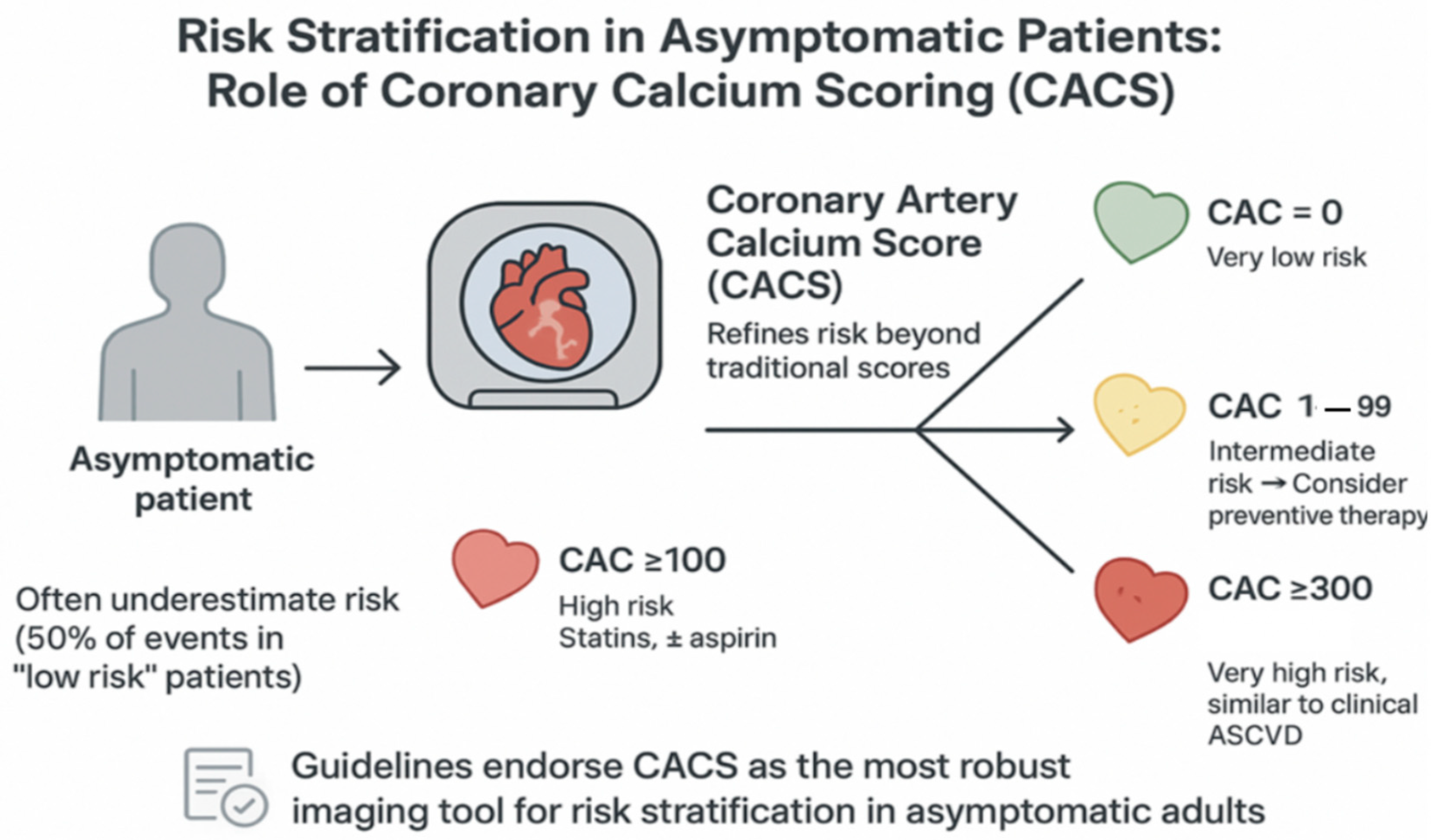
Role of Coronary Artery Calcium Score CT in Risk Stratification of Asymptomatic Individuals
Abstract
1. Introduction
2. Material and Methods
3. Results
3.1. CACS by Cardiac CT for the Screening of Subclinical Atherosclerosis
3.2. Role of CT in Specific Populations
3.3. Value of Coronary Calcium Detection in Non-Coronary CT
3.4. Progression of Coronary Artery Calcification
3.5. Addressing Risk with CACS
3.6. Future Role/Perspectives
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Kannel, W.B.; Schatzkin, A. Sudden death: Lessons from subsets in population studies. J. Am. Coll. Cardiol. 1985, 5 (Suppl. 6), 141B–149B. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez, B.; Fernández-Ortiz, A.; Fernández-Friera, L.; García-Lunar, I.; Andrés, V.; Fuster, V. Progression of Early Subclinical Atherosclerosis (PESA) Study: JACC Focus Seminar 7/8. J. Am. Coll. Cardiol. 2021, 78, 156–179. [Google Scholar] [CrossRef]
- Kim, K.J.; Choi, S.I.; Lee, M.S.; Kim, J.A.; Chun, E.J.; Jeon, C.H. The prevalence and characteristics of coronary atherosclerosis in asymptomatic subjects classified as low risk based on traditional risk stratification algorithm: Assessment with coronary CT angiography. Heart 2013, 99, 1113–1117. [Google Scholar] [CrossRef]
- Neumann, J.T.; de Lemos, J.A.; Apple, F.S.; Leong, D.P. Cardiovascular biomarkers for risk stratification in primary prevention. Eur. Heart J. 2025, 46, ehaf517. [Google Scholar] [CrossRef]
- Mach, F.; Koskinas, K.C.; Roeters van Lennep, J.E.; Tokgözoğlu, L.; Badimon, L.; Baigent, C.; Benn, M.; Binder, C.J.; Catapano, A.L.; De Backer, G.G.; et al. 2025 Focused Update of the 2019 ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur. Heart J. 2025, 46, ehaf190. [Google Scholar] [CrossRef]
- Edvardsen, T.; Asch, F.M.; Davidson, B.; Delgado, V.; DeMaria, A.; Dilsizian, V.; Gaemperli, O.; Garcia, M.J.; Kamp, O.; Lee, D.C.; et al. Non-Invasive Imaging in Coronary Syndromes: Recommendations of the European Association of Cardiovascular Imaging and the American Society of Echocardiography, in Collaboration with the American Society of Nuclear Cardiology, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 2022, 35, 329–354. [Google Scholar] [CrossRef]
- Abdelrahman, K.M.; Chen, M.Y.; Dey, A.K.; Virmani, R.; Finn, A.V.; Khamis, R.Y.; Choi, A.D.; Min, J.K.; Williams, M.C.; Buckler, A.J.; et al. Coronary computed tomography angiography from clinical uses to emerging technologies: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2020, 76, 1226–1243. [Google Scholar] [CrossRef]
- Neglia, D.; Liga, R.; Gimelli, A.; Podlesnikar, T.; Cvijić, M.; Pontone, G.; Miglioranza, M.H.; Guaricci, A.I.; Seitun, S.; Clemente, A.; et al. Use of cardiac imaging in chronic coronary syndromes: The EURECA imaging registry. Eur. Heart J. 2023, 44, 142–158. [Google Scholar] [CrossRef]
- Shreya, D.; Zamora, D.I.; Patel, G.S.; Grossmann, I.; Rodriguez, K.; Soni, M.; Joshi, P.K.; Patel, S.C.; Sange, I. Coronary artery calcium score—A reliable indicator of coronary artery disease? Cureus 2021, 13, e20149. [Google Scholar] [CrossRef]
- Alluri, K.; Joshi, P.H.; Henry, T.S.; Blumenthal, R.S.; Nasir, K.; Blaha, M.J. Scoring of coronary artery calcium scans: History, assumptions, current limitations, and future directions. Atherosclerosis 2015, 239, 109–117. [Google Scholar] [CrossRef]
- Silverman, M.G.; Blaha, M.J.; Krumholz, H.M.; Budoff, M.J.; Blankstein, R.; Sibley, C.T.; Agatston, A.; Blumenthal, R.S.; Nasir, K. Impact of coronary artery calcium on coronary heart disease events in individuals at the extremes of traditional risk factor burden: The Multi-Ethnic Study of Atherosclerosis. Eur. Heart J. 2014, 35, 2232–2241. [Google Scholar] [CrossRef] [PubMed]
- Erbel, R.; Möhlenkamp, S.; Moebus, S.; Schmermund, A.; Lehmann, N.; Stang, A.; Dragano, N.; Grönemeyer, D.; Seibel, R.; Kälsch, H.; et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: The Heinz Nixdorf Recall Study. J. Am. Coll. Cardiol. 2010, 56, 1397–1406. [Google Scholar] [CrossRef] [PubMed]
- Budoff, M.J.; Kinninger, A.; Gransar, H.; Achenbach, S.; Al-Mallah, M.; Bax, J.J.; Berman, D.S.; Cademartiri, F.; Callister, T.Q.; Chang, H.J.; et al. When does a calcium score equate to secondary prevention? Insights from the Multinational CONFIRM Registry. JACC Cardiovasc. Imaging 2017, 10, 397–407. [Google Scholar] [CrossRef]
- Nasir, K.; Rubin, J.; Blaha, M.J.; Shaw, L.J.; Blankstein, R.; Rivera, J.J.; Khan, A.N.; Berman, D.; Raggi, P.; Callister, T.; et al. Interplay of coronary artery calcification and traditional risk factors for the prediction of all-cause mortality in asymptomatic individuals. Circ. Cardiovasc. Imaging 2012, 5, 467–473. [Google Scholar] [CrossRef]
- Le, V.T.; Knight, S.; Min, D.B.; McCubrey, R.O.; Horne, B.D.; Jensen, K.R.; Meredith, K.G.; Mason, S.M.; Lappé, D.L.; Anderson, J.L.; et al. Absence of coronary artery calcium during positron emission tomography stress testing in patients without known coronary artery disease identifies individuals with very low risk of cardiac events. Circ. Cardiovasc. Imaging 2020, 13, e009907. [Google Scholar] [CrossRef]
- Dzaye, O.; Dardari, Z.A.; Cainzos-Achirica, M.; Blankstein, R.; Agatston, A.S.; Duebgen, M.; Yeboah, J.; Szklo, M.; Budoff, M.J.; Lima, J.A.; et al. Warranty period of a calcium score of zero: Comprehensive analysis from MESA. JACC Cardiovasc. Imaging 2021, 14, 990–1002. [Google Scholar] [CrossRef]
- Valenti, V.; Ó Hartaigh, B.; Heo, R.; Cho, I.; Schulman-Marcus, J.; Gransar, H.; Truong, Q.A.; Shaw, L.J.; Knapper, J.; Kelkar, A.A.; et al. A 15-year warranty period for asymptomatic individuals without coronary artery calcium: A prospective follow-up of 9,715 individuals. J. Cardiovasc. Magn. Reson. 2015, 17, 1. [Google Scholar] [CrossRef]
- Matos, D.; Ferreira, A.M.; de Araújo Gonçalves, P.; Gama, F.; Freitas, P.; Guerreiro, S.; Cardoso, G.; Tralhão, A.; Dores, H.; Abecasis, J.; et al. Coronary artery calcium scoring and cardiovascular risk reclassification in patients undergoing coronary computed tomography angiography. Rev. Port. Cardiol. 2021, 40, 25–30. [Google Scholar] [CrossRef]
- Nakao, Y.M.; Miyamoto, Y.; Higashi, M.; Noguchi, T.; Ohishi, M.; Kubota, I.; Tsutsui, H.; Kawasaki, T.; Furukawa, Y.; Yoshimura, M.; et al. Sex differences in impact of coronary artery calcification to predict coronary artery disease. Heart 2018, 104, 1118–1124. [Google Scholar] [CrossRef]
- Fernández-Friera, L.; Peñalvo, J.L.; Fernández-Ortiz, A.; Ibañez, B.; López-Melgar, B.; Laclaustra, M.; Oliva, B.; Mocoroa, A.; Mendiguren, J.; de Vega, V.M.; et al. Prevalence, Vascular Distribution, and Multiterritorial Extent of Subclinical Atherosclerosis in a Middle-Aged Cohort: The PESA (Progression of Early Subclinical Atherosclerosis) Study. Circulation 2015, 131, 2104–2113. [Google Scholar] [CrossRef]
- Dzaye, O.; Razavi, A.C.; Dardari, Z.A.; Shaw, L.J.; Berman, D.S.; Budoff, M.J.; Miedema, M.D.; Nasir, K.; Rozanski, A.; Rumberger, J.A.; et al. Modeling the Recommended Age for Initiating Coronary Artery Calcium Testing Among At-Risk Young Adults. J. Am. Coll. Cardiol. 2021, 78, 1573–1583. [Google Scholar] [CrossRef]
- Budoff, M.J.; Young, R.; Burke, G.; Carr, J.J.; Detrano, R.C.; Folsom, A.R.; Kronmal, R.; Lima, J.A.C.; Liu, K.J.; McClelland, R.L.; et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: The multi-ethnic study of atherosclerosis (MESA). Eur. Heart J. 2018, 39, 2401–2408. [Google Scholar] [CrossRef] [PubMed]
- Elias-Smale, S.E.; Vliegenthart Proença, R.; Koller, M.T.; Kavousi, M.; van Rooij, F.J.A.; Hunink, M.G.; Steyerberg, E.W.; Hofman, A.; Oudkerk, M.; Witteman, J.C. Coronary calcium score improves classification of coronary heart disease risk in the elderly: The Rotterdam Study. J. Am. Coll. Cardiol. 2010, 56, 1407–1414. [Google Scholar] [CrossRef]
- Venkataraman, P.; Stanton, T.; Liew, D.; Huynh, Q.; Nicholls, S.J.; Mitchell, G.K.; Watts, G.F.; Tonkin, A.M.; Marwick, T.H. Coronary artery calcium scoring in cardiovascular risk assessment of people with family histories of early onset coronary artery disease. Med. J. Aust. 2020, 213, 170–177. [Google Scholar] [CrossRef]
- Gallo, A.; de Isla, P.L.; Charriere, S.; Vimont, A.; Alonso, R.; Muniz-Grijalvo, O.; Diaz-Diaz, J.L.; Zambon, D.; Moulin, P.; Bruckert, E.; et al. The added value of coronary calcium score in predicting cardiovascular events in familial hypercholesterolemia. JACC Cardiovasc. Imaging 2021, 14, 2414–2424. [Google Scholar] [CrossRef]
- Christou, G.A.; Deligiannis, A.P.; Kouidi, E.J. The role of cardiac computed tomography in pre-participation screening of mature athletes. Eur. J. Sport Sci. 2022, 22, 636–649. [Google Scholar] [CrossRef]
- Azour, L.; Kadoch, M.A.; Ward, T.J.; Eber, C.D.; Jacobi, A.H. Estimation of cardiovascular risk on routine chest CT: Ordinal coronary artery calcium scoring as an accurate predictor of Agatston score ranges. J. Cardiovasc. Comput. Tomogr. 2017, 11, 8–15. [Google Scholar] [CrossRef]
- Chiles, C.; Duan, F.; Gladish, G.; Ravenel, J.G.; Baginski, S.G.; Snyder, B.; Demello, S.; Desjardins, S.S.; Munden, R.F.; NLST Study Team. Association of coronary artery calcification and mortality in the National Lung Screening Trial: A comparison of three scoring methods. Radiology 2015, 276, 82–90. [Google Scholar] [CrossRef]
- Bastarrika, G.; Alonso, A.; Saiz-Mendiguren, R.; Arias, J.; Cosín, O. Cuantificación de la calcificación coronaria mediante tomografía computarizada torácica de baja dosis sin sincronización cardiaca. Radiología 2010, 52, 30–36. [Google Scholar] [CrossRef]
- Gopal, A.; Nasir, K.; Liu, S.T.; Flores, F.R.; Chen, L.; Budoff, M.J. Coronary calcium progression rates with a zero initial score by electron beam tomography. Int. J. Cardiol. 2007, 117, 227–231. [Google Scholar] [CrossRef]
- Wang, F.M.; Ballew, S.H.; Folsom, A.R.; Wagenknecht, L.E.; Howard, C.M.; Coresh, J.; Budoff, M.J.; Blaha, M.J.; Matsushita, K. Mid- to late-life traditional cardiovascular risk factor exposure and zero coronary artery calcium: The ARIC (Atherosclerosis Risk in Communities) Study. JACC Cardiovasc. Imaging 2025, 18, 973–984. [Google Scholar] [CrossRef]
- Budoff, M.J.; Hokanson, J.E.; Nasir, K.; Shaw, L.J.; Kinney, G.L.; Chow, D.; Demoss, D.; Nuguri, V.; Nabavi, V.; Ratakonda, R.; et al. Progression of coronary artery calcium predicts all-cause mortality. J. Cardiovasc. Comput. Tomogr. 2011, 5, 122–130. [Google Scholar] [CrossRef]
- López-Melgar, B.; Fernández-Friera, L.; Oliva, B.; García-Ruiz, J.M.; Sánchez-Cabo, F.; Bueno, H.; Mendiguren, J.M.; Lara-Pezzi, E.; Andrés, V.; Ibáñez, B.; et al. Short-term progression of multiterritorial subclinical atherosclerosis. J. Am. Coll. Cardiol. 2020, 75, 1617–1627. [Google Scholar] [CrossRef]
- Denissen, S.J.A.M.; van der Aalst, C.M.; Vonder, M.; Oudkerk, M.; de Koning, H.J. Impact of a cardiovascular disease risk screening result on preventive behaviour in asymptomatic participants of the ROBINSCA trial. Eur. J. Prev. Cardiol. 2019, 26, 1313–1322. [Google Scholar] [CrossRef] [PubMed]
- Van der Aalst, C.M.; Denissen, S.J.A.M.; Vonder, M.; Gratama, J.W.C.; Adriaansen, H.J.; Kuijpers, D.; Vliegenthart, R.; Roeters van Lennep, J.E.; van der Harst, P.; Braam, R.L.; et al. Screening for cardiovascular disease risk using traditional risk factor assessment or coronary artery calcium scoring: The ROBINSCA trial. Eur. Heart J. Cardiovasc. Imaging 2020, 21, 1216–1224. [Google Scholar] [CrossRef]
- Hecht, H.S.; Cronin, P.; Blaha, M.J.; Budoff, M.J.; Kazerooni, E.A.; Narula, J.; Yankelevitz, D.; Abbara, S. 2016 SCCT/STR guidelines for coronary artery calcium scoring of noncontrast noncardiac chest CT scans: A report of the Society of Cardiovascular Computed Tomography and Society of Thoracic Radiology. J. Cardiovasc. Comput. Tomogr. 2017, 11, 74–84. [Google Scholar] [CrossRef]
- Ahmadi, A.; Argulian, E.; Leipsic, J.; Newby, D.E.; Narula, J. From subclinical atherosclerosis to plaque progression and acute coronary events: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2019, 74, 1608–1617. [Google Scholar] [CrossRef]
| Study Name | Year | Study Type | Population Included | Study Results |
|---|---|---|---|---|
| Ibáñez et al. [3] | 2021 | Narrative review of the PESA study | 4184 asymptomatic middle age adults (40–54 years) | High prevalence and progression of atherosclerosis even in low risk patients by traditional scores |
| Kim et al. [4] | 2013 | Retrospective observational study | 2133 asymptomatic low risk patients according to NCEP | High prevalence of atherosclerotic disease |
| Silverman et al. [12] | 2014 | Prospective cohort study | 6698 asymptomatic patients from MESA study | >300 UA CACS high risk CACS = 0 UA very low risk |
| Erbel et al. [13] | 2010 | Prospective Population Study | 4487 Germans, 45–75 years, without CVD | CACS improves risk stratification and reclassification. |
| Budoff et al. (CONFIRM) [14] | 2017 | Prospective Multinational Registry | 4511 asymptomatic individuals without CVD, mean age 57.6 years | CACS > 300 risk is comparable to secondary prevention. |
| Nasir et al. [15] | 2012 | Prospective Cohort | 44,052 asymptomatic, mean age 54 years, 34% women, without CVD | CACS predicts all-cause mortality better than traditional risk factors. |
| Le Viet et al. [16] | 2020 | Retrospective Cohort | 5528 patients with no prior history of coronary artery disease | CACS = 0 is associated with an extremely low risk. |
| Dzaye et al. [17] | 2021 | Prospective cohort | 3116 asymptomatic adults study MESA | Very low risk progression in CACS 0 in 5–7 years. |
| Valenti et al. [18] | 2015 | Prospective cohort | 9715 asymptomatic adults | CACS = 0 warranty period up to 15 years |
| Matos et al. [19] | 2021 | Multicenter Retrospective | 467 participants, 53% women, mean age 60 years | CACS is useful for risk reclassification, with no clear direct impact on therapies. |
| Nakao et al. [20] | 2018 | Multicenter Prospective, subgroup analysis by sex | 991 patients between 50 and 74 years old, 46% women | CACS predicts CVD with greater strength in men. |
| Fernández-Friera et al. [21] | 2015 | Prospective Cohort | 4184 asymptomatic adults (40–54 years old) | High prevalence of atherosclerotic disease in other vascular territories than coronary arteries |
| Dzayet al. [22] | 2021 | Prospective Cohort | 22,346 asymptomatic adults (30–50 years old) | Optimal age for first CACS depending on the patient |
| Budoff et al. [23] | 2018 | Prospective Cohort | 4184 asymptomatic adults (45–84 years old) study MESA | CACS > 100 high risk and CACS = 0 low risk |
| Elias-Smale et al. [24] | 2010 | Prospective Cohort | 2028 patients ≥ 55 years (mean age 69.6), without coronary artery disease | CACS improves risk classification in the elderly. |
| Venkataraman et al. [25] | 2020 | Prospective Observational Study | 1059 people between 40 and 70 years old, asymptomatic but with a family history of premature CVD | CACS improves risk stratification. |
| Gallo et al. [26] | 2021 | Prospective Cohort | 1624 asymptomatic adults with hypercholesterolemia | CACS improves reclassification of cardiovascular risk in this group |
| Christou et al. [27] | 2022 | Narrative review | Asymptomatic mature athletes (over 35 years old) | Greater atherosclerotic burden and proportionally greater risk, although the plaques tend to be more calcified and stable than in sedentary individuals |
| Azour et al. [28] | 2017 | Observational transversal | 222 adults undergoing routine chest computed tomography and ECG-gated for coronary calcium scoring | ungated chest CT predicts with high accuracy the ranges of the Agatston score, with a strong correlation (r = 0.811) and excellent interobserver agreement (k = 0.95); |
| Chiles et al. [29] | 2015 | Observational retrospective | 1575 older adults, high-risk smokers who underwent low-dose computed tomography for lung cancer screening | The presence and quantity of coronary calcium was strongly associated with coronary and all-cause mortality in a graduated manner. |
| Bastarrika et at. [30] | 2010 | Observational | 48 asymptomatic adult smokers (44 men, 4 women; mean age 59.7 years) included in a lung cancer early detection program. | Excellent concordance (CCC ≥ 0.81) and no significant differences in the estimation of the total coronary calcium score compared to ECG-gated cardiac tomography |
| Gopal et al. [31] | 2007 | Prospective cohort | 710 asymptomatic adults all with CACS equal to zero on initial electron beam computed tomography | 62% of individuals maintained a zero calcium score during follow-up, and only 2% developed significant progression (>50 Agatston units) during the follow-up period. |
| Wang et al. [32] | 2025 | Observational prospective cohort | 2044 asymptomatic community adults free of clinical coronary artery disease from the ARIC study | Low levels of total cholesterol (<160 mg/dL), systolic blood pressure (<125 mm Hg), high HDL cholesterol (>45 mg/dL), and never having smoked are significantly associated with a higher likelihood of having a coronary calcium score equal to zero. |
| Budoff et al. [33] | 2010 | Prospective cohort | 4609 asymptomatic adults | Coronary calcium score progression was significantly and independently associated with all-cause mortality. |
| López Melgar et al. [34] | 2020 | Prospective cohort | 3514 asymptomatic middle-aged adults (mean age 45.7 years; 63% men) from the PESA study | The progression of multi-territorial subclinical atherosclerosis was detected in 41.5% of participants in just 3 years, being more frequent in peripheral territories assessed by ultrasound than in CACS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Díaz, D.; Díez-Villanueva, P.; López-Melgar, B.; Flores, L.; De Toffol, G.; Ramos, A.; Montes, Á.; Cecconi, A.; Jiménez-Borreguero, J.; Alfonso, F. Role of Coronary Artery Calcium Score CT in Risk Stratification of Asymptomatic Individuals. J. Cardiovasc. Dev. Dis. 2025, 12, 442. https://doi.org/10.3390/jcdd12110442
Gómez-Díaz D, Díez-Villanueva P, López-Melgar B, Flores L, De Toffol G, Ramos A, Montes Á, Cecconi A, Jiménez-Borreguero J, Alfonso F. Role of Coronary Artery Calcium Score CT in Risk Stratification of Asymptomatic Individuals. Journal of Cardiovascular Development and Disease. 2025; 12(11):442. https://doi.org/10.3390/jcdd12110442
Chicago/Turabian StyleGómez-Díaz, Darío, Pablo Díez-Villanueva, Beatriz López-Melgar, Luis Flores, Gianluca De Toffol, Agustín Ramos, Álvaro Montes, Alberto Cecconi, Jesús Jiménez-Borreguero, and Fernando Alfonso. 2025. "Role of Coronary Artery Calcium Score CT in Risk Stratification of Asymptomatic Individuals" Journal of Cardiovascular Development and Disease 12, no. 11: 442. https://doi.org/10.3390/jcdd12110442
APA StyleGómez-Díaz, D., Díez-Villanueva, P., López-Melgar, B., Flores, L., De Toffol, G., Ramos, A., Montes, Á., Cecconi, A., Jiménez-Borreguero, J., & Alfonso, F. (2025). Role of Coronary Artery Calcium Score CT in Risk Stratification of Asymptomatic Individuals. Journal of Cardiovascular Development and Disease, 12(11), 442. https://doi.org/10.3390/jcdd12110442






