms of antifungal resistance. Antibiotics 2020, 9, 312. [Google Scholar] [CrossRef]
- Choukri, F.; Benderdouche, M.; Sednaoui, P. In vitro susceptibility profile of 200 recent clinical isolates of Candida spp. to topical antifungal treatments of vulvovaginal candidiasis, the imidazoles and nystatin agents. J. Mycol. Med. 2014, 24, 303–307. [Google Scholar] [CrossRef]
- Sonthalia, S.; Agrawal, M.; Sehgal, V. Topical ciclopirox olamine 1%: Revisiting a unique antifungal. Indian Dermatol. Online J. 2019, 10, 481. [Google Scholar] [CrossRef]
- Abrams, B.; Hanel, H.; Hoehler, T. Ciclopirox olamine: A hydroxypyridine antifungal agent. Clin. Dermatol. 1991, 9, 471–477. [Google Scholar] [CrossRef]
- Jandourek, A.; Brown, P.; Vazquez, J.A. Community-acquired fungemia due to a multiple-azole-resistant strain of Candida tropicalis. Clin. Infect. Dis. 1999, 29, 1583–1584. [Google Scholar] [CrossRef]
- Vazquez, J.A.; Sobel, J.D. Anidulafungin: A novel echinocandin. Clin. Infect. Dis. 2006, 43, 215–222. [Google Scholar] [CrossRef]
- European Medicines Agency. Suspension of Marketing Authorisations for Oral Ketoconazole Benefit of Oral Ketoconazole Does Not Outweigh Risk of Liver Injury in Fungal Infections on 25 July 2013, the European Medicines Agency’s Committee on Medicinal Products for Human Use; European Medicines Agency: London, UK, 2013. [Google Scholar]
- Gupta, A. Systemic antifungal agents. In Comprehensive Dermatologic Drug Therapy; Wolverton, S., Ed.; Saunder: Philadelphia, PA, USA, 2007; pp. 101–112. [Google Scholar]
- Talapko, J.; Matijević, T.; Juzbašić, M.; Antolović-Požgain, A.; Škrlec, I. Antibacterial Activity of Silver and Its Application in Dentistry, Cardiology and Dermatology. Microorganisms 2020, 8, 1400. [Google Scholar] [CrossRef] [PubMed]
- Hassan, A.; Mansour, K.; Mahmoud, H. Biosynthesis of silver nanoparticles(Ag-Nps) (a model of metals) by Candida albicans and its antifungal activity on Some fungal pathogens (Trichophyton mentagrophytes and Candida albicans). N. Y. Sci. J. 2013, 6, 27–34. [Google Scholar]
- Choi, J.S.; Lee, J.W.; Shin, U.C.; Lee, M.W.; Kim, D.J.; Kim, S.W. Inhibitory activity of silver nanoparticles synthesized using lycopersicon esculentum against biofilm formation in candida species. Nanomaterials 2019, 9, 1512. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G.; Lionakis, M.S.; Arendrup, M.C.; Ostrosky-Zeichner, L.; Kullberg, B.J. Invasive candidiasis. Nat. Rev. Dis. Prim. 2018, 4, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Jabra-Rizk, M.A.; Kong, E.F.; Tsui, C.; Nguyen, M.H.; Clancy, C.J.; Fidel, P.L.; Noverr, M. Candida albicans pathogenesis: Fitting within the host-microbe damage response framework. Infect. Immun. 2016, 84, 2724–2739. [Google Scholar] [CrossRef] [PubMed]
- Rosati, D.; Bruno, M.; Jaeger, M.; Ten Oever, J.; Netea, M.G. Recurrent Vulvovaginal Candidiasis: An Immunological Perspective. Microorganisms 2020, 8, 144. [Google Scholar] [CrossRef]
- Gonzalez-Lara, M.F.; Ostrosky-Zeichner, L. Invasive Candidiasis. Semin. Respir. Crit. Care Med. 2020, 41, 3–12. [Google Scholar] [CrossRef]
- Yapar, N. Epidemiology and risk factors for invasive candidiasis. Ther. Clin. Risk Manag. 2014, 10, 95–105. [Google Scholar] [CrossRef]
- Kauffman, C.A.; Vazquez, J.A.; Sobel, J.D.; Gallis, H.A.; McKinsey, D.S.; Karchmer, A.W.; Sugar, A.M.; Sharkey, P.K.; Wise, G.J.; Mangi, R.; et al. Prospective multicenter surveillance study of funguria in hospitalized patients. Clin. Infect. Dis. 2000, 30, 14–18. [Google Scholar] [CrossRef]
- Ang, B.S.P.; Telenti, A.; King, B.; Steckelberg, J.M.; Wilson, W.R. Candidemia from a urinary tract source: Microbiological aspects and clinical significance. Clin. Infect. Dis. 1993, 17, 662–666. [Google Scholar] [CrossRef]
- Haron, E.; Vartivarian, S.; Anaissie, E.; Dekmezian, R.; Bodey, G. Primary Candida pneumonia. Experience at a large cancer center and review of the literature. Medicine 1993, 72, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Kontoyiannis, D.P.; Reddy, B.T.; Torres, H.A.; Luna, M.; Lewis, R.E.; Tarrand, J.; Bodey, G.P.; Raad, I.I. Pulmonary candidiasis in patients with cancer: An autopsy study. Clin. Infect. Dis. 2002, 34, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Barton, M.; Shen, A.; O’Brien, K.; Robinson, J.L.; Davies, H.D.; Simpson, K.; Asztalos, E.; Langley, J.; Le Saux, N.; Sauve, R.; et al. Early-onset invasive candidiasis in extremely low birth weight infants: Perinatal acquisition predicts poor outcome. Clin. Infect. Dis. 2017, 64, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, R.M.; Linssen, C.F.; Guion, N.; Van Mook, W.N.; Bergmans, D.C. Candida pneumonia in intensive care unit? Open Forum Infect. Dis. 2014, 1. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.D.; Perfect, J.R. Fungal infections of the bones and joints. Curr. Infect. Dis. Rep. 2001, 3, 450–460. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.J.; Mejicano, G.C. Vertebral osteomyelitis due to Candida species: Case report and literature review. Clin. Infect. Dis. 2001, 33, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Gamaletsou, M.N.; Kontoyiannis, D.P.; Sipsas, N.V.; Moriyama, B.; Alexander, E.; Roilides, E.; Brause, B.; Walsh, T.J. Candida osteomyelitis: Analysis of 207 pediatric and adult cases (1970-2011). Clin. Infect. Dis. 2012, 55, 1338–1351. [Google Scholar] [CrossRef]
- Shoham, S.; Nucci, M.; Walsh, T.J. Mucocutaneous and Deeply Invasive Candidiasis. In Tropical Infectious Diseases; Guerrant, R.L., Walker, D.H., Weller, P.F., Eds.; Elsevier Inc.: Boston, MA, USA, 2011; pp. 589–596. ISBN 9780702039355. [Google Scholar]
- Weitkamp, J.H.; Nania, J.J. Infectious Diseases. In Neonatal Neurology; Fenichel, G.M., Ed.; Elsevier Inc.: Boston, MA, USA, 2007; pp. 109–141. ISBN 9780443067242. [Google Scholar]
- Mamtani, S.S.; Aljanabi, N.M.; Gupta Rauniyar, R.P.; Acharya, A.; Malik, B.H. Candida Endocarditis: A Review of the Pathogenesis, Morphology, Risk Factors, and Management of an Emerging and Serious Condition. Cureus 2020, 12. [Google Scholar] [CrossRef]
- Baddley, J.W.; Benjamin, D.K.; Patel, M.; Miró, J.; Athan, E.; Barsic, B.; Bouza, E.; Clara, L.; Elliott, T.; Kanafani, Z.; et al. Candida infective endocarditis. Eur. J. Clin. Microbiol. Infect. Dis. 2008, 27, 519–529. [Google Scholar] [CrossRef]
- Author, C.; Shokohi, T.; Reza Aghili, S.; Ali Boroumand, M.; Hashemi Fesharaki, S.; Salmanian, B. Intravenous Catheter-Associated Candidemia due to Candida membranaefaciens: The First Iranian Case. J. Tehran Univ. Heart Center 2015, 10, 101–105. [Google Scholar]
- Logan, C.; Martin-Loeches, I.; Bicanic, T. Invasive candidiasis in critical care: Challenges and future directions. Intensive Care Med. 2020, 46, 2001–2014. [Google Scholar] [CrossRef] [PubMed]
- Calandra, T.; Roberts, J.A.; Antonelli, M.; Bassetti, M.; Vincent, J.L. Diagnosis and management of invasive candidiasis in the ICU: An updated approach to an old enemy. Crit. Care 2016, 20, 125. [Google Scholar] [CrossRef] [PubMed]
- Beardsley, J.; Halliday, C.L.; Chen, S.C.A.; Sorrell, T.C. Responding to the emergence of antifungal drug resistance: Perspectives from the bench and the bedside. Future Microbiol. 2018, 13, 1175–1191. [Google Scholar] [CrossRef] [PubMed]
- Wiederhold, N.P. Antifungal resistance: Current trends and future strategies to combat. Infect. Drug Resist. 2017, 10, 249–259. [Google Scholar] [CrossRef] [PubMed]
- Costa-de-Oliveira, S.; Rodrigues, A.G. Candida albicans Antifungal Resistance and Tolerance in Bloodstream Infections: The Triad Yeast-Host-Antifungal. Microorganisms 2020, 8, 154. [Google Scholar] [CrossRef] [PubMed]
- Siddharthan, T.; Karakousis, P.C.; Checkley, W. Empirical antifungal therapy in critically ill patients with sepsis. JAMA J. Am. Med. Assoc. 2016, 316, 1549–1550. [Google Scholar] [CrossRef] [PubMed]
- Eschenauer, G.A.; Kwak, E.J.; Humar, A.; Potoski, B.A.; Clarke, L.G.; Shields, R.K.; Abdel-Massih, R.; Silveira, F.P.; Vergidis, P.; Clancy, C.J.; et al. Targeted Versus Universal Antifungal Prophylaxis Among Liver Transplant Recipients. Am. J. Transplant. 2015, 15, 180–189. [Google Scholar] [CrossRef]
- Hsu, J.F.; Lai, M.Y.; Lee, C.W.; Chu, S.M.; Wu, I.H.; Huang, H.R.; Lee, I.T.; Chiang, M.C.; Fu, R.H.; Tsai, M.H. Comparison of the incidence, clinical features and outcomes of invasive candidiasis in children and neonates. BMC Infect. Dis. 2018, 18, 194. [Google Scholar] [CrossRef]
- Badiee, P. Evaluation of human body fluids for the diagnosis of fungal infections. Biomed. Res. Int. 2013, 2013. [Google Scholar] [CrossRef]
- Cobo, F.; Rodríguez-Granger, J.; Sampedro, A.; Aliaga-Martínez, L.; Navarro-Marí, J.M. Candida Prosthetic Joint Infection. A Review of Treatment Methods. J. Bone Jt. Infect. 2017, 2, 114–121. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Castanheira, M. Nosocomial candidiasis: Antifungal stewardship and the importance of rapid diagnosis. Med. Mycol. 2016, 54, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Tissot, F.; Agrawal, S.; Pagano, L.; Petrikkos, G.; Groll, A.H.; Skiada, A.; Lass-Flörl, C.; Calandra, T.; Viscoli, C.; Herbrecht, R. ECIL-6 guidelines for the treatment of invasive candidiasis, aspergillosis and mucormycosis in leukemia and hematopoietic stem cell transplant patients. Haematologica 2017, 102, 433–444. [Google Scholar] [CrossRef]
- Bow, E.J.; Evans, G.; Fuller, J.; Laverdière, M.; Rotstein, C.; Rennie, R.; Shafran, S.D.; Sheppard, D.; Carle, S.; Phillips, P.; et al. Canadian clinical practice guidelines for invasive candidiasis in adults. Can. J. Infect. Dis. Med. Microbiol. 2010, 21. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; McGuire, T.M.; Hollingworth, S.A.; Dong, Y.; Van Driel, M.L. Antifungal agents for invasive candidiasis in non-neutropenic critically ill adults: What do the guidelines recommend? Int. J. Infect. Dis. 2019, 89, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Patterson, T.F.; Thompson, G.R.; Denning, D.W.; Fishman, J.A.; Hadley, S.; Herbrecht, R.; Kontoyiannis, D.P.; Marr, K.A.; Morrison, V.A.; Nguyen, M.H.; et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the infectious diseases society of America. Clin. Infect. Dis. 2016, 63, e1–e60. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.D.; Perfect, J.R. Use of antifungal combination therapy: Agents, order, and timing. Curr. Fungal Infect. Rep. 2010, 4, 87–95. [Google Scholar] [CrossRef]

| Bone | Brain | Eye | Heart | Kidney | Liver and Spleen | Lung |
|---|---|---|---|---|---|---|
| Osteomyelitis | Brain abscess | Choroiditis | Endocarditis | Candiduria | Chronic disseminated candidiasis | Focal abscess |
| Spondylodiscitis | Meningo-encephalitis | Retinitis | Pyelonephritis | Focal abscess | ||
| Endophthalmitis | Pyonephrosis | |||||
| Renal abscess |
| Candida albicans | ||
|---|---|---|
| Preferred Initial Therapy | Alternative Initial Therapy | Preferred Step-Down Therapy |
| Echinocandin | Fluconazole | Fluconazole |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Talapko, J.; Juzbašić, M.; Matijević, T.; Pustijanac, E.; Bekić, S.; Kotris, I.; Škrlec, I. Candida albicans—The Virulence Factors and Clinical Manifestations of Infection. J. Fungi 2021, 7, 79. https://doi.org/10.3390/jof7020079
Talapko J, Juzbašić M, Matijević T, Pustijanac E, Bekić S, Kotris I, Škrlec I. Candida albicans—The Virulence Factors and Clinical Manifestations of Infection. Journal of Fungi. 2021; 7(2):79. https://doi.org/10.3390/jof7020079
Chicago/Turabian StyleTalapko, Jasminka, Martina Juzbašić, Tatjana Matijević, Emina Pustijanac, Sanja Bekić, Ivan Kotris, and Ivana Škrlec. 2021. "Candida albicans—The Virulence Factors and Clinical Manifestations of Infection" Journal of Fungi 7, no. 2: 79. https://doi.org/10.3390/jof7020079
APA StyleTalapko, J., Juzbašić, M., Matijević, T., Pustijanac, E., Bekić, S., Kotris, I., & Škrlec, I. (2021). Candida albicans—The Virulence Factors and Clinical Manifestations of Infection. Journal of Fungi, 7(2), 79. https://doi.org/10.3390/jof7020079







