Oxidized Low-Density Lipoprotein Serum Concentrations and Cardiovascular Morbidity in End Stage of Renal Disease †
Abstract
:1. Introduction
2. Methods
2.1. Patients
2.2. Blood Collection
2.3. Laboratory Measurements
2.4. Hemodynamic and Echo-Cardiographical Measurements
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Limitations
Author Contributions
Funding
Conflicts of Interest
References
- Wen, C.P.; Cheng, T.Y.; Tsai, M.K.; Chang, Y.C.; Chan, H.T.; Tsai, S.P.; Chiang, P.H.; Hsu, C.C.; Sung, P.K.; Hsu, Y.H.; et al. All-cause mortality attributable to chronic kidney disease: A prospective cohort study based on 462 293 adults in Taiwan. Lancet 2008, 28, 2173–2182. [Google Scholar] [CrossRef]
- Inaba, M.; Ueda, M. Vascular Calcification—Pathological Mechanism and Clinical Application—The significance of arterial calcification in unstable plaques. Clin. Calcium 2015, 25, 679–686. [Google Scholar] [PubMed]
- Go, A.S.; Chertow, G.M.; Fan, D.; McCulloch, C.E.; Hsu, C.Y. Chronic kidneydisease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 2004, 351, 1296–1305. [Google Scholar] [CrossRef] [PubMed]
- Han, S.S.; Cho, G.Y.; Park, Y.S.; Baek, S.H.; Ahn, S.Y.; Kim, S.; Chin, H.J.; Chae, D.W.; Na, K.Y. Predictive value of echocardiographic parameters for clinical events in patients starting hemodialysis. J. Korean Med. Sci. 2015, 30, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Madamanchi, N.R.; Vendrov, A.; Runge, M.S. Oxidative stress and vascular disease. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 29–38. [Google Scholar] [CrossRef] [PubMed]
- George, J.; Wexler, D.; Roth, A.; Barak, T.; Sheps, D.; Keren, G. Usefulness of antioxidized LDL antibody determination for assessment of clinical control in subjects with heart failure. Eur. J. Heart Fail 2006, 8, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Vaziri, N.D. Oxidative stress in chronic renal failure: The nature, mechanism and consequences. Semin. Nephrol. 2004, 24, 469–473. [Google Scholar] [CrossRef] [PubMed]
- Marsche, G.; Saemann, M.D.; Heinemann, A.; Holzer, M. Inflammation alters HDL composition and function: Implications for HDL-raising therapies. Pharmacol. Ther. 2013, 137, 341–351. [Google Scholar] [CrossRef] [PubMed]
- Susantitaphong, P.; Siribamrungwong, M.; Jaber, B.L. Convective therapies versus low-flux hemodialysis for chronic kidney failure: A meta-analysis of randomized controlled trials. Nephrol. Dial. Transplant. 2013, 28, 2859–2874. [Google Scholar] [CrossRef] [PubMed]
- Sternby, J.; Daugirdas, J.T. Theoretical basis for and improvement of Daugirdas’ second generation formula for single-pool Kt/V. Int. J. Artif. Organs. 2015, 38, 632–637. [Google Scholar] [CrossRef] [PubMed]
- Silva, E.A.; Flexa, F.; Zanella, M.T. Impact of abdominal fat and insulin resistance on arterial hypertension in non-obese women. Arq. Bras. Endocrinol. Metabol. 2009, 53, 340–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luman, M.; Jerotskaja, J.; Lauri, K.; Fridolin, I. Dialysis dose and nutrition assessment by optical on-line dialysis adequacy monitor. Clin. Nephrol. 2009, 72, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Nguyen-Khoa, T.; Massy, Z.A.; De Bandt, J.P.; Kebede, M.; Salama, L.; Lambrey, G.; Witko-Sarsat, V.; Drüeke, T.B.; Lacour, B.; Thévenin, M. Oxidative stress and haemodialysis: Role of inflammation and duration of dialysis treatment. Nephrol. Dial. Transplant. 2001, 16, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Jahromi, S.R.; Hosseini, S.; Razeghi, E.; Meysamie Ap Sadrzadeh, H. Malnutrition predicting factors in hemodialysis patients. Saudi J. Kidney Dis. Transplant. 2010, 21, 846–851. [Google Scholar]
- Hung, A.M.; Ikizler, T.A. Factors determining insulin resistance in chronic hemodialysis patients. Contrib. Nephrol. 2011, 171, 127–134. [Google Scholar] [PubMed]
- Zanetti, M.; Barazzoni, R.; Guarnieri, G. Inflammation and insulin resistance in uremia. J. Ren. Nutr. 2008, 18, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Sies, H. Oxidative stress: Oxidants and antioxidants. Exp. Physiol. 1997, 82, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Al-Biltagi, M.; Tolba, O.A.; ElHafez, M.A.; Abo-Elezz, A.A.; El Kady, E.K.; Hazza, S.M. Oxidative stress and cardiac dysfunction in children with chronic renal failure on regular hemodialysis. Pediatr. Nephrol. 2016, 31, 1329–1339. [Google Scholar] [CrossRef] [PubMed]
- Schimke, I.; Müller, J.; Dandel, M.; Gremmels, H.D.; Bayer, W.; Wallukat, B.; Wallukat, G.; Hetzer, R. Reduced oxidative stress in parallel to improved cardiac performance one year after selective removal of anti-beta 1-adrenoreceptor autoantibodies in patients with idiopathic dilated cardiomyopathy: Data of a preliminary study. J. Clin. Apher. 2005, 20, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Aluganti Narasimhulu, C.; Litvinov, D.; Sengupta, B.; Jones, D.; Sai-Sudhakar, C.; Firstenberg, M.; Sun, B.; Parthasarathy, S. Increased presence of oxidized low-density lipoprotein in the left ventricular blood of subjects with cardiovascular disease. Physiol. Rep. 2016, 4, e12726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wagner, S.; Apetrii, M.; Massy, Z.A.; Kleber, M.E.; Delgado, G.E.; Scharnagel, H.; März, W.; Metzger, M.; Rossignol, P.; Jardine, A.; et al. Oxidized LDL, statin use, morbidity, and mortality in patients receiving maintenance hemodialysis. Free Radic. Res. 2017, 51, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Drożdż, D.; Kwinta, P.; Sztefko, K.; Kordon, Z.; Drożdż, T.; Łątka, M.; Miklaszewska, M.; Zachwieja, K.; Rudziński, A.; Pietrzyk, J.A. Oxidative Stress Biomarkers and Left Ventricular Hypertrophy in Children with Chronic Kidney Disease. Oxid. Med. Cell Longev. 2016, 2016, 7520231. [Google Scholar] [CrossRef] [PubMed]
- Larivière, R.; Gauthier-Bastien, A.; Ung, R.V.; St-Hilaire, J.; Mac-Way, F.; Richard, D.E.; Agharazii, M. Endothelin type A receptor blockade reduces vascular calcification and inflammation in rats with chronic kidney disease. J. Hypertens. 2017, 35, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Agharazii, M.; St-Louis, R.; Gautier-Bastien, A.; Ung, R.V.; Mokas, S.; Larivière, R.; Richard, D.E. Inflammatory cytokines and reactive oxygen species as mediators of chronic kidney disease-related vascular calcification. Am. J. Hypertens. 2015, 28, 746–755. [Google Scholar] [CrossRef] [PubMed]
- Descamps-Latscha, B.; Drüeke, T.; Witko-Sarsat, V. Dialysis-induced oxidative stress: Biological aspects, clinical consequences, and therapy. Semin. Dial. 2001, 14, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Moreno, J.M.; Herencia, C.; de Oca, A.M.; Díaz-Tocados, J.M.; Vergara, N.; Gómez-Luna, M.J.; López-Argüello, S.D.; Camargo, A.; Peralbo-Santaella, E.; Rodríguez-Ortiz, M.E.; et al. High phosphate induces a pro-inflammatory response by vascular smooth muscle cells and modulation by vitamin D derivatives. Clin. Sci. 2017, 28, 1449–1463. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Moreno, J.M.; Herencia, C.; Montes de Oca, A.; Muñoz-Castañeda, J.R.; Rodríguez-Ortiz, M.E.; Díaz-Tocados, J.M.; Peralbo-Santaella, E.; Camargo, A.; Canalejo, A.; Canalejo, A.; et al. Vitamin D modulates tissue factor and protease-activated receptor 2 expression in vascular smooth muscle cells. FASEB J. 2016, 30, 1367–1376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristic | Hemodiafiltration Patients (n = 96) Mean ± SD or/Mean Rank | Healthy Control Subjects (n = 45) Mean ± SD or/Mean Rank | p Value |
|---|---|---|---|
| Gender (males %/females %) | 62(64.6%)/34(35.4%) | 24 (53.3%)/21 (46.7%) | 0.1 |
| Age (years) | 62.1 ± 14.2 | 59.6 ± 11.9 | 0.6 |
| BMI (Kg/m2) | 25.08 ± 3.9 | 25.9 ± 3.6 | 0.2 |
| Cholesterol (mg/dL) | 163.4 ± 45.3 * | 188.7 ± 27.3 | 0.001 |
| LDL (mg/dL) | 90.5 ± 37.2 | 99.08 ± 29.6 | 0.8 |
| HDL (mg/dL) | 38.9 ± 9.7 * | 53.9 ± 8.9 | 0.001 |
| Triglycerides (mg/dL) | 172.1 ± 87.1 * | 86.8 ± 35.6 | 0.001 |
| oxLDL (ng/mL) | 69.4 * | 54.4 | 0.03 |
| OxLDL/LDL (ng/mg) | 76.2 * | 59.8 | 0.02 |
| Glucose (mg/dL) | 96.2 ± 22.2 * | 89.06 ± 9.6 | 0.009 |
| Insulin (μU/mL) | 78.6 * | 50.8 | 0.001 |
| HOMA-IR (mmol/L) | 79.9 * | 52.02 | 0.001 |
| hsCRP (mg/L) | 8.6 ± 5.9 * | 2.8 ± 2.3 | 0.001 |
| MCP-1 (pg/mL) | 69.8 | 68.6 | 0.9 |
| TNF-α (pg/mL) | 83.6 * | 65.08 | 0.01 |
| i-PTH (pg/mL) | 86.08 * | 34.09 | 0.001 |
| Characteristic | Patients with Ejection Fraction Less Than 50% (n = 26) Mean ± SD/Mean Rank | Patients with Ejection Fraction More Than 50% (n = 70) Mean ± SD/Mean Rank | p Value |
|---|---|---|---|
| Age (years) | 68.8 ± 12.6 * | 59.6 ± 14.1 | 0.005 |
| Dialysis vintage (years) | 52.8 | 46.9 | 0.4 |
| spKt/V for urea | 46.1 | 49.4 | 0.6 |
| nPCR (g/Kg/day) | 2.2 ± 0.6 | 2.2 ± 0.5 | 0.9 |
| Interdialytic urine volume (mL) | 225 ± 154.1 | 361.4 ± 326.4 | 0.3 |
| Interdialytic weight gain (L) | 2.2 ± 0.7 | 2.3 ± 1.1 | 0.4 |
| BMI (Kg/m2) | 24.8 ± 3.3 | 25.2 ± 4.04 | 0.7 |
| Hb (gr/dL) | 11.6 ± 1.3 | 11.9 ± 1.4 | 0.3 |
| Cholesterol (mg/dL) | 158.5 ± 47.3 | 165.2 ± 44.8 | 0.5 |
| LDL (mg/dL) | 85.2 ± 35.1 | 92.5 ± 37.8 | 0.4 |
| HDL (mg/dL) | 38.5 ± 10.6 | 39.02 ± 9.4 | 0.8 |
| Triglycerides (mg/dL) | 181.7 ± 111.6 | 168.6 ± 76.7 | 0.6 |
| oxLDL (ng/mL) | 55.9 | 45.7 | 0.1 |
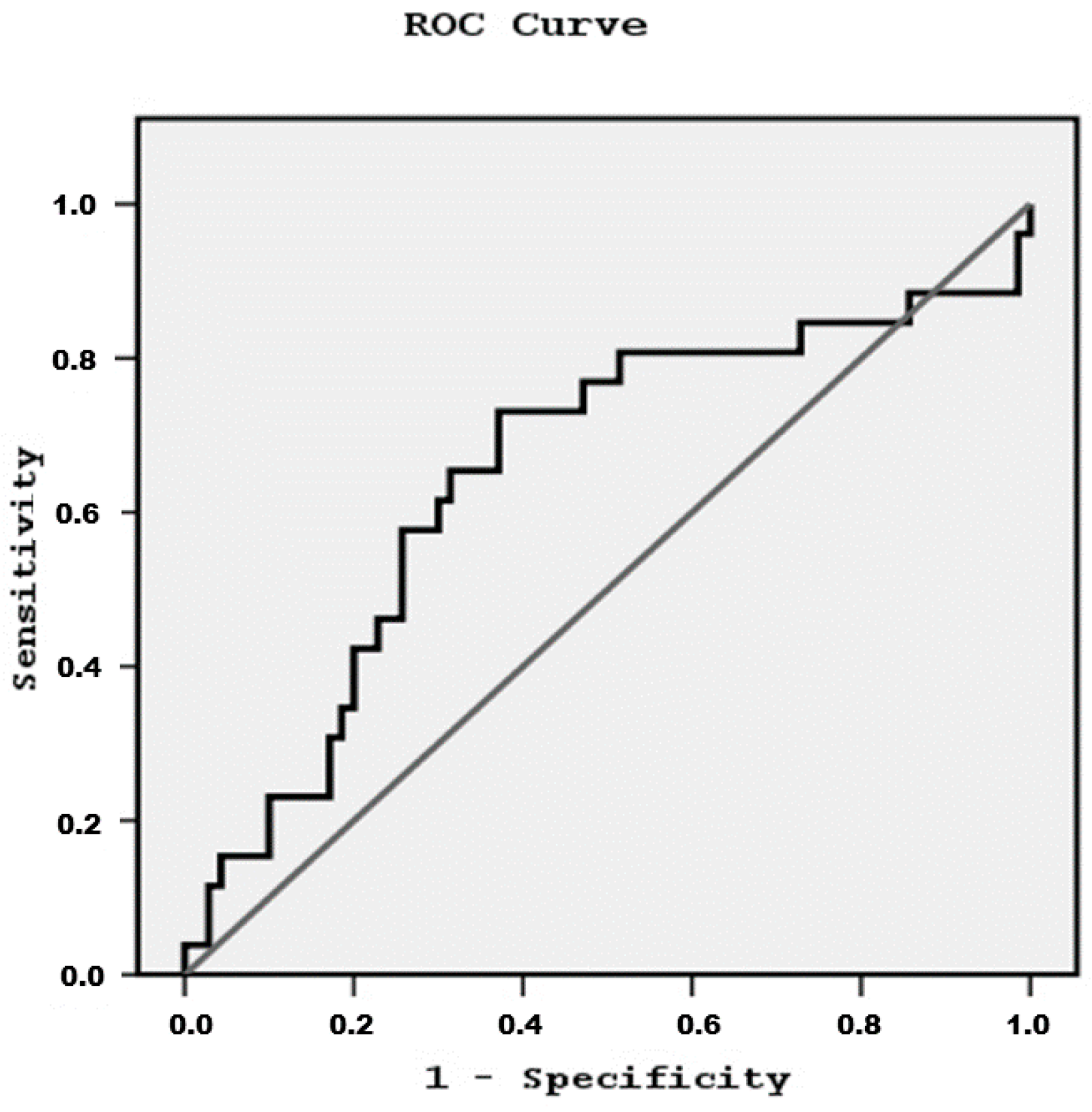
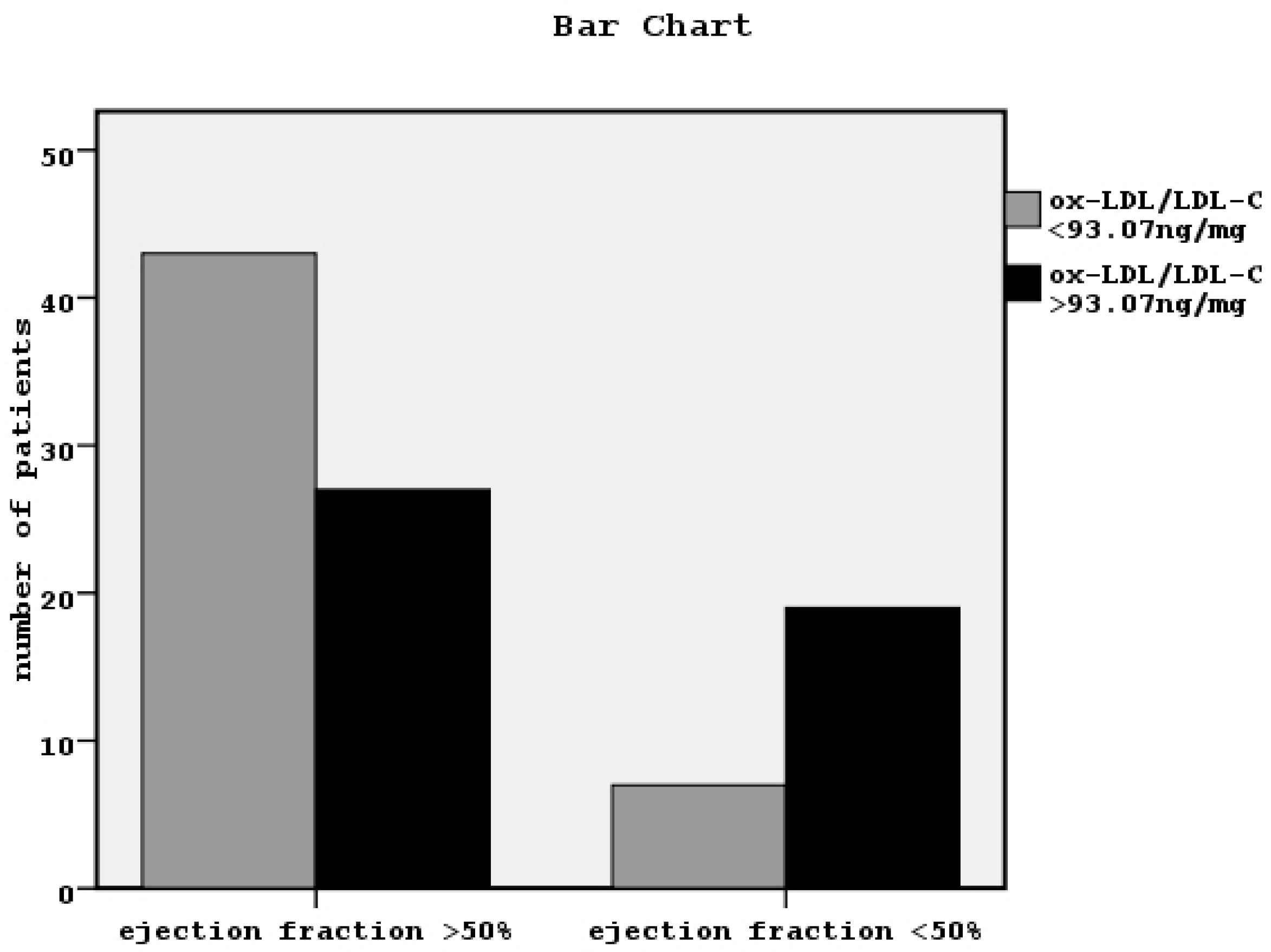
| OxLDL/LDL (ng/mg) | 58.9 * | 44.6 | 0.02 |
| Albumin (gr/dL) | 43.8 | 50.2 | 0.3 |
| Glucose (mg/dL) | 95.03 ± 20.9 | 96.6 ± 22.9 | 0.7 |
| Insulin (μU/mL) | 44.7 | 49.9 | 0.4 |
| HOMA-IR (mmol/L) | 44.9 | 49.8 | 0.5 |
| hsCRP (mg/L) | 12.06 ± 5.4* | 7.4 ± 5.7 | 0.001 |
| MCP-1 (pg/mL) | 51.3 | 41.04 | 0.1 |
| TNF-α (pg/mL) | 50.06 | 44.3 | 0.3 |
| i-PTH (pg/mL) | 47.3 | 48.9 | 0.8 |
| SBP (mmHg) | 135.1 ± 24.6 | 130.4 ± 23.5 | 0.4 |
| MBP (mmHg) | 99.4 ± 14.8 | 97.2 ± 13.6 | 0.5 |
| c-fPWV (m/s) | 12.04 ± 1.9 * | 11.02 ± 1.7 | 0.01 |
| Augmentation index (Aix, %) | 25.04 ± 2.2 | 23.8 ± 2.3 | 0.03 |
| Pulse pressure (PP, mmHg) | 64.5 ± 22.7 * | 54.4 ± 19.1 | 0.03 |
| ABI | ±0.5 | ±0.4 | 0.4 |
| EF (%) | 25.8 ± 2.7 * | 58.4 ± 3.07 | 0.001 |
| E/A ratio | 31.5 * | 54.8 | 0.001 |
| Thickness of interventricular septum (mm) | 13.7 ± 2.0 * | 12.1 ± 2.0 | 0.001 |
| Characteristic | p-Value | Odds Ratio | Confidence Interval |
|---|---|---|---|
| age | 0.01 | 1.06 | 1.01–1.11 |
| gender | 0.8 | 1.1 | 0.3–3.8 |
| Diabetes mellitus | 0.6 | 1.7 | 0.2–11.3 |
| hypertension | 0.1 | 0.4 | 0.1–1.4 |
| smoking | 0.4 | 1.9 | 0.4–8.6 |
| spKt/V for urea | 0.9 | 0.9 | 0.2–4.5 |
| nPCR | 0.2 | 0.5 | 0.2–1.5 |
| Vitamin D therapy | 0.02 | 0.2 | 0.06–0.8 |
| Ox-LDL/LDL-C | 0.004 | 6.2 | 1.8–21.2 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raikou, V.; Kardalinos, V.; Kyriaki, D. Oxidized Low-Density Lipoprotein Serum Concentrations and Cardiovascular Morbidity in End Stage of Renal Disease. J. Cardiovasc. Dev. Dis. 2018, 5, 35. https://doi.org/10.3390/jcdd5030035
Raikou V, Kardalinos V, Kyriaki D. Oxidized Low-Density Lipoprotein Serum Concentrations and Cardiovascular Morbidity in End Stage of Renal Disease. Journal of Cardiovascular Development and Disease. 2018; 5(3):35. https://doi.org/10.3390/jcdd5030035
Chicago/Turabian StyleRaikou, Vaia, Vasilios Kardalinos, and Despina Kyriaki. 2018. "Oxidized Low-Density Lipoprotein Serum Concentrations and Cardiovascular Morbidity in End Stage of Renal Disease" Journal of Cardiovascular Development and Disease 5, no. 3: 35. https://doi.org/10.3390/jcdd5030035
APA StyleRaikou, V., Kardalinos, V., & Kyriaki, D. (2018). Oxidized Low-Density Lipoprotein Serum Concentrations and Cardiovascular Morbidity in End Stage of Renal Disease. Journal of Cardiovascular Development and Disease, 5(3), 35. https://doi.org/10.3390/jcdd5030035





