RETRACTED: A Systematic Review of Personalized Health Applications through Human–Computer Interactions (HCI) on Cardiovascular Health Optimization
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Study Selection
Inclusion and Exclusion Criteria
2.3. Data Extraction and Analysis
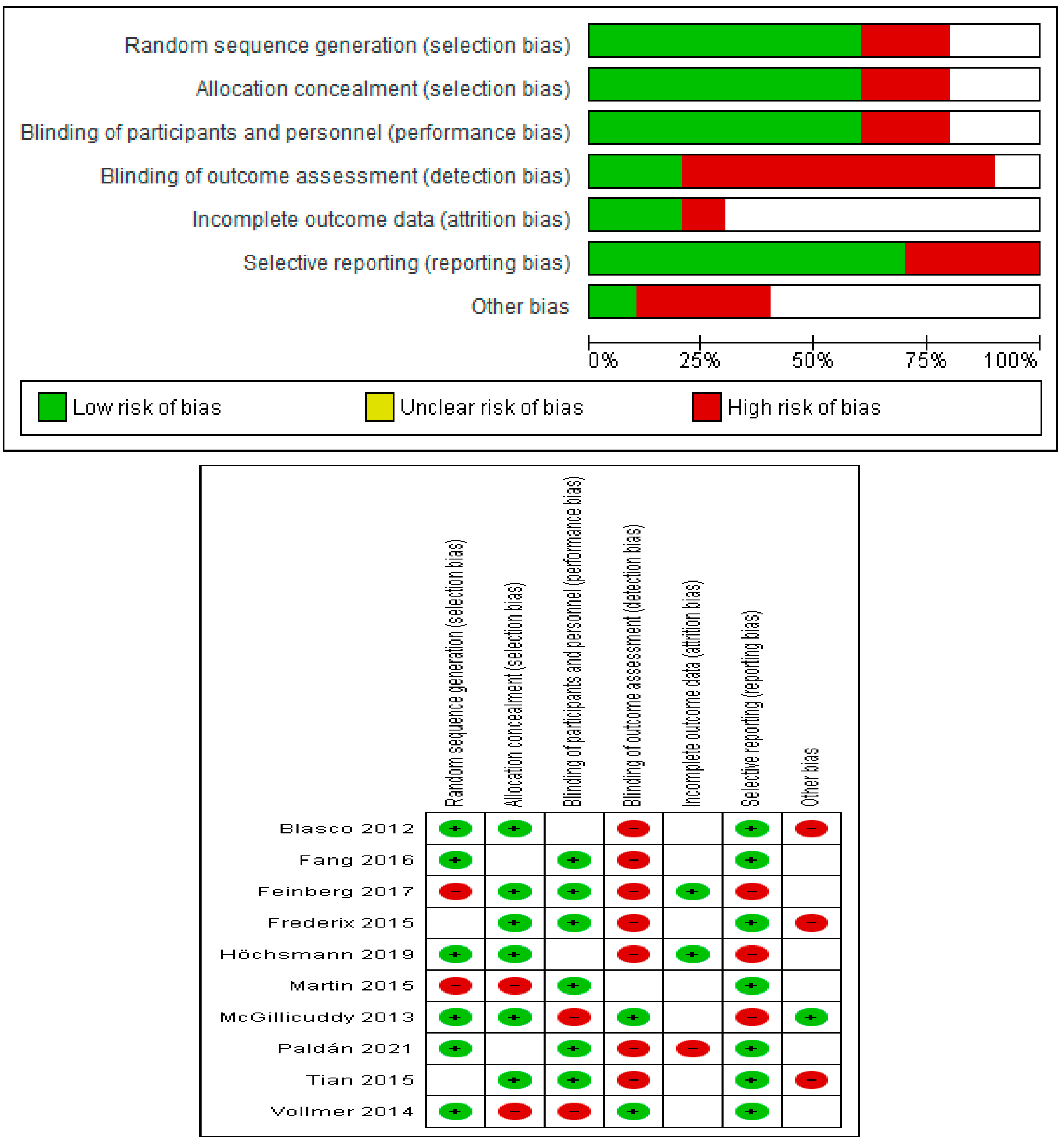
2.4. Risk of Bias
3. Results
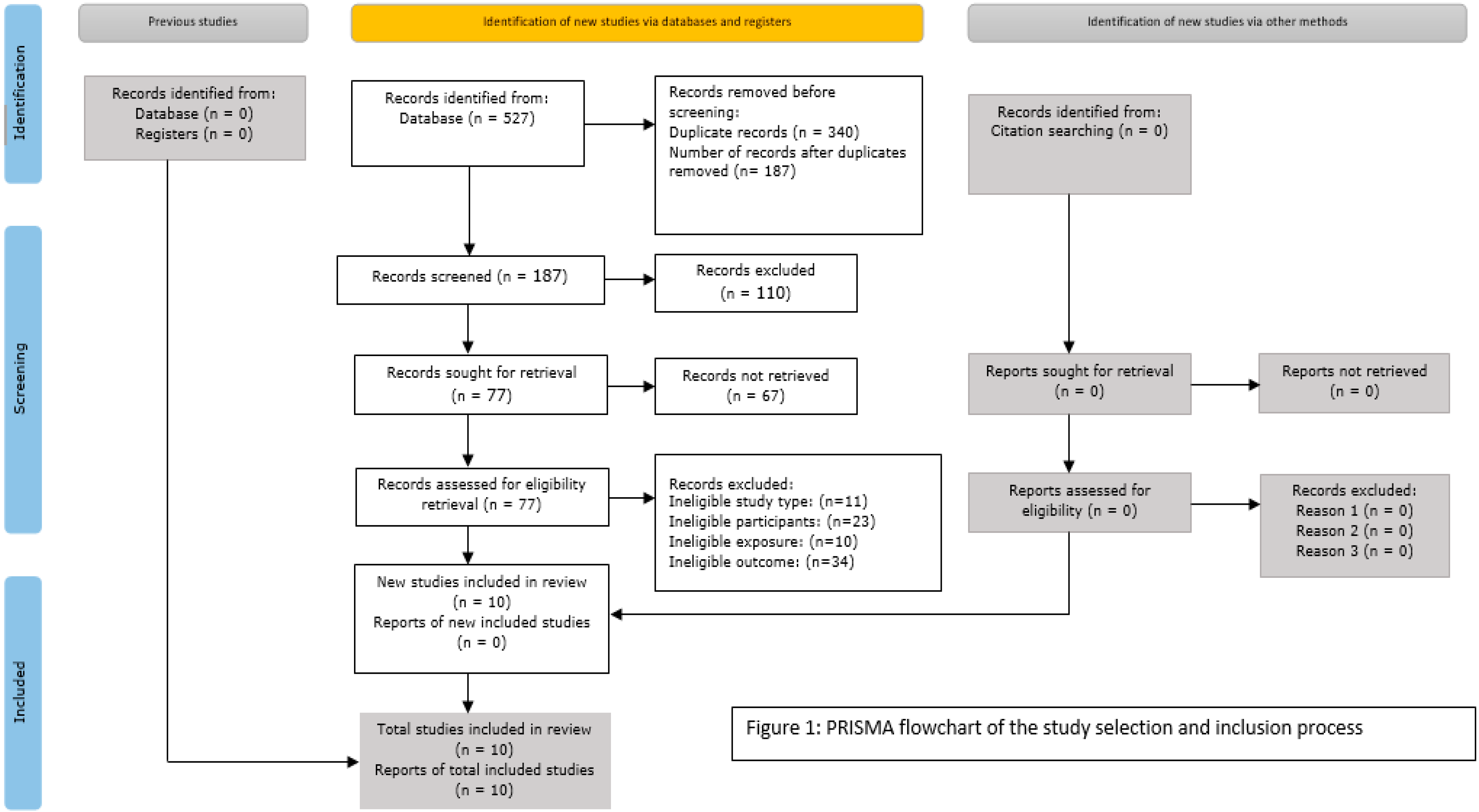
3.1. Study Selection Process
3.2. Characteristics of Included Studies
3.3. Risk of Bias of the Included Study
3.4. Thematic Synthesis of Results
3.4.1. Telehealth (mHealth App) Interventions
3.4.2. Effectiveness of App Interventions
4. Discussion and Conclusions
4.1. Discussion
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gay, H.C.; Rao, S.G.; Vaccarino, V.; Ali, M.K. Effects of different dietary interventions on blood pressure: Systematic review and meta-analysis of randomized controlled trials. Hypertension 2016, 67, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Soriano, J.B.; Kendrick, P.J.; Paulson, K.R.; Gupta, V.; Abrams, E.M.; Adedoyin, R.A.; Moradi, M. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 2020, 8, 585–596. [Google Scholar] [CrossRef]
- Koumpouros, Y. A highly user-centered design approach for developing a mobile health app for pain management (PainApp). In Proceedings of the 14th PErvasive Technologies Related to Assistive Environments Conference, Corfu, Greece, 29 June–2 July 2021; Volume 29, pp. 320–329. [Google Scholar]
- Simon, S.T.; Kini, V.; Levy, A.E.; Ho, P.M. Medication adherence in cardiovascular medicine. BMJ 2021, 11, 374. [Google Scholar] [CrossRef] [PubMed]
- Pan, A.; Zhao, F. User acceptance factors for mHealth. In International Conference on Human-Computer Interaction; Springer: Cham, Switzerland, 2018; Volume 15, pp. 173–184. [Google Scholar]
- Akkaş, M.A.; Sokullu, R.; Çetin, H.E. Healthcare and patient monitoring using IoT. Internet Things 2020, 1, 100173. [Google Scholar] [CrossRef]
- Evans, E.; Zengul, A.; Hall, A.; Qu, H.; Willig, A.; Cherrington, A.; Thirumalai, M. Disability-inclusive diabetes selfmanagement telehealth program: Protocol for a pilot and feasibility study. JMIR Res. Protoc. 2021, 10, e31689. [Google Scholar] [CrossRef]
- Soiza, R.L.; Myint, P.K. The Scottish Intercollegiate guidelines network (sign) 157: Guidelines on risk reduction and management of delirium. Medicina 2019, 55, 491. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA.Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Martin, S.S.; Feldman, D.I.; Blumenthal, R.S.; Jones, S.R.; Post, W.S.; McKibben, R.A.; Michos, E.D.; Ndumele, C.E.; Ratchford, E.V.; Coresh, J.; et al. mActive: A randomized clinical trial of an automated mHealth intervention for physicalactivity promotion. J. Am. Heart Assoc. 2015, 4, e002239. [Google Scholar] [CrossRef]
- McGillicuddy, J.W.; Gregoski, M.J.; Weiland, A.K.; Rock, R.A.; Brunner-Jackson, B.M.; Patel, S.K.; Thomas, B.S.; Taber, D.J.; Chavin, K.D.; Baliga, P.K.; et al. Mobile health medication adherence and blood pressure control in renal transplant recipients: A proof-of-concept randomized controlled trial. JMIR Res. Protoc. 2013, 2, e2633. [Google Scholar] [CrossRef]
- Höchsmann, C.; Infanger, D.; Klenk, C.; Königstein, K.; Walz, S.P.; Schmidt-Trucksäss, A. Effectiveness of a behavior change technique–based smartphone game to improve intrinsic motivation and physical activity adherence in patients with type 2 diabetes: Randomized controlled trial. JMIR Serious Games 2019, 7, e11444. [Google Scholar] [CrossRef]
- Paldán, K.; Steinmetz, M.; Simanovski, J.; Rammos, C.; Ullrich, G.; Jánosi, R.A.; Moebus, S.; Rassaf, T.; Lortz, J. Supervised Exercise Therapy Using Mobile Health Technology in Patients with Peripheral Arterial Disease: Pilot Randomized Controlled Trial. JMIR mHealth uHealth 2021, 9, e24214. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, L.; Menon, J.; Smith, R.; Rajeev, J.G.; Kumar, R.K.; Banerjee, A. Potential for mobile health (mHealth) prevention of cardiovascular diseases in Kerala: A population-based survey. Indian Heart J. 2017, 69, 182–199. [Google Scholar] [CrossRef] [PubMed]
- Frederix, I.; Hansen, D.; Coninx, K.; Vandervoort, P.; Vandijck, D.; Hens, N.; Van Craenenbroeck, E.; Van Driessche, N.; Dendale, P. Medium-term effectiveness of a comprehensive internet-based and patient-specific telerehabilitation program with text messaging support for cardiac patients: Randomized controlled trial. J. Med. Internet Res. 2015, 17, e4799. [Google Scholar] [CrossRef]
- Fang, R.; Li, X. Electronic messaging support service programs improve adherence to lipid-lowering therapy among outpatients with coronary artery disease: An exploratory randomised control study. J. Clin. Nurs. 2016, 25, 664–671. [Google Scholar] [CrossRef]
- Blasco, A.; Carmona, M.; Fernández-Lozano, I.; Salvador, C.H.; Pascual, M.; Sagredo, P.G.; Somolinos, R.; Muñoz, A.; García-López, F.; Escudier, J.M.; et al. Evaluation of a telemedicine service for the secondary prevention of coronaryartery disease. J. Cardiopulm. Rehabil. Prev. 2012, 32, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Tian, M.; Ajay, V.S.; Dunzhu, D.; Hameed, S.S.; Li, X.; Liu, Z.; Li, C.; Chen, H.; Cho, K.; Li, R.; et al. A cluster-randomized, controlled trial of a simplified multifaceted management program for individuals at high cardiovascular risk (SimCard trial) in rural Tibet, China, and Haryana, India. Circulation 2015, 132, 815–824. [Google Scholar] [CrossRef]
- Vollmer, W.M.; Owen-Smith, A.A.; Tom, J.O.; Laws, R.; Ditmer, D.G.; Smith, D.H.; Waterbury, A.C.; Schneider, J.L.; Yonehara, C.H.; Williams, A.; et al. Improving adherence to cardiovascular disease medications with information technology. Am. J. Manag. Care 2014, 20, SP502. [Google Scholar] [PubMed]
- Liu, S. Epigenetics advancing personalized nanomedicine in cancer therapy. Adv. Drug Deliv. Rev. 2012, 64, 1532–1543. [Google Scholar] [CrossRef]
- Gandapur, Y.; Kianoush, S.; Kelli, H.M.; Misra, S.; Urrea, B.; Blaha, M.J.; Graham, G.; Marvel, F.A.; Martin, S.S. The role of mHealth for improving medication adherence in patients with cardiovascular disease: A systematic review. Eur. Heart J. Qual. Care Clin. Outcomes 2016, 2, 237–244. [Google Scholar] [CrossRef]
- Urrea, B.; Misra, S.; Plante, T.B.; Kelli, H.M.; Misra, S.; Blaha, M.J.; Martin, S.S. Mobile health initiatives to improve outcomes in primary prevention of cardiovascular disease. Curr. Treat. Options Cardiovasc. Med. 2015, 17, 1–12. [Google Scholar] [CrossRef]
- Yardley, L.; Morrison, L.; Bradbury, K.; Muller, I. The person-based approach to intervention development: Application to digital health-related behavior change interventions. J. Med. Internet Res. 2015, 17, e4055. [Google Scholar] [CrossRef] [PubMed]
- Heran, B.S.; Chen, J.M.; Ebrahim, S.; Moxham, T.; Oldridge, N.; Rees, K.; Thompson, D.R.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2011. [CrossRef]
- Zwisler, A.D.; Norton, R.J.; Dean, S.G.; Dalal, H.; Tang, L.H.; Wingham, J.; Taylor, R.S. Home-based cardiac rehabilitation for people with heart failure: A systematic review and meta-analysis. Int. J. Cardiol. 2016, 221, 963–969. [Google Scholar] [CrossRef] [PubMed]
- Pollock, M.L.; Franklin, B.A.; Balady, G.J.; Chaitman, B.L.; Fleg, J.L.; Fletcher, B.; Limacher, M.; Piña, I.L.; Stein, R.A.; Williams, M.; et al. Resistance exercise in individuals with and without cardiovascular disease: Benefits, rationale, safety, and prescription an advisory from the committee on exercise, rehabilitation, and prevention, council on clinical cardiology, American Heart Association. Circulation 2000, 101, 828–833. [Google Scholar] [CrossRef] [PubMed]
- Mathur, S.; Zammitt, N.N.; Frier, B.M. Optimal glycaemic control in elderly people with type 2 diabetes: What does the evidence say? Drug Saf. 2015, 38, 17–32. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.L.; Fonarow, G.C.; Horwich, T.B. Obesity and the obesity paradox in heart failure. Prog. Cardiovasc. Dis. 2014, 56, 409–414. [Google Scholar] [CrossRef]
| Author & Year | Country | Study Design | No. of Participants | Intervention | Follow up Duration | Measurement Methods | Results/Outcomes | Limitations | Conclusion |
|---|---|---|---|---|---|---|---|---|---|
| Feinberg et al., 2017 | India | Survey | 262 | mHealth (mobile phone use in healthcare) | NA | IBM-SPSS version 20 was used for data analysis. Kolmogorov–Smirnov tests were used to identify variable normality. Relevant variables with statistical significance of p < 0.10 were identified using Chi-square tests for categorical covariates, Kruskal–Wallis test for non-continuously distributed covariates, and independent sample t-tests for continuously distributed covariates. Logistic regression was used to investigate the relationship between these variables and mobile phone usage characteristics. A p-value ≤0.05 was considered statistically significant. | 92% were willing to receive mHealth advice; 94% favored mobile medication reminders; 70.3% and 73% preferred voice calls over short messaging service (SMS) for delivering health information and medication reminders, respectively. 85.9% would send home recorded information on their blood pressure, weight, medication use, and lifestyle to a doctor. | Over-presentation of high economic status in the sample affected generalizability for other population sectors. Study also used convenience sampling and a limited sample size that affect its generalizability to represent the whole population. | Majority of the population approved the use of mHealth interventions, with preference of further investigation on mHealth use as educational tool to manage cardiovascular disease |
| Höchsmann et al., 2019 | Finland | RCT | 36 (45–70 years) | mHealth app (smartphone game as a behavioral change technique) | 24 weeks | Intrinsic physical activity (PA) motivation was assessed with an abridged 12-item version of the Intrinsic Motivation Inventory (IMI) before and after the intervention. Adherence to the game-proposed PA recommendations during the intervention period was assessed in the intervention group via the phone-recorded game usage data | Intrinsic PA motivation (IMI total score) increased significantly in the intervention group (+6.4 (SD 4.2; p < 0.001) points) while it decreased by 1.9 (SD 16.5; p = 0.623) points in the control group. The usage data revealed that participants in the intervention group used the game for an average of 131.1 (SD 48.7) minutes of in-game walking and for an average of 15.3 (SD 24.6) minutes of strength training per week, implying a significant positive association between total in-game training (min) and change in IMI total score (beta = 0.0028; 95% CI 0.0007–0.0049; p = 0.01). | The study lacked an objective measure of records of any additional physical activity (PA) beyond phone recorded PA. These periods without phone wear likely led to an underestimation of unknown magnitude of the true number of daily steps. | Study shows that a novel smartphone exergame that incorporates established motivational elements and personalized PA recommendations in the storyline can generate significant increases in intrinsic PA motivation in inactive individuals with type 2 diabetes |
| Paldán et al., 2021 | Finland | RCT | 46 | mHealth app (mobile intervention software-TrackPAD) | 3 months | The distance covered in the 6-minute walking test using the TENALEA software. The PAD-related peripheral arterial disease quality of life (PAD-QoL) was assessed by the PAD-QoL questionnaire at baseline and follow-up. | The intervention group (n = 19) increased their mean 6-min walking distance (83 m, SD 72.2), while the control group (n = 20) decreased their mean distance after 3 months of follow-up (–38.8 m, SD 53.7; p = 0.01). The peripheral arterial disease–related quality of life increased significantly in terms of “symptom perception” and “limitations in physical functioning.” Users’ feedback showed increased motivation and a changed attitude toward performing supervised exercise training. | There were weaknesses of the general gestural concept resulting from advanced age of the user groups who are inexperienced in using mHealth. Since the study designed a platform for both iOS and Android, some technical issues occurred due to the different technical implementations of the provider. | The mobile intervention TrackPAD was linked to a change in prognosis-relevant outcome measures combined with enhanced coping with the disease |
| Vollmer et al., 2014 | Kaiser Permanente health plan regions (Northwest, Hawaii and Georgia) | RCT | 21,752 (above 40 years) | Interactive voice recognition calls (IVR regular and IVR advanced). IVR participants received automated phone calls when they were due or overdue for a refill. IVR+ participants received these phone calls, plus personalized reminder letters, live outreach calls, EMR-based feedback to their primary care providers, and additional mailed materials. | 12 months | A modified version of the Proportion of Days Covered (PDC) was used to measure medication adherence as the primary measure. EMR was used to capture age, race, gender, and healthcare utilization for diabetes and CVD, as well as BP and lipid levels. | IVR+ and IVR interventions increased adherence to statins and angiotensin-converting enzyme inhibitors/angiotensin receptor blockers (ACEIs/ARBs) compared with usual care (1.6 to 3.7 percentage points). Adherence to ACEIs/ARBs was also significantly higher for IVR+ relative to IVR participants. Among statin users, IVR+ participants had significantly lower low-density lipoprotein (LDL) levels at follow-up compared with UC (Δ = −1.5; 95% CI, −2.7 to −0.2 mg/dL); this effect was seen mainly in those with baseline LDL levels >100 mg/dL (Δ = −3.6; 95% CI, −5.9 to −1.3 mg/dL). | A substantial number of participants were never reached by phone, thus diluting delivery and potentially the effectiveness of the IVR intervention. Indeed, the IVR+ intervention was designed largely in recognition of this limitation, although the incremental effect of the added IVR+ components was also small/ | Technology-based tools, in conjunction with an EMR, can improve adherence to chronic disease medications and measured cardiovascular disease risk factors. |
| Fang & Li, 2016 | China | RCT | 280 outpatients, including 200 men (71.42%) and 80 women (28.58%) ranging in age from 38 to 69 years. | mHealth technologies (short message service, short message service + Micro Letter, and phone). | 6 months | Study used the four-item dichotomous Morisky Medication Adherence Scale (MMAS) to assess drug compliance. | Results showed that the SMS and SMS + ML groups had better cumulative adherence (lower MMAS scores) after six months compared to the phone group. The SMS + ML group had better cumulative adherence (lower MMAS scores) after six months compared to the SMS group. | Study limitations are that it required access to a cellular data network, literacy, and the ability to use a smart phone. | Short message service and messaging applications, such as Micro Letter, are effective means of providing discharged patients with reminders and coronary artery disease-related health information. Implementation of a short message service + Micro Letter program can improve outpatient adherence to medication. The use of smart-phone communication technologies increased adherence to medications in patients with CAD. |
| Frederix et al., 2015 | Belgium | RCT | 140 (intervention group; n = 70) or to conventional cardiac rehabilitation alone (control group; n = 70) | Internet based, patient-tailored telerehabilitation program with short message service (SMS) | 24 weeks | The primary outcome measure was peak aerobic capacity (VO2 peak), measured during maximal cardiopulmonary exercise testing with breath-by-breath gas exchange analysis at baseline and after 6 and 24 weeks (Jaeger MS-CPX). | Mean aerobic capacity increased significantly in intervention group patients (n = 69) from baseline (mean 22.46, SD 0.78 mL/[min*kg]) to 24 weeks (mean 24.46, SD 1.00 mL/[min*kg], p < 0.01) versus control group patients (n = 70), who did not change significantly (baseline: mean 22.72, SD 0.74 mL/[min*kg]; 24 weeks: mean 22.15, SD 0.77 mL/[min*kg], p = 0.09). Between-group analysis of aerobic capacity confirmed a significant difference between the intervention group and control group in favor of the intervention group (p < 0.001). At 24 weeks, self-reported physical activity improved more in the intervention group compared to the control group (p = 0.01) as did the global HRQL score (p = 0.01). | The telerehab was designed to recruit broad cardiac patient population but ended up with minority of patient participants, thus reducing the generalizability of the findings for the chronic heart failure patients. | Study showed that comprehensive tele rehabilitation program can lead to a bigger improvement in both physical fitness (VO2 peak) and associated health-related quality of life (HRQL) compared to center-based cardiac rehabilitation alone. |
| Blasco et al., 2012 | Spain | RCT | 203 | Patients randomized to the TMG were temporarily provided with an automatic sphygmomanometer, glucose lipid meter, and cellular phone. | 12 months | Outcome measures were resting BP, body mass index (BMI), smoking status, LDL-c, and glycated hemoglobin A1c (HbA1c), all measured at the initial and final visits for comparison. Smoking status was determined by self-report and confirmed by a 1-step cotinine immunoassay in urine | Telemonitoring (TMG) patients were more likely (RR 1.4; 95% CI 1.1–1.7) to experience improvement in cardiovascular risk factors profile than control patients (69.6% vs. 50.5%, p 0.010). TMG patients achieved treatment goals for BP (62.1% vs. 42.9%, p 0.012) and HbA1c (86.4% vs. 54.2%, p 0.018), with no differences in smoking cessation or LDL-c. Body mass index was significantly lower in TMG (0.77 kg/m2 vs. 0.29 kg/m2, p 0.005). | A telemonitoring program, via mobile phone messages, appears to be useful for improving the risk profile in acute coronary syndrome (ACS) survivors and can be an effective tool for secondary prevention, especially for overweight patients. | |
| Martin et al., 2015 | U.S.A, Marylland | RCT | 48 | Automated mHealth tracking technology (digital physical activity tracking was performed using the Fitbug Orb, a wearable, display-free, triaxial accelerometer that pairs with low-energy Bluetooth with compatible smartphones) linked with smart texting system | 6 months | The primary outcome measure was the mean change in accelerometer-measured daily step count assessed from baseline through phase I and II. | The phase I change in activity was non significantly higher in unblinded participants versus blinded controls by 1024 daily steps (95% confidence interval [CI], −580 to 2628; p = 0.21). In phase II, participants receiving texts increased their daily steps over those not receiving texts by 2534 (95% CI, 1318 to 3750; p < 0.001) and over blinded controls by 3376 (95% CI, 1951 to 4801; p < 0.001). | The study had a limited sample size, hence, it best interpreted as exploratory evidence rather or a pilot trial study. The study also used adult smartphone participants thus making its generalizability uncertain. | An automated tracking-texting intervention increased physical activity with, but not without, the texting component. In ambulatory cardiology patients who are smartphone users, a novel mHealth intervention coupling smart texts to digital tracking significantly increased near-term physical activity. |
| Tian et al., 2015 | China & India | RCT | 2086 | Android-powered app (Simplified Cardiovascular management Study; SimCard) | 12 months | The primary outcome was the net difference between groups in the change in the proportion of patient-reported antihypertensive medication use. The outcomes were assessed with data collected during baseline and post intervention surveys from all high-risk individuals in both intervention and control villages in a standardized manner. | In comparison with the control group, the intervention group had a 25.5% (p < 0.001) higher net increase in the primary outcome of the proportion of patient-reported antihypertensive medication use pre- and post-intervention. There were also significant differences in certain secondary outcomes: aspirin use (net difference: 17.1%; p < 0.001) and systolic blood pressure (–2.7 mm Hg; p = 0.04 | This study was not able to evaluate the effectiveness of different components or specific measures of the simplified cardiovascular management program, e.g., any given lifestyle modification or prescription of appropriate medication. Additionally, the imbalances of two baseline characteristics (history of coronary heart disease and history of diabetes mellitus) in India could have potentially affected the outcome assessment. | The results indicate that the simplified cardiovascular management program improved quality of primary care and clinical outcomes in resource-poor settings in China and India. Larger trials in more places are needed to ascertain the potential impacts on mortality and morbidity outcomes. |
| McGillicuddy et al., 2013 | U.S.A | RCT | 20 | Prototype mHealth technology (A smartphone enabled medication adherence and BP self-management system). The prototype mHealth system consisted of a wireless GSM electronic medication tray, a wireless Bluetooth-enabled BP monitor, and a smartphone. | 3 months | Medication adherence was examined using a 2 (treatment group: mHealth, SC) × 4 (time: pre-intervention, 1, 2, and 3 months) repeated measures analyses of variance (ANOVA). Resting BP was examined using a 2 (treatment group: mHealth, SC) by 4 (time: pre-intervention, 1, 2, and 3 months) repeated measures ANOVA. | Compared to the standard care control group (SC), the mHealth intervention group exhibited significant improvements in medication adherence and significant reductions in clinic-measured systolic blood pressures across the monthly evaluations. Physicians made more anti-hypertensive medication adjustments in the mHealth group versus the standard care group (7 adjustments in 5 patients versus 3 adjustments in 3 patients) during the 3-month trial based on the information provided in the weekly reports. | All the study subjects were recruited from a single transplant center which jeopardizes its generalizability. Besides, the randomly assigned groups differed significantly in age and adherence prior to the intervention raises questions about the validity of the conclusions. Finally, those who chose to participate in the mHealth-based RCT might be predisposed to a more positive attitude toward mHealth and thereby introduce a positive bias. | These data support the acceptability and feasibility of the prototype mHealth system. Further trials with larger sample sizes and additional biomarkers (e.g., whole blood medication levels) are needed to examine efficacy and effectiveness of the system for improving medication adherence and blood pressure control after kidney transplantation over longer time periods. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quazi, S.; Malik, J.A. RETRACTED: A Systematic Review of Personalized Health Applications through Human–Computer Interactions (HCI) on Cardiovascular Health Optimization. J. Cardiovasc. Dev. Dis. 2022, 9, 273. https://doi.org/10.3390/jcdd9080273
Quazi S, Malik JA. RETRACTED: A Systematic Review of Personalized Health Applications through Human–Computer Interactions (HCI) on Cardiovascular Health Optimization. Journal of Cardiovascular Development and Disease. 2022; 9(8):273. https://doi.org/10.3390/jcdd9080273
Chicago/Turabian StyleQuazi, Sameer, and Javid Ahmad Malik. 2022. "RETRACTED: A Systematic Review of Personalized Health Applications through Human–Computer Interactions (HCI) on Cardiovascular Health Optimization" Journal of Cardiovascular Development and Disease 9, no. 8: 273. https://doi.org/10.3390/jcdd9080273
APA StyleQuazi, S., & Malik, J. A. (2022). RETRACTED: A Systematic Review of Personalized Health Applications through Human–Computer Interactions (HCI) on Cardiovascular Health Optimization. Journal of Cardiovascular Development and Disease, 9(8), 273. https://doi.org/10.3390/jcdd9080273






