Effectiveness of High-Intensity Interval Training and Continuous Moderate-Intensity Training on Blood Pressure in Physically Inactive Pre-Hypertensive Young Adults
Abstract
:1. Introduction
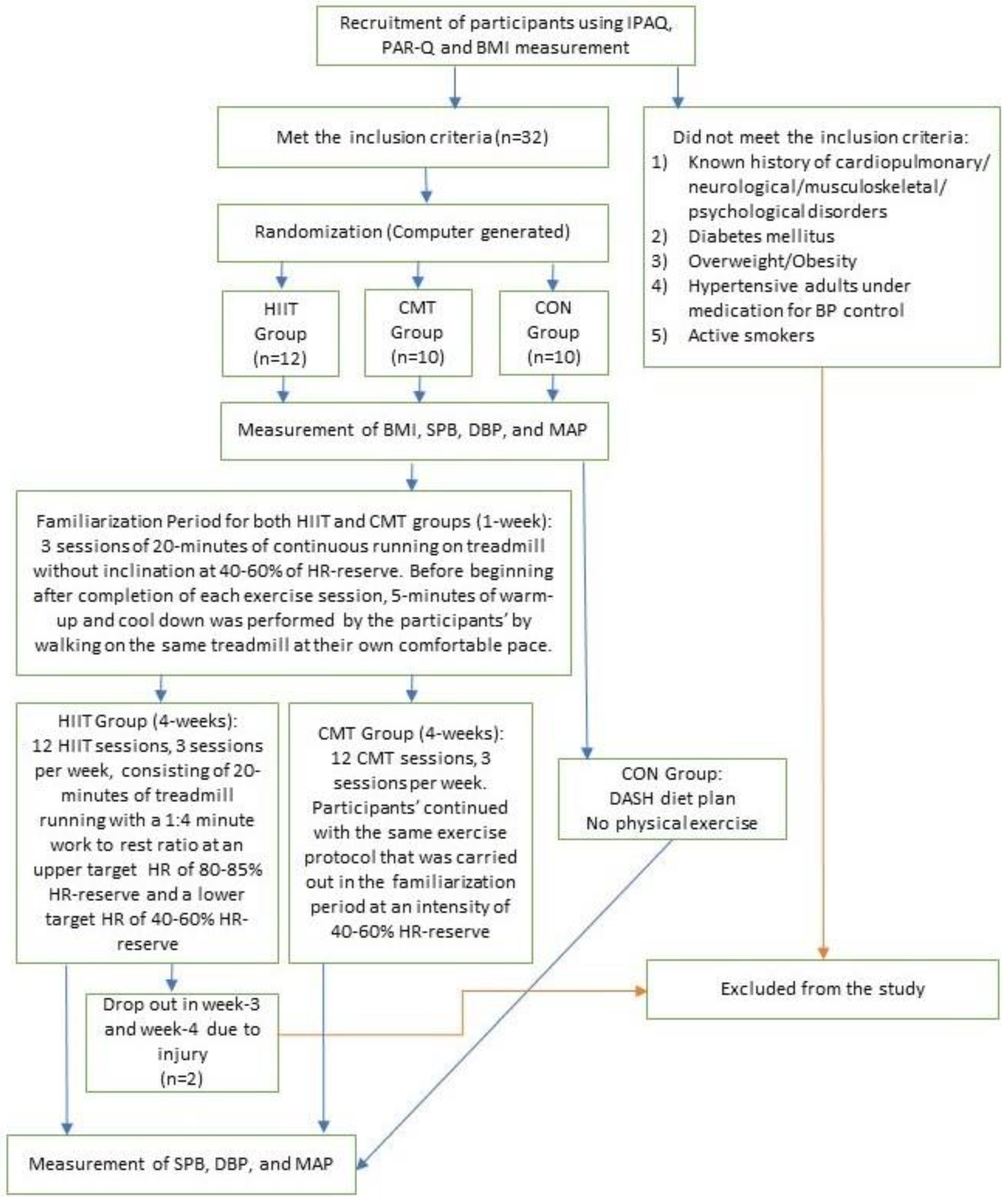
2. Materials and Methods
2.1. Study Setting and Subjects
2.2. Body Mass Index and Blood Pressure Measurement
2.3. Exercise Intervention Protocol
2.4. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Comparison within the Groups
3.3. Comparison between the Groups
4. Discussion
5. Strengths, Limitations and Recommendations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chow, C.K.; Teo, K.K.; Rangarajan, S.; Islam, S.; Gupta, R.; Avezum, A.; Bahonar, A.; Chifamba, J.; Dagenais, G.; Diaz, R.; et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013, 310, 959–968. [Google Scholar] [CrossRef] [Green Version]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; Ferranti, S.; Després, J.P.; Fullerton, H.J.; et al. Executive summary: Heart disease and stroke statistics-2016 update: A report from the american heart association. Circulation 2016, 133, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr.; et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The jnc 7 report. JAMA 2003, 289, 2560–2571. [Google Scholar] [CrossRef] [PubMed]
- Vasan, R.S.; Larson, M.G.; Leip, E.P.; Evans, J.C.; O’Donnell, C.J.; Kannel, W.B.; Levy, D. Impact of high-normal blood pressure on the risk of cardiovascular disease. N. Engl. J. Med. 2001, 345, 1291–1297. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Whelton, P.K.; Appel, L.J.; Charleston, J.; Klag, M.J. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension 2000, 35, 544–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nytrøen, K.l.; Rolid, K.; Andreassen, A.K.; Yardley, M.; Gude, E.; Dahle, D.O.; Bjørkelund, E.; Relbo, A.; Grov, I.; Philip, W.J.; et al. Effect of high-intensity interval training in de novo heart transplant recipients in Scandinavia: One-year follow-up of the HITTS randomized, controlled study. Circulation 2019, 139, 2198–2211. [Google Scholar] [CrossRef]
- Silva, M.I.C.; Mostarda, C.T.; Moreira, E.D.; Silva, K.A.S.; Santos, F.; Angelis, K.; Farah, V.M.A.; Irigoyen, M.C. Preventive role of exercise training in autonomic, hemodynamic and metabolic parameters in rats under high risk of metabolic syndrome development. J. Appl. Physiol. 2013, 114, 786–791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Araujo, A.J.S.D.; Santos, A.C.V.D.; Souza, K.D.S.; Aires, M.B.; Filho, V.J.S.; Fioretto, E.T.; Mota, M.M.; Santos, M.R.V. Resistance training controls arterial blood pressure in rats with l-name-induced hypertension. Arq. Bras. Cardiol. 2013, 100, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Bell, T.P.; McIntyre, K.A.; Hadley, R. Effect of long-term physical exercise on blood pressure in african americans. Int. J. Exerc. Sci. 2014, 7, 3. [Google Scholar] [CrossRef] [Green Version]
- Diaz, K.M.; Shimbo, D. Physical Activity and the Prevention of Hypertension. Curr. Hypertens. Rep. 2013, 15, 659–668. [Google Scholar] [CrossRef] [Green Version]
- Cornelissen, V.A.; Smart, N.A. Exercise Training for Blood Pressure: A Systematic Review and Meta-analysis. J. Am. Heart Assoc. 2013, 2, e004473. [Google Scholar] [CrossRef] [Green Version]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the american college of sports medicine and the american heart association. Circulation 2007, 116, 1081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hambrecht, R.; Fiehn, E.; Weigl, C.; Gielen, S.; Hamann, C.; Kaiser, R.; Yu, J.; Adams, V.; Niebauer, J.; Schuler, G. Regular physical exercise corrects endothelial dysfunction and improves exercise capacity in patients with chronic heart failure. Circulation 1998, 24, 2709–2715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guimarães, G.V.; Ciolac, E.G.; Carvalho, V.O.; D’Avila, V.M.; Bortolotto, L.A.; Bocchi, E.A. Effects of continuous vs. Interval exercise training on blood pressure and arterial stiffness in treated hypertension. Hypertens. Res. 2010, 33, 627. [Google Scholar] [CrossRef]
- Ciolac, E.G.; Bocchi, E.A.; Bortolotto, L.A.; Carvalho, V.O.; Greve, J.; Guimaraes, G.V. Effects of high-intensity aerobic interval training vs. Moderate exercise on hemodynamic, metabolic and neuro-humoral abnormalities of young normotensive women at high familial risk for hypertension. Hypertens. Res. 2010, 33, 836. [Google Scholar] [CrossRef]
- Ciolac, E.G.; Bocchi, E.A.; Greve, J.M.; Guimarães, G.V. Heart rate response to exercise and cardiorespiratory fitness of young women at high familial risk for hypertension: Effects of interval vs continuous training. Eur. J. Cardiovasc. Prev. Rehabil. 2011, 18, 824–830. [Google Scholar] [CrossRef]
- Tjønna, A.E.; Lee, S.J.; Rognmo, Ø.; Stølen, T.O.; Bye, A.; Haram, P.M.; Loennechen, J.P.; Al-Share, Q.Y.; Skogvoll, E.; Slørdahl, S.A.; et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: A pilot study. Circulation 2008, 118, 346–354. [Google Scholar] [CrossRef] [Green Version]
- Ciolac, E.G.; Guimarães, G.V.; Bortolotto, L.A.; Doria, E.L.; Bocchi, E.A. Acute effects of continuous and interval aerobic exercise on 24-h ambulatory blood pressure in long-term treated hypertensive patients. Int. J. Cardiol. 2009, 133, 381–387. [Google Scholar] [CrossRef]
- Pescatello, L.M.; Franclin, B.A.; Fagard, R.; Faqquhar, W.B. Exercise and hypertension. Med. Sci. Sports Exerc. 2004, 36, 533–553. [Google Scholar] [CrossRef] [PubMed]
- Guiraud, T.; Nigam, A.; Gremeaux, V.; Meyer, P.; Juneau, M.; Bosquet, L. High-intensity interval training in cardiac rehabilitation. Sports Med. 2012, 42, 587–605. [Google Scholar] [CrossRef] [PubMed]
- Gillen, J.B.; Gibala, M.J. Is high-intensity interval training a time-efficient exercise strategy to improve health and fitness? Appl. Physiol. Nutr. Metab. 2013, 39, 409–412. [Google Scholar] [CrossRef] [PubMed]
- Helgerud, J.; Hoydal, K.; Wang, E.; Karlsen, T.; Berg, P.; Bjerkaas, M.; Simonsen, T.; Helgesen, C.; Hjorth, N.; Bach, R.; et al. Aerobic high-intensity intervals improve v o2max more than moderate training. Med. Sci. Sports Exerc. 2007, 39, 665–671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wisløff, U.; Støylen, A.; Loennechen, J.P.; Bruvold, M.; Rognmo, Ø.; Haram, P.M.; Tjønna, A.E.; Helgerud, J.; Slørdahl, S.A.; Lee, S.J.; et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: A randomized study. Circulation 2007, 115, 3086–3094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costa, E.C.; Hay, J.L.; Kehler, D.S.; Boreskie, K.F.; Arora, R.C.; Umpierre, D.; Szwajcer, A.; Duhamel, T.A. Effects of high-intensity interval training versus moderate-intensity continuous training on blood pressure in adults with pre-to established hypertension: A systematic review and meta-analysis of randomized trials. Sports Med. 2018, 48, 2127–2142. [Google Scholar] [CrossRef] [PubMed]
- Cicolini, G.; Pizzi, C.; Palma, E.; Bucci, M.; Schioppa, F.; Mezzetti, A.; Manzoli, L. Differences in blood pressure by body position (supine, Fowler’s, and sitting) in hypertensive subjects. Am. J. Hypertens. 2011, 24, 1073–1079. [Google Scholar] [CrossRef] [PubMed]
- Manzoli, L.; Simonetti, V.; D’Errico, M.M.; De Vito, C.; Flacco, M.E.; Forni, C.; La Torre, G.; Liguori, G.; Messina, G.; Mezzetti, A.; et al. (In) accuracy of blood pressure measurement in 14 Italian hospitals. J. Hypertens. 2012, 30, 1955–1960. [Google Scholar] [CrossRef] [Green Version]
- Silva, B.N.C.; Petrella, A.F.; Christopher, N.; Marriott, C.F.; Gill, D.P.; Owen, A.M.; Petrella, R.J. The benefits of high-intensity interval training on cognition and blood pressure in older adults with hypertension and subjective cognitive decline: Results from the heart & mind study. Front. Aging. Neurosci. 2021, 13, 643809. [Google Scholar]
- Keteyian, S.J.; Hibner, B.A.; Bronsteen, K.; Kerrigan, D.; Aldred, H.A.; Reasons, L.M.; Saval, M.A.; Brawner, C.A.; Schairer, J.R.; Thompson, T.M. Greater improvement in cardiorespiratory fitness using higher-intensity interval training in the standard cardiac rehabilitation setting. J. Cardiopulm. Rehabil. Prev. 2014, 34, 98–105. [Google Scholar] [CrossRef]
- Nasi, M.; Patrizi, G.; Pizzi, C.; Landolfo, M.; Boriani, G.; Dei Cas, A.; Cicero, A.F.; Fogacci, F.; Rapezzi, C.; Sisca, G. The role of physical activity in individuals with cardiovascular risk factors: An opinion paper from Italian Society of Cardiology-Emilia Romagna-Marche and SIC-Sport. J. Cardiovasc. Med. 2019, 20, 631–639. [Google Scholar] [CrossRef]
- Facioli, T.D.P.; Buranello, M.C.; Regueiro, E.M.G.; Basso-Vanelli, R.P.; Durand, M.D.T. Effect of physical training on nitric oxide levels in patients with arterial hypertension: An integrative review. Int. J. Cardiovasc. Sci. 2021, 35, 253–264. [Google Scholar] [CrossRef]
- Lamina, S. Effects of continuous and interval training programs in the management of hypertension: A randomized controlled trial. J. Clin. Hypertens. 2010, 12, 841–849. [Google Scholar] [CrossRef] [PubMed]
- Punia, S.; Kulandaivelan, S.; Singh, V.; Punia, V. Effect of aerobic exercise training on blood pressure in indians: Systematic review. Int. J. Chronic Dis. 2016. [Google Scholar] [CrossRef] [Green Version]
- Leal, J.M.; Galliano, L.M.; Del Vecchio, F.B. Effectiveness of high-intensity interval training versus moderate-intensity continuous training in hypertensive patients: A systematic review and meta-analysis. Curr. Hypertens. Rep. 2020, 22, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Olea, M.A.; Mancilla, R.; Martínez, S.; Díaz, E. Effects of high intensity interval training on blood pressure in hypertensive subjects. Rev. Med. Chil. 2017, 145, 1154–1159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skutnik, B.C.; Smith, J.R.; Johnson, A.M.; Kurti, S.P.; Harms, C.A. The effect of low volume interval training on resting blood pressure in pre-hypertensive subjects: A preliminary study. Phys. Sportsmed. 2016, 44, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Skutnik, B.C. The Effects of High Intensity Interval Training on Resting Mean Arterial Pressure and C-Reactive Protein Content in Prehypertensive Subjects. Ph.D. Thesis, Kansas State University, Manhattan, KS, USA, 2013. [Google Scholar]
- Grace, F.; Herbert, P.; Elliott, A.D.; Richards, J.; Beaumont, A.; Sculthorpe, N.F. High intensity interval training (HIIT) improves resting blood pressure, metabolic (MET) capacity and heart rate reserve without compromising cardiac function in sedentary aging men. Exp. Gerontol. 2018, 109, 75–81. [Google Scholar] [CrossRef]
- Muth, B.J. Cardiovascular Effects of High-Intensity Interval Training and Moderate-Intensity Continuous Training in Sedentary Individuals. Ph.D. Thesis, University of Delaware, Newark, DE, USA, 2018. [Google Scholar]
- García-Hermoso, A.; Cerrillo-Urbina, A.J.; Herrera-Valenzuela, T.; Cristi-Montero, C.; Saavedra, J.M.; Martínez-Vizcaíno, V. Is high-intensity interval training more effective on improving cardiometabolic risk and aerobic capacity than other forms of exercise in overweight and obese youth? A meta-analysis. Obes. Rev. 2016, 17, 531–540. [Google Scholar] [CrossRef]
- Wahl, P.; Jansen, F.; Achtzehn, S.; Schmitz, T.; Bloch, W.; Mester, J.; Werner, N. Effects of high intensity training and high volume training on endothelial microparticles and angiogenic growth factors. PLoS ONE 2014, 9, e96024. [Google Scholar] [CrossRef] [Green Version]
- Juraschek, S.P.; Miller, E.R.; Weaver, C.M.; Appel, L.J. Effects of Sodium Reduction and the DASH Diet in Relation to Baseline Blood Pressure. Randomized Controlled Trial. J. Am. Coll. Cardiol. 2017, 70, 2841–2848. [Google Scholar] [CrossRef]
- Paula, T.P.; Viana, L.V.; Neto, A.T.; Leitao, C.B.; Gross, J.L.; Azevedo, M.J. Effects of the DASH Diet and Walking on Blood Pressure in Patients with Type 2 Diabetes and Uncontrolled Hypertension: A Randomized Controlled Trial. J. Clin. Hypertens. 2015, 17, 895–901. [Google Scholar] [CrossRef] [PubMed]
- Filippou, C.D.; Tsioufis, C.P.; Thomopoulos, C.G.; Mihas, C.C.; Dimitriadis, K.S.; Sotiropoulou, L.I.; Chrysochoou, C.A.; Nihoyannopoulos, P.I.; Tousoulis, D.M. Dietary Approaches to Stop Hypertension (DASH) Diet and Blood Pressure Reduction in Adults with and without Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2020, 11, 1150–1160. [Google Scholar] [CrossRef] [PubMed]
| Group | Statistic | p-Value | |
|---|---|---|---|
| Pre-SBP mean | HIIT Group | 0.960 | 0.780 |
| CMT Group | 0.981 | 0.972 | |
| CON Group | 0.853 | 0.063 | |
| Pre-DBP mean | HIIT Group | 0.970 | 0.890 |
| CMT Group | 0.912 | 0.294 | |
| CON Group | 0.874 | 0.112 | |
| Pre-MAP mean | HIIT Group | 0.989 | 0.995 |
| CMT Group | 0.921 | 0.365 | |
| CON Group | 0.923 | 0.387 |
| HIIT Group X ± SD | CMT Group X ± SD | CON Group X ± SD | ||||
|---|---|---|---|---|---|---|
| Pre-Test | Post-Test | Pre-Test | Post-Test | Pre-Test | Post-Test | |
| SBP (mmHg) | 122.76 ± 2.65 | 119 ± 3.91 | 125.23 ± 3.76 | 123.67 ± 3.98 | 127.93 ± 5.09 | 128.37 ± 5.32 |
| DBP (mmHg) | 78.57 ± 5.36 | 75.63 ± 4.86 | 77.23 ± 4.54 | 75.73 ± 4.26 | 74.00 ± 6.23 | 73.60 ± 5.78 |
| MAP (mmHg) | 93.14 ± 3.46 | 90.09 ± 2.57 | 93.20 ± 2.89 | 91.71 ± 3.08 | 91.98 ± 4.62 | 91.86 ± 4.18 |
| Paired Differences | ||||||
|---|---|---|---|---|---|---|
| Groups | Mean | Std. Deviation | t | df | p-Value | |
| CON Group | ||||||
| Pair 1 | Pre-SBP mean–post-SBP mean | −0.43 | 3.68 | −0.37 | 9 | 0.718 |
| Pair 2 | Pre-DBP mean–post-DBP mean | 0.40 | 3.35 | 0.38 | 9 | 0.714 |
| Pair 3 | Pre-MAP mean–post-MAP mean | 0.11 | 2.50 | 0.14 | 9 | 0.892 |
| CMT Group | ||||||
| Pair 1 | Pre-SBP mean–post-SBP mean | 1.57 | 1.54 | 3.22 | 9 | 0.011 |
| Pair 2 | Pre-DBP mean–post-DBP mean | 1.50 | 3.10 | 1.53 | 9 | 0.161 |
| Pair 3 | Pre-MAP mean–post-MAP mean | 1.49 | 2.12 | 2.22 | 9 | 0.054 |
| HIIT Group | ||||||
| Pair 1 | Pre-SBP mean–post-SBP mean | 3.76 | 2.83 | 4.20 | 9 | 0.002 |
| Pair 2 | Pre-DBP mean–post-DBP mean | 2.93 | 2.23 | 4.16 | 9 | 0.002 |
| Pair 3 | Pre-MAP mean–post-MAP mean | 3.05 | 1.64 | 5.90 * | 9 | <0.0005 |
| ANOVA | ||||||
|---|---|---|---|---|---|---|
| Sum of Squares | df | Mean Square | F | p-Value | ||
| SBP | Between Groups | 69.72 | 2 | 34.86 | 5.02 * | 0.014 |
| Within Groups | 187.53 | 27 | 6.95 | |||
| Total | 257.25 | 29 | ||||
| DBP | Between Groups | 32.25 | 2 | 16.12 | 1.87 | 0.173 |
| Within Groups | 232.47 | 27 | 8.61 | |||
| Total | 264.71 | 29 | ||||
| MAP | Between Groups | 43.08 | 2 | 21.54 | 4.76 * | 0.017 |
| Within Groups | 122.13 | 27 | 4.52 | |||
| Total | 165.21 | 29 | ||||
| Dependent Variable | (I) Group | (J) Group | Mean Difference (I-J) | p-Value |
|---|---|---|---|---|
| SBP | HIIT | CMT | −1.83 | 0.282 |
| CON | −3.73 * | 0.010 | ||
| CMT | HIIT | 1.83 | 0.282 | |
| CON | −1.90 | 0.258 | ||
| CON | HIIT | 3.73 * | 0.010 | |
| CMT | 1.90 | 0.258 | ||
| MAP | HIIT | CT | −1.57 | 0.244 |
| CON | −2.93 * | 0.013 | ||
| CMT | HIIT | 1.56 | 0.244 | |
| CON | −1.37 | 0.337 | ||
| CON | HIIT | 2.93 * | 0.013 | |
| CMT | 1.37 | 0.337 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
John, A.T.; Chowdhury, M.; Islam, M.R.; Mir, I.A.; Hasan, M.Z.; Chong, C.Y.; Humayra, S.; Higashi, Y. Effectiveness of High-Intensity Interval Training and Continuous Moderate-Intensity Training on Blood Pressure in Physically Inactive Pre-Hypertensive Young Adults. J. Cardiovasc. Dev. Dis. 2022, 9, 246. https://doi.org/10.3390/jcdd9080246
John AT, Chowdhury M, Islam MR, Mir IA, Hasan MZ, Chong CY, Humayra S, Higashi Y. Effectiveness of High-Intensity Interval Training and Continuous Moderate-Intensity Training on Blood Pressure in Physically Inactive Pre-Hypertensive Young Adults. Journal of Cardiovascular Development and Disease. 2022; 9(8):246. https://doi.org/10.3390/jcdd9080246
Chicago/Turabian StyleJohn, Anil T, Moniruddin Chowdhury, Md. Rabiul Islam, Imtiyaz Ali Mir, Md Zobaer Hasan, Chao Yi Chong, Syeda Humayra, and Yukihito Higashi. 2022. "Effectiveness of High-Intensity Interval Training and Continuous Moderate-Intensity Training on Blood Pressure in Physically Inactive Pre-Hypertensive Young Adults" Journal of Cardiovascular Development and Disease 9, no. 8: 246. https://doi.org/10.3390/jcdd9080246
APA StyleJohn, A. T., Chowdhury, M., Islam, M. R., Mir, I. A., Hasan, M. Z., Chong, C. Y., Humayra, S., & Higashi, Y. (2022). Effectiveness of High-Intensity Interval Training and Continuous Moderate-Intensity Training on Blood Pressure in Physically Inactive Pre-Hypertensive Young Adults. Journal of Cardiovascular Development and Disease, 9(8), 246. https://doi.org/10.3390/jcdd9080246






