Depression, Anxiety, and Quality of Life in a Cardiac Rehabilitation Program Without Dedicated Mental Health Resources Post-Myocardial Infarction
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Cardiac Rehabilitation Program
2.3. MH Assessment During CRP
2.4. MH Interventions During CRP
2.5. MH Outcomes After CRP
2.6. Ethics
2.7. Statistical Analysis
3. Results
3.1. Cohort Description
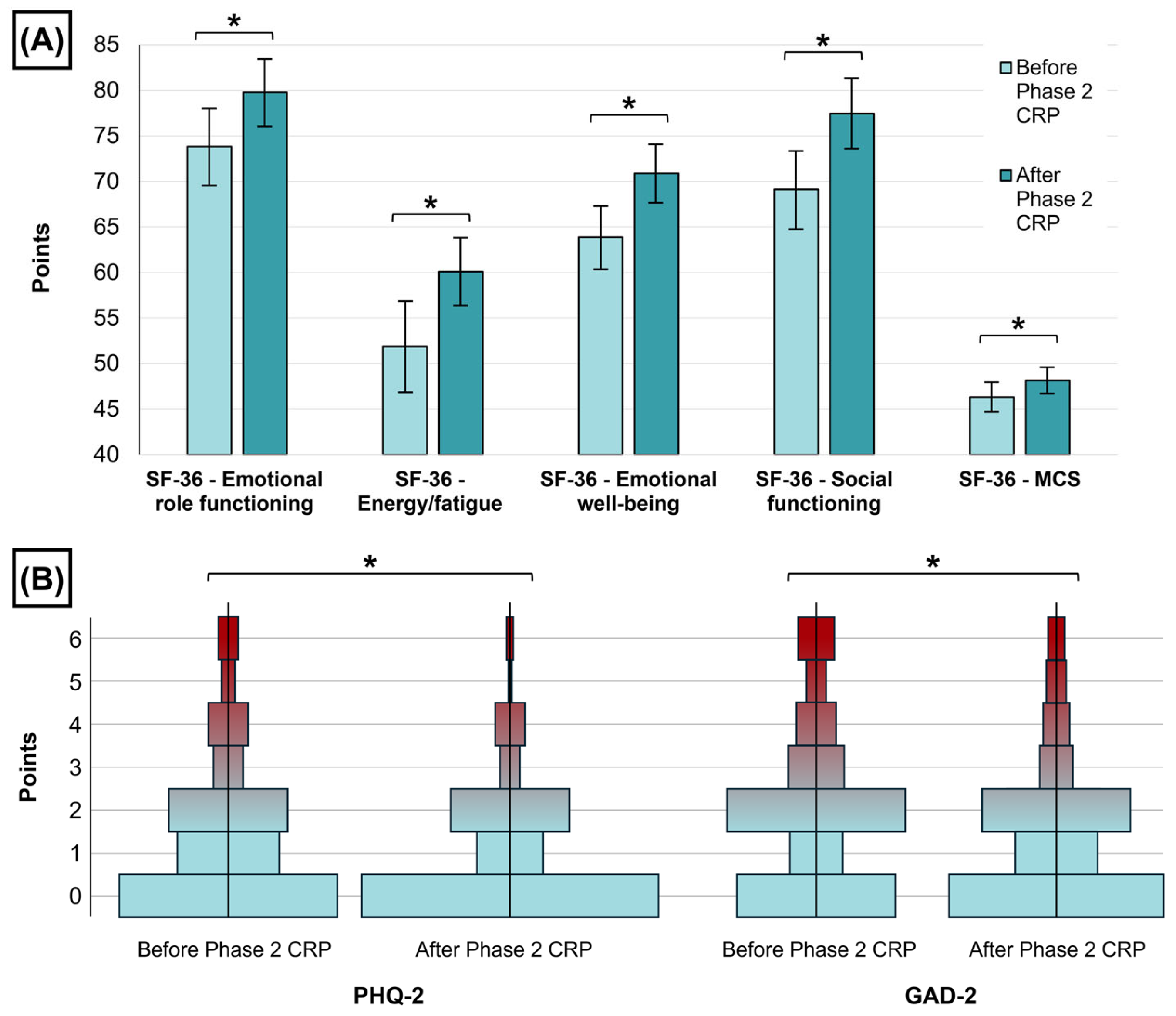
3.2. MH Outcomes Before and After Phase 2 CRP
3.3. Depression and Anxiety Symptoms After Phase 2 CRP
4. Discussion
4.1. Mental Health After MI
4.2. Cardiac Rehabilitation and Mental Health
4.3. MH Interventions During CRPs
4.4. Prioritization of MH Resources During CRP
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| C/CPET | Conventional or Cardiopulmonary Exercise Testing |
| CRP | Cardiac Rehabilitation Program |
| GAD-2 | Generalized Anxiety Disorder 2-item |
| GRACE | Global Registry of Acute Coronary Events |
| IPAQ | International Physical Activity Questionnaire |
| LDL-C | Low-Density Lipoprotein Cholesterol |
| LVEF | Left Ventricular Ejection Fraction |
| MCS | Mental Component Summary |
| MH | Mental Health |
| MI | Myocardial Infarction |
| OMI | Occlusion Myocardial Infarction |
| PHQ-2 | Patient Health Questionnaire 2-item |
| QoL | Quality of Life |
| SF-36 | 36-Item Short Form Survey Instrument |
| SPSS | Statistical Package for the Social Sciences |
| STEMI | ST-segment Elevation Myocardial Infarction |
References
- Martin, S.S.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Barone Gibbs, B.; Beaton, A.Z.; Boehme, A.K.; et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation 2024, 149, E347–E913. [Google Scholar] [CrossRef] [PubMed]
- Lui, J.N.M.; Williams, C.; Keng, M.J.; Hopewell, J.C.; Sammons, E.; Chen, F.; Gray, A.; Bowman, L.; Landray, S.M.J.; Mihaylova, B.; et al. Impact of New Cardiovascular Events on Quality of Life and Hospital Costs in People with Cardiovascular Disease in the United Kingdom and United States. J. Am. Heart Assoc. 2023, 12, e030766. [Google Scholar] [CrossRef] [PubMed]
- Watkins, L.L.; Koch, G.G.; Sherwood, A.; Blumenthal, J.A.; Davidson, J.R.T.; O’Connor, C.; Sketch, M.H. Association of Anxiety and Depression With All-Cause Mortality in Individuals With Coronary Heart Disease. J. Am. Heart Assoc. 2013, 2, e000068. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Zheng, Y.; Ma, J.; Zhang, M.; Zhang, Y.; Liu, X.; Chen, L.; Yang, Q.; Sun, Y.; Wu, J.; et al. Effect of Exercise-Based Cardiac Rehabilitation on Anxiety and Depression in Patients with Myocardial Infarction: A Systematic Review and Meta-Analysis. Heart Lung 2019, 48, 1–7. [Google Scholar] [CrossRef]
- Meijer, A.; Conradi, H.J.; Bos, E.H.; Thombs, B.D.; Van Melle, J.P.; De Jonge, P. Prognostic Association of Depression Following Myocardial Infarction with Mortality and Cardiovascular Events: A Meta-Analysis of 25 Years of Research. Gen. Hosp. Psychiatry 2011, 33, 203–216. [Google Scholar] [CrossRef]
- Sakamoto, M.; Suematsu, Y.; Yano, Y.; Kaino, K.; Teshima, R.; Matsuda, T.; Fujita, M.; Tazawa, R.; Fujimi, K.; Miura, S. Depression and Anxiety Are Associated with Physical Performance in Patients Undergoing Cardiac Rehabilitation: A Retrospective Observational Study. J. Cardiovasc. Dev. Dis. 2022, 9, 21. [Google Scholar] [CrossRef]
- Dibben, G.O.; Faulkner, J.; Oldridge, N.; Rees, K.; Thompson, D.R.; Zwisler, A.-D.; Taylor, R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease: A Meta-Analysis. Eur. Heart J. 2023, 44, 452–469. [Google Scholar] [CrossRef]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the Management of Acute Coronary Syndromes. Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef]
- Virani, S.S.; Newby, L.K.; Arnold, S.V.; Bittner, V.; Brewer, L.C.; Demeter, S.H.; Dixon, D.L.; Fearon, W.F.; Hess, B.; Johnson, H.M.; et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2023, 148, E9–E119. [Google Scholar] [CrossRef]
- Vrints, C.; Andreotti, F.; Koskinas, K.C.; Rossello, X.; Adamo, M.; Ainslie, J.; Banning, A.P.; Budaj, A.; Buechel, R.R.; Chiariello, G.A.; et al. 2024 ESC Guidelines for the Management of Chronic Coronary Syndromes. Eur. Heart J. 2024, 45, 3415–3537. [Google Scholar] [CrossRef]
- Mansilla-Chacón, M.; Gómez-Urquiza, J.L.; Martos-Cabrera, M.B.; Albendín-García, L.; Romero-Béjar, J.L.; Cañadas-De La Fuente, G.A.; Suleiman-Martos, N. Effects of Supervised Cardiac Rehabilitation Programmes on Quality of Life among Myocardial Infarction Patients: A Systematic Review and Meta-Analysis. J. Cardiovasc. Dev. Dis. 2021, 8, 166. [Google Scholar] [CrossRef] [PubMed]
- Stefanakis, M.; Batalik, L.; Antoniou, V.; Pepera, G. Safety of Home-Based Cardiac Rehabilitation: A Systematic Review. Heart Lung 2022, 55, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.S.; Dalal, H.M.; McDonagh, S.T.J. The Role of Cardiac Rehabilitation in Improving Cardiovascular Outcomes. Nat. Rev. Cardiol. 2021, 19, 180–194. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.W.; Serber, E.R.; Kuhn, T. Psychosocial Management in Cardiac Rehabilitation: Current Practices, Recommendations, and Opportunities. Prog. Cardiovasc. Dis. 2022, 73, 76–83. [Google Scholar] [CrossRef]
- Brown, T.M.; Pack, Q.R.; Aberegg, E.; Brewer, L.C.; Ford, Y.R.; Forman, D.E.; Gathright, E.C.; Khadanga, S.; Ozemek, C.; Thomas, R.J.; et al. Core Components of Cardiac Rehabilitation Programs: 2024 Update: A Scientific Statement From the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation 2024, 150, e328–e347. [Google Scholar] [CrossRef]
- Bush, M.; Evenson, K.R.; Aylward, A.; Cyr, J.M.; Kucharska-Newton, A. Psychosocial Services Provided by Licensed Cardiac Rehabilitation Programs. Front. Rehabil. Sci. 2023, 4, 1093086. [Google Scholar] [CrossRef]
- Jackson, A.C.; Le Grande, M.R.; Higgins, R.O.; Rogerson, M.; Murphy, B.M. Psychosocial Screening and Assessment Practice within Cardiac Rehabilitation: A Survey of Cardiac Rehabilitation Coordinators in Australia. Heart Lung Circ. 2017, 26, 64–72. [Google Scholar] [CrossRef]
- Cahill, M.C.; Bilanovic, A.; Kelly, S.; Bacon, S.; Grace, S.L. Screening for Depression in Cardiac Rehabilitation: A REVIEW. J. Cardiopulm. Rehabil. Prev. 2015, 35, 225–230. [Google Scholar] [CrossRef]
- McKenzie, K.M.; Park, L.K.; Lenze, E.J.; Montgomery, K.; Rashdi, S.; Deych, E.; Stranczek, N.A.; McKenzie, E.J.; Rich, M.W.; Garr Barry, V.; et al. A Prospective Cohort Study of the Impact of Outpatient Intensive Cardiac Rehabilitation on Depression and Cardiac Self-Efficacy. Am. Heart J. Plus Cardiol. Res. Pract. 2022, 13, 100100. [Google Scholar] [CrossRef]
- Levis, B.; Sun, Y.; He, C.; Wu, Y.; Krishnan, A.; Bhandari, P.M.; Neupane, D.; Imran, M.; Brehaut, E.; Negeri, Z.; et al. Accuracy of the PHQ-2 Alone and in Combination With the PHQ-9 for Screening to Detect Major Depression: Systematic Review and Meta-Analysis. JAMA 2020, 323, 2290. [Google Scholar] [CrossRef]
- Hlynsson, J.I.; Carlbring, P. Diagnostic Accuracy and Clinical Utility of the PHQ-2 and GAD-2: A Comparison with Long-Format Measures for Depression and Anxiety. Front. Psychol. 2024, 15, 1259997. [Google Scholar] [CrossRef] [PubMed]
- Staples, L.G.; Dear, B.F.; Gandy, M.; Fogliati, V.; Fogliati, R.; Karin, E.; Nielssen, O.; Titov, N. Psychometric Properties and Clinical Utility of Brief Measures of Depression, Anxiety, and General Distress: The PHQ-2, GAD-2, and K-6. Gen. Hosp. Psychiatry 2019, 56, 13–18. [Google Scholar] [CrossRef] [PubMed]
- García-Sánchez, E.; Santamaría-Peláez, M.; Benito Figuerola, E.; Carballo García, M.J.; Chico Hernando, M.; García García, J.M.; González-Bernal, J.J.; González-Santos, J. Comparison of SF-36 and RAND-36 in Cardiovascular Diseases: A Reliability Study. J. Clin. Med. 2024, 13, 6106. [Google Scholar] [CrossRef] [PubMed]
- Laucis, N.C.; Hays, R.D.; Bhattacharyya, T. Scoring the SF-36 in Orthopaedics: A Brief Guide. J. Bone Jt. Surg. 2015, 97, 1628–1634. [Google Scholar] [CrossRef]
- López-García, E.; Banegas, J.R.; Pérez-Regadera, A.G.; Gutiérrez-Fisac, J.L.; Alonso, J.; Rodríguez-Artalejo, F. Valores de referencia de la versión española del Cuestionario de Salud SF-36 en población adulta de más de 60 años. Med. Clínica 2003, 120, 568–573. [Google Scholar] [CrossRef]
- Huber, A.; Oldridge, N.; Höfer, S. International SF-36 Reference Values in Patients with Ischemic Heart Disease. Qual. Life Res. 2016, 25, 2787–2798. [Google Scholar] [CrossRef]
- Inicio—Pacientes—Aula Abierta RC. Available online: https://pacientes.aularc.es/ (accessed on 4 January 2025).
- Rao, A.; Zecchin, R.; Newton, P.; Phillips, J.; DiGiacomo, M.; Denniss, A.; Hickman, L. The Prevalence and Impact of Depression and Anxiety in Cardiac Rehabilitation: A Longitudinal Cohort Study. Eur. J. Prev. Cardiol. 2020, 27, 478–489. [Google Scholar] [CrossRef]
- Sreenivasan, J.; Khan, M.S.; Khan, S.U.; Hooda, U.; Aronow, W.S.; Panza, J.A.; Levine, G.N.; Commodore-Mensah, Y.; Blumenthal, R.S.; Michos, E.D. Mental Health Disorders among Patients with Acute Myocardial Infarction in the United States. Am. J. Prev. Cardiol. 2021, 5, 100133. [Google Scholar] [CrossRef]
- Feng, L.; Li, L.; Liu, W.; Yang, J.; Wang, Q.; Shi, L.; Luo, M. Prevalence of Depression in Myocardial Infarction: A PRISMA-Compliant Meta-Analysis. Medicine 2019, 98, e14596. [Google Scholar] [CrossRef]
- Roest, A.M.; Martens, E.J.; Denollet, J.; De Jonge, P. Prognostic Association of Anxiety Post Myocardial Infarction With Mortality and New Cardiac Events: A Meta-Analysis. Psychosom. Med. 2010, 72, 563–569. [Google Scholar] [CrossRef]
- Lian, Y.; Xiang, J.; Wang, X.; Kaminga, A.C.; Chen, W.; Lai, Z.; Dai, W.; Yang, J. Prevalence of Moderate to Severe Anxiety Symptoms among Patients with Myocardial Infarction: A Meta-Analysis. Psychiatr. Q. 2022, 93, 161–180. [Google Scholar] [CrossRef] [PubMed]
- Feng, H.-P.; Chien, W.-C.; Cheng, W.-T.; Chung, C.-H.; Cheng, S.-M.; Tzeng, W.-C. Risk of Anxiety and Depressive Disorders in Patients with Myocardial Infarction: A Nationwide Population-Based Cohort Study. Medicine 2016, 95, e4464. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, S.H.; Ghaemian, A.; Mehdizadeh, E.; Ashraf, H. Contribution of Depression and Anxiety to Impaired Quality of Life in Survivors of Myocardial Infarction. Int. J. Psychiatry Clin. Pract. 2014, 18, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Garrels, E.; Kainth, T.; Silva, B.; Yadav, G.; Gill, G.; Salehi, M.; Gunturu, S. Pathophysiological Mechanisms of Post-Myocardial Infarction Depression: A Narrative Review. Front. Psychiatry 2023, 14, 1225794. [Google Scholar] [CrossRef]
- Lapa, M.E.; Swabe, G.M.; Rollman, B.L.; Muldoon, M.F.; Thurston, R.C.; Magnani, J.W. Assessment of Depression and Adherence to Guideline-Directed Medical Therapies Following Percutaneous Coronary Intervention. JAMA Netw. Open 2022, 5, e2246317. [Google Scholar] [CrossRef]
- Ashour, A.M.; Masa’deh, R.; Hamaideh, S.H.; Elshatarat, R.A.; Yacoub, M.I.; Almagharbeh, W.T.; Alhejaili, A.A.; Alshahrani, B.D.; Sobeh, D.E.; Eltayeb, M.M. Examining the Influence of Anxiety and Depression on Medication Adherence among Patients Diagnosed with Acute Myocardial Infarction. BMC Psychol. 2024, 12, 473. [Google Scholar] [CrossRef]
- Ambrosetti, M.; Abreu, A.; Corrà, U.; Davos, C.H.; Hansen, D.; Frederix, I.; Iliou, M.C.; Pedretti, R.F.E.; Schmid, J.-P.; Vigorito, C.; et al. Secondary Prevention through Comprehensive Cardiovascular Rehabilitation: From Knowledge to Implementation. 2020 Update. A Position Paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2021, 28, 460–495. [Google Scholar] [CrossRef]
- Flygare, O.; Boberg, J.; Rück, C.; Hofmann, R.; Leosdottir, M.; Mataix-Cols, D.; De La Cruz, L.F.; Richman, P.; Wallert, J. Association of Anxiety or Depression with Risk of Recurrent Cardiovascular Events and Death after Myocardial Infarction: A Nationwide Registry Study. Int. J. Cardiol. 2023, 381, 120–127. [Google Scholar] [CrossRef]
- Leissner, P.; Held, C.; Humphries, S.; Rondung, E.; Olsson, E.M.G. Association of Anxiety and Recurrent Cardiovascular Events: Investigating Different Aspects of Anxiety. Eur. J. Cardiovasc. Nurs. 2024, 23, 720–727. [Google Scholar] [CrossRef]
- Cha, S.; Chang, W.K.; Lee, K.; Han, K.; Paik, N.-J.; Kim, W.-S. Prevalence and Impact of Depression and Anxiety among Older Myocardial Infarction Survivors: A Nationwide Cohort Study. J. Affect. Disord. 2024, 354, 408–415. [Google Scholar] [CrossRef]
- Kim, J.-M.; Stewart, R.; Kim, J.-W.; Kang, H.-J.; Kim, S.-W.; Shin, I.-S.; Hong, Y.J.; Ahn, Y.; Jeong, M.H.; Yoon, J.-S. Impact of Depression at Early and Late Phases Following Acute Coronary Syndrome on Long-Term Cardiac Outcomes. J. Affect. Disord. 2020, 260, 592–596. [Google Scholar] [CrossRef]
- Wen, Y.; Yang, Y.; Shen, J.; Luo, S. Anxiety and Prognosis of Patients with Myocardial Infarction: A Meta-analysis. Clin. Cardiol. 2021, 44, 761–770. [Google Scholar] [CrossRef] [PubMed]
- Helmark, C.; Harrison, A.; Pedersen, S.S.; Doherty, P. Systematic Screening for Anxiety and Depression in Cardiac Rehabilitation—Are We There Yet? Int. J. Cardiol. 2022, 352, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Dibben, G.; Faulkner, J.; Oldridge, N.; Rees, K.; Thompson, D.R.; Zwisler, A.-D.; Taylor, R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease. Cochrane Database Syst. Rev. 2021, 2021, CD001800. [Google Scholar] [CrossRef]
- Bravo-Escobar, R.; González-Represas, A.; Gómez-González, A.M.; Heredia-Torres, Á. Effectiveness of E-Health Cardiac Rehabilitation Program on Quality of Life Associated with Symptoms of Anxiety and Depression in Moderate-Risk Patients. Sci. Rep. 2021, 11, 3760. [Google Scholar] [CrossRef]
- Anderson, L.; Sharp, G.A.; Norton, R.J.; Dalal, H.; Dean, S.G.; Jolly, K.; Cowie, A.; Zawada, A.; Taylor, R.S. Home-Based versus Centre-Based Cardiac Rehabilitation. Cochrane Database Syst. Rev. 2017, 2017, CD007130. [Google Scholar] [CrossRef]
- Wrzeciono, A.; Mazurek, J.; Cieślik, B.; Kiper, P.; Gajda, R.; Szczepańska-Gieracha, J. Psychologically-Enhanced Cardiac Rehabilitation for Psychological and Functional Improvement in Patients with Cardiovascular Disease: A Systematic Review with Meta-Analysis and Future Research Directions. Physiotherapy 2024, 125, 101412. [Google Scholar] [CrossRef]
- Albus, C.; Herrmann-Lingen, C.; Jensen, K.; Hackbusch, M.; Münch, N.; Kuncewicz, C.; Grilli, M.; Schwaab, B.; Rauch, B.; German Society of Cardiovascular Prevention & Rehabilitation (DGPR). Additional Effects of Psychological Interventions on Subjective and Objective Outcomes Compared with Exercise-Based Cardiac Rehabilitation Alone in Patients with Cardiovascular Disease: A Systematic Review and Meta-Analysis. Eur. J. Prev. Cardiol. 2019, 26, 1035–1049. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Sherwood, A.; Smith, P.J.; Watkins, L.; Mabe, S.; Kraus, W.E.; Ingle, K.; Miller, P.; Hinderliter, A. Enhancing Cardiac Rehabilitation With Stress Management Training: A Randomized, Clinical Efficacy Trial. Circulation 2016, 133, 1341–1350. [Google Scholar] [CrossRef]
- Wells, A.; Reeves, D.; Capobianco, L.; Heal, C.; Davies, L.; Heagerty, A.; Doherty, P.; Fisher, P. Improving the Effectiveness of Psychological Interventions for Depression and Anxiety in Cardiac Rehabilitation: PATHWAY—A Single-Blind, Parallel, Randomized, Controlled Trial of Group Metacognitive Therapy. Circulation 2021, 144, 23–33. [Google Scholar] [CrossRef]
- Zhamaliyeva, L.M.; Zhamankulova, D.G.; Abenova, N.A.; Koshmaganbetova, G.K. Educational Intervention Effects on Depression and Anxiety in Patients after Myocardial Infarction: A Randomized Controlled Trial. J. Cardiovasc. Dev. Dis. 2023, 10, 267. [Google Scholar] [CrossRef] [PubMed]
- Zambrano, J.; Celano, C.M.; Januzzi, J.L.; Massey, C.N.; Chung, W.; Millstein, R.A.; Huffman, J.C. Psychiatric and Psychological Interventions for Depression in Patients With Heart Disease: A Scoping Review. J. Am. Heart Assoc. 2020, 9, e018686. [Google Scholar] [CrossRef] [PubMed]
- Blumenthal, J.A.; Rozanski, A. Exercise as a Therapeutic Modality for the Prevention and Treatment of Depression. Prog. Cardiovasc. Dis. 2023, 77, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Murphy, B.; Le Grande, M.; Alvarenga, M.; Worcester, M.; Jackson, A. Anxiety and Depression After a Cardiac Event: Prevalence and Predictors. Front. Psychol. 2020, 10, 3010. [Google Scholar] [CrossRef]
- Murphy, B.M.; Higgins, R.O.; Shand, L.; Page, K.; Holloway, E.; Le Grande, M.R.; Jackson, A.C. Improving Health Professionals’ Self-Efficacy to Support Cardiac Patients’ Emotional Recovery: The ‘Cardiac Blues Project’. Eur. J. Cardiovasc. Nurs. 2017, 16, 143–149. [Google Scholar] [CrossRef]


| All Patients (n = 164) | Negative Depression/Anxiety Screening After Phase 2 CRP (n = 131) | Positive Depression/Anxiety Screening After Phase 2 CRP (n = 33) | p-Value | |
|---|---|---|---|---|
| Clinical variables | ||||
| Age (years) | 61.35 ± 10.76 | 62.55 ± 11.05 | 56.6 ± 8.05 | 0.004 |
| Male sex (%) | 142 (86.6) | 115 (87.8) | 27 (81.8) | 0.37 |
| Hypercholesterolemia (%) | 147 (89.6) | 116 (88.5) | 31 (93.9) | 0.36 |
| Hypertension (%) | 90 (54.9) | 73 (55.7) | 17 (51.5) | 0.66 |
| Diabetes mellitus (%) | 33 (20.1) | 29 (22.1) | 4 (12.1) | 0.2 |
| Killip class ≥2 (%) | 45 (27.4) | 38 (29) | 7 (21.2) | 0.37 |
| GRACE risk score | 115.85 ± 29.25 | 116.68 ± 29.8 | 112.58 ± 27.11 | 0.47 |
| Infarct location | 0.33 | |||
| Anterior (%) | 72 (43.9) | 59 (45) | 13 (39.4) | |
| Inferior (%) | 73 (44.5) | 57 (43.5) | 16 (48.5) | |
| Lateral (%) | 12 (7.3) | 8 (6.1) | 4 (12.1) | |
| OMI (%) | 7 (4.3) | 7 (5.3) | 0 (0) | |
| LVEF (%) | 52.43 ± 10.55 | 52.5 ± 10.6 | 52.12 ± 10.5 | 0.85 |
| LVEF <50% (%) | 56 (34.1) | 45 (34.4) | 11 (33.3) | 0.91 |
| Risk stratification for CRP (%) | 0.47 | |||
| Low risk | 60 (36.6) | 48 (36.6) | 12 (36.4) | |
| Intermediate risk | 47 (28.7) | 40 (30.5) | 7 (21.2) | |
| High risk | 57 (34.8) | 43 (32.8) | 14 (42.4) | |
| Exercise training modality during CRP | 0.08 | |||
| Ambulatory training (%) | 132 (80.5) | 109 (83.2) | 23 (69.7) | |
| Supervised in-hospital training (%) | 32 (19.5) | 22 (16.8) | 10 (30.3) | |
| Cardiovascular risk factors | ||||
| Smoking habit before CRP (%) | 83 (50.6) | 65 (49.6) | 18 (54.5) | 0.61 |
| Smoking habit after CRP (%) | 9 (5.5) | 7 (5.3) | 2 (6.1) | 0.87 |
| Systolic pressure (mmHg) | ||||
| Before CRP | 125.05 ± 16.08 | 125.53 ± 16.19 | 123.15 ± 15.71 | 0.45 |
| After CRP | 114.96 ± 10.08 | 115.29 ± 10.03 | 113.64 ± 10.33 | 0.4 |
| Mean change | −10.09 ± 14 * | −10.24 ± 13.35 * | −9.52 ± 16.54 * | 0.79 |
| LDL-C (mg/dL) | ||||
| Before CRP | 101.85 ± 13.95 | 99.24 ± 34.31 | 111.88 ± 42.66 | 0.08 |
| After CRP | 44.43 ± 13.95 | 43.84 ± 13.37 | 46.76 ± 16.05 | 0.28 |
| Mean change | −57.29 ± 36.43 * | −55.26 ± 34.67 * | −65.12 ± 42.22 * | 0.17 |
| LDL-C <55 mg/dL after CRP (%) | 136 (82.9) | 112 (85.5) | 24 (72.7) | 0.08 |
| Weight (kg) | ||||
| Before CRP | 80.7 ± 15.18 | 80.74 ± 15.69 | 80.55 ± 13.21 | 0.95 |
| After CRP | 79.15 ± 14.55 | 79.23 ± 14.93 | 78.8 ± 13.18 | 0.88 |
| Mean change | −1.56 ± 5.99 * | −1.51 ± 5.58 * | −1.75 ± 7.49 | 0.84 |
| BMI | ||||
| Before CRP | 27.72 ± 4.62 | 27.67 ± 4.6 | 27.97 ± 4.76 | 0.73 |
| After CRP | 27.21 ± 4.45 | 27.15 ± 4.4 | 27.42 ± 4.72 | 0.76 |
| Mean change | −0.52 ± 2.02 * | −0.51 ± 1.88 * | −0.55 ± 2.53 | 0.92 |
| BMI ≥30 before CRP (%) | 39 (23.8) | 30 (22.9) | 9 (27.3) | 0.6 |
| BMI ≥30 after CRP (%) | 31 (18.9) | 26 (19.8) | 5 (15.2) | 0.54 |
| PREDIMED ≥8 points before CRP (%) | 118 (72) | 93 (71) | 25 (75.8) | 0.59 |
| PREDIMED ≥8 points after CRP (%) | 143 (87.2) | 113 (86.3) | 30 (90.9) | 0.48 |
| Therapeutic adherence before CRP (4 points in Morisky-Green, %) | 130 (79.3) | 104 (79.4) | 26 (78.8) | 0.94 |
| Therapeutic adherence after CRP (4 points in Morisky-Green, %) | 151 (92.1) | 120 (91.6) | 31 (93.9) | 0.66 |
| MH and QoL outcomes | ||||
| Previous history of anxiety | 22 (13.4) | 14 (10.7) | 8 (24.2) | 0.04 |
| Previous history of depression | 13 (7.9) | 7 (5.3) | 96 (18.2) | 0.02 |
| SF-36—Emotional role functioning (points) | ||||
| Before CRP | 73.83 ± 27.98 | 78.37 ± 25.59 | 55.81 ± 30.16 | <0.001 |
| After CRP | 79.78 ± 24.23 | 86.39 ± 18.67 | 53.54 ± 26.19 | <0.001 |
| Mean change | 5.94 ± 27.98 * | 8.01 ± 27.67 * | −2.27 ± 28.13 | 0.06 |
| SF-36—Energy/fatigue (points) | ||||
| Before CRP | 51.88 ± 32.98 | 56.69 ± 33.72 | 32.77 ± 21.2 | <0.001 |
| After CRP | 60.12 ± 24.42 | 66.48 ± 20.02 | 34.86 ± 24.22 | <0.001 |
| Mean change | 8.24 ± 29.57 * | 9.79 ± 31.62 * | 2.09 ± 18.54 | 0.18 |
| SF-36—Emotional well-being (points) | ||||
| Before CRP | 63.87 ± 23.03 | 68.17 ± 21.68 | 46.82 ± 20.42 | <0.001 |
| After CRP | 70.88 ± 21.15 | 77.71 ± 16.26 | 43.79 ± 16.01 | <0.001 |
| Mean change | 7.01 ± 22.31 * | 9.54 ± 22.39 * | −3.03 ± 19.2 | 0.004 |
| SF-36—Social functioning (points) | ||||
| Before CRP | 69.13 ± 28.19 | 73.38 ± 26.47 | 52.27 ± 28.89 | <0.001 |
| After CRP | 77.44 ± 25.34 | 84.06 ± 20.04 | 51.14 ± 27.31 | <0.001 |
| Mean change | 8.31 ± 25 * | 10.69 ± 27.87 * | −1.14 ± 31.15 | 0.04 |
| SF-36—Mental component summary (MCS) | ||||
| Before CRP | 46.31 ± 10.64 | 48.21 ± 10.38 | 38.77 ± 8.1 | <0.001 |
| After CRP | 48.16 ± 9.51 | 50.94 ± 7.62 | 37.1 ± 8.18 | <0.001 |
| Mean change | 1.85 ± 10.23 * | 2.73 ± 10.65 * | −1.67 ± 7.5 | 0.03 |
| PHQ-2 (points) | ||||
| Before CRP | 1 [0, 2] | 1 [0, 2] | 2 [1, 4] | <0.001 |
| After CRP | 0 [0, 2] | 0 [0, 1] | 3 [2, 4] | <0.001 |
| Median change | 0 [0, −1] * | 0 [0, −1] * | 0 [1, −1] | 0.03 |
| GAD-2 (points) | ||||
| Before CRP | 2 [0, 3] | 2 [0, 2] | 3 [2, 5] | <0.001 |
| After CRP | 1 [0, 2] | 1 [0, 2] | 4 [3, 5] | <0.001 |
| Median change | 0 [0, −1] * | 0 [0, −2] * | 0 [2, −1] | 0.005 |
| Physical fitness variables | ||||
| IPAQ (METS/week) | ||||
| Before CRP | 1386 [668.25–2748.75] | 1386 [693–2772] | 1188 [495–2722.5] | 0.23 |
| After CRP | 3662 [2106–6484.5] | 4005 [2331–7074] | 2772 [1713–5359.5] | 0.02 |
| Median change | 1845 [502.5–4370.25] * | 2148 [513–4599] * | 1374 [406–2986.5] * | 0.09 |
| Peak VO2 (ml/kg/min) | ||||
| Before CRP | 25.93 ± 9.17 | 25.71 ± 8.95 | 26.79 ± 10.11 | 0.55 |
| After CRP | 30.05 ± 10.36 | 30.07 ± 10.46 | 29.95 ± 10.13 | 0.95 |
| Mean change | 4.12 ± 5.25 * | 4.36 ± 5.2 * | 3.16 ± 5.42 * | 0.24 |
| Psychological and psychiatric therapy before Phase 2 CRP | ||||
| Psychotherapy | 8 (4.9) | 5 (3.8) | 3 (9.1) | 0.21 |
| Psychiatric follow-up | 8 (4.9) | 6 (4.6) | 2 (6.1) | 0.72 |
| Anxiolytic pharmacotherapy | 19 (11.6) | 16 (12.2) | 3 (9.1) | 0.62 |
| Antidepressant pharmacotherapy | 16 (9.8) | 11 (8.4) | 5 (15.2) | 0.24 |
| Psychological and psychiatric therapy after Phase 2 CRP | ||||
| Psychotherapy | 8 (4.9) | 3 (2.3) | 5 (15.2) | 0.002 |
| Psychiatric follow-up | 9 (5.5) | 4 (3.1) | 5 (15.2) | 0.006 |
| Anxiolytic pharmacotherapy | 31 (18.9) | 20 (15.3) | 11 (33.3) | 0.02 |
| Antidepressant pharmacotherapy | 28 (17.1) | 15 (11.5) | 13 (39.4) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertolín-Boronat, C.; Marcos-Garcés, V.; Merenciano-González, H.; Martínez Mas, M.L.; Climent Alberola, J.I.; Perez, N.; López-Bueno, L.; Esteban Argente, M.C.; Valls Reig, M.; Arizón Benito, A.; et al. Depression, Anxiety, and Quality of Life in a Cardiac Rehabilitation Program Without Dedicated Mental Health Resources Post-Myocardial Infarction. J. Cardiovasc. Dev. Dis. 2025, 12, 92. https://doi.org/10.3390/jcdd12030092
Bertolín-Boronat C, Marcos-Garcés V, Merenciano-González H, Martínez Mas ML, Climent Alberola JI, Perez N, López-Bueno L, Esteban Argente MC, Valls Reig M, Arizón Benito A, et al. Depression, Anxiety, and Quality of Life in a Cardiac Rehabilitation Program Without Dedicated Mental Health Resources Post-Myocardial Infarction. Journal of Cardiovascular Development and Disease. 2025; 12(3):92. https://doi.org/10.3390/jcdd12030092
Chicago/Turabian StyleBertolín-Boronat, Carlos, Víctor Marcos-Garcés, Héctor Merenciano-González, María Luz Martínez Mas, Josefa Inés Climent Alberola, Nerea Perez, Laura López-Bueno, María Concepción Esteban Argente, María Valls Reig, Ana Arizón Benito, and et al. 2025. "Depression, Anxiety, and Quality of Life in a Cardiac Rehabilitation Program Without Dedicated Mental Health Resources Post-Myocardial Infarction" Journal of Cardiovascular Development and Disease 12, no. 3: 92. https://doi.org/10.3390/jcdd12030092
APA StyleBertolín-Boronat, C., Marcos-Garcés, V., Merenciano-González, H., Martínez Mas, M. L., Climent Alberola, J. I., Perez, N., López-Bueno, L., Esteban Argente, M. C., Valls Reig, M., Arizón Benito, A., Payá Rubio, A., Ríos-Navarro, C., de Dios, E., Gavara, J., Jiménez-Navarro, M. F., Chorro, F. J., Sanchis, J., & Bodi, V. (2025). Depression, Anxiety, and Quality of Life in a Cardiac Rehabilitation Program Without Dedicated Mental Health Resources Post-Myocardial Infarction. Journal of Cardiovascular Development and Disease, 12(3), 92. https://doi.org/10.3390/jcdd12030092







