Limitations of Baseline Impedance, Impedance Drop and Current for Radiofrequency Catheter Ablation Monitoring: Insights from In silico Modeling
Abstract
:1. Introduction
2. Methods
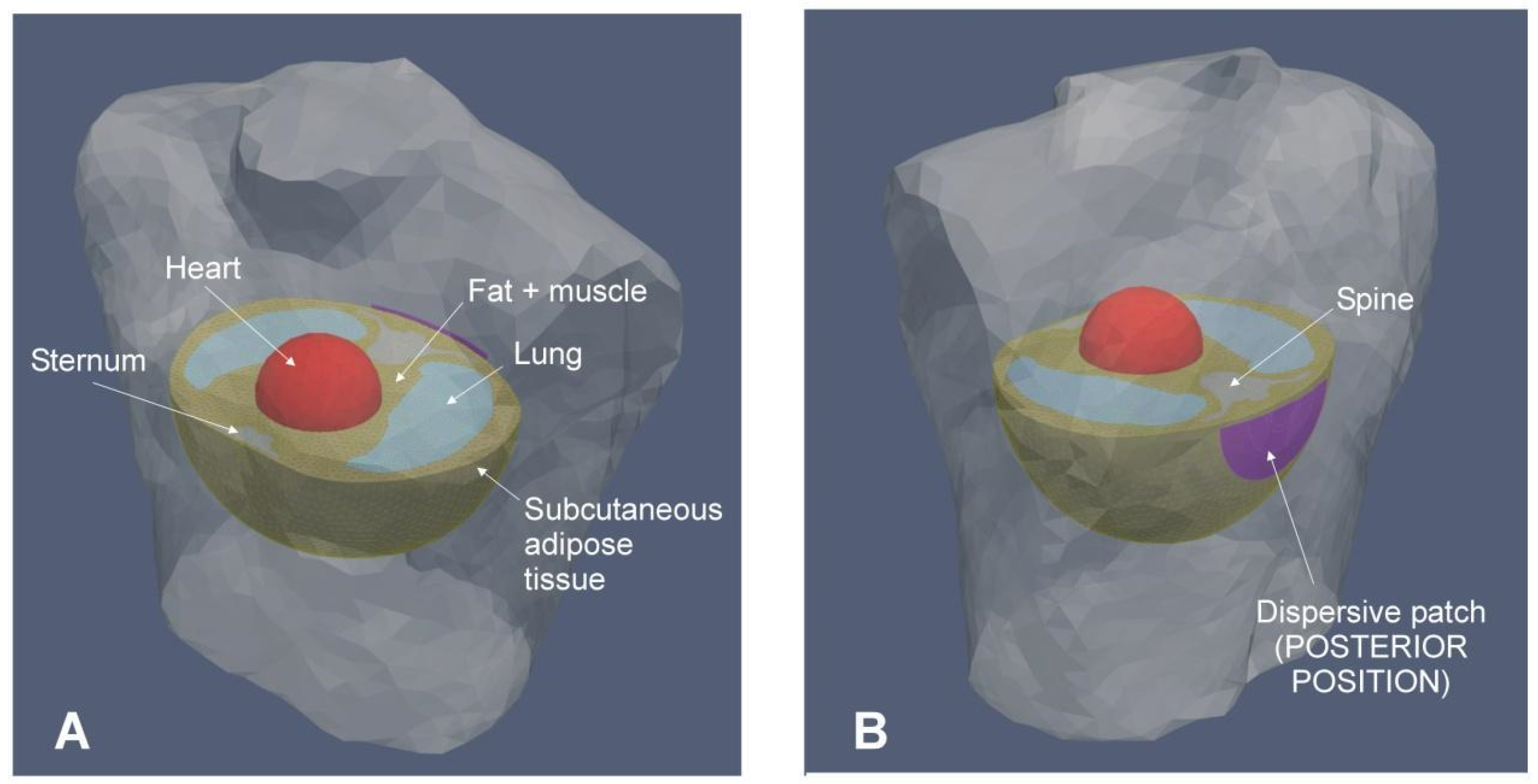
2.1. Model Description
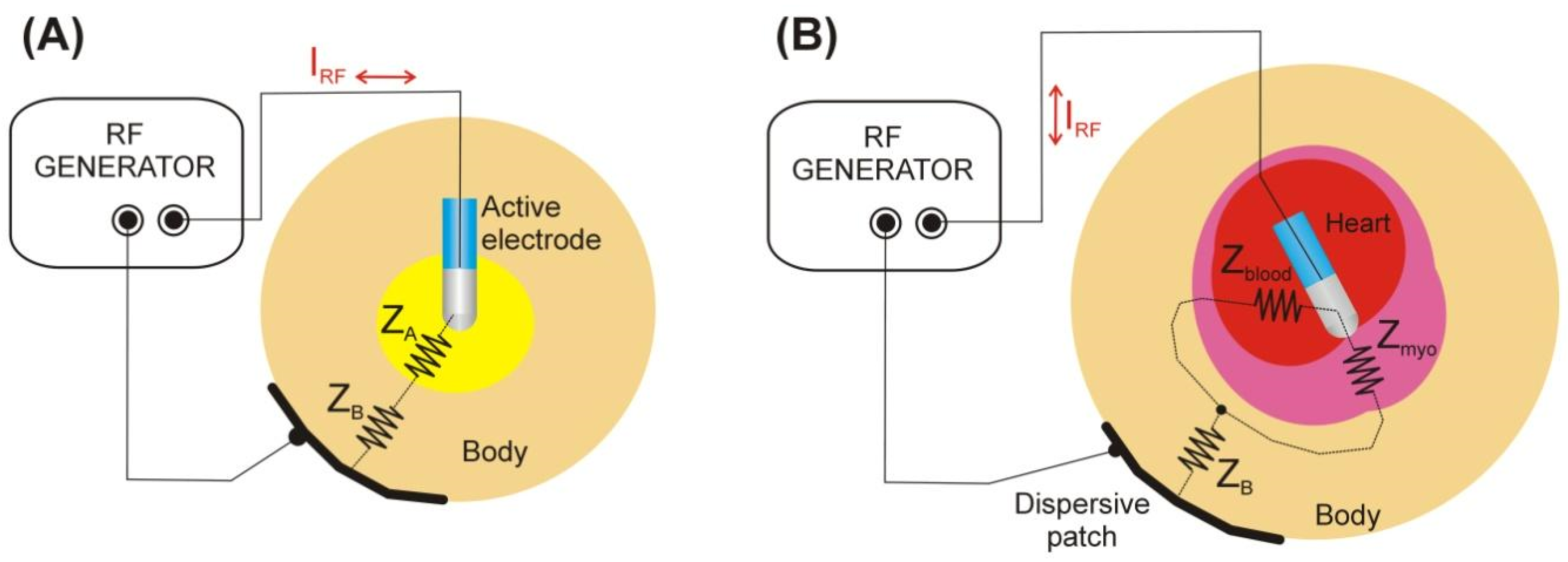
2.2. Modeling the Dispersion of ‘Remote’ Impedance ZB
2.3. Modeling the Dispersion of ‘Local’ Impedance ZA
2.4. The Concept of ‘Corrected Power’
2.5. Statistics
3. Results
3.1. Morphological Data from the CT Scans
3.2. Effect of ‘Remote’ Impedance ZB
3.3. Effect of ‘Local’ Impedance ZA
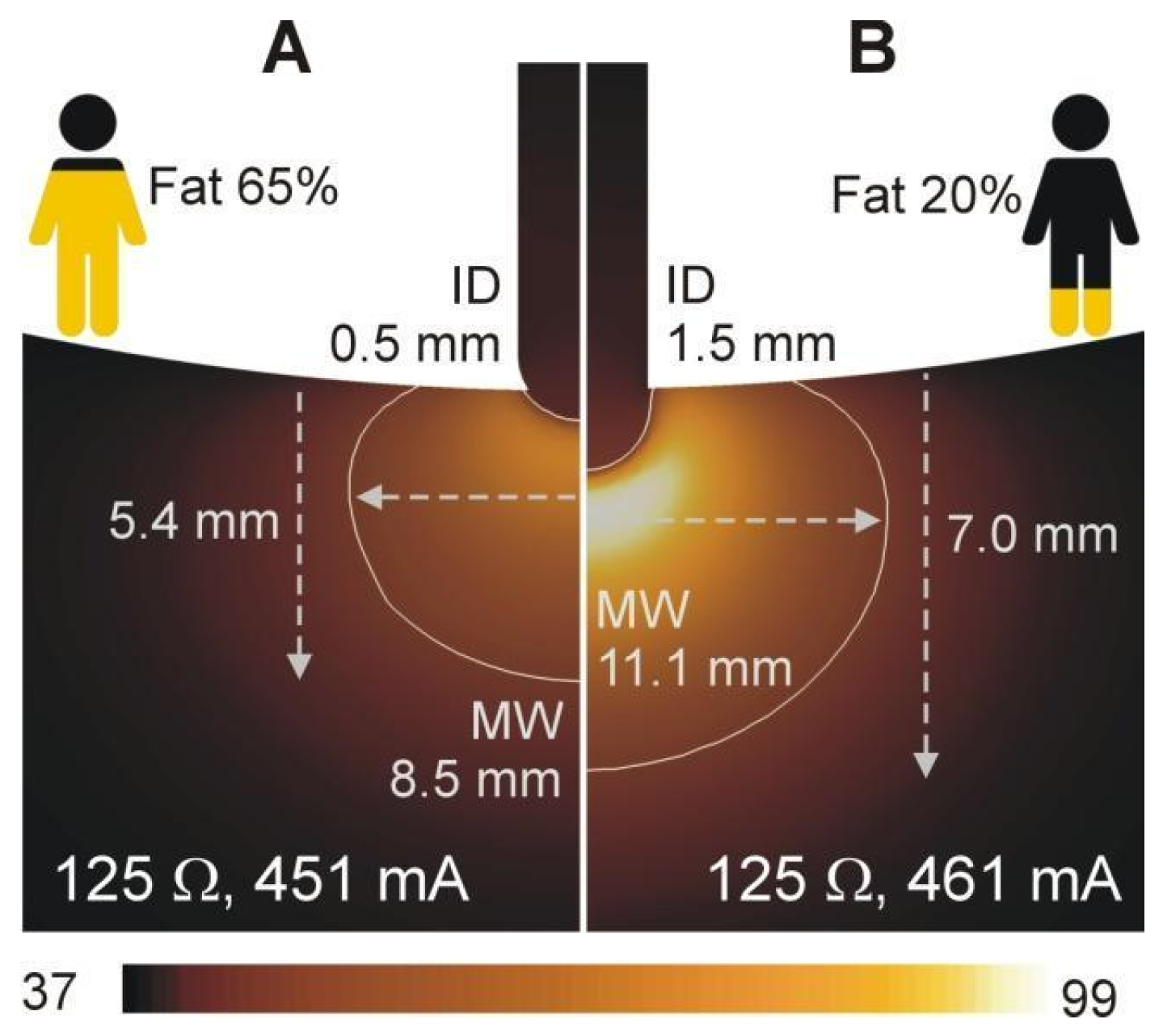
3.4. Relationship between Current, Baseline Impedance and Lesion Size
3.5. Impact of Correcting Power According Baseline Impedance
4. Discussion
4.1. Main Findings
- (1)
- Increasing ZB by increasing the percent tissue fat resulted in higher baseline impedance, lower RF current, and smaller lesion formation controlling for the catheter insertion depth. In contrast, increasing ZA by increasing the insertion depth of the ablation electrode also resulted in higher baseline impedances and lower RF current but larger lesion sizes, controlling for the tissue fat percentage.
- (2)
- Identical baseline impedances as result of different relative contributions of ZA and ZB can lead to similar observed RF currents but very different lesion sizes.
- (3)
- Impedance drop during RF delivery showed a monotonic relationship with lesion size, while observed RF current during RF delivery did not show a predictable relationship with lesion size.
- (4)
- When using ‘corrected power’ to account for baseline impedances, the correction formula only results in similar lesion sizes if differences in Z are due to variation in ZB rather than ZA.
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barkagan, M.; Rottmann, M.; Leshem, E.; Shen, C.; Buxton, A.E.; Anter, E. Effect of Baseline Impedance on Ablation Lesion Dimensions. Circ. Arrhythmia Electrophysiol. 2018, 11, e006690. [Google Scholar] [CrossRef] [PubMed]
- Bhaskaran, A.; Barry, M.A.; Pouliopoulos, J.; Nalliah, C.; Qian, P.; Chik, W.; Thavapalachandran, S.; Davis, L.; McEwan, A.; Thomas, S.; et al. Circuit Impedance Could Be a Crucial Factor Influencing Radiofrequency Ablation Efficacy and Safety: A Myocardial Phantom Study of the Problem and its Correction. J. Cardiovasc. Electrophysiol. 2016, 27, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Shapira-Daniels, A.; Barkagan, M.; Rottmann, M.; Sroubek, J.; Tugal, D.; Carlozzi, M.A.; McConville, J.W.; Buxton, A.E.; Anter, E. Modulating the Baseline Impedance: An Adjunctive Technique for Maximizing Radiofrequency Lesion Dimensions in Deep and Intramural Ventricular Substrate. Circ. Arrhythmia Electrophysiol. 2019, 12, e007336. [Google Scholar] [CrossRef] [PubMed]
- Khoshknab, M.; Kuo, L.; Zghaib, T.; Arkles, J.; Santangeli, P.; Marchlinski, F.E.; Han, Y.; Desjardins, B.; Nazarian, S. Esophageal luminal temperature rise during atrial fibrillation ablation is associated with lower radiofrequency electrode distance and baseline impedance. J. Cardiovasc. Electrophysiol. 2021, 32, 1857–1864. [Google Scholar] [CrossRef] [PubMed]
- Berjano, E.; d’Avila, A. Lumped Element Electrical Model based on Three Resistors for Electrical Impedance in Radiofrequency Cardiac Ablation: Estimations from Analytical Calculations and Clinical Data. Open Biomed. Eng. J. 2013, 12, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Wittkampf, F.H.; Nakagawa, H. RF catheter ablation: Lessons on lesions. Pacing Clin. Electrophysiol. 2006, 29, 1285–1297. [Google Scholar] [CrossRef] [PubMed]
- Hasgall, P.A.; Di Gennaro, F.; Baumgartner, C.; Neufeld, E.; Lloyd, B.; Gosselin, M.C.; Payne, D.; Klingenböck, A.; Kuster, N. IT’IS Database for Thermal and Electromagnetic Parameters of Biological Tissues, Version 4.1. 22 February 2022. Available online: https://itis.swiss/virtual-population/tissue-properties/overview/ (accessed on 26 September 2022).
- González-Suárez, A.; Pérez, J.J.; Irastorza, R.M.; D’Avila, A.; Berjano, E. Computer modeling of radiofrequency cardiac ablation: 30 years of bioengineering research. Comput. Methods Programs Biomed. 2022, 214, 106546. [Google Scholar] [CrossRef] [PubMed]
- Pérez, J.J.; González-Suárez, A.; Maher, T.; Nakagawa, H.; d’Avila, A.; Berjano, E. Relationship between luminal esophageal temperature and volume of esophageal injury during RF ablation: In silico study comparing low power-moderate duration vs. high power-short duration. J. Cardiovasc. Electrophysiol. 2022, 33, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Langtangen, H.P.; Logg, A. Solving PDEs in Python. The FEniCS Tutorial I; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar] [CrossRef]
- Geuzaine, C.; Remacle, J.F. Gmsh: A three-dimensional finite element mesh generator with built-in pre- and post-processing facilities. Int. J. Numer. Methods Eng. 2009, 79, 1309–1331. [Google Scholar] [CrossRef]
- Irastorza, R.M.; Maher, T.; Barkagan, M.; Liubasuskas, R.; Berjano, E.; d’Avila, A. Anterior vs. Posterior Position of Dispersive Patch during RF Catheter Ablation: Insights from In-Silico Modeling. SSRN’s eLibrary. Available online: https://ssrn.com/abstract=4112830 (accessed on 26 September 2022).
- Pérez, J.J.; Ewertowska, E.; Berjano, E. Computer modeling for radiofrequency bipolar ablation inside ducts and vessels: Relation between pullback speed and impedance progress. Lasers Surg Med. 2020, 52, 897–906. [Google Scholar] [CrossRef] [PubMed]
- Van der Walt, S.; Schönberger, J.L.; Nunez-Iglesias, J.; Boulogne, F.; Warner, J.D.; Yager, N.; Gouillart, E.; Yu, T.; The Scikit-Image Contributors. scikit-image: Image processing in Python. PeerJ 2014, 2, e453. [Google Scholar] [CrossRef] [PubMed]
- Bourier, F.; Popa, M.; Kottmaier, M.; Maurer, S.; Bahlke, F.; Telishevska, M.; Lengauer, S.; Koch-Büttner, K.; Kornmayer, M.; Risse, E.; et al. RF electrode-tissue coverage significantly influences steam pop incidence and lesion size. J. Cardiovasc. Electrophysiol. 2021, 32, 1594–1599. [Google Scholar] [CrossRef] [PubMed]
- Sulkin, M.S.; Laughner, J.I.; Hilbert, S.; Kapa, S.; Kosiuk, J.; Younan, P.; Romero, I.; Shuros, A.; Hamann, J.J.; Hindricks, G.; et al. Novel Measure of Local Impedance Predicts Catheter-Tissue Contact and Lesion Formation. Circ. Arrhythmia Electrophysiol. 2018, 11, e005831. [Google Scholar] [CrossRef] [PubMed]
- Iwakawa, H.; Takigawa, M.; Goya, M.; Iwata, T.; Martin, C.A.; Anzai, T.; Takahashi, K.; Amemiya, M.; Yamamoto, T.; Sekigawa, M.; et al. Clinical implications of local impedance measurement using the IntellaNav MiFi OI ablation catheter: An ex vivo study. J. Interv. Card. Electrophysiol. 2022, 63, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Gunawardene, M.; Münkler, P.; Eickholt, C.; Akbulak, R.Ö.; Jularic, M.; Klatt, N.; Hartmann, J.; Dinshaw, L.; Jungen, C.; Moser, J.M.; et al. A novel assessment of local impedance during catheter ablation: Initial experience in humans comparing local and generator measurements. Europace 2019, 21 (Suppl. S1), i34–i42. [Google Scholar] [CrossRef] [PubMed]




| Element/Material | σ (S/m) | k (W/m·K) | ρ (kg/m3) | c (J/kg·K) |
|---|---|---|---|---|
| Electrode/Pt-Ir | 4.6 × 106 | 71 | 21,500 | 132 |
| Catheter/Polyurethane | 10−5 | 23 | 1440 | 1050 |
| Cardiac wall/Myocardium | 0.281 | 0.56 | 1081 | 3686 |
| Cardiac chamber/Blood | 0.748 | Thermal problem not solved | ||
| Muscle | 0.446 | 0.49 | 1090 | 3421 |
| Subcutaneous fat (infiltrated fat) | 0.0438 | 0.21 | 911 | 2348 |
| Lungs | 0.215 | 0.39 | 722 | 3886 |
| Spine, sternum/bone * | 0.055 | 0.315 | 1543 | 1793 |
| Pt # | Sex | Age (years) | BMI (kg/m2) | BSA (m2) | Sternum-LA (mm) | LA-Spine (mm) | %Fat |
|---|---|---|---|---|---|---|---|
| 1 | M | 33 | 34.18 | 2.41 | 163 | 114 | 52 |
| 2 | M | 58 | 39.38 | 2.27 | 159 | 139 | 65 |
| 3 | F | 38 | 37.73 | 2.37 | 170 | 110 | 72 |
| 4 | M | 84 | 29.52 | 1.87 | 142 | 105 | 78 |
| 5 | F | 43 | 30.30 | 1.68 | 149 | 89 | 63 |
| 6 | M | 61 | 26.41 | 1.94 | 140 | 109 | 61 |
| 7 | F | 90 | 25.06 | 1.73 | 140 | 114 | 78 |
| 8 | M | 55 | 36.24 | 2.58 | 171 | 125 | 73 |
| 9 | M | 67 | 29.40 | 2.14 | 161 | 160 | 62 |
| 10 | M | 72 | 34.96 | 2.49 | 161 | 128 | 78 |
| 11 | M | 66 | 29.98 | 2.02 | 174 | 129 | 65 |
| 12 | F | 61 | 24.80 | 1.82 | 137 | 112 | 51 |
| 13 | M | 73 | 26.66 | 2.17 | 165 | 106 | 54 |
| 14 | F | 49 | 35.48 | 1.96 | 146 | 113 | 81 |
| 15 | M | 75 | 22.96 | 2.01 | 149 | 100 | 55 |
| 16 | M | 86 | 31.48 | 2.05 | 146 | 117 | 59 |
| 17 | M | 59 | 30.78 | 2.24 | 171 | 134 | 36 |
| 18 | M | 79 | 30.72 | 2.09 | 168 | 127 | 40 |
| 19 | M | 69 | 37.31 | 2.50 | 172 | 155 | 63 |
| 20 | F | 63 | 17.38 | 1.37 | 110 | 73 | 29 |
| Mean | 64.1 | 30.54 | 2.09 | 154.7 | 118.0 | 61 | |
| SD | 15.5 | 5.59 | 0.31 | 16.2 | 20.4 | 14 | |
| Min | 90 | 39.38 | 2.58 | 174 | 160 | 81 | |
| Max | 33 | 17.38 | 1.37 | 110 | 73 | 29 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Irastorza, R.M.; Maher, T.; Barkagan, M.; Liubasuskas, R.; Pérez, J.J.; Berjano, E.; d’Avila, A. Limitations of Baseline Impedance, Impedance Drop and Current for Radiofrequency Catheter Ablation Monitoring: Insights from In silico Modeling. J. Cardiovasc. Dev. Dis. 2022, 9, 336. https://doi.org/10.3390/jcdd9100336
Irastorza RM, Maher T, Barkagan M, Liubasuskas R, Pérez JJ, Berjano E, d’Avila A. Limitations of Baseline Impedance, Impedance Drop and Current for Radiofrequency Catheter Ablation Monitoring: Insights from In silico Modeling. Journal of Cardiovascular Development and Disease. 2022; 9(10):336. https://doi.org/10.3390/jcdd9100336
Chicago/Turabian StyleIrastorza, Ramiro M., Timothy Maher, Michael Barkagan, Rokas Liubasuskas, Juan J. Pérez, Enrique Berjano, and Andre d’Avila. 2022. "Limitations of Baseline Impedance, Impedance Drop and Current for Radiofrequency Catheter Ablation Monitoring: Insights from In silico Modeling" Journal of Cardiovascular Development and Disease 9, no. 10: 336. https://doi.org/10.3390/jcdd9100336
APA StyleIrastorza, R. M., Maher, T., Barkagan, M., Liubasuskas, R., Pérez, J. J., Berjano, E., & d’Avila, A. (2022). Limitations of Baseline Impedance, Impedance Drop and Current for Radiofrequency Catheter Ablation Monitoring: Insights from In silico Modeling. Journal of Cardiovascular Development and Disease, 9(10), 336. https://doi.org/10.3390/jcdd9100336









