Pre-operative Machine Learning for Heart Transplant Patients Bridged with Temporary Mechanical Circulatory Support †
Abstract
:1. Introduction
2. Materials and Methods
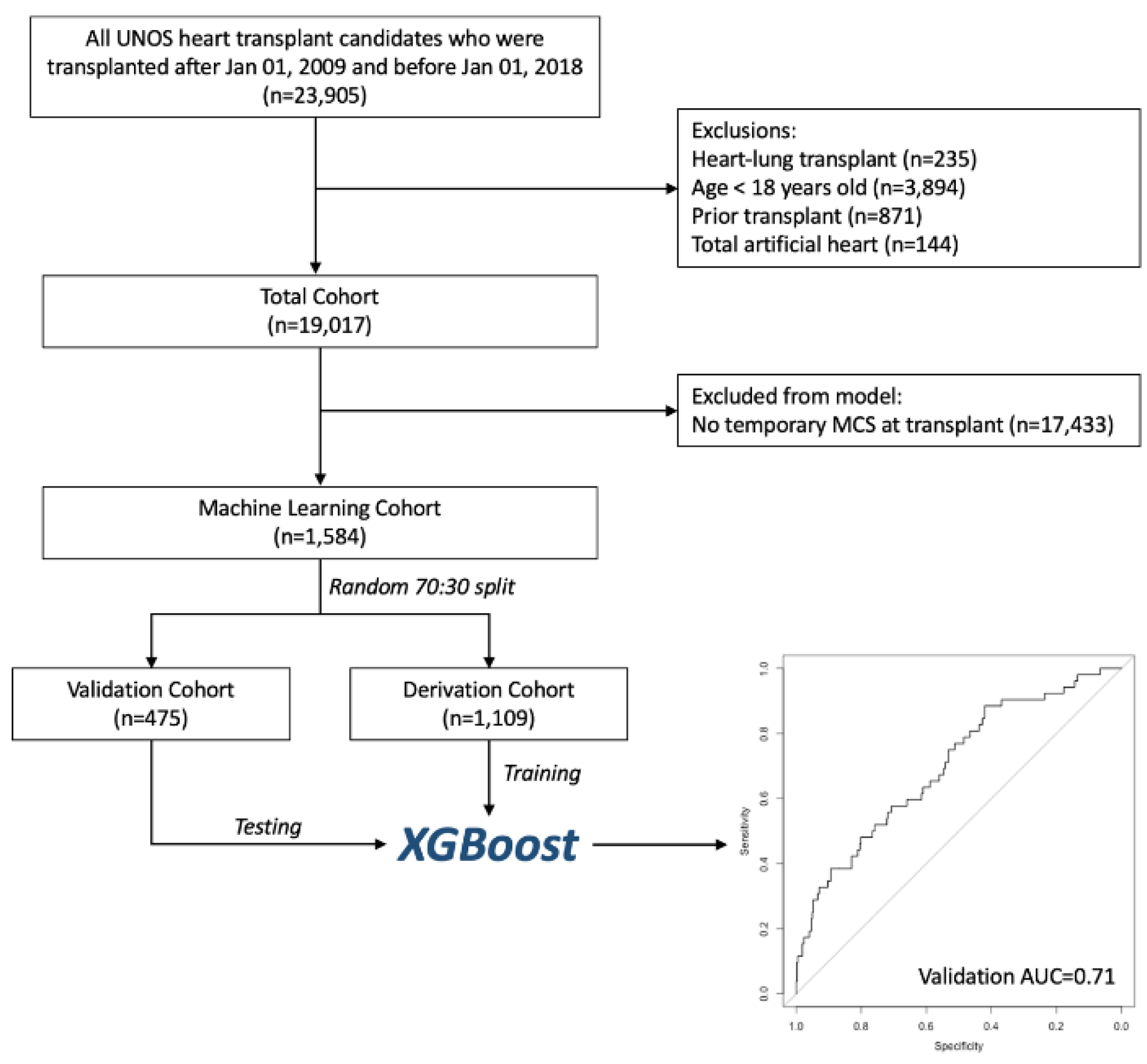
2.1. Patient Selection
2.2. Primary Outcome
2.3. Machine Learning Model Development
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Model Performance
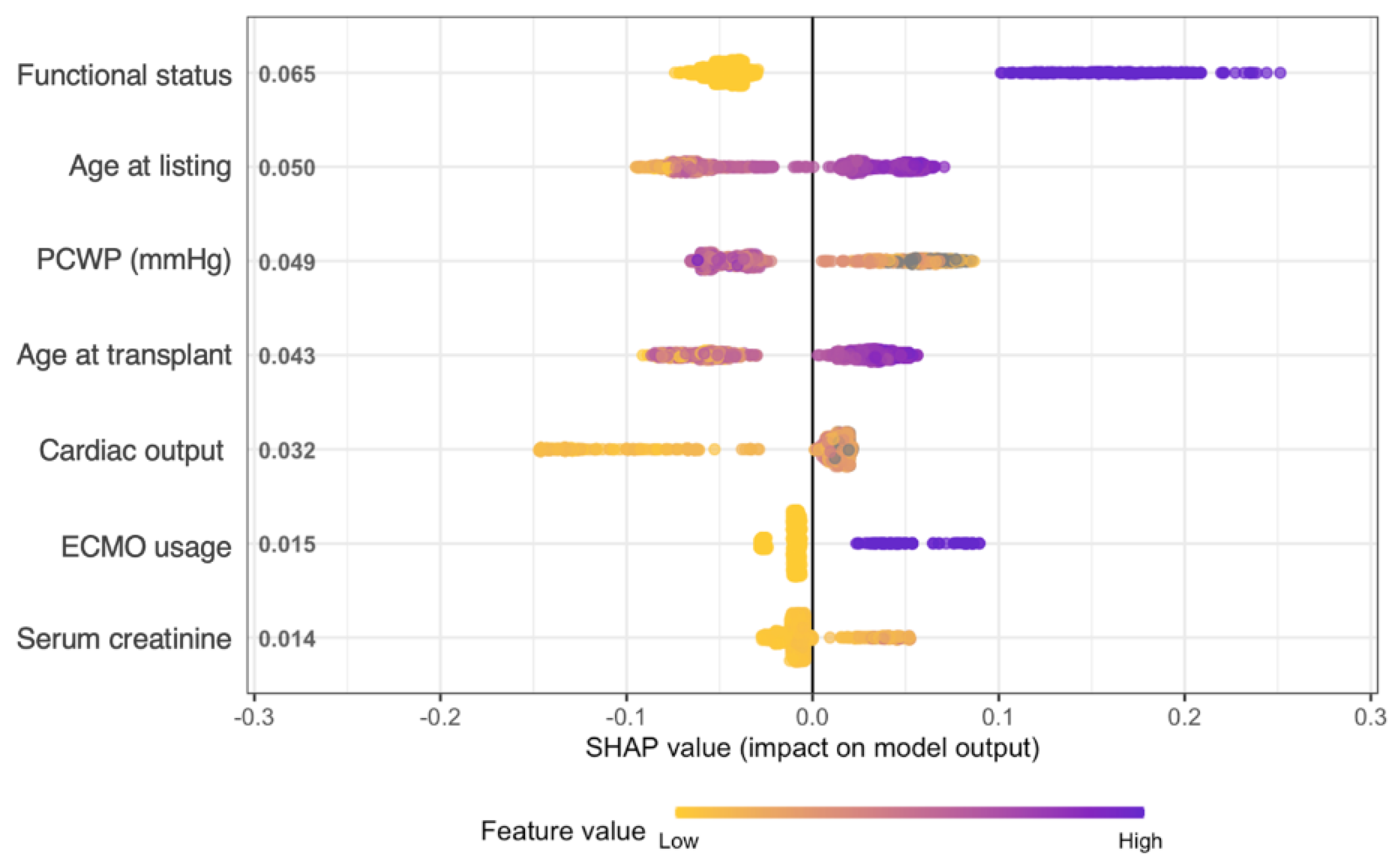
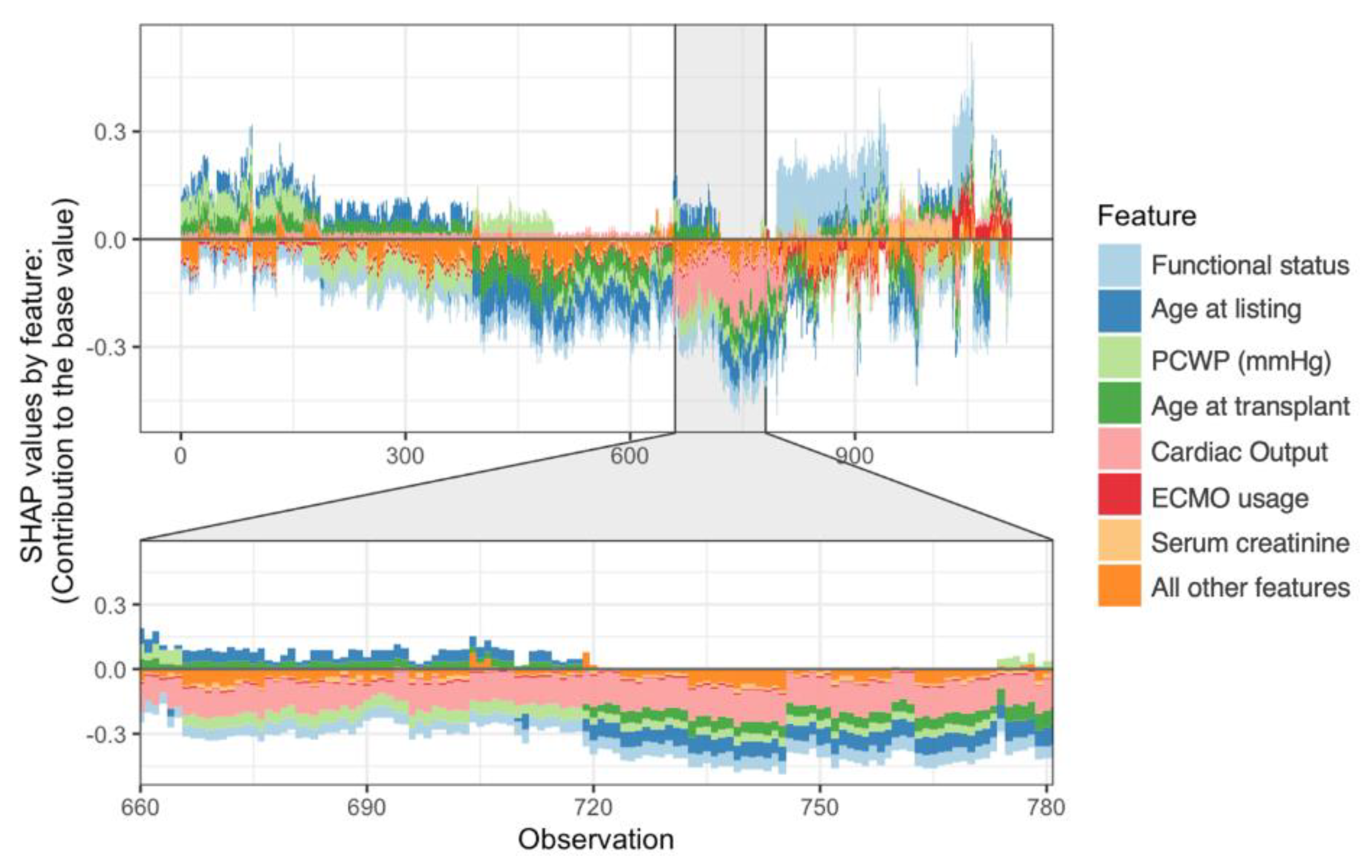
3.3. Model Explanations
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AUC | Area under the Receiver Operator Characteristics Curve |
| BTT | bridge to transplant |
| CO | cardiac output |
| ECMO | extracorporeal membrane oxygenation |
| IABP | intra-aortic balloon pump |
| ML | machine learning |
| OHT | orthotopic heart transplantation |
| PCWP | pulmonary capillary wedge pressure |
| PVAD | percutaneous ventricular assist device |
| SHAP | Shapley Additive Explanations |
| STS | Society of Thoracic Surgeons |
| tMCS | temporary mechanical circulatory support |
| UNOS | United Network for Organ Sharing |
References
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; CaseyJr, D.E.; Drazner, M.H.; Fonarow, C.C.; Geraci, S.A.; Horwich, T.; Januzzi, J.L.; et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013, 128, e240–e327. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Services, Organ Procurement and Transplantation Net-work. Adult Heart Allocation. 2018. Available online: https://optn.transplant.hrsa.gov/learn/professional-education/adult-heart-allocation/ (accessed on 10 November 2021).
- Varshney, A.S.; Berg, D.D.; Katz, J.N.; Baird-Zars, V.M.; Bohula, E.A.; Carnicelli, A.P.; Chaudhry, S.P.; Guo, J.; Lawler, P.R.; Nativi-Nicolau, J.; et al. Use of Temporary Mechanical Circulatory Support for Management of Cardiogenic Shock Before and After the United Network for Organ Sharing Donor Heart Allocation System Changes. JAMA Cardiol. 2020, 5, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Hong, K.N.; Iribarne, A.; Worku, B.; Takayama, H.; Gelijns, A.C.; Naka, Y.; Jeevanandam, V.; Russo, M.J. Who Is the High-Risk Recipient? Predicting Mortality After Heart Transplant Using Pretransplant Donor and Recipient Risk Factors. Ann. Thorac. Surg. 2011, 92, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Weiss, E.S.; Allen, J.G.; Kilic, A.; Russell, S.D.; Baumgartner, W.A.; Conte, J.V.; Shah, A.S. Development of a quantitative donor risk index to predict short-term mortality in orthotopic heart transplantation. J. Hear. Lung Transplant. 2011, 31, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Weiss, E.S.; Allen, J.G.; Arnaoutakis, G.J.; George, T.J.; Russell, S.D.; Shah, A.S.; Conte, J.V. Creation of a Quantitative Recipient Risk Index for Mortality Prediction After Cardiac Transplantation (IMPACT). Ann. Thorac. Surg. 2011, 92, 914–922. [Google Scholar] [CrossRef]
- Schulze, P.C.; Jiang, J.; Yang, J.; Cheema, F.H.; Schaeffle, K.; Kato, T.S.; Farr, M.; Restaino, S.; Deng, M.; Maurer, M.; et al. Preoperative Assessment of High-Risk Candidates to Predict Survival After Heart Transplantation. Circ. Hear. Fail. 2013, 6, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Yin, M.Y.; Wever-Pinzon, O.; Mehra, M.R.; Selzman, C.H.; Toll, A.E.; Cherikh, W.S.; Nativi-Nicolau, J.; Fang, J.C.; Kfoury, A.G.; Gilbert, E.M.; et al. Post-transplant outcome in patients bridged to transplant with temporary mechanical circulatory support devices. J. Hear. Lung Transplant. 2019, 38, 858–869. [Google Scholar] [CrossRef]
- Rajkomar, A.; Dean, J.; Kohane, I. Machine Learning in Medicine. N. Engl. J. Med. 2019, 380, 1347–1358. [Google Scholar] [CrossRef]
- Sidey-Gibbons, J.A.M.; Sidey-Gibbons, C.J. Machine learning in medicine: A practical introduction. BMC Med. Res. Methodol. 2019, 19, 1–18. [Google Scholar] [CrossRef]
- Sánchez-Cabo, F.; Rossello, X.; Fuster, V.; Benito, F.; Manzano, J.P.; Silla, J.C.; Fernández-Alvira, J.M.; Oliva, B.; Fernández-Friera, L.; López-Melgar, B.; et al. Machine Learning Improves Cardiovascular Risk Definition for Young, Asymptomatic Individuals. J. Am. Coll. Cardiol. 2020, 76, 1674–1685. [Google Scholar] [CrossRef]
- Kampaktsis, P.N.; Tzani, A.; Doulamis, I.P.; Moustakidis, S.; Drosou, A.; Diakos, N.; Drakos, S.G.; Briasoulis, A. State-of-the-art machine learning algorithms for the prediction of outcomes after contemporary heart transplantation: Results from the UNOS database. Clin. Transplant. 2021, 35, e14388. [Google Scholar] [CrossRef] [PubMed]
- Lin, A.; Van Diemen, V.; Motwani, M.; McElhinney, P.; Otaki, Y.; Kwan, A.; Han, D.; Kuronuma, K.; Klein, E.; Grodecki, K.; et al. Machine Learning Ischemia Risk Score From Coronary Ct Angi-Ography Predicts Lesion-Specific Ischemia And Impaired Myocardial Blood Flow: Results From The Pacific Trial. J. Am. Coll. Cardiol. 2021, 77, 1269. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. XGBoost: A Scalable Tree Boosting System. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, ACM, San Francisco, CA, USA, 13–17 August 2016. [Google Scholar]
- Lundberg, S.M.; Lee, S.-I. A Unified Approach to Interpreting Model Predictions. In Advances in Neural Information Processing Systems; MIT Press: Cambridge, MA, USA, 2017; pp. 4768–4777. [Google Scholar]
- Delong, E.R.; Delong, D.M.; Clarke-Pearson, D.L. Comparing the Areas under Two or More Correlated Receiver Operating Characteristic Curves: A Nonparametric Approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Coutance, G.; Kransdorf, E.; Bonnet, G.; Loupy, A.; Kobashigawa, J.; Patel, J.K. Statistical performance of 16 posttransplant risk scores in a contemporary cohort of heart transplant recipients. Am. J. Transplant. 2020, 21, 645–656. [Google Scholar] [CrossRef]
- O’Brien, S.M.; Feng, L.; He, X.; Xian, Y.; Jacobs, J.P.; Badhwar, V.; Kurlansky, P.A.; Furnary, A.P.; Cleveland, J.C., Jr.; Lobdell, K.W.; et al. The Society of Thoracic Surgeons 2018 Adult Cardiac Surgery Risk Models: Part 2—Statistical Methods and Results. Ann. Thorac. Surg. 2018, 105, 1419–1428. [Google Scholar] [CrossRef]
- Ong, C.S.; Reinertsen, E.; Sun, H.; Moonsamy, P.; Mohan, N.; Funamoto, M.; Kaneko, T.; Shekar, P.S.; Schena, S.; Lawton, J.S.; et al. Prediction of operative mortality for patients undergoing cardiac surgical procedures without established risk scores. J. Thorac. Cardiovasc. Surg. 2021. [Google Scholar] [CrossRef]
- Kilic, A.; Goyal, A.; Miller, J.K.; Gleason, T.G.; Dubrawksi, A. Performance of a Machine Learning Algorithm in Predicting Outcomes of Aortic Valve Replacement. Ann. Thorac. Surg. 2020, 111, 503–510. [Google Scholar] [CrossRef]
- Kilic, A.; Goyal, A.; Miller, J.K.; Gjekmarkaj, E.; Tam, W.L.; Gleason, T.G.; Sultan, I.; Dubrawksi, A. Predictive Utility of a Machine Learning Algorithm in Estimating Mortality Risk in Cardiac Surgery. Ann. Thorac. Surg. 2019, 109, 1811–1819. [Google Scholar] [CrossRef]
- Freund, Y.; Schapire, R.E. A Short Introduction to Boosting. J. Jpn. Soc. Artif. Intell. 1999, 14, 1612. [Google Scholar]
- Yoon, J.; Zame, W.R.; Banerjee, A.; Cadeiras, M.; Alaa, A.M.; Van Der Schaar, M. Personalized survival predictions via Trees of Predictors: An application to cardiac transplantation. PLoS ONE 2018, 13, e0194985. [Google Scholar] [CrossRef]
- Killian, M.O.; Payrovnaziri, S.N.; Gupta, D.; Desai, D.; He, Z. Machine learning–based prediction of health outcomes in pediatric organ transplantation recipients. JAMIA Open 2021, 4, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hinton, G. Deep Learning—A Technology With the Potential to Transform Health Care. JAMA 2018, 320, 1101–1102. [Google Scholar] [CrossRef] [PubMed]
- Karnofsky, D.A.; Burchenal, J.H. The clinical evaluation of chemotherapeutic agents in cancer. In Evaluation of Chemotherapeutic Agents; MacLeod, C.M., Ed.; Columbia University Press: New York, NY, USA, 1949; pp. 191–205. [Google Scholar]
- Abd Elrahman, S.M.; Abraham, A. A Review of Class Imbalance Problem. J. Netw. Innov. Comput. 2013, 1, 332–340. [Google Scholar]
- Defilippis, E.M.; Psotka, M.A.; Khazanie, P.; Cowger, J.; Cogswell, R. Exploring Physician Perceptions of the 2018 United States Heart Transplant Allocation System. J. Card. Fail. 2022, 28, 670–674. [Google Scholar] [CrossRef]
- Parker, W.F.; Chung, K.; Anderson, A.S.; Siegler, M.; Huang, E.S.; Churpek, M.M. Practice Changes at U.S. Transplant Centers After the New Adult Heart Allocation Policy. J. Am. Coll. Cardiol. 2020, 75, 2906–2916. [Google Scholar] [CrossRef]

| Variable | Survived n = 1405 | Died n = 179 | p Value |
|---|---|---|---|
| Age, years | 55 (45–62) | 59 (50–64) | <0.001 |
| Male sex | 1037 (73.8%) | 132 (73.7%) | 0.99 |
| Diabetes | 383 (27.3%) | 65 (36.3%) | 0.01 |
| Body mass index (kg/m2) | 26.0 (23.1–29.8) | 27.2 (23.7–30.8) | 0.019 |
| Ischemic time, hours | 3.1 (2.4–3.8) | 3.2 (2.6–3.8) | 0.42 |
| Total days on waitlist | 34 (12–90) | 43 (12–117) | 0.17 |
| Ethnicity | 0.34 | ||
| White | 903 (64.3%) | 111 (62.0%) | |
| Black | 333 (23.7%) | 38 (21.2%) | |
| Hispanic | 106 (7.5%) | 19 (10.6%) | |
| Other | 63 (4.5%) | 11 (6.1%) | |
| Donor age, years | 30 (23–41) | 34 (23–45) | 0.12 |
| Donor male sex | 949 (67.5%) | 117 (65.4%) | 0.56 |
| Hemodynamics at listing | |||
| Cardiac output | 3.9 (3.14–4.82) | 4 (3.185–4.7) | 0.70 |
| PCWP | 22.0 (16.0–28.0) | 21.0 (15.0–28.0) | 0.66 |
| MPAP | 32 (25–38) | 31.5 (24–39.5) | 0.45 |
| PA systolic pressure | 45 (36–54) | 48 (37–56.5) | 0.17 |
| PA diastolic pressure | 23 (17–28) | 22 (16.5–29.5) | 0.99 |
| Inotrope usage | 661 (47.0%) | 82 (45.8%) | 0.75 |
| Hemodynamics at transplant | |||
| Cardiac output | 4 (3.19–5) | 4.14 (3.4–5.1) | 0.10 |
| PCWP | 22.0 (16.0–28.0) | 20.5 (13.5–27.0) | 0.04 |
| MPAP | 31 (24–39) | 30 (23–38) | 0.28 |
| PA systolic pressure | 45 (35–55) | 42 (34–55) | 0.36 |
| PA diastolic pressure | 23 (16–29) | 22 (16–28) | 0.22 |
| Inotrope usage | 813 (57.9%) | 89 (49.7%) | 0.04 |
| Serum creatinine (mg/dl) | 1.14 (0.90–1.50) | 1.30 (1.00–1.70) | 0.001 |
| Total bilirubin (mg/dL) | 0.9 (0.6–1.4) | 1.0 (0.6–1.7) | 0.05 |
| Implantable cardiac defibrillator | 1015 (72.6%) | 142 (80.2%) | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shou, B.L.; Chatterjee, D.; Russel, J.W.; Zhou, A.L.; Florissi, I.S.; Lewis, T.; Verma, A.; Benharash, P.; Choi, C.W. Pre-operative Machine Learning for Heart Transplant Patients Bridged with Temporary Mechanical Circulatory Support. J. Cardiovasc. Dev. Dis. 2022, 9, 311. https://doi.org/10.3390/jcdd9090311
Shou BL, Chatterjee D, Russel JW, Zhou AL, Florissi IS, Lewis T, Verma A, Benharash P, Choi CW. Pre-operative Machine Learning for Heart Transplant Patients Bridged with Temporary Mechanical Circulatory Support. Journal of Cardiovascular Development and Disease. 2022; 9(9):311. https://doi.org/10.3390/jcdd9090311
Chicago/Turabian StyleShou, Benjamin L., Devina Chatterjee, Joseph W. Russel, Alice L. Zhou, Isabella S. Florissi, Tabatha Lewis, Arjun Verma, Peyman Benharash, and Chun Woo Choi. 2022. "Pre-operative Machine Learning for Heart Transplant Patients Bridged with Temporary Mechanical Circulatory Support" Journal of Cardiovascular Development and Disease 9, no. 9: 311. https://doi.org/10.3390/jcdd9090311
APA StyleShou, B. L., Chatterjee, D., Russel, J. W., Zhou, A. L., Florissi, I. S., Lewis, T., Verma, A., Benharash, P., & Choi, C. W. (2022). Pre-operative Machine Learning for Heart Transplant Patients Bridged with Temporary Mechanical Circulatory Support. Journal of Cardiovascular Development and Disease, 9(9), 311. https://doi.org/10.3390/jcdd9090311





