Complete Atrioventricular Block Caused by Retrograde Transaortic Approach
Abstract
:1. Introduction
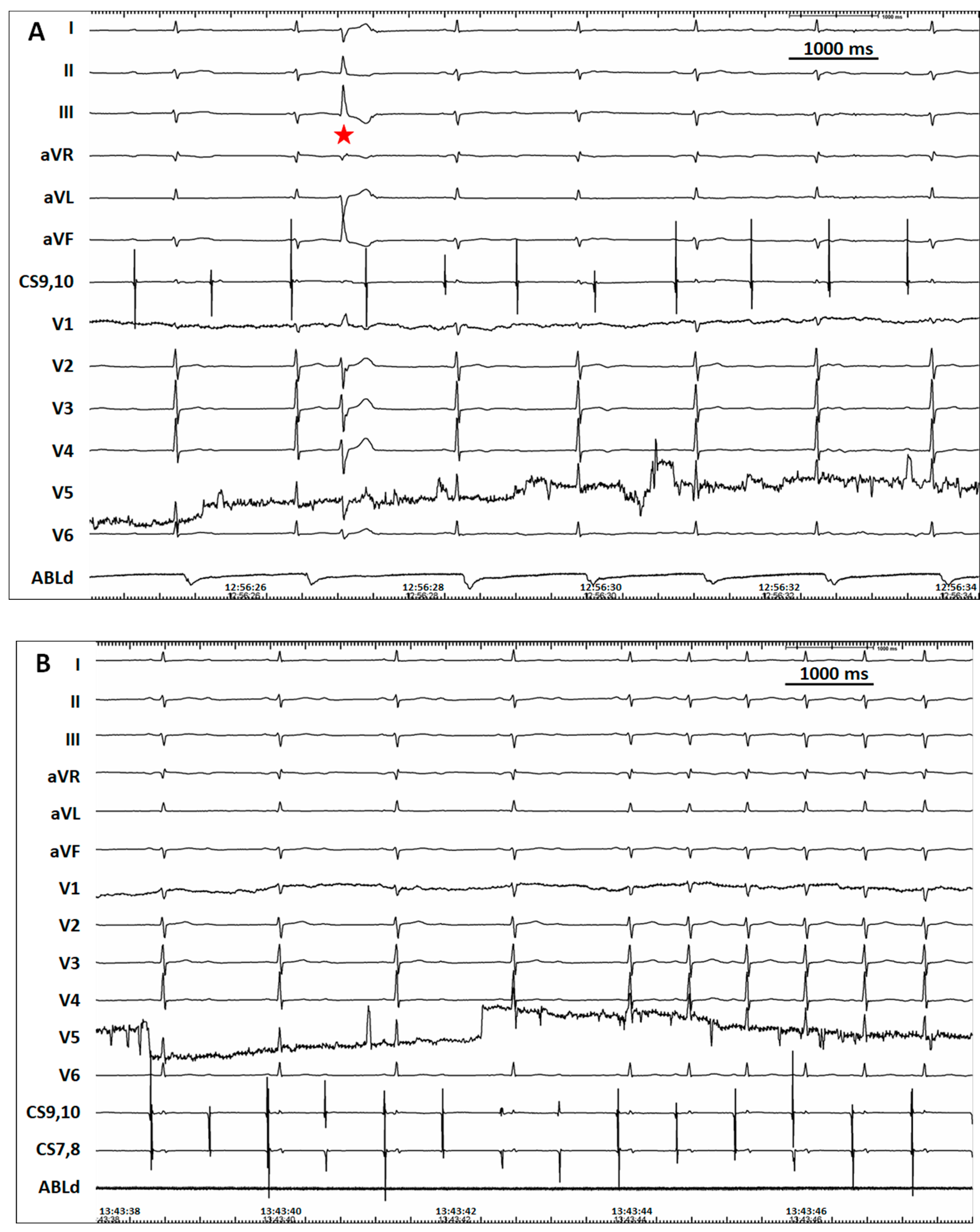
2. Case Report
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, S.; Lu, X.; Peng, S.; Xue, Y.; Zhou, G.; Ling, Z.; Wei, Y.; Yang, K.; Fu, W.; Cai, L.; et al. Ablation at Right Coronary Cusp as an Alternative and Favorable Approach to Eliminate Premature Ventricular Complexes Originating From the Proximal Left Anterior Fascicle. Circ. Arrhythmia Electrophysiol. 2020, 13, e008173. [Google Scholar] [CrossRef]
- Chen, S.; Yang, K.; Lu, X.; Liu, S. Ablation From the Right Coronary Cusp Eliminated Premature Ventricular Contractions Originating From the Proximal Left Anterior Fascicle. Circ. J. 2019, 83, 2327. [Google Scholar] [CrossRef]
- Adlan, A.M.; Campbell, T.; Fairbairn, T.; Aggarwal, S.; Nawaytou, O.; Penha, D.; Todd, D.; Mahida, S. Retrograde aortic access during ventricular tachycardia ablation: Indications, techniques, and challenges. J. Cardiovasc. Electrophysiol. 2019, 30, 2629–2639. [Google Scholar] [CrossRef]
- Anselmino, M.; Matta, M.; Saglietto, A.; Calò, L.; Giustetto, C.; Scaglione, M.; Gaita, F. Transseptal or retrograde approach for transcatheter ablation of left sided accessory pathways: A systematic review and meta-analysis. Int. J. Cardiol. 2018, 272, 202–207. [Google Scholar] [CrossRef]
- Elizari, M. The normal variants in the left bundle branch system. J. Electrocardiol. 2017, 50, 389–399. [Google Scholar] [CrossRef]
- Massing, G.K.; James, T.N. Anatomical configuration of the His bundle and bundle branches in the human heart. Circulation 1976, 53, 609–621. [Google Scholar] [CrossRef]
- Chen, S.; Zhang, F.; Wei, Y.; Lu, X.; Zhou, G.; Liu, S. Alternating and gradually changing narrow QRS complex tachycardia in a patient with heart failure: What is the mechanism? Ann. Noninvasive Electrocardiol. 2021, 26, e12836. [Google Scholar] [CrossRef]
- Chen, S.; Wei, Y.; Zhou, G.; Lu, X.; Liu, S. To the Editor—The characteristics and potential origin of the proximal left anterior fascicle premature ventricular complexes. Heart Rhythm 2022. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, S.; Lu, X.; Zhang, Q.; Wei, Y.; Zhou, G.; Liu, S. Complete Atrioventricular Block Caused by Retrograde Transaortic Approach. J. Cardiovasc. Dev. Dis. 2022, 9, 293. https://doi.org/10.3390/jcdd9090293
Chen S, Lu X, Zhang Q, Wei Y, Zhou G, Liu S. Complete Atrioventricular Block Caused by Retrograde Transaortic Approach. Journal of Cardiovascular Development and Disease. 2022; 9(9):293. https://doi.org/10.3390/jcdd9090293
Chicago/Turabian StyleChen, Songwen, Xiaofeng Lu, Qitong Zhang, Yong Wei, Genqing Zhou, and Shaowen Liu. 2022. "Complete Atrioventricular Block Caused by Retrograde Transaortic Approach" Journal of Cardiovascular Development and Disease 9, no. 9: 293. https://doi.org/10.3390/jcdd9090293
APA StyleChen, S., Lu, X., Zhang, Q., Wei, Y., Zhou, G., & Liu, S. (2022). Complete Atrioventricular Block Caused by Retrograde Transaortic Approach. Journal of Cardiovascular Development and Disease, 9(9), 293. https://doi.org/10.3390/jcdd9090293




