Summation of Precordial R Wave Amplitudes, a Clinical Parameter for Detecting Early TTR Amyloidosis Cardiac Involvement
Abstract
1. Introduction
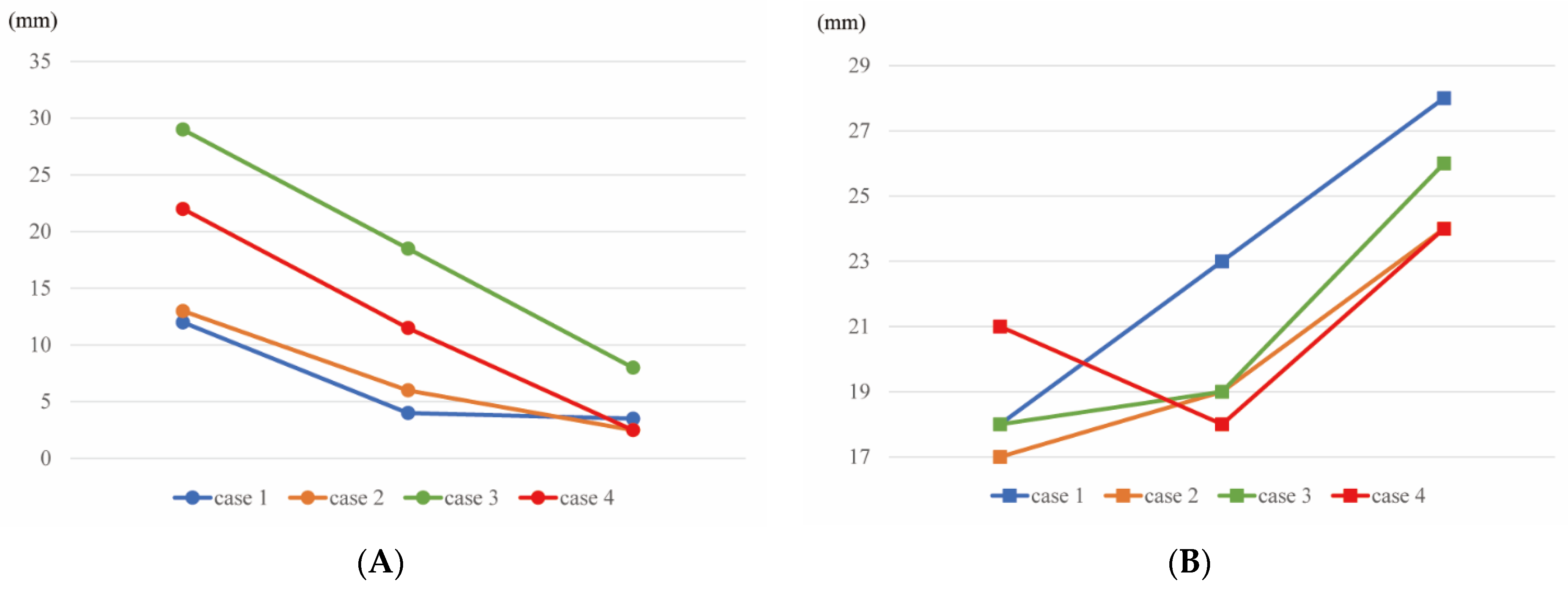
2. Case Presentation
3. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Maurer, M.S.; Schwartz, J.H.; Gundapaneni, B.; Elliott, P.M.; Merlini, G.; Waddington-Cruz, M.; Kristen, A.V.; Grogan, M.; Witteles, R.; Damy, T.; et al. ATTR-ACT Study Investigators. Tafamidis Treatment for Patients with Transthyretin Amyloid Cardiomyopathy. N. Engl. J. Med. 2018, 379, 1007–1016. [Google Scholar] [CrossRef] [PubMed]
- Porcari, A.; Bussani, R.; Merlo, M.; Varrà, G.G.; Pagura, L.; Rozze, D.; Sinagra, G. Incidence and Characterization of Concealed Cardiac Amyloidosis Among Unselected Elderly Patients Undergoing Post-mortem Examination. Front. Cardiovasc. Med. 2021, 8, 749523. [Google Scholar] [CrossRef] [PubMed]
- Lindmark, K.; Pilebro, B.; Sundström, T.; Lindqvist, P. Prevalence of wild type transtyrethin cardiac amyloidosis in a heart failure clinic. ESC Heart Fail. 2021, 8, 745–749. [Google Scholar] [CrossRef]
- González-López, E.; Gallego-Delgado, M.; Guzzo-Merello, G.; Moral, F.J.D.H.-D.; Cobo-Marcos, M.; Robles, C.; Bornstein, B.; Salas, C.; Lara-Pezzi, E.; Alonso-Pulpon, L.; et al. Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur. Heart J. 2015, 36, 2585–2594. [Google Scholar] [CrossRef] [PubMed]
- Ladefoged, B.; Dybro, A.; Povlsen, J.A.; Vase, H.; Clemmensen, T.S.; Poulsen, S.H. Diagnostic delay in wild type transthyretin cardiac amyloidosis-A clinical challenge. Int. J. Cardiol. 2020, 304, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Hanna, M.; Ruberg, F.L.; Maurer, M.S.; Dispenzieri, A.; Dorbala, S.; Falk, R.H.; Hoffman, J.; Jaber, W.; Soman, P.; Witteles, R.M.; et al. Cardiac Scintigraphy with Technetium-99m-Labeled Bone-Seeking Tracers for Suspected Amyloidosis: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2020, 75, 2851–2862. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Naharro, A.; Treibel, T.A.; Abdel-Gadir, A.; Bulluck, H.; Zumbo, G.; Knight, D.S.; Kotecha, T.; Francis, R.; Hutt, D.F.; Rezk, T.; et al. Magnetic Resonance in Transthyretin Cardiac Amyloidosis. J. Am. Coll. Cardiol. 2017, 70, 466–477. [Google Scholar] [CrossRef]
- Rapezzi, C.; Quarta, C.C.; Guidalotti, P.L.; Pettinato, C.; Fanti, S.; Leone, O.; Ferlini, A.; Longhi, S.; Lorenzini, M.; Reggiani, L.B.; et al. Role of (99m) Tc-DPD scintigraphy in diagnosis and prognosis of hereditary transthyretin-related cardiac amyloidosis. JACC Cardiovasc. Imaging 2011, 4, 659–670. [Google Scholar] [CrossRef]
- Gillmore, J.D.; Damy, T.; Fontana, M.; Hutchinson, M.; Lachmann, H.J.; Martinez-Naharro, A.; Quarta, C.C.; Rezk, T.; Whelan, C.J.; Gonzalez-Lopez, E.; et al. A new staging system for cardiac transthyretin amyloidosis. Eur. Heart J. 2018, 39, 2799–2806. [Google Scholar] [CrossRef] [PubMed]
- Grogan, M.; Scott, C.G.; Kyle, R.A.; Zeldenrust, S.R.; Gertz, M.A.; Lin, G.; Klarich, K.W.; Miller, W.L.; Maleszewski, J.J.; Dispenzieri, A. Natural History of Wild-Type Transthyretin Cardiac Amyloidosis and Risk Stratification Using a Novel Staging System. J. Am. Coll. Cardiol. 2016, 68, 1014–1020. [Google Scholar] [CrossRef] [PubMed]
- Cappelli, F.; Vignini, E.; Martone, R.; Perlini, S.; Mussinelli, R.; Sabena, A.; Morini, S.; Gabriele, M.; Taborchi, G.; Bartolini, S.; et al. Baseline ECG Features and Arrhythmic Profile in Transthyretin Versus Light Chain Cardiac Amyloidosis. Circ. Heart Fail. 2020, 13, e006619. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.; Kang, L.; Tian, Z.; Chen, W.; Guo, W.; Xu, J.; Chen, T.; Fang, L.; Zeng, Y.; Cheng, K.; et al. Utility of combined indexes of electrocardiography and echocardiography in the diagnosis of biopsy proven primary cardiac amyloidosis. Ann. Noninvasive Electrocardiol. 2011, 16, 25–29. [Google Scholar] [CrossRef] [PubMed]
- DePace, N.L.; Colby, J.; Hakki, A.H.; Manno, B.; Horowitz, L.N.; Iskandrian, A.S. Poor R wave progression in the precordial leads: Clinical implications for the diagnosis of myocardial infarction. J. Am. Coll. Cardiol. 1983, 2, 1073–1079. [Google Scholar] [CrossRef]
- Cyrille, N.B.; Goldsmith, J.; Alvarez, J.; Maurer, M.S. Prevalence and prognostic significance of low QRS voltage among the three main types of cardiac amyloidosis. Am. J. Cardiol. 2014, 114, 1089–1093. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Li, J.; Tian, Z.; Fang, Q. Clinical correlates and prognostic values of pseudoinfarction in cardiac light-chain amyloidosis. J. Cardiol. 2016, 68, 426–430. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Lee, G.Y.; Choi, J.O.; Kim, K.; Kim, S.J.; Jeon, E.S. Associations of Electrocardiographic Parameters with Left Ventricular Longitudinal Strain and Prognosis in Cardiac Light Chain Amyloidosis. Sci. Rep. 2019, 9, 7746. [Google Scholar] [CrossRef] [PubMed]
- Ruberg, F.L.; Berk, J.L. Transthyretin (TTR) cardiac amyloidosis. Circulation 2012, 126, 1286–1300. [Google Scholar] [CrossRef]
- Augusto, J.B.; Johner, N.; Shah, D.; Nordin, S.; Knott, K.D.; Rosmini, S.; Lau, C.; Alfarih, M.; Hughes, R.; Seraphim, A.; et al. The myocardial phenotype of Fabry disease pre-hypertrophy and pre-detectable storage. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 790–799. [Google Scholar] [CrossRef]
- Koike, H.; Ikeda, S.; Takahashi, M.; Kawagashira, Y.; Iijima, M.; Misumi, Y.; Ando, Y.; Ikeda, S.I.; Katsuno, M.; Sobue, G. Schwann cell and endothelial cell damage in transthyretin familial amyloid polyneuropathy. Neurology 2016, 87, 2220–2229. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Isotani, Y.; Amiya, E.; Ishida, J.; Komuro, I. Summation of Precordial R Wave Amplitudes, a Clinical Parameter for Detecting Early TTR Amyloidosis Cardiac Involvement. J. Cardiovasc. Dev. Dis. 2022, 9, 348. https://doi.org/10.3390/jcdd9100348
Isotani Y, Amiya E, Ishida J, Komuro I. Summation of Precordial R Wave Amplitudes, a Clinical Parameter for Detecting Early TTR Amyloidosis Cardiac Involvement. Journal of Cardiovascular Development and Disease. 2022; 9(10):348. https://doi.org/10.3390/jcdd9100348
Chicago/Turabian StyleIsotani, Yoshitaka, Eisuke Amiya, Junichi Ishida, and Issei Komuro. 2022. "Summation of Precordial R Wave Amplitudes, a Clinical Parameter for Detecting Early TTR Amyloidosis Cardiac Involvement" Journal of Cardiovascular Development and Disease 9, no. 10: 348. https://doi.org/10.3390/jcdd9100348
APA StyleIsotani, Y., Amiya, E., Ishida, J., & Komuro, I. (2022). Summation of Precordial R Wave Amplitudes, a Clinical Parameter for Detecting Early TTR Amyloidosis Cardiac Involvement. Journal of Cardiovascular Development and Disease, 9(10), 348. https://doi.org/10.3390/jcdd9100348





