The Effects of COVID-19 on Antifungal Prescribing in the UK—Lessons to Learn
Abstract
1. Introduction
2. Materials and Methods
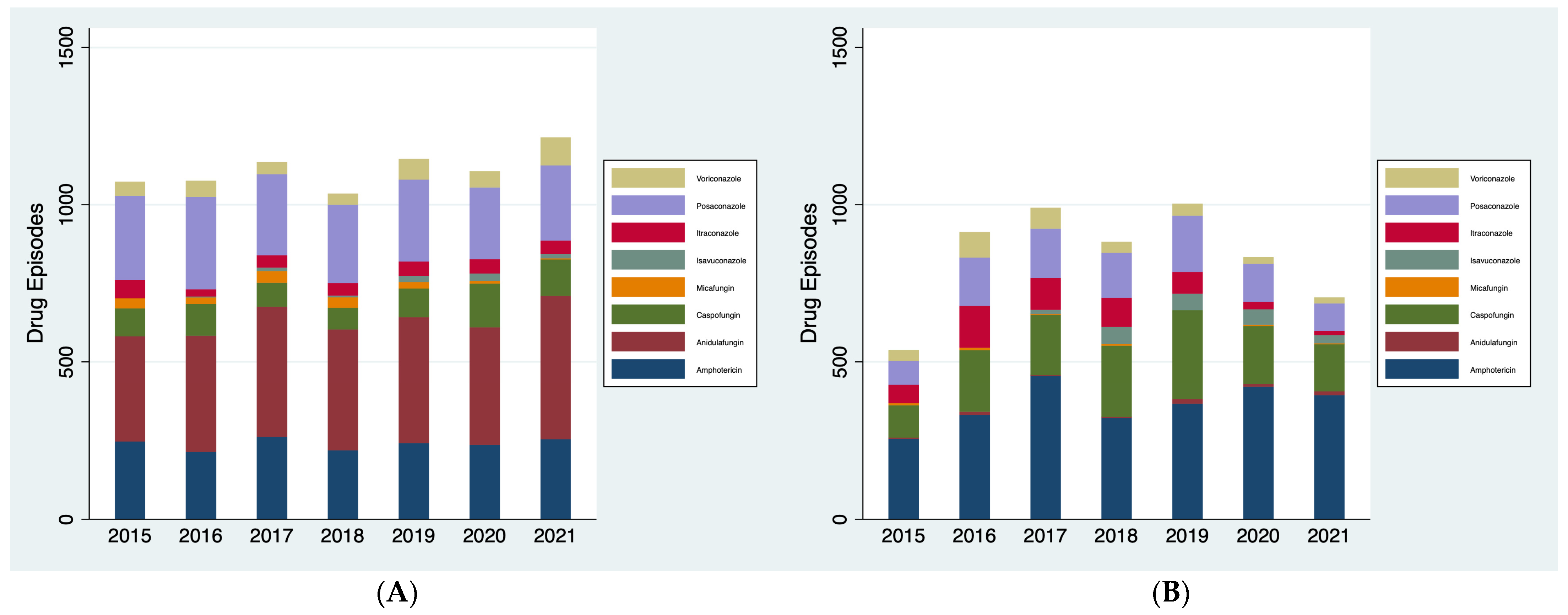
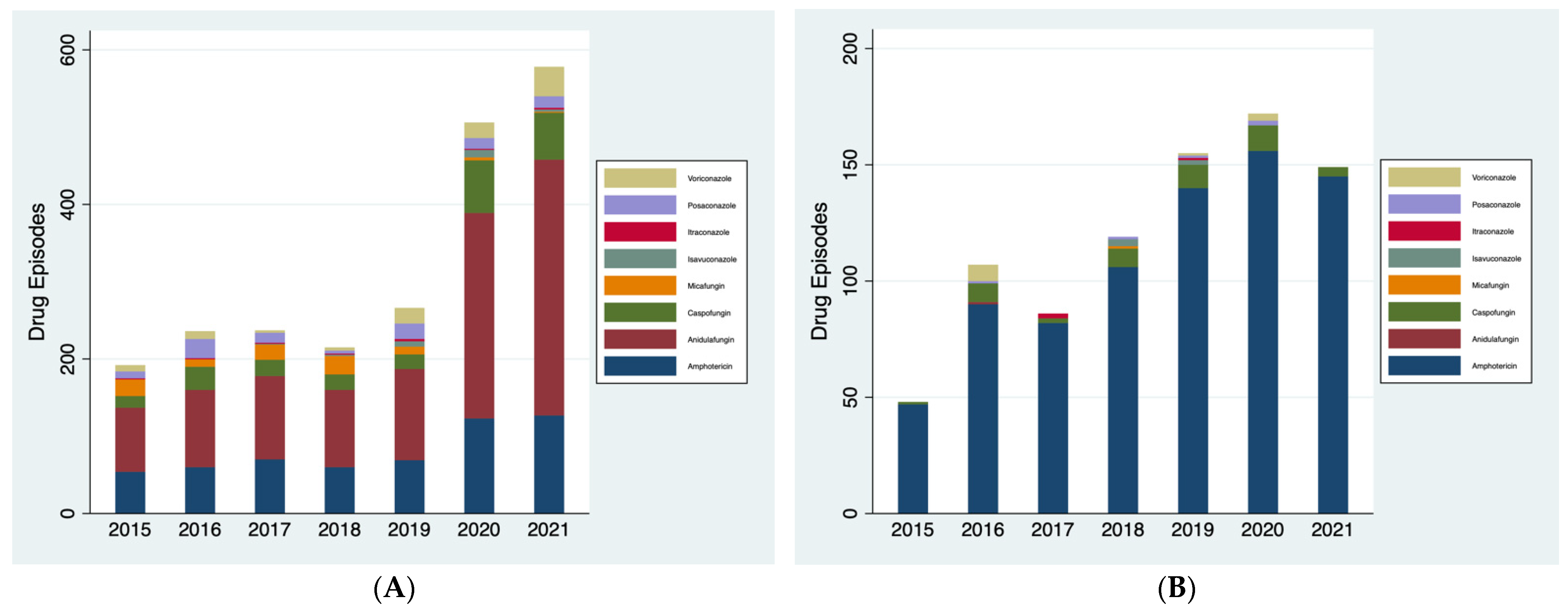
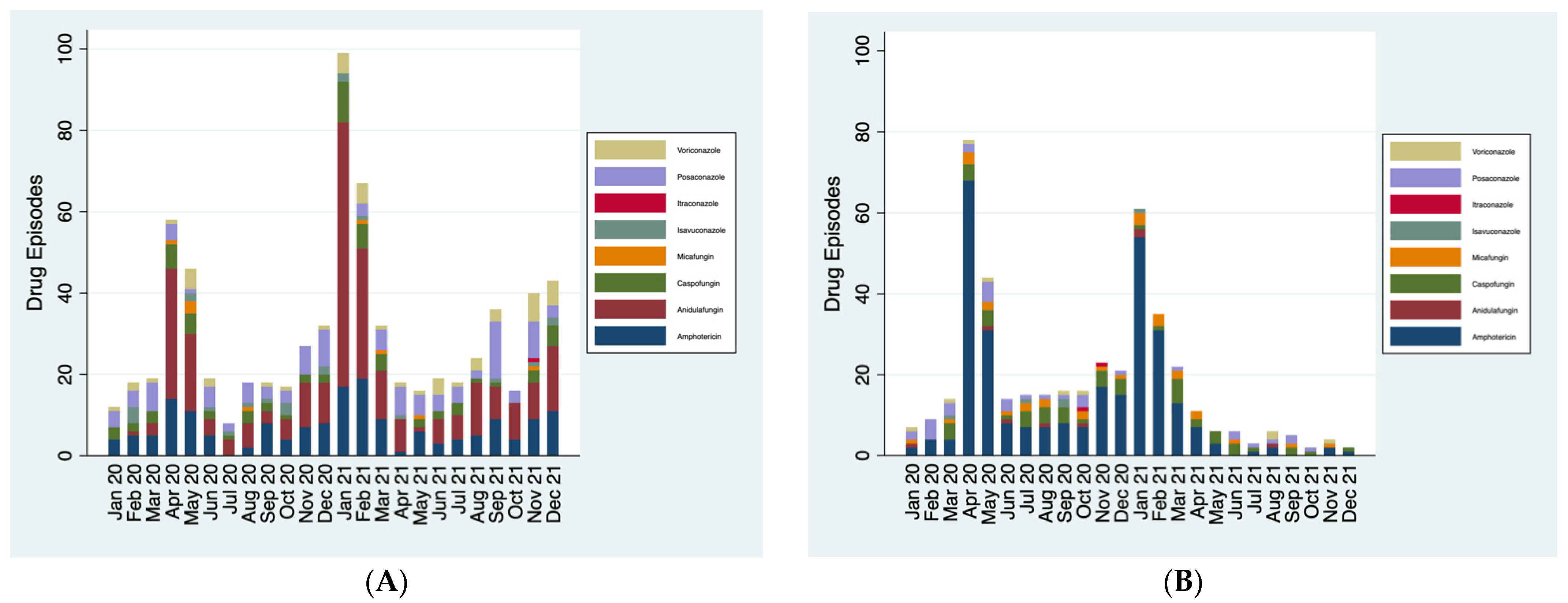
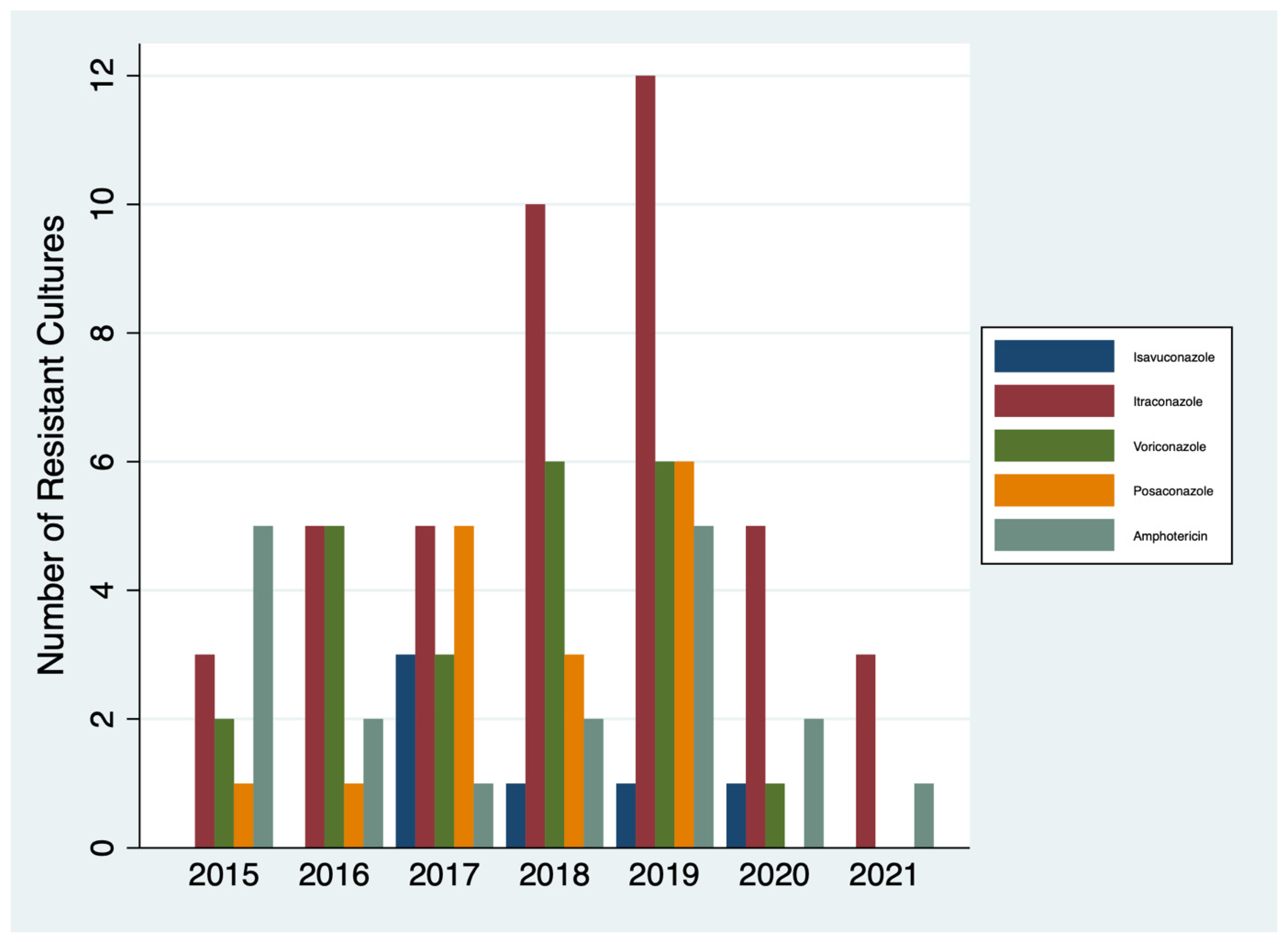
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brown, G.D.; Denning, D.W.; Gow, N.A.; Levitz, S.M.; Netea, M.G.; White, T.C. Hidden Killers: Human Fungal Infections. Sci. Transl. Med. 2012, 4, 165rv13. [Google Scholar] [CrossRef] [PubMed]
- Bongomin, F.; Gago, S.; Oladele, R.O.; Denning, D.W. Global and Multi-National Prevalence of Fungal Diseases-Estimate Precision. J. Fungi 2017, 3, 57. [Google Scholar] [CrossRef] [PubMed]
- Pegorie, M.; Denning, D.W.; Welfare, W. Estimating the burden of invasive and serious fungal disease in the United Kingdom. J. Infect. 2017, 74, 60–71. [Google Scholar] [CrossRef] [PubMed]
- Webb, B.J.; Ferraro, J.P.; Rea, S.; Kaufusi, S.; E Goodman, B.; Spalding, J. Epidemiology and Clinical Features of Invasive Fungal Infection in a US Health Care Network. Open Forum Infect. Dis. 2018, 5, ofy187. [Google Scholar] [CrossRef] [PubMed]
- Perlin, D.S.; Rautemaa-Richardson, R.; Alastruey-Izquierdo, A. The global problem of antifungal resistance: Prevalence, mechanisms, and management. Lancet Infect. Dis. 2017, 17, e383–e392. [Google Scholar] [CrossRef]
- Fisher, M.C.; Alastruey-Izquierdo, A.; Berman, J.; Bicanic, T.; Bignell, E.M.; Bowyer, P.; Bromley, M.; Brüggemann, R.; Garber, G.; Cornely, O.A.; et al. Tackling the emerging threat of antifungal resistance to human health. Nat. Rev. Microbiol. 2022, 20, 557–571. [Google Scholar] [CrossRef]
- Risum, M.; Hare, R.K.; Gertsen, J.B.; Kristensen, L.; Rosenvinge, F.S.; Sulim, S.; Abou-Chakra, N.; Bangsborg, J.; Røder, B.L.; Marmolin, E.S.; et al. Azole resistance in Aspergillus fumigatus. The first 2-year’s Data from the Danish National Surveillance Study, 2018–2020. Mycoses 2022, 65, 419–428. [Google Scholar] [CrossRef]
- WHO. WHO Factsheet on Antimicrobial Resistance. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 3 December 2023).
- English Surveillance Programme for Antimicrobial Utilisation and Resistance 2020–2021. Available online: https://www.gov.uk/government/publications/english-surveillance-programme-antimicrobial-utilisation-and-resistance-espaur-report (accessed on 4 December 2023).
- English Surveillance Programme for Antimicrobial Utilisation and Resistance 2021–2022. Available online: https://www.gov.uk/government/publications/english-surveillance-programme-antimicrobial-utilisation-and-resistance-espaur-report (accessed on 4 December 2023).
- Jackson, R.; Kartoglu, I.; Stringer, C.; Gorrell, G.; Roberts, A.; Song, X.; Wu, H.; Agrawal, A.; Lui, K.; Groza, T.; et al. CogStack—Experiences of deploying integrated information retrieval and extraction services in a large National Health Service Foundation Trust hospital. BMC Med. Inform. Decis. Mak. 2018, 18, 47. [Google Scholar] [CrossRef]
- Koehler, P.; Bassetti, M.; Chakrabarti, A.; Chen, S.C.A.; Colombo, A.L.; Hoenigl, M.; Klimko, N.; Lass-Flörl, C.; Oladele, R.O.; Vinh, D.C.; et al. Defining and managing COVID-19-associated pulmonary aspergillosis: The 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect. Dis. 2021, 21, e149–e162. [Google Scholar] [CrossRef]
- Guinea, J.; Verweij, P.; Meletiadis, J.; Mouton, J.; Barchiesi, F.; Arendrup, M.; Arikan-Akdagli, S.; Castanheira, M.; Chryssanthou, E.; Friberg, N.; et al. How to: EUCAST recommendations on the screening procedure E.Def 10.1 for the detection of azole resistance in Aspergillus fumigatus isolates using four-well azole-containing agar plates. Clin. Microbiol. Infect. 2019, 25, 681–687. [Google Scholar] [CrossRef]
- Ullmann, A.J.; Aguado, J.M.; Arikan-Akdagli, S.; Denning, D.W.; Groll, A.H.; Lagrou, K.; Lass-Flörl, C.; Lewis, R.E.; Munoz, P.; Verweij, P.E.; et al. Diagnosis and management of Aspergillus diseases: Executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin. Microbiol. Infect. 2018, 24 (Suppl. S1), e1–e38. [Google Scholar] [CrossRef] [PubMed]
- Schelenz, S.; Hagen, F.; Rhodes, J.L.; Abdolrasouli, A.; Chowdhary, A.; Hall, A.; Ryan, L.; Shackleton, J.; Trimlett, R.; Meis, J.F.; et al. First hospital outbreak of the globally emerging Candida auris in a European hospital. Antimicrob. Resist. Infect. Control 2016, 5, 35. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 62, e1–e50. [Google Scholar] [CrossRef] [PubMed]
- Cornely, O.A.; Bassetti, M.; Calandra, T.; Garbino, J.; Kullberg, B.J.; Lortholary, O.; Meersseman, W.; Akova, M.; Arendrup, M.C.; Arikan-Akdagli, S.; et al. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: Non-neutropenic adult patients. Clin. Microbiol. Infect. 2012, 18 (Suppl. S7), 19–37. [Google Scholar] [CrossRef] [PubMed]
- Patterson, T.F.; Thompson, G.R., III; Denning, D.W.; Fishman, J.A.; Hadley, S.; Herbrecht, R.; Kontoyiannis, D.P.; Marr, K.A.; Morrison, V.A.; Nguyen, M.H.; et al. Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 63, e1–e60. [Google Scholar] [CrossRef]
- Ye, Q.; Yu, X.; Chen, W.; Li, M.; Gu, S.; Huang, L.; Zhan, Q.; Wang, C. Impact of extracorporeal membrane oxygenation on voriconazole plasma concentrations: A retrospective study. Front. Pharmacol. 2022, 13, 972585. [Google Scholar] [CrossRef]
- Ibrahim, S.M.; Adlan, N.; Alomair, S.M.; Butaiban, I.; Alsalman, A.; Bawazeer, A.; Alqahtani, M.; Mohamed, D.; Emeka, P.M. Evaluation of Systemic Antifungal Prescribing Knowledge and Practice in the Critical Care Setting among ICU Physicians and Clinical Pharmacists: A Cross-Sectional Study. Antibiotics 2023, 12, 238. [Google Scholar] [CrossRef]
- Nivoix, Y.; Launoy, A.; Lutun, P.; Moulin, J.-C.; Phai Pang, K.-A.; Fornecker, L.-M.; Wolf, M.; Levêque, D.; Letscher-Bru, V.; Beretz, L.; et al. Adherence to recommendations for the use of antifungal agents in a tertiary care hospital. J. Antimicrob. Chemother. 2012, 67, 2506–2513. [Google Scholar] [CrossRef]
- Valerio, M.; Rodriguez-Gonzalez, C.G.; Muñoz, P.; Caliz, B.; Sanjurjo, M.; Bouza, E.; on behalf of the COMIC Study Group. Evaluation of antifungal use in a tertiary care institution: Antifungal stewardship urgently needed. J. Antimicrob. Chemother. 2014, 69, 1993–1999. [Google Scholar] [CrossRef]
- Zilberberg, M.D.; Kollef, M.H.; Arnold, H.; Labelle, A.; Micek, S.T.; Kothari, S.; Shorr, A.F. Inappropriate empiric antifungal therapy for candidemia in the ICU and hospital resource utilization: A retrospective cohort study. BMC Infect. Dis. 2010, 10, 150. [Google Scholar] [CrossRef]
- Valerio, M.; Vena, A.; Bouza, E.; Reiter, N.; Viale, P.; Hochreiter, M.; Giannella, M.; Muñoz, P.; on behalf the COMIC study group (Collaborative group on Mycosis). How much European prescribing physicians know about invasive fungal infections management? BMC Infect. Dis. 2015, 15, 80. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. COVID-19 Rapid Guideline: Managing COVID-19. 2021. Available online: https://www.nice.org.uk/guidance/ng191 (accessed on 4 December 2023).
- Charani, E.; Edwards, R.; Sevdalis, N.; Alexandrou, B.; Sibley, E.; Mullett, D.; Franklin, B.D.; Holmes, A. Behavior Change Strategies to Influence Antimicrobial Prescribing in Acute Care: A Systematic Review. Clin. Infect. Dis. 2011, 53, 651–662. [Google Scholar] [CrossRef] [PubMed]
- Talkhan, H.; Stewart, D.; Mcintosh, T.; Ziglam, H.; Abdulrouf, P.V.; Al-Hail, M.; Diab, M.; Cunningham, S. The use of theory in the development and evaluation of behaviour change interventions to improve antimicrobial prescribing: A systematic review. J. Antimicrob. Chemother. 2020, 75, 2394–2410. [Google Scholar] [CrossRef] [PubMed]
- Papoutsi, C.; Mattick, K.; Pearson, M.; Brennan, N.; Briscoe, S.; Wong, G. Social and professional influences on antimicrobial prescribing for doctors-in-training: A realist review. J. Antimicrob. Chemother. 2017, 72, 2418–2430. [Google Scholar] [CrossRef] [PubMed]
- Hart, E.; Nguyen, M.; Allen, M.; Clark, C.M.; Jacobs, D.M. A systematic review of the impact of antifungal stewardship interventions in the United States. Ann. Clin. Microbiol. Antimicrob. 2019, 18, 24. [Google Scholar] [CrossRef]
- Chong, W.H.; Neu, K.P. Incidence, diagnosis and outcomes of COVID-19-associated pulmonary aspergillosis (CAPA): A systematic review. J. Hosp. Infect. 2021, 113, 115–129. [Google Scholar] [CrossRef]
- Frost, F.J.; Nazareth, D.S.; Charman, S.C.; Winstanley, C.; Walshaw, M.J. Ivacaftor Is Associated with Reduced Lung Infection by Key Cystic Fibrosis Pathogens. A Cohort Study Using National Registry Data. Ann. Am. Thorac. Soc. 2019, 16, 1375–1382. [Google Scholar] [CrossRef]
- Logan, C.; Hemsley, C.; Fife, A.; Edgeworth, J.; Mazzella, A.; Wade, P.; Goodman, A.; Hopkins, P.; Wyncoll, D.; Ball, J.; et al. A multisite evaluation of antifungal use in critical care: Implications for antifungal stewardship. JAC Antimicrob. Resist. 2022, 4, dlac055. [Google Scholar] [CrossRef]
- Agrawal, S.; Barnes, R.; Brüggemann, R.J.; Rautemaa-Richardson, R.; Warris, A. The role of the multidisciplinary team in antifungal stewardship. J. Antimicrob. Chemother. 2016, 71 (Suppl. S2), ii37–ii42. [Google Scholar] [CrossRef]
| Positive Diagnostic Testing | Negative/No Diagnostic Testing | |
|---|---|---|
| Administered antifungals | 68 | 197 |
| Not administered antifungals | 18 | 168 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pates, K.; Shang, Z.; Jabbar, R.; Armstrong-James, D.; Schelenz, S.; Periselneris, J.; Arcucci, R.; Shah, A. The Effects of COVID-19 on Antifungal Prescribing in the UK—Lessons to Learn. J. Fungi 2024, 10, 787. https://doi.org/10.3390/jof10110787
Pates K, Shang Z, Jabbar R, Armstrong-James D, Schelenz S, Periselneris J, Arcucci R, Shah A. The Effects of COVID-19 on Antifungal Prescribing in the UK—Lessons to Learn. Journal of Fungi. 2024; 10(11):787. https://doi.org/10.3390/jof10110787
Chicago/Turabian StylePates, Katharine, Zhendan Shang, Rebeka Jabbar, Darius Armstrong-James, Silke Schelenz, Jimstan Periselneris, Rossella Arcucci, and Anand Shah. 2024. "The Effects of COVID-19 on Antifungal Prescribing in the UK—Lessons to Learn" Journal of Fungi 10, no. 11: 787. https://doi.org/10.3390/jof10110787
APA StylePates, K., Shang, Z., Jabbar, R., Armstrong-James, D., Schelenz, S., Periselneris, J., Arcucci, R., & Shah, A. (2024). The Effects of COVID-19 on Antifungal Prescribing in the UK—Lessons to Learn. Journal of Fungi, 10(11), 787. https://doi.org/10.3390/jof10110787







