Heart Rate Variability in Acute Myocardial Infarction: Results of the HeaRt-V-AMI Single-Center Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. HRV Measurement
2.3. Study Outcomes
2.4. Statistical Analysis
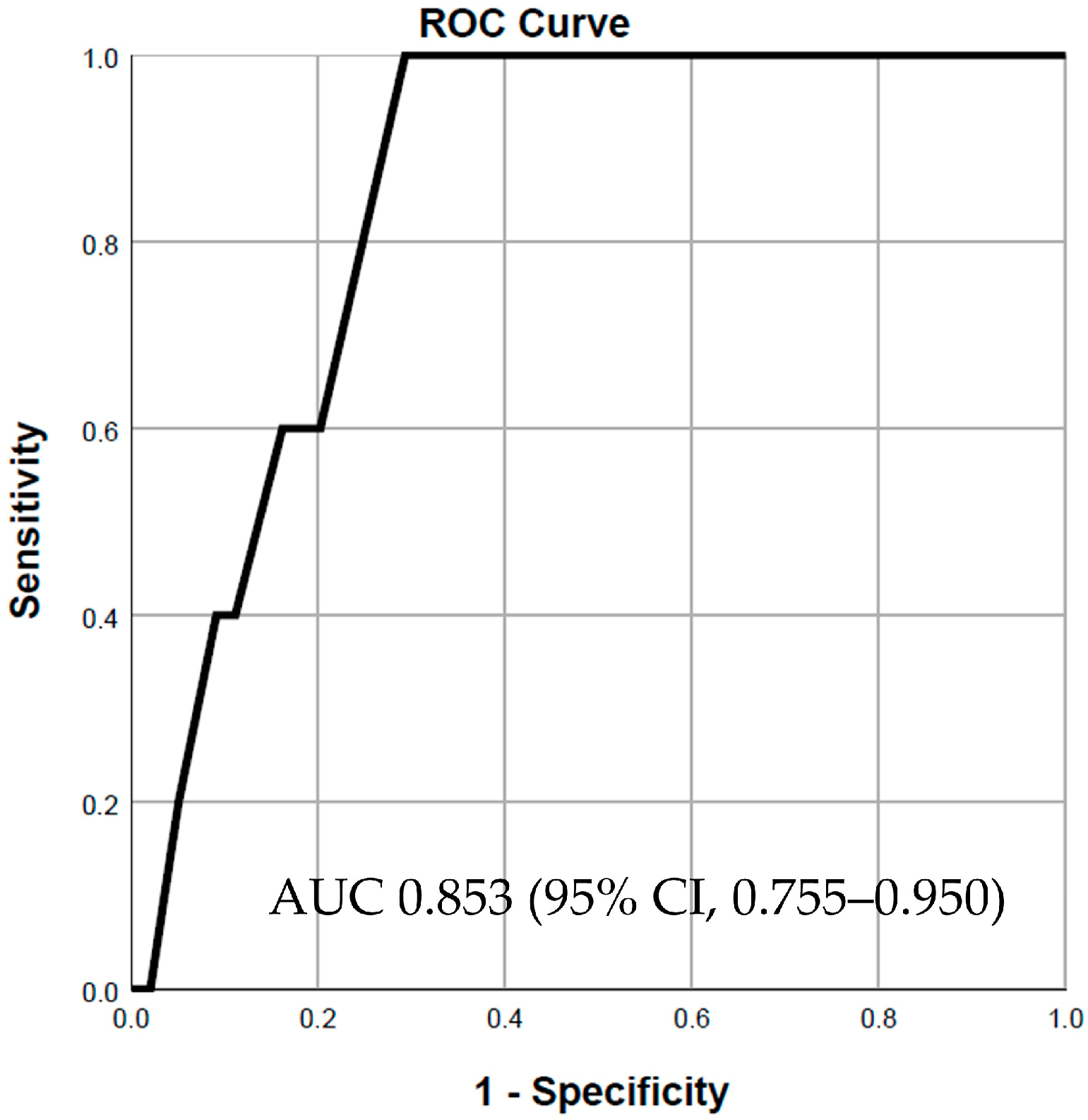
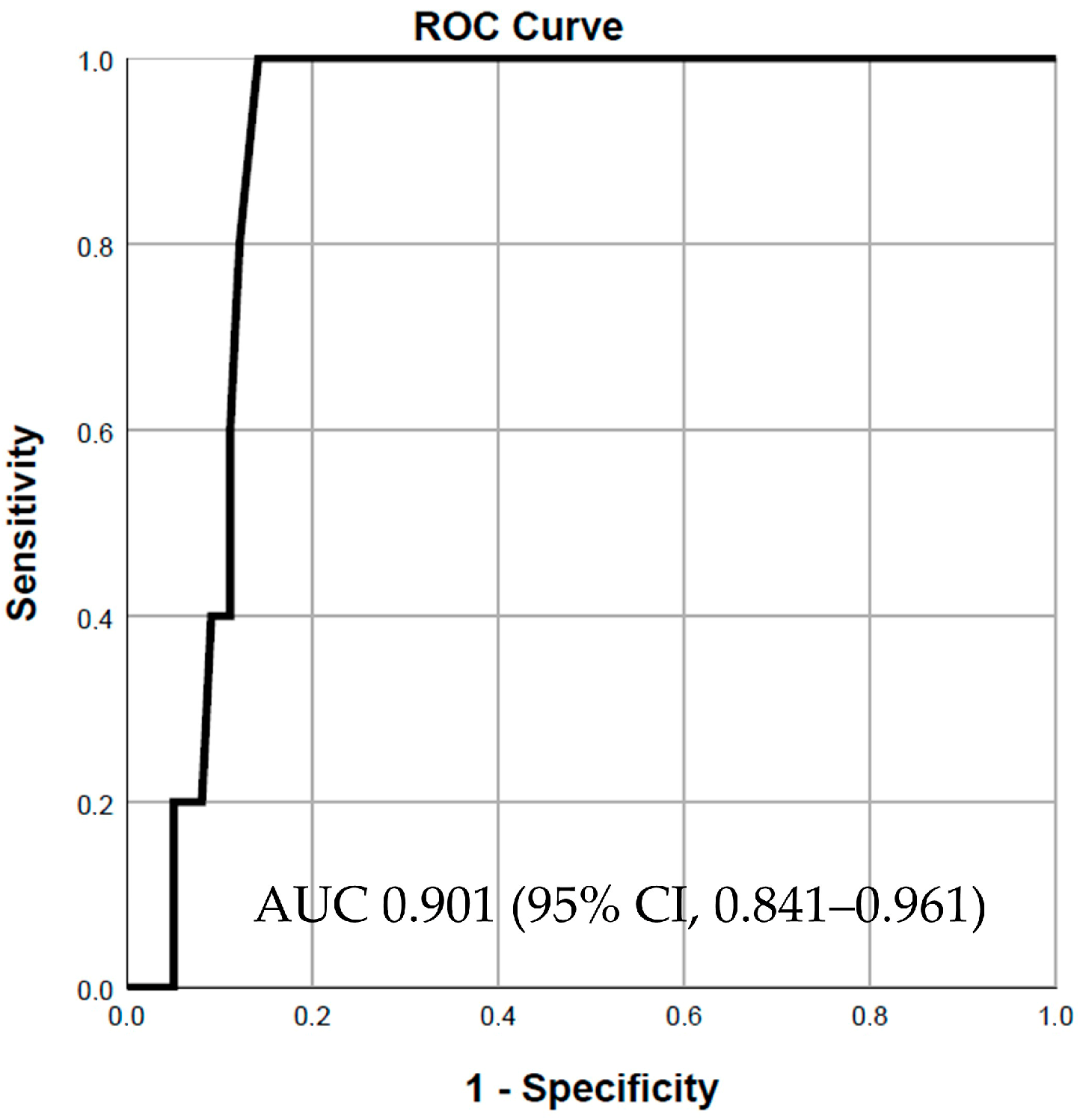
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth Universal Definition of Myocardial Infarction (2018). Circulation 2018, 138, e618–e651. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes: Developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef] [PubMed]
- Bošković, A.; Belada, N.; Knežević, B. Prognostic value of heart rate variability in post-infarction patients. Vojnosanit. Pregl. 2014, 71, 925–930. [Google Scholar] [CrossRef] [PubMed]
- Coviello, I.; Pinnacchio, G.; Laurito, M.; Stazi, A.; Battipaglia, I.; Barone, L.; Mollo, R.; Russo, G.; Villano, A.; Sestito, A.; et al. Prognostic role of heart rate variability in patients with ST-segment elevation acute myocardial infarction treated by primary angioplasty. Cardiology 2013, 124, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Ablonskytė-Dūdonienė, R.; Bakšytė, G.; Čeponienė, I.; Kriščiukaitis, A.; Drėgūnas, K.; Ereminienė, E. Impedance cardiography and heart rate variability for long-term cardiovascular outcome prediction after myocardial infarction. Medicina 2012, 48, 350–358. [Google Scholar] [CrossRef]
- Balanescu, S.; Corlan, A.D.; Dorobantu, M.; Gherasim, L. Prognostic value of heart rate variability after acute myocardial infarction. Med. Sci. Monit. 2004, 10, Cr307-15. [Google Scholar] [PubMed]
- Schuurmans, A.A.T.; de Looff, P.; Nijhof, K.S.; Rosada, C.; Scholte, R.H.J.; Popma, A.; Otten, R. Validity of the Empatica E4 Wristband to Measure Heart Rate Variability (HRV) Parameters: A Comparison to Electrocardiography (ECG). J. Med. Syst. 2020, 44, 190. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.-Y.; Ma, H.-P.; Lin, C.; Lo, M.-T.; Lin, L.-Y.; Chen, T.-Y.; Wu, C.-K.; Chiang, J.-Y.; Lee, J.-K.; Hung, C.-S.; et al. Heart rhythm complexity analysis in patients with inferior ST-elevation myocardial infarction. Sci. Rep. 2023, 13, 20861. [Google Scholar] [CrossRef] [PubMed]
- Kida, N.; Tsubakihara, Y.; Kida, H.; Ageta, S.; Arai, M.; Hamada, Y.; Matsuura, N. Usefulness of measurement of heart rate variability by holter ECG in hemodialysis patients. BMC Nephrol. 2017, 18, 8. [Google Scholar] [CrossRef] [PubMed]
- Chakko, S.; Fernandez, A.; Sequeira, R.; Kessler, K.M.; Myerburg, R.J. Heart rate variability during the first 24 hours of successfully reperfused acute myocardial infarction: Paradoxic decrease after reperfusion. Am. Heart J. 1996, 132, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Huikuri, H.V.; Tapanainen, J.M.; Lindgren, K.; Raatikainen, P.; Mäkikallio, T.H.; Juhani Airaksinen, K.E.; Myerburg, R.J. Prediction of sudden cardiac death after myocardial infarction in the beta-blocking era. J. Am. Coll. Cardiol. 2003, 42, 652–658. [Google Scholar] [CrossRef]
- Lin, S.; Yang, X.; Guo, X.; Ye, J.; Hu, X.; Dong, H.; Zhou, Y. Impact of Short-Term Heart Rate Variability in Patients with STEMI Treated by Delayed versus Immediate Stent in Primary Percutaneous Coronary Intervention: A Prospective Cohort Study. Comput. Math. Methods Med. 2022, 2022, 2533664. [Google Scholar] [CrossRef] [PubMed]
- Bergamaschi, L.; Landi, A.; Maurizi, N.; Pizzi, C.; Leo, L.A.; Arangalage, D.; Iglesias, J.F.; Eeckhout, E.; Schwitter, J.; Valgimigli, M.; et al. Acute Response of the Noninfarcted Myocardium and Surrounding Tissue Assessed by T2 Mapping After STEMI. JACC Cardiovasc. Imaging 2024, 17, 610–621. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Overall (n = 104) |
|---|---|
| Age, mean ± SD, years | 60.64 ± 13.36 |
| Women, n (%) | 31 (29.8) |
| BMI, mean ± SD, kg/m2 | 28.42 ± 5.69 |
| BSA, mean ± SD, m2 | 1.91 ± 0.25 |
| Smoking, n (%) | 61 (58.65) |
| Alcohol consumption, n (%) | 17 (16.35) |
| Sedentarism, n (%) | 96 (92.31) |
| Time to PCI, median (IQR), hours | 8.0 (6.0–10.25) |
| History of IHD, n (%) | 16 (15.4) |
| Arterial hypertension, n (%) | 58 (55.8) |
| Previous stroke, n (%) | 6 (5.8) |
| Diabetes mellitus | 22 (21.15) |
| PAD, n (%) | 3 (2.9) |
| COPD, n (%) | 3 (2.9) |
| Chronic hepatitis, n (%) | 1 (1.0) |
| Prior beta-blocker, n (%) | 24 (23.1) |
| Killip class | |
| Class I, n (%) | 69 (66.3) |
| Class II, n (%) | 29 (27.9) |
| Class III, n (%) | 6 (5.8) |
| STEMI territory | |
| Anterior (V3, V4), n (%) | 3 (2.9) |
| Anteroseptal (V1–V4), n (%) | 23 (22.1) |
| Anterolateral (V3–V6), n (%) | 1 (1.0) |
| Extensive anterior (V1–V6), n (%) | 25 (24.0) |
| Inferior (II, III, aVF) | 52 (50.0) |
| SBP, mean ± SD, mmHg | 145.85 ± 21.85 |
| eGFR, mean ± SD, mL/min/1.73 m2 | 82.96 ± 23.56 |
| CK-MB, admission, median (IQR), U/L | 48.0 (23.0–89.2) |
| CK-MB, peak, median (IQR), U/L | 188 (87.0–288.5) |
| AST, median (IQR), U/L | 56 (36.0–102.5) |
| ALT, median (IQR), U/L | 34.0 (25.0–51.7) |
| CRP, median (IQR), mg/dL | 29.9 (12.5–65.7) |
| Fibrinogen, median (IQR), mg/dL | 431.0 (371.7–517.0) |
| LDL, mean ± SD, mg/dL | 136.1 ± 53.5 |
| Triglycerides, mean ± SD, mg/dL | 165.8 ± 108.9 |
| Blood glucose, mean ± SD, mg/dL | 162.8 ± 60.8 |
| LVEF, admission, median (IQR), % | 40.0 (34.7–45.0) |
| LVEF, discharge, median (IQR), % | 40.0 (35.0–47.0) |
| E/A | |
| <1, n (%) | 63 (60.6) |
| >2, n (%) | 5 (4.8) |
| PCI Characteristics | Overall (n = 104) |
|---|---|
| Coronary lesions | |
| Single artery, n (%) | 48 (46.2) |
| Two arteries, n (%) | 33 (31.7) |
| Three arteries, n (%) | 23 (22.1) |
| Culprit artery | |
| LAD, n (%) | 50 (48.1) |
| LCX, n (%) | 14 (13.5) |
| RCA, n (%) | 37 (35.6) |
| LM, n (%) | 2 (1.9) |
| DG, n (%) | 1 (1.0) |
| LM disease, n (%) | 4 (3.8) |
| Initial TIMI flow | |
| TIMI 0, n (%) | 57 (54.8) |
| TIMI 1, n (%) | 10 (9.6) |
| TIMI 2, n (%) | 18 (17.3) |
| TIMI 3, n (%) | 19 (18.3) |
| Final TIMI flow | |
| TIMI 0, n (%) | 0 (0) |
| TIMI 1, n (%) | 1 (1.0) |
| TIMI 2, n (%) | 10 (9.6) |
| TIMI 3, n (%) | 92 (88.5) |
| Contrast media, mean ± SD, mL | 204.8 ± 51.4 |
| HRV Parameters | Overall | First 5 min | Last 5 min |
|---|---|---|---|
| SDNN, median (IQR), ms | 29.2 (20.87–40.85) | 29.5 (20.7–43.7) | 28.15 (19.1–39.0) |
| RMSSD, median (IQR), ms | 32.5 (25.7–46.4) | 36.7 (25.2–52.0) | 29.8 (22.3–45.5) |
| NN50, median (IQR), beats | 89.0 (36.0–159.5) | 28.5 (11.0–51.7) | 18.5 (7.7–45.7) |
| pNN50, median (IQR), % | 7.5 (3.1–17.7) | 10.3 (3.0–20.7) | 4.5 (2.0–17.9) |
| RR triangular index, median (IQR), ms | 6.3 (5.3–8.8) | 6.2 (4.8–8.7) | 6.1 (4.5–8.0) |
| VLF, median (IQR), ms2 | 75.8 (35.7–142.4) | 66.0 (19.1–130.5) | 40.2 (22.5–154.6) |
| VLF, median (IQR), log | 4.3 (3.5–4.9) | 4.1 (2.9–4.8) | 3.6 (3.0–5.0) |
| LF, median (IQR), ms2 | 372.9 (175.3–654.5) | 365.2 (108.2–712.5) | 359.2 (101.0–751.5) |
| LF, median (IQR), log | 5.9 (5.1–6.4) | 5.8 (4.6–6.5) | 5.8 (4.5–6.6) |
| LF, median (IQR), n.u. | 66.9 (59.8–74.8) | 63.9 (54.9–73.5) | 65.3 (56.0–75.4) |
| HF, median (IQR), ms2 | 168.5 (96.1–310.0) | 188.0 (71.4–332.5) | 155.5 (59.4–290.3) |
| HF, median (IQR), log | 5.1 (4.5–5.7) | 5.2 (4.2–5.8) | 5.0 (4.0–5.6) |
| HF, median (IQR), n.u. | 32.7 (25.0–39.8) | 35.1 (25.8–44.5) | 34.3 (24.4–43.2) |
| LF/HF median (IQR) | 2.0 (1.4–2.9) | 1.7 (1.2–2.8) | 1.9 (1.2–3.0) |
| SD1, median (IQR), ms | 23.0 (18.2–32.9) | 26.0 (17.8–37.0) | 21.1 (15.8–32.2) |
| SD2, median (IQR), ms | 33.3 (22.2–44.5) | 32.7 (22.2–47.8) | 32.2 (21.4–46.3) |
| SD2/SD1, median (IQR) | 1.3 (1.0–1.5) | 1.2 (0.9–1.5) | 1.3 (1.0–1.6) |
| ApEn, median (IQR) | 1.3 (1.2–1.4) | 1.0 (0.9–1.1) | 1.0 (0.9–1.1) |
| HRV Parameters | First vs. Last 5 min of PCI | p-Value |
|---|---|---|
| SDNN, ms | Z −2.155 | p = 0.031 |
| RMSSD, median (IQR), ms | Z −3.436 | p < 0.001 |
| NN50, median (IQR), beats | Z −1.807 | p = 0.071 |
| pNN50, median (IQR), % | Z −3.043 | p = 0.002 |
| RR triangular index, median (IQR), ms | Z −1.786 | p = 0.075 |
| VLF, median (IQR), ms2 | Z −0.417 | p = 0.677 |
| VLF, median (IQR), log | Z −0.581 | p = 0.580 |
| LF, median (IQR), ms2 | Z −0.987 | p = 0.324 |
| LF, median (IQR), log | Z −0.737 | p = 0.447 |
| LF, median (IQR), n.u. | Z −0.858 | p = 0.395 |
| HF, median (IQR), ms2 | Z −2.289 | p = 0.022 |
| HF, median (IQR), log | Z −2.116 | p = 0.033 |
| HF, median (IQR), n.u. | Z −0.914 | p = 0.358 |
| LF/HF median (IQR) | Z −1.199 | p = 0.235 |
| SD1, median (IQR), ms | Z −3.446 | p < 0.001 |
| SD2, median (IQR), ms | Z −1.850 | p = 0.064 |
| SD2/SD1, median (IQR) | Z −3.748 | p < 0.001 |
| ApEn, median (IQR) | Z −1.931 | p = 0.055 |
| HRV Parameters | Deceased | Survivors | p-Value |
|---|---|---|---|
| HRV during entire PCI duration | |||
| SDNN, median (IQR), ms | 23.9 (20.2–35.6) | 29.2 (21.2–41.1) | p = 0.806 |
| RMSSD, median (IQR), ms | 38.9 (29.8–49.5) | 32.3 (25.1–46.1) | p = 0.361 |
| NN50, median (IQR), beats | 102.0 (51.0–106.0) | 86.5 (32.2–167.7) | p = 0.981 |
| pNN50, median (IQR), % | 14.1 (7.3–22.5) | 7.2 (2.9–17.4) | p = 0.205 |
| RR triangular index, median (IQR), ms | 5.7 (4.9–6.3) | 6.3 (5.3–8.8) | p = 0.447 |
| VLF, median (IQR), ms2 | 33.3 (29.2–76.2) | 75.8 (37.7–142.6) | p = 0.155 |
| VLF, median (IQR), log | 3.5 (3.3–4.3) | 4.3 (3.6–4.9) | p = 0.157 |
| LF, median (IQR), ms2 | 178.5 (113.5–194.5) | 391.0 (178.2–681.7) | p = 0.064 |
| LF, median (IQR), log | 5.1 (4.7–5.2) | 5.9 (5.1–6.5) | p = 0.052 |
| LF, median (IQR), n.u. | 63.8 (58.0–70.4) | 66.9 (59.9–74.8) | p = 0.369 |
| HF, median (IQR), ms2 | 100.4 (81.6–106.4) | 178.7 (96.5–323.5) | p = 0.108 |
| HF, median (IQR), log | 4.6 (4.4–4.6) | 5.1 (4.5–5.7) | p = 0.106 |
| HF, median (IQR), n.u. | 35.9 (29.4–41.7) | 32.7 (25.0–39.7) | p = 0.373 |
| LF/HF median (IQR) | 1.7 (1.3–2.3) | 2.0 (1.5–2.9) | p = 0.352 |
| SD1, median (IQR), ms | 27.5 (21.1–35.1) | 22.8 (17.7–32.6) | p = 0.349 |
| SD2, median (IQR), ms | 19.7 (19.2–36.3) | 33.3 (22.7–45.2) | p = 0.240 |
| SD2/SD1, median (IQR) | 0.9 (0.8–1.0) | 1.3 (1.0–1.6) | p = 0.008 |
| ApEn, median (IQR) | 1.2 (1.0–1.2) | 1.3 (1.2–1.4) | p = 0.019 |
| HRV in the first 5 min of PCI | |||
| SDNN, median (IQR), ms | 32.3 (20.5–44.8) | 29.3 (21.0–43.5) | p = 0.841 |
| RMSSD, median (IQR), ms | 51.9 (32.0–69.0) | 36.3 (24.3–51.5) | p = 0.240 |
| NN50, median (IQR), beats | 23.0 (17.0–33.0) | 28.5 (11.0–50.7) | p = 0.847 |
| pNN50, median (IQR), % | 26.1 (7.4–26.6) | 9.1 (2.8–20.5) | p = 0.174 |
| RR triangular index, median (IQR), ms | 5.1 (4.8–6.4) | 6.2 (4.8–9.1) | p = 0.256 |
| VLF, median (IQR), ms2 | 24.0 (20.5–88.7) | 66.0 (18.9–136.7) | p = 0.357 |
| VLF, median (IQR), log | 3.1 (3.0–4.4) | 4.1 (2.9–4.8) | p = 0.365 |
| LF, median (IQR), ms2 | 139.7 (22.7–252.3) | 387.5 (110.9–744.7) | p = 0.056 |
| LF, median (IQR), log | 4.9 (3.1–5.5) | 5.8 (4.6–6.5) | p = 0.067 |
| LF, median (IQR), n.u. | 58.1 (53.1–59.8) | 65.3 (55.0–73.8) | p = 0.252 |
| HF, median (IQR), ms2 | 93.3 (37.4–125.8) | 194.7 (73.3–341.1) | p = 0.099 |
| HF, median (IQR), log | 4.5 (3.6–4.8) | 5.2 (4.2–5.8) | p = 0.106 |
| HF, median (IQR), n.u. | 41.7 (39.9–46.6) | 34.0 (25.8–44.3) | p = 0.216 |
| LF/HF median (IQR) | 1.3 (1.1–1.4) | 1.9 (1.2–2.8) | p = 0.199 |
| SD1, median (IQR), ms | 36.7 (22.7–49.1) | 25.7 (17.2–36.6) | p = 0.234 |
| SD2, median (IQR), ms | 27.2 (18.2–39.5) | 32.7 (22.4–48.0) | p = 0.499 |
| SD2/SD1, median (IQR) | 0.8 (0.7–0.8) | 1.2 (1.0–1.5) | p = 0.006 |
| ApEn, median (IQR) | 1.0 (0.6–1.0) | 1.0 (0.9–1.1) | p = 0.188 |
| HRV in the last 5 min of PCI | |||
| SDNN, median (IQR), ms | 24.3 (19.3–44.7) | 28.4 (19.1–38.7) | p = 0.944 |
| RMSSD, median (IQR), ms | 34.2 (28.2–45.2) | 29.8 (21.9–45.7) | p = 0.429 |
| NN50, median (IQR), beats | 39.0 (18.0–40.0) | 18.0 (7.0–47.2) | p = 0.333 |
| pNN50, median (IQR), % | 10.2 (4.0–21.9) | 4.5 (1.8–17.4) | p = 0.246 |
| RR triangular index, median (IQR), ms | 4.7 (4.3–7.1) | 6.1 (4.5–8.0) | p = 0.580 |
| VLF, median (IQR), ms2 | 35.5 (18.7–77.9) | 40.2 (23.2–155.0) | p = 0.489 |
| VLF, median (IQR), log | 3.5 (2.9–4.3) | 3.69 (3.1–5.0) | p = 0.456 |
| LF, median (IQR), ms2 | 400.4 (81.8–424.4) | 337.1 (106.5–794.2) | p = 0.377 |
| LF, median (IQR), log | 5.9 (4.4–6.0) | 5.7 (4.6–6.6) | p = 0.352 |
| LF, median (IQR), n.u. | 72.9 (51.0–74.6) | 65.1 (56.2–75.0) | p = 0.932 |
| HF, median (IQR), ms2 | 129.6 (78.3–143.6) | 168.0 (59.3–328.7) | p = 0.279 |
| HF, median (IQR), log | 4.8 (4.3–4.9) | 5.1 (4.0–5.6) | p = 0.262 |
| HF, median (IQR), n.u. | 26.8 (25.2–48.8) | 34.4 (24.8–43.0) | p = 0.944 |
| LF/HF median (IQR) | 2.7 (1.0–2.9) | 1.8 (1.3–2.9) | p = 0.938 |
| SD1, median (IQR), ms | 24.2 (19.9–32.0) | 21.1 (15.5–32.4) | p = 0.429 |
| SD2, median (IQR), ms | 24.4 (18.8–33.6) | 32.3 (21.4–46.4) | p = 0.329 |
| SD2/SD1, median (IQR) | 1.0 (0.9–1.0) | 1.3 (1.0–1.6) | p = 0.018 |
| ApEn, median (IQR) | 1.0 (0.8–1.0) | 1.0 (1.0–1.1) | p = 0.165 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brinza, C.; Floria, M.; Scripcariu, D.-V.; Covic, A.M.; Covic, A.; Popa, I.V.; Statescu, C.; Burlacu, A. Heart Rate Variability in Acute Myocardial Infarction: Results of the HeaRt-V-AMI Single-Center Cohort Study. J. Cardiovasc. Dev. Dis. 2024, 11, 254. https://doi.org/10.3390/jcdd11080254
Brinza C, Floria M, Scripcariu D-V, Covic AM, Covic A, Popa IV, Statescu C, Burlacu A. Heart Rate Variability in Acute Myocardial Infarction: Results of the HeaRt-V-AMI Single-Center Cohort Study. Journal of Cardiovascular Development and Disease. 2024; 11(8):254. https://doi.org/10.3390/jcdd11080254
Chicago/Turabian StyleBrinza, Crischentian, Mariana Floria, Dragos-Viorel Scripcariu, Alexandra Maria Covic, Adrian Covic, Iolanda Valentina Popa, Cristian Statescu, and Alexandru Burlacu. 2024. "Heart Rate Variability in Acute Myocardial Infarction: Results of the HeaRt-V-AMI Single-Center Cohort Study" Journal of Cardiovascular Development and Disease 11, no. 8: 254. https://doi.org/10.3390/jcdd11080254
APA StyleBrinza, C., Floria, M., Scripcariu, D.-V., Covic, A. M., Covic, A., Popa, I. V., Statescu, C., & Burlacu, A. (2024). Heart Rate Variability in Acute Myocardial Infarction: Results of the HeaRt-V-AMI Single-Center Cohort Study. Journal of Cardiovascular Development and Disease, 11(8), 254. https://doi.org/10.3390/jcdd11080254








