Differences in the Treatment of Acute Coronary Syndrome in the Pre-COVID and COVID Era: An Analysis from Two German High-Volume Centers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
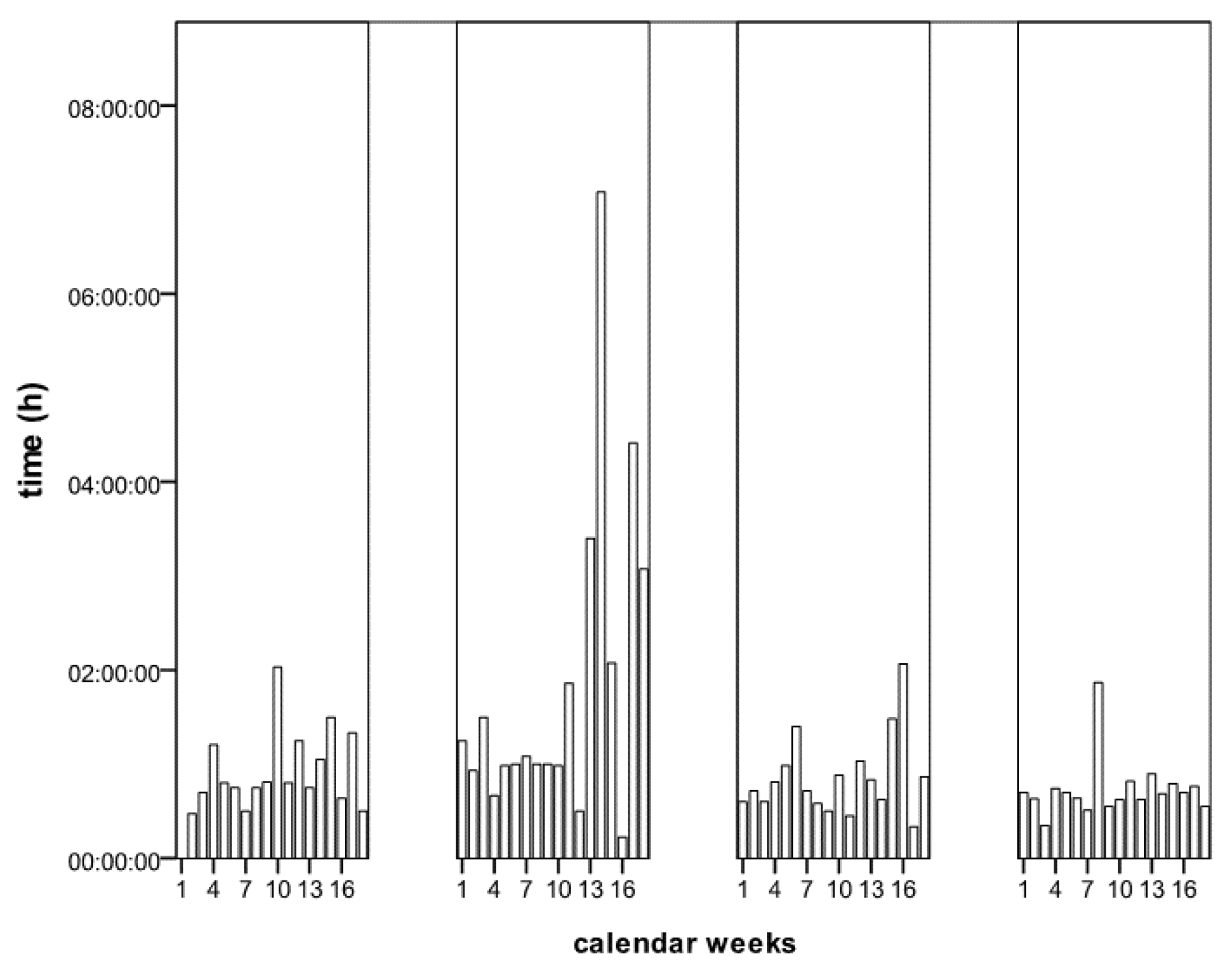
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.; Lau, E.; Wong, J.Y.; et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- RKI. Die Pandemie in Deutschland in Den Nächsten Monaten—Ziele, Schwerpunktthemen Und Instrumente Für Den Infek-Tionsschutz, Stand 23.10.2020. 2020. Available online: www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Strategie_Ergaenzung_Covid.html (accessed on 30 October 2021).
- Nef, H.M.; for the CoVCAD–Study Group; Elsässer, A.; Möllmann, H.; Abdel-Hadi, M.; Bauer, T.; Brück, M.; Eggebrecht, H.; Ehrlich, J.R.; Ferrari, M.W.; et al. Impact of the COVID-19 pandemic on cardiovascular mortality and catherization activity during the lockdown in central Germany: An observational study. Clin. Res. Cardiol. 2021, 110, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, L. The untold toll—The pandemic’s effects on patients without Covid-19. N. Engl. J. Med. 2020, 382, 2368–2371. [Google Scholar] [CrossRef] [PubMed]
- Seiffert, M.; Brunner, F.J.; Remmel, M.; Thomalla, G.; Marschall, U.; L’Hoest, H.; Acar, L.; Debus, E.S.; Blankenberg, S.; Gerloff, C.; et al. Temporal trends in the presentation of cardiovascular and cerebrovascular emergencies during the COVID-19 pandemic in Germany: An analysis of health insurance claims. Clin. Res. Cardiol. 2020, 109, 1540–1548. [Google Scholar] [CrossRef] [PubMed]
- Chieffo, A.; Stefanini, G.G.; Price, S.; Barbato, E.; Tarantini, G.; Karam, N.; Moreno, R.; Buchanan, G.L.; Gilard, M.; Halvorsen, S.; et al. EAPCI position statement on invasive management of acute coronary syndromes during the COVID-19 pandemic. Eur. Heart J. 2020, 41, 1839–1851. [Google Scholar] [CrossRef] [PubMed]
- Gluckman, T.J.; Wilson, M.A.; Chiu, S.-T.; Penny, B.W.; Chepuri, V.B.; Waggoner, J.W.; Spinelli, K.J. Case Rates, Treatment approaches, and outcomes in acute myocardial infarction during the Coronavirus disease 2019 pandemic. JAMA Cardiol. 2020, 5, 1419. [Google Scholar] [CrossRef] [PubMed]
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N. Engl. J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef] [PubMed]
- Lodigiani, C.; Iapichino, G.; Carenzo, L.; Cecconi, M.; Ferrazzi, P.; Sebastian, T.; Kucher, N.; Studt, J.-D.; Sacco, C.; Bertuzzi, A.; et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb. Res. 2020, 191, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Mafham, M.M.; Spata, E.; Goldacre, R.; Gair, D.; Curnow, P.; Bray, M.; Hollings, S.; Roebuck, C.; Gale, C.P.; A Mamas, M.; et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 2020, 396, 381–389. [Google Scholar] [CrossRef]
- Al-Quteimat, O.M.; Amer, A.M. The Impact of the COVID-19 pandemic on cancer patients. Am. J. Clin. Oncol. 2020, 43, 452–455. [Google Scholar] [CrossRef] [PubMed]
- COVIDSurg Collaborative; Glasbey, J.C.; Nepogodiev, D.; Simoes, J.F.F.; Omar, O.M.; Venn, M.L.; Evans, J.P.; Futaba, K.; Knowles, C.H.; Minaya-Bravo, A.; et al. Outcomes from elective colorectal cancer surgery during the SARS-CoV-2 pandemic. Color. Dis. 2020, 23, 732–749. [Google Scholar] [CrossRef]
- Scholz, K.H.; Maier, S.K.G.; Maier, L.S.; Lengenfelder, B.; Jacobshagen, C.; Jung, J.; Fleischmann, C.; Werner, G.S.; Olbrich, H.G.; Ott, R.; et al. Impact of treatment delay on mortality in ST-segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: Results from the German prospective, multicentre FITT-STEMI trial. Eur. Heart J. 2018, 39, 1065–1074. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Luca, G.; Suryapranata, H.; Ottervanger, J.P.; Antman, E.M. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: Every minute of delay counts. Circulation 2004, 109, 1223–1225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Awan, A.; Ogunti, R.; Fatima, U.; Gonzalez, H.; Ganta, N.; Rizwan, M.; Mahajan, A.; Opoku-Asare, I. Timing of percutaneous coronary intervention in non-ST elevation acute coronary syndrome—Meta-analysis and systematic review of literature. Cardiovasc. Revascularization Med. 2019, 21, 1398–1404. [Google Scholar] [CrossRef] [PubMed]
- Alexander, K.P.; Newby, L.K.; Cannon, C.P.; Armstrong, P.; Gibler, W.B.; Rich, M.W.; Van de Werf, F.; White, H.D.; Weaver, W.D.; Naylor, M.D.; et al. Acute coronary care in the elderly, Part I: Non-st-segment-elevation acute coronary syndromes: A scientific statement for healthcare professionals from the american heart association council on clinical cardiology: In collaboration with the society of geriatric cardiology. Circulation 2007, 115, 2549–2569. [Google Scholar] [CrossRef] [Green Version]
- Alexander, K.P.; Newby, L.K.; Armstrong, P.; Cannon, C.P.; Gibler, W.B.; Rich, M.W.; Van de Werf, F.; White, H.D.; Weaver, W.D.; Naylor, M.D.; et al. Acute coronary care in the elderly, Part II: St-segment-elevation myocardial infarction: A sci-entific statement for healthcare professionals from the american heart association council on clinical cardiology: In collabo-ration with the society of geriatric cardiology. Circulation 2007, 115, 2570–2589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rhee, C.; Baker, M.; Vaidya, V.; Tucker, R.; Resnick, A.; Morris, C.A.; Klompas, M.; Program, F.T.C.P.E. Incidence of nosocomial COVID-19 in patients hospitalized at a large US academic medical center. JAMA Netw. Open 2020, 3, e2020498. [Google Scholar] [CrossRef] [PubMed]
- RKI. Täglicher Lagebericht des rki zur Coronavirus-Krankheit-2019 (covid-19) 17.11.2020. Stand 23.10.2020. Available online: https://www.rki.de/EN/Home/homepage_node.html (accessed on 30 October 2021).
- DeFilippis, E.M.; Reza, N.; Donald, E.; Givertz, M.M.; Lindenfeld, J.; Jessup, M. Considerations for heart failure care during the COVID-19 pandemic. JACC Heart Fail. 2020, 8, 681–691. [Google Scholar] [CrossRef]
- Pothineni, N.V.K.; Santangeli, P.; Deo, R.; Marchlinski, F.E.; Hyman, M.C. COVID-19 and electrophysiology procedures—Review, reset, reboot!!! J. Interv. Card. Electrophysiol. 2020, 59, 303–305. [Google Scholar] [CrossRef] [PubMed]



| 2019 (n = 463) | 2020 (n = 503) | p | |||||
|---|---|---|---|---|---|---|---|
| Mean | min/max/SD | % | Mean | min/max/SD | % | ||
| Age (years) | 67.6 | 17–95, 5.3 | 67.6 | 19–95, 12.2 | 0.97 | ||
| Sex female, no. (%) | 27.4 | 28.2 | 0.83 | ||||
| BMI | 27.7 | 13.8–67, 5.3 | 27.6 | 18.6–53, 4.5 | 0.66 | ||
| Arterial hypertension | 74.3 | 77.9 | 0.21 | ||||
| DM | 26.8 | 33.6 | 0.02 | ||||
| Hypercholesterolemia | 53.1 | 59.4 | 0.05 | ||||
| Renal failure | 34.8 | 35.4 | 0.89 | ||||
| Pulmonary hypertension | 5.6 | 7.8 | 0.19 | ||||
| Atrial fibrillation | 14.7 | 16.3 | 0.53 | ||||
| PAD | 14.5 | 16.3 | 0.48 | ||||
| Current smoker | 27.7 | 26.0 | 0.62 | ||||
| CABG | 6.9 | 9.5 | 0.16 | ||||
| Pre-PCI | 17.1 | 20.1 | 0.24 | ||||
| Apoplexy | 7.6 | 8.5 | 0.63 | ||||
| Pre-MI | 13.6 | 15.7 | 0.37 | ||||
| LV-EF | 48.2 | 10–76, 13.8 | 47.7 | 5–73, 13.2 | 0.58 | ||
| 2019 (n = 463) | 2020 (n = 503) | p | |||
|---|---|---|---|---|---|
| n | % or Mean | n | % or Mean | ||
| STEMI | 161 | 34.8 | 167 | 33.2 | 0.64 |
| NSTEMI | 302 | 65.2 | 336 | 66.8 | 0.64 |
| Cardiogenic Schock | 23 | 4.9 | 31 | 6.2 | 0.48 |
| MCS (IABP, Impella, ECMO) | 24 | 5.2 | 27 | 5.4 | 1.00 |
| Radial approach | 290 | 62.6 | 335 | 66.6 | 0.21 |
| Procedure time (min) | 56.3 | 55.3 | 0.67 | ||
| Heart rate (per min) | 78.0 | 79.5 | 0.19 | ||
| BP mean (mmHg) | 90.5 | 90.1 | 0.80 | ||
| Initial hsTnT (ng/mL) | 0.6 | 0.7 | 0.62 | ||
| Initial CK (U/L) | 388.3 | 438.1 | 0.41 | ||
| Max hsTnT (ng/mL) | 2.1 | 2.1 | 0.82 | ||
| Max CK (U/L) | 1274.9 | 1276.3 | 0.99 | ||
| Peripheral vascular complication | 18 | 3.9 | 14 | 2.8 | 0.38 |
| Death in cath lab | 2 | 0.4 | 3 | 0.6 | 1.00 |
| Intrahospital death | 29 | 6.3 | 34 | 6.8 | 0.79 |
| Mortality of CS | 13 | 56.5 | 22 | 71 | 0.39 |
| ICU stay (d) | 2.7 | 2.2 | 0.08 | ||
| Hospital stay (d) | 8.2 | 6.9 | <0.01 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eckner, D.; Hofmann, E.M.; Ademaj, F.; Martinovic, K.; Vogt, F.; Becher, P.M.; Schrage, B.; Westermann, D.; Pauschinger, M. Differences in the Treatment of Acute Coronary Syndrome in the Pre-COVID and COVID Era: An Analysis from Two German High-Volume Centers. J. Cardiovasc. Dev. Dis. 2021, 8, 145. https://doi.org/10.3390/jcdd8110145
Eckner D, Hofmann EM, Ademaj F, Martinovic K, Vogt F, Becher PM, Schrage B, Westermann D, Pauschinger M. Differences in the Treatment of Acute Coronary Syndrome in the Pre-COVID and COVID Era: An Analysis from Two German High-Volume Centers. Journal of Cardiovascular Development and Disease. 2021; 8(11):145. https://doi.org/10.3390/jcdd8110145
Chicago/Turabian StyleEckner, Dennis, Eva M. Hofmann, Fadil Ademaj, Kristinko Martinovic, Ferdinand Vogt, Peter Moritz Becher, Benedikt Schrage, Dirk Westermann, and Matthias Pauschinger. 2021. "Differences in the Treatment of Acute Coronary Syndrome in the Pre-COVID and COVID Era: An Analysis from Two German High-Volume Centers" Journal of Cardiovascular Development and Disease 8, no. 11: 145. https://doi.org/10.3390/jcdd8110145
APA StyleEckner, D., Hofmann, E. M., Ademaj, F., Martinovic, K., Vogt, F., Becher, P. M., Schrage, B., Westermann, D., & Pauschinger, M. (2021). Differences in the Treatment of Acute Coronary Syndrome in the Pre-COVID and COVID Era: An Analysis from Two German High-Volume Centers. Journal of Cardiovascular Development and Disease, 8(11), 145. https://doi.org/10.3390/jcdd8110145







