Abstract
Loperamide is a synthetic opioid commonly used as an antidiarrheal due to its activation of u-opioid receptors in the myenteric plexus. In therapeutic doses, it inhibits peristalsis and has anti-secretory and anti-motility effects, until metabolized by intestinal and hepatic CYP3A4 and CYP2C8 into inactive metabolites. Furthermore, loperamide also inhibits L-type voltage-gated calcium (Ca2+) channels, increases action potential duration, and can induce arrhythmias and even cardiotoxicity, particularly when taken in extremely high doses. Thus, the aim of this study was to perform an integrative review of the available evidence in the recent literature on the cardiac risks of acute and chronic use of loperamide. In electrocardiogram (ECG) analysis, the most common finding was QTc prolongation in 27 cases, followed by QRS prolongation, first-degree atrioventricular (AV) block, torsades de pointes, ventricular tachycardia, and right bundle branch block. As for the symptoms encountered, syncope, weakness, palpitations, lightheadedness, shortness of breath, nausea, vomiting, bradycardia, and cardiac arrest were the most common. Loperamide can inhibit hERG voltage-gated potassium (K+) channels (Kv11.1), leading to the prolongation of repolarization, QTc interval prolongation, and increased risk of torsades de pointes. In addition, loperamide can inhibit voltage-gated sodium (Na+) channels (Nav1.5), impairing electrical cardiac conduction and potentiating QRS interval widening. Therefore, QTc prolongation, torsades de pointes, and other ECG alterations are of particular concern regarding loperamide toxicity, particularly when overdosed.
1. Introduction
Loperamide is a synthetic opioid commonly used as an antidiarrheal. Its main therapeutic effects result from the activation of µ-opioid receptors in the myenteric plexus, until it is metabolized by intestinal and hepatic CYP3A4 and CYP2C8 into inactive metabolites. In therapeutic doses, it also inhibits peristalsis and has anti-secretory and anti-motility effects [1]. Loperamide is a substrate of P-glycoprotein-mediated efflux, which explains its low net penetration of the blood–brain barrier. Consequently, loperamide does not produce analgesia, euphoria, or respiratory depression at doses ≤ 16 mg/day, and it is classified as a drug with low abuse potential [2]; however, when ingested in high doses, loperamide crosses the blood–brain barrier due to P-Glycoprotein saturation and may produce euphoria and analgesia, which can lead to drug abuse [1].
It was previously shown that loperamide is a blocker of cardiac hERG voltage-gated potassium (K+) channels (Kv11.1) and Nav1.5. Blockade of cardiac Kv11.1 channels is commonly associated with drug-induced QT interval prolongation, whereas the blockade of cardiac Nav1.5 channels leads to QRS interval widening. In addition, loperamide also blocks L-type voltage-activated Ca2+ channels, increases action potential duration, and can induce other arrhythmias [3] and even cardiotoxicity in extremely high doses [2].
In 2016, the U.S. Food and Drug Administration (FDA) warned about the risk of QT interval prolongation, torsades de pointes arrhythmia, and cardiac arrest at higher-than-recommended doses [1]. Since then, new reports of potential cardiac complications of loperamide use have appeared in the scientific literature. Thus, the aim of this study was to analyze the available evidence in the recent literature on the cardiac risks of the acute and chronic use of loperamide.
2. Materials and Methods
The study is an integrative review of the literature performed according to Toronto, C. and Remington, R. (2020) about the risk of arrhythmias and cardiac lesions with the acute or chronic use of loperamide [4]. The research was carried out in the PubMed, Embase, Scopus, and BVS databases. Articles in Portuguese, English, or Spanish between 2018 and 2022 were included. The descriptors searched were ‘loperamide’, ’ECG’, ‘EKG’, ‘loperamide abuse’, and ‘cardiotoxicity’. A total of 190 research papers were found, of which 118 were non-duplicates. After evaluation by title, 59 potentially relevant papers were considered. Of these, after a new evaluation of the abstracts, 13 could not be obtained in full and were excluded, and 46 were considered. The 46 papers were read in full, and, of these, 29 relevant papers were selected to compose the final sample for this study.
3. Eligibility Criteria
Only original case reports of cardiac toxicity or cardiac arrhythmias after loperamide abuse, overuse, or chronic use were included. An irrelevant study was defined as a non-case report, such as commentaries or letters to the editor.
Articles that had no mention in their title of the use of loperamide or mentioned abuse of other opioids and drugs in general, management of diarrhea with no mention of loperamide abuse, and clinical studies in animals were excluded.
During the selection by abstract, animal studies, letters to the editor, case reports in which more than one type of opioid was abused in addition to loperamide, articles that only mentioned loperamide but not the abuse of the drug, and articles that were not found in the media were discarded. We included articles that mentioned management after loperamide abuse, case reports of loperamide abuse in humans, loperamide cardiotoxicity, and syndromes diagnosed after loperamide abuse.
Finally, the selection of full articles included only case reports that mentioned changes in electrocardiogram after abuse of loperamide in humans; articles in which abuse of more than one type of opioid was reported were excluded. Previous cardiovascular disease or other comorbidities were not considered as exclusion or inclusion criteria.
4. Selection Process
The study was conducted by two reviewers who analyzed the initial sample separately, applying the same filters and inclusion and exclusion criteria, and both reached the same final sample.
For the analysis, Microsoft Excel was used to organize the articles to generate a table from the databases by applying the filters: selected descriptors and articles published in the last 5 years. All selection was performed manually by the reviewers without associated tools.
Provided the sample of this study, we extracted the author, year of publication, age, dose of ingested loperamide, symptoms/signs, ECG results, treatment, and clinical outcome (Figure 1).
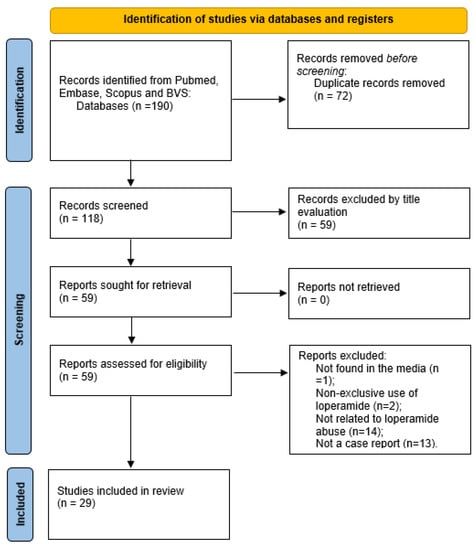
Figure 1.
Flow chart of the selection process for case reports of cardiac lesions with the acute or chronic use of loperamide.
5. Results
This article reviewed a total of 29 cases of intentional abuse or non-intentional misuse of loperamide. Fourteen patients (48%) were male and fifteen (52%) were female. Their ages ranged from 14 to 49 years old; the mean age was 31.5 years (30 years among males; 33 years among females).
Table 1 details all male cases; the dose of ingested loperamide ranged from 20 to 600 mg; the mean dose was 181.5 mg. One case did not report a loperamide dose. The most common symptom was syncope in six cases (43%); weakness was observed in 23% of patients; other common symptoms were cardiac arrest, lightheadedness, nausea and vomiting, shortness of breath and abdominal pain (15% of cases); palpitations, dizziness, and tonic–clonic seizures (8% of cases).

Table 1.
Male cases.
Most ECG analyses of males (93%) showed QTc and QRS elevation. QTc ranged from 500 to 800 ms; the mean interval was 632 ms. QRS was included in eight cases, in which it was found to be elevated, between 136 and 170 ms. In two cases, ST elevation was seen, consistent with type 1 Brugada patterns. Other alterations included AV block with sinus bradycardia; ventricular arrhythmias and ventricular tachycardia; and torsades de pointes (each in 15% of cases).
In 50% of cases, ECGs returned to normal in 3–5 days after treatment. A diagnosis of Brugada syndrome was made in two cases, one of which was secondary to loperamide abuse.
Table 2 details female cases. The dose of ingested loperamide ranged from 12 mg to 600 mg; the mean dose was 205.56 mg, and one case did not report the loperamide dose ingested. The most common symptoms were syncope (44%) and palpitations (25%). Other symptoms included: bradycardia (19%); dyspnea (19%); arrhythmia (13%); generalized weakness (13%); and, less commonly, hypoxia; hypertension; atypical chest pain; shortness of breath; hypotension; tachycardia; bradypnea; hypoglycemia; light-headedness; and loss of consciousness.

Table 2.
Female cases.
All ECGs of female patients showed QTc elevation in the 425–831 ms range; the mean interval was 621 ms. QRS was included in six cases, in which it was found to be elevated, between 142 and 270 ms. In 25% of cases, there was first-degree AV block; in 19%, torsades de pointes; in 13%, prolonged PR interval; and in 13%, ST elevation. In seven cases, ECGs returned to normal in 1–3 days after the treatment.
Considering all cases in both tables, 13 cases (50%) ingested more than 200 mg of loperamide, and 13 cases (50%) ingested less than 200 mg; one case reported ingestion of 96 to 320 mg, and two cases (6.9%) did not report a loperamide dose. The most common ECG alterations were QTc prolongation in 27 cases (93%), followed by QRS prolongation in 12 cases (41%); first-degree AV block in 6 cases (20%); torsades de pointes in 5 cases (17%); ventricular tachycardia and right bundle branch block in 3 cases each (10%); idioventricular rhythm, prolonged PR, and inverted T waves, each in 2 cases (6.8%); and tachycardia, sinus tachycardia, S3 gallop, and ventricular fibrillation in 1 case each (3.4%).
As for the symptoms encountered, there were 13 cases (44%) with syncope, 5 cases (17%) with weakness, 5 cases (17%) with palpitations, 4 cases (13%) with lightheadedness, and 4 cases (13%) with shortness of breath. Nausea, vomiting, and bradycardia were present in three cases (10%). Cardiac arrest was present in two cases (6.8%), as were tachycardia, arrhythmia, and abdominal pain. Diaphoresis, constipation, hypothermia, bradypnea, hypoglycemia, hypotension, chest pain, hypertension, dyspnea, itching, confusion, loss of consciousness, gastrointestinal symptoms, hypoxia, and lethargy were present in one case each (3.4%), and one case occurred in which no symptom was recorded.
The most common treatments in both tables were magnesium sulfate, given in 15 cases (52%) and sodium bicarbonate, given in 8 cases (28%). Isoproterenol was utilized in five cases (17%). Lidocaine was administered in three cases (10%) and amiodarone in four cases (14%). Betamethasone, furosemide, nitroglycerin, NIPPV, potassium replacement, supportive care, metoprolol, naloxone, N-acetylcysteine infusion, dextrose, atropine, dopamine, norepinephrine, hydration, cardiac monitor, inotropic support, loop recorder, cardioconversion, acetaminophen, morphine, lorazepam, and ondansetron were each used in only one case.
Analyzing the outcomes, in 16 cases (55%), the ECG returned to normal; 4 cases (13%) had torsades de pointes; in 3 cases (13%), isoproterenol was used; 3 cases (13%) were put in a temporary pacemaker; 2 cases (6.8%) cases occurred with Brugada syndrome; and in 2 cases (6.8%), electrical cardioversions were performed. A holter was placed in one case (3.4%); buprenorphine–naloxone or buprenorphine was also administered in one case (3.4%) each. Hypoxia-related brain injury was reported in one case (3.4%), as well as resolution of tachycardia and bradycardia, cardiopulmonary resuscitation, and monitoring for 72 h. In other cases, there were: recommended follow-ups with a cardiologist (2 cases; 6.8%), a psychiatrist (1 case; 3.4%), and genetic testing (1 case; 3.4%). There was also a case in which the patient developed ventricular tachycardia and ventricular fibrillation.
6. Discussion
The mechanism of loperamide’s cardiotoxicity is currently unknown. The most likely related mechanism is the inhibition of voltage-gated sodium and potassium channels in cardiac cells. Nav1.5 channels are responsible for action potential amplitude, impulse conduction velocity, and successful propagation. Thus, since loperamide also blocks Nav1.5 channels, which may result in the impairment of electrical cardiac conduction, leading to the potentiation of QRS interval widening and Brugada patterns [5,6,7,10,19,32,33,34]. The blockade of Kv11.1 channels by loperamide results in the prolongation of repolarization that produces QTc interval prolongation and increases the risk of torsades de pointes. Repolarization delay leads to early after-depolarization, heterogeneous myocardial repolarization, and torsades de pointes caused by the inhibition of the delayed rectifier potassium current. QTc prolongation is a significant concern regarding loperamide toxicity [7,9,19].
Previous reports of loperamide toxicity show a broadening of the QRS complex and the prolongation of the QT interval in relation to the onset of cardiac arrhythmias such as tachycardias, polymorphic ventricular tachycardia, and sudden cardiac death. QRS and QTc prolongation was the most common cardiac alteration found in the study, followed by first-degree AV block with sinus bradycardia, ST elevation, torsades de pointes, and Brugada pattern [19,35]. Teigeler et al., 2019 [9] published the ECG demonstrated the polymorphic ventricular tachycardia, with prolonged QTc, after the abuse of loperamide.
Initially, patients should be evaluated for any reversible risk factors for QTc prolongation, such as electrolyte abnormalities such as hypokalemia and hypomagnesemia. For the treatment of loperamide-induced cardiotoxicity, each case must be individualized with its due comorbidities and changes; however, in an analysis of the 29 articles used as a basis for the work, the main treatment options can be listed according to their greater efficiency (without dosage specified in the articles): the IV infusion of magnesium sulfate, the IV infusion of sodium bicarbonate, IV lidocaine, IV amiodarone, and atropine. Torsades secondary to loperamide toxicity may not respond well to therapies with magnesium or sodium bicarbonate; thus, other agents such as atropine, amiodarone, lidocaine, and metoprolol might be necessary. Treatment may also require cardiac pacing, electrical cardioversion, or IV isoproterenol in some cases to achieve heart rate overdrive for arrhythmia control. When associated ventricular dysrhythmias occur, treatment with magnesium sulfate and sodium bicarbonate has been successful [19,33].
Furthermore, processes of decontamination, increased elimination, and the use of an antidote and supportive care might be considered in the treatment of loperamide-induced cardiotoxicity. Activated charcoal can be used for loperamide adsorption and decontamination, as it can considerably reduce loperamide concentrations due to reduced gastrointestinal smooth muscle motility. On the other hand, as of now, there are no effective evidence-based strategies to promote the elimination of loperamide [16]. Loperamide-induced cardiotoxicity is at least partially caused by the blockade of sodium channels. This likely explains why the administration of IV sodium bicarbonate may help attenuate arrhythmogenic effects of loperamide, such as QTc interval prolongation. Nevertheless, the use of sodium bicarbonate may itself cause concerning changes in serum potassium and magnesium concentrations.
There are no specific recommendations regarding patient life support, but general actions to be considered as possible supportive treatments for loperamide toxicity include defibrillation; the intravenous administration of magnesium sulfate, amiodarone, or lidocaine; and excessive stimulation. The half-life of loperamide is relatively long, between 9 and 30 h, and the electrical disturbances that lead to the onset of cardiac arrhythmias due to the actions of loperamide persist for several days [16]. The data on the use of magnesium sulfate in the treatment of cardiac arrhythmias are conflicting, as there is evidence to suggest that it is unlikely to result in decreased mortality when introduced either early or later in patients with fibrinolytic treatment or even in high doses, i.e., greater than 75 mmol. In addition, there may be an increased incidence of cardiovascular disorders, such as bradycardia, hypotension, and flushing [36,37]. However, there is also evidence to show that magnesium administration can reduce the incidence of major ventricular arrhythmias, such as ventricular fibrillation and ventricular tachycardia.
7. Conclusions
When overdosed, loperamide blocks cardiac sodium and potassium channels, resulting in a variety of cardiac rhythm abnormalities, such as QTc and QRS prolongation, first-degree AV block, torsades de pointes, ventricular tachycardia, and right bundle branch block.
Author Contributions
Conceptualization, B.C.L., G.H., M.O.T., A.C.-N. and F.S.M.-R.; methodology, B.C.L., G.H., A.C.-N. and F.S.M.-R.; formal analysis, B.C.L., G.H., L.A.D.N., J.V.R.M., F.S.T. and F.S.M.-R.; resources, M.O.T., R.Y.L., A.C.-N. and F.S.M.-R.; data curation, B.C.L. and G.H.; writing—original draft preparation, B.C.L., G.H., M.P.-O. and F.S.M.-R.; writing—review and editing, M.P.-O., L.A.D.N., J.V.R.M., F.S.T., R.Y.L., A.C.-N. and F.S.M.-R.; visualization, B.C.L. and G.H.; supervision, A.C.-N. and F.S.M.-R.; project administration, F.S.M.-R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ali, M.; Mujahid, A.; Bulathsinghala, C.P.; Surani, S. Cardiac Arrhythmia Secondary to Loperamide Abuse and Toxicity. Cureus 2020, 12, e6936. [Google Scholar] [CrossRef] [PubMed]
- Cicci, J.D.; Jagielski, S.M.; Clarke, M.M.; Rayson, R.A.; Cavender, M.A. Loperamide Overdose Causing Torsades de Pointes and Requiring Impella Temporary Mechanical Support: A Case Report. Eur. Heart J.-Case Rep. 2019, 3, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, A.; Bodar, V.; Malekzadegan, M.; Singh, S.; Frumkin, W.; Mangla, A.; Doshi, K. Loperamide Induced Life Threatening Ventricular Arrhythmia. Case Rep. Cardiol. 2016, 2016, 5040176. [Google Scholar] [CrossRef] [PubMed]
- Toronto, C.E.; Remington, R. A Step-By-Step Guide to Conducting an Integrative Review, 1st ed.; Springer International Publishing AG: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Sun, C.; Brice, J.A.; Clark, R.F. Brugada-Type Pattern on Electrocardiogram Associated with High-Dose Loperamide Abuse. J. Emerg. Med. 2018, 54, 484–486. [Google Scholar] [CrossRef] [PubMed]
- Stefek, B.; Wolfe, L.T.; Cohen, M. Brugada Syndrome Associated with Adolescent Loperamide Abuse. Pediatrics 2018, 142, e20181423. [Google Scholar] [CrossRef]
- Simon, M.; Rague, J. A Case Report of Torsade de Pointes and Brugada Pattern Associated with Loperamide Misuse and Supratherapeutic Loperamide Concentrations. J. Emerg. Med. 2021, 61, e54–e59. [Google Scholar] [CrossRef]
- Jablonski, S.; Cowgill, J.; Powers, J. Loperamide Cardiotoxicity: A Byproduct of the Opioid Epidemic; Maine Medical Center: Portland, ME, USA, 2019; Volume 1050, Available online: https://knowledgeconnection.mainehealth.org/mmc/1050 (accessed on 22 November 2022).
- Teigeler, T.; Stahura, H.; Alimohammad, R.; Kalahasty, G.; Koneru, J.N.; Ellenbogen, M.; Ellenbogen, K.A.; Padala, S.K. Electrocardiographic Changes in Loperamide Toxicity: Case Report and Review of Literature. J. Cardiovasc. Electrophysiol. 2019, 30, 2618–2626. [Google Scholar] [CrossRef]
- Kohli, U.; Altujjar, M.; Sharma, R.; Hassan, S. Wide Interindividual Variability in Cardiovascular Toxicity of Loperamide: A Case Report and Review of Literature. HeartRhythm Case Rep. 2019, 5, 221–224. [Google Scholar] [CrossRef]
- Escobedo, Y.; Wilson, G.; Costa, S.M.; Ellington, T. The Long-Lasting High: Cardiac Complications from Loperamide Toxicity’; White Medical Center: Dallas, TX, USA, 2020; Volume 2842. [Google Scholar] [CrossRef]
- Atoot, A.; Sholem, S.; Khaddash, I.; Zuberi, J. Transient Brugada Pattern Induced by Loperamide Abuse. Cureus 2020, 12, e8037. [Google Scholar] [CrossRef]
- Palkar, P.; Kothari, D. Bradycardia and Syncope in a Patient Presenting with Loperamide Abuse. Cureus 2018, 10, e2599. [Google Scholar] [CrossRef]
- Modi, V.; Krinock, M.; Desai, R.; Stevens, S.; Nanda, S. Loperamide-Induced Cardiac Events: Case Reports and Review. Cureus 2021, 13, e20744. [Google Scholar] [CrossRef] [PubMed]
- Larsen, T.R.; McMunn, J.; Ahmad, H.; AlMahameed, S.T. Ventricular Tachycardia Triggered by Loperamide and Famotidine Abuse. Drug Saf.-Case Rep. 2018, 5, 11. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, S.; Baig, M.A. A heart-wrenching case of loperamide toxicity. Asian Pac. J. Med. Toxicol. 2019, 8, 141–143. Available online: http://apjmt.mumsac.ir (accessed on 22 November 2022).
- Stone, B.; Zariwala, A.; Acho, M.; Barbash, I. Managing the Cardiotoxicity of Loperamide Overdose, an Emerging Issue in the Opioid Crisis. In C41. Critical Care Case Reports: Toxicology and Poisonings; American Thoracic Society: New York, NY, USA, 2019; p. 4809. [Google Scholar]
- Parker, B.M.; Rao, T.; Matta, A.; Quitanna, M.; Reynolds, H.N.; Stein, D.M.; Haase, D. Loperamide Induced Cardiac Arrhythmia Successfully Supported with Veno-Arterial ECMO (VA-ECMO), Molecular Adsorbent Recirculating System (MARS) and Continuous Renal Replacement Therapy (CRRT). Clin. Toxicol. 2019, 57, 1118–1122. [Google Scholar] [CrossRef] [PubMed]
- Isang, E.; Shali, L.; Morris, C.B.; Mahlow, J. Loperamide-Induced Torsades de Pointes. Cureus 2021, 13, e20299. [Google Scholar] [CrossRef] [PubMed]
- Kapaganti, S.; Anwar Ansari, S.; Saba, R.; Elkhouly, A.; Hassib, M. A Rare Case of Loperamide-Induced Cardiac Arrest. Cureus 2020, 12, e9396. [Google Scholar] [CrossRef]
- Whittaker, G.; Newman, J. Loperamide: An Emerging Drug of Abuse and Cause of Prolonged QTc. Clin. Med. 2021, 21, 150–152. [Google Scholar] [CrossRef]
- Rawala, M.S.; Gulati, R.; Rizvi, S. Cardiac Dysrhythmia Associated with Opioid Toxicity. Cureus 2020, 12, e8243. [Google Scholar] [CrossRef]
- De Vera, J.; Kim, H.B.; Sakr, A.E. A Case Report of Loperamide-Induced Ventricular Storm. J. Investig. Med. High Impact Case Rep. 2021, 9, 232470962199076. [Google Scholar] [CrossRef]
- Gaines, H.; Mao, T.; Murray, C.; Sivaram, C.A. The Twisted Truth: Identifying and Treating Torsade de Pointes (TDP) in Surreptitious Drug Use; University of Oklahoma Health Sciences Center: Oklahoma City, OK, USA, 2020; Volume 2819. [Google Scholar] [CrossRef]
- Rojas, S.F.; Oglat, A.; Bonilla, H.M.G.; Jeroudi, O.; Sharp, W.; Valderrábano, M.; Schurmann, P.A. Loperamide Mimicking Brugada Pattern. Methodist DeBakey Cardiovasc. J. 2018, 14, e1–e3. [Google Scholar] [CrossRef]
- Idris, A.; Mihora, D.C.; Kaye, K. Loperamide Abuse Cardiotoxicity. Should Loperamide Still Be an over the Counter Medication? Am. J. Emerg. Med. 2018, 36, 1716.e1–1716.e3. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.; Chitturi, K.R.; Hatcher, C.; Clewing, M.; Nagueh, S.F. Loperamide Toxicity Revealing Apical Hypertrophic Cardiomyopathy. Methodist DeBakey Cardiovasc. J. 2021, 17, 65. [Google Scholar] [CrossRef] [PubMed]
- Zaman, M.O.; Ali, M.U.; Finkel, J. A Case of Loperamide Induced Cardiac Syncope; Crozer Chester Medical Center: Springfield, PA, USA, 2018; Volume 2550. [Google Scholar] [CrossRef]
- Wang, A.; Nguyen, M.; Diaz, J.; Smith, T. Loperamide Toxicity Mimicking Peripartum Cardiomyopathy. Am. J. Emerg. Med. 2020, 38, 693.e5–693.e6. [Google Scholar] [CrossRef] [PubMed]
- Sapra, A.; Bhandari, P.; Gupta, S.; Kraleti, S.; Bahuva, R. A Rising Concern of Loperamide Abuse: A Case Report on Resulting Cardiac Complications. Cureus 2019, 11, e6314. [Google Scholar] [CrossRef]
- Myllymaki, A.; Westerbergh, J.; Carlsson, H.; Hoje, J. Torsade de pointes following repeated massive loperamide ingestions. Lakartidningen 2020, 117, FWWW. [Google Scholar] [PubMed]
- Lee, V.R.; Vera, A.; Alexander, A.; Ruck, B.; Nelson, L.S.; Wax, P.; Campleman, S.; Brent, J.; Calello, D.P. Loperamide Misuse to Avoid Opioid Withdrawal and to Achieve a Euphoric Effect: High Doses and High Risk. Clin. Toxicol. 2019, 57, 175–180. [Google Scholar] [CrossRef]
- Akel, T.; Bekheit, S. Loperamide Cardiotoxicity: A Brief Review. Ann. Noninvasive Electrocardiol. 2018, 23, e12505. [Google Scholar] [CrossRef]
- Riaz, I.B.; Khan, M.S.; Kamal, M.U.; Sipra, Q.-A.R.; Riaz, A.; Zahid, U.; Bhattacharjee, S. Cardiac Dysrhythmias Associated with Substitutive Use of Loperamide: A Systematic Review. Am. J. Ther. 2019, 26, e170–e182. [Google Scholar] [CrossRef]
- Wolfes, J.; Ellermann, C.; Burde, S.; Leitz, P.; Bögeholz, N.; Willy, K.; Fehr, M.; Reinke, F.; Eckardt, L.; Frommeyer, G. Divergent Electrophysiological Effects of Loperamide and Naloxone in a Sensitive Whole-Heart Model. Cardiovasc. Toxicol. 2021, 21, 248–254. [Google Scholar] [CrossRef]
- Li, J.; Zhang, Q.; Zhang, M.; Egger, M. Intravenous Magnesium for Acute Myocardial Infarction. Cochrane Database Syst. Rev. 2007, 2009, CD002755. [Google Scholar] [CrossRef]
- Ho, K.M.; Sheridan, D.J.; Paterson, T. Use of Intravenous Magnesium to Treat Acute Onset Atrial Fibrillation: A Meta-Analysis. Heart 2007, 93, 1433–1440. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).