Ten-Year Experience with Endomyocardial Biopsy after Orthotopic Heart Transplantation: Comparison between Trans-Jugular and Trans-Femoral Approach
Abstract
1. Introduction
2. Materials and Methods
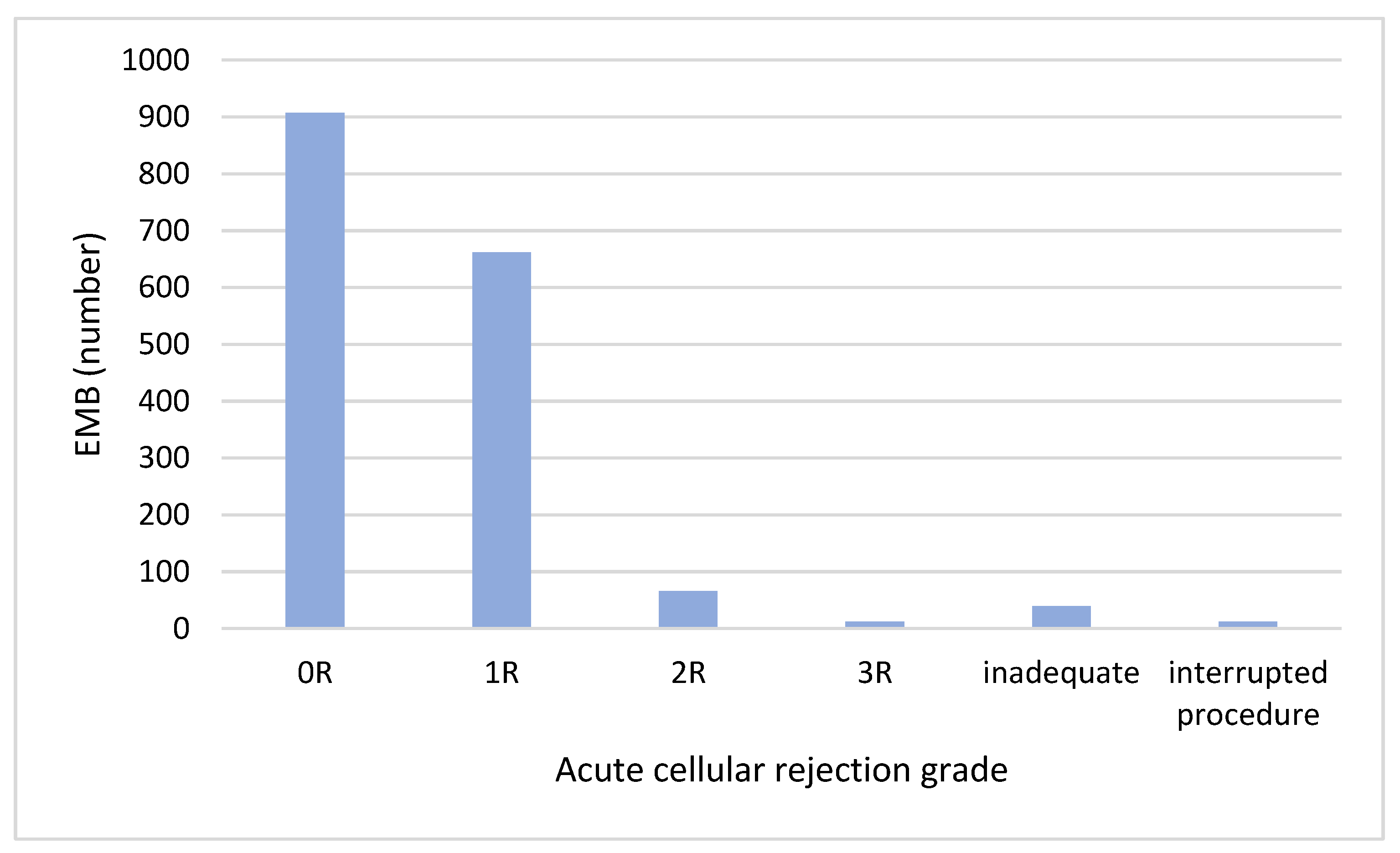
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Galeone, A.; Kirsch, M.; Barreda, E.; Fernandez, F.; Vaissier, E.; Pavie, A.; Leprince, P.; Varnous, S. Clinical outcome and quality of life of patients surviving 20 years or longer after heart transplantation. Transpl. Int. 2014, 27, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Lund, L.H.; Edwards, L.B.; Kucheryavaya, A.Y.; Benden, C.; Dipchand, A.I.; Goldfarb, S.; Levvey, B.J.; Meiser, B.; Rossano, J.W.; Yusen, R.D.; et al. The Registry of the International Society for Heart and Lung Transplantation: Thirty-second Official Adult Heart Transplantation Report–2015; Focus Theme: Early Graft Failure. J. Heart Lung Transplant. 2015, 34, 1244–1254. [Google Scholar] [CrossRef] [PubMed]
- Lund, L.H.; Edwards, L.B.; Kucheryavaya, A.Y.; Benden, C.; Christie, J.D.; Dipchand, A.I.; Dobbels, F.; Goldfarb, S.B.; Levvey, B.J.; Meiser, B.; et al. The registry of the International Society for Heart and Lung Transplantation: Thirty-first official adult heart transplant report—2014; focus theme: Retransplantation. J. Heart Lung Transplant. 2014, 33, 996–1008. [Google Scholar] [CrossRef] [PubMed]
- Kent, G.; Sutton, D.C.; Sutton, G.C. Needle biopsy of the human ventricular myocardium. Q. Bull. Northwestern Univ. Med. Sch. 1956, 30, 213–214. [Google Scholar]
- Sakakibara, S.; Konno, S. Endomyocardial biopsy. JPN Heart J. 1962, 3, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Caves, P.K.; Stinson, E.B.; Graham, A.F.; Billingham, M.E.; Grehl, T.M.; Shumway, N.E. Percutaneous Transvenous Endomyocardial Biopsy. JAMA 1973, 225, 288–291. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.; Marshall, H.; Allison, S. The femoral venous approach to endomyocardial biopsy: Comparison with internal jugular and transarterial approaches. Am. J. Cardiol. 1984, 53, 833–837. [Google Scholar] [CrossRef] [PubMed]
- Stewart, S.; Winters, G.L.; Fishbein, M.C.; Tazelaar, H.D.; Kobashigawa, J.; Abrams, J.; Andersen, C.B.; Angelini, A.; Berry, G.J.; Burke, M.M.; et al. Revision of the 1990 working formulation for the standardization of nomenclature in the diagnosis of heart rejection. J. Heart Lung Transplant. 2005, 24, 1710–1720. [Google Scholar] [CrossRef]
- Crespo-Leiro, M.G.; Zuckermann, A.; Bara, C.; Mohacsi, P.; Schulz, U.; Boyle, A.; Ross, H.J.; Parameshwar, J.; Zakliczyński, M.; Fiocchi, R.; et al. Concordance among pathologists in the second Cardiac Allograft Rejection Gene Expression Observational Study (CARGO II). Transplantation 2012, 94, 1172–1177. [Google Scholar] [CrossRef]
- Seferovic, P.M.; Tsutsui, H.; McNamara, D.M.; Ristić, A.D.; Basso, C.; Bozkurt, B.; Cooper, L.T., Jr.; Filippatos, G.; Ide, T.; Inomata, T.; et al. Heart Failure Association of the ESC, Heart Failure Society of America and Japanese Heart Failure Society position statement on endomyocardial biopsy. Eur. J. Heart Fail. 2021, 23, 854–871. [Google Scholar] [CrossRef]
- Costanzo, M.R.; Dipchand, A.; Starling, R.; Anderson, A.; Chan, M.; Desai, S.; Fedson, S.; Fisher, P.; Gonzales-Stawinski, G.; Martinelli, L.; et al. The International Society of Heart and Lung Transplantation guidelines for the care of heart transplant recipients. J Heart Lung Transplant. 2010, 29, 914–956. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, A.; Kindermann, I.; Kindermann, M.; Mahfoud, F.; Ukena, C.; Athanasiadis, A.; Hill, S.; Mahrholdt, H.; Voehringer, M.; Schieber, M.; et al. Comparative evaluation of left and right ventricular endomyocardial biopsy: Differences in complication rate and diagnostic performance. Circulation 2010, 122, 900–909. [Google Scholar] [CrossRef] [PubMed]
- Holzmann, M.; Nicko, A.; Kühl, U.; Noutsias, M.; Poller, W.; Hoffmann, W.; Morguet, A.; Witzenbichler, B.; Tschöpe, C.; Schultheiss, H.P.; et al. Complication rate of right ventricular endomyocardial biopsy via the femoral approach: A retrospective and prospective study analyzing 3048 diagnostic procedures over an 11-year period. Circulation 2008, 118, 1722–1728. [Google Scholar] [CrossRef]
- Cooper, L.T.; Baughman, K.L.; Feldman, A.M.; Frustaci, A.; Jessup, M.; Kuhl, U.; Levine, G.N.; Narula, J.; Starling, R.C.; Towbin, J.; et al. The role of endomyocardial biopsy in the management of cardiovascular disease: A scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Circulation 2007, 116, 2216–2233. [Google Scholar] [CrossRef]
- Shah, Z.; Vuddanda, V.; Rali, A.S.; Pamulapati, H.; Masoomi, R.; Gupta, K. National trends and procedural complications from endomyocardial biopsy: Results from the National Inpatient Sample, 2007-2014. Cardiology 2018, 141, 125–131. [Google Scholar] [CrossRef]
- Bermpeis, K.; Esposito, G.; Gallinoro, E.; Paolisso, P.; Bertolone, D.T.; Fabbricatore, D.; Mileva, N.; Munhoz, D.; Buckley, J.; Wyffels, E.; et al. Safety of Right and Left Ventricular Endomyocardial Biopsy in Heart Transplantation and Cardiomyopathy Patients. JACC Heart Fail. 2022, 10, 963–973. [Google Scholar] [CrossRef]
- Vilalta, A. Cost and Use Trends of Endomyocardial Biopsy in Heart Transplant Patients: A 4-Year Claims Data Analysis. Transplant. Proc. 2023, 55, 2186–2190. [Google Scholar] [CrossRef] [PubMed]
- Fiorelli, A.I.; Coelho, G.H.; Aiello, V.D.; Benvenuti, L.A.; Palazzo, J.F.; Santos Júnior, V.P.; Canizares, B.; Dias, R.R.; Stolf, N.A. Tricuspid valve injury after heart transplantation due to endomyocardial biopsy: An analysis of 3550 biopsies. Transplant. Proc. 2012, 44, 2479–2482. [Google Scholar] [CrossRef]
- Mielniczuk, L.; Haddad, H.; Davies, R.A.; Veinot, J.P. Tricuspid valve chordal tissue in endomyocardial biopsy specimens of patients with significant tricuspid regurgitation. J. Heart Lung Transplant. 2005, 24, 1586–1590. [Google Scholar] [CrossRef]
- Wong, R.C.; Abrahams, Z.; Hanna, M.; Pangrace, J.; Gonzalez-Stawinski, G.; Starling, R.; Taylor, D. Tricuspid regurgitation after cardiac transplantation: An old problem revisited. J. Heart Lung Transplant. 2008, 27, 247–252. [Google Scholar] [CrossRef]
- Chan, M.C.; Giannetti, N.; Kato, T.; Kornbluth, M.; Oyer, P.; Valantine, H.A.; Robbins, R.C.; Hunt, S.A. Severe tricuspid regurgitation after heart transplantation. J. Heart Lung Transplant. 2001, 20, 709–717. [Google Scholar] [CrossRef]
- Filsoufi, F.; Salzberg, S.P.; Anderson, C.A.; Couper, G.S.; Cohn, L.H.; Adams, D.H. Optimal surgical management of severe tricuspid regurgitation in cardiac transplant patients. J. Heart Lung Transplant. 2006, 25, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, V.; Cantarovich, M.; Cecere, R.; Giannetti, N. Tricuspid regurgitation after cardiac transplantation: How many biopsies are too many? J. Heart Lung Transplant. 2005, 24, S227–S231. [Google Scholar] [CrossRef]
- Al-Hijji, M.; El Sabbagh, A.; El Hajj, S.; AlKhouli, M.; El Sabawi, B.; Cabalka, A.; Miranda, W.R.; Holmes, D.R.; Rihal, C.S. Coronary Artery Fistulas: Indications, Techniques, Outcomes, and Complications of Transcatheter Fistula Closure. JACC Cardiovasc. Interv. 2021, 14, 1393–1406. [Google Scholar] [CrossRef]
- Saraiva, F.; Matos, V.; Goncalves, L.; Antunes, M.; Providencia, L.A. Complications of endomyocardial biopsy in heart transplant recipients: A retrospective study of 2117 consecutive procedures. Transplant. Proc. 2011, 43, 1908–1912. [Google Scholar] [CrossRef] [PubMed]
- Somers, J.M.; Verney, G.I. Coronary cameral fistulae following heart transplantation. Clin. Radiol. 1991, 44, 419–421. [Google Scholar] [CrossRef] [PubMed]
- Henzlova, M.J.; Nath, H.; Bucy, R.P.; Bourge, R.C.; Kirklin, J.K.; Rogers, W.J. Coronary artery to right ventricle fistula in heart transplant recipients: A complication of endomyocardial biopsy. J. Am. Coll. Cardiol. 1989, 14, 258–261. [Google Scholar] [CrossRef]
- Sandhu, J.S.; Utretsky, B.F.; Zerbe, T.R.; Goldsmith, A.S.; Reddy, P.S.; Kormos, R.L.; Griffith, B.P.; Hardesty, R.L. Coronary artery fistula in the heart transplant patient: A potential complication of endomyocardial biopsy. Circulation 1989, 79, 350–356. [Google Scholar] [CrossRef]
- Isogai, T.; Yasunaga, H.; Matsui, H.; Ueda, T.; Tanaka, H.; Horiguchi, H.; Fushimi, K. Hospital volume and cardiac complications of endomyocardial biopsy: A retrospective cohort study of 9508 adult patients using a nationwide inpatient database in Japan. Clin. Cardiol. 2015, 38, 164–170. [Google Scholar] [CrossRef]
- ACS Committee on Perioperative Care. Revised statement on recommendations for use of real-time ultrasound guidance for placement of central venous catheters. Bull. Am. Coll. Surg. 2011, 96, 36–37. [Google Scholar]
- Saugel, B.; Scheeren, T.W.L.; Teboul, J.L. Ultrasound-guided central venous catheter placement: A structured review and recommendations for clinical practice. Crit. Care 2017, 21, 225. [Google Scholar] [CrossRef] [PubMed]
- Cusi, V.; Vaida, F.; Wettersten, N.; Rodgers, N.; Tada, Y.; Gerding, B.; Urey, M.A.; Greenberg, B.; Adler, E.D.; Kim, P.J. Incidence of Acute Rejection Compared with Endomyocardial Biopsy Complications for Heart Transplant Patients in the Contemporary Era. Transplantation, 2023; Online ahead of print. [Google Scholar] [CrossRef]
- Pergola, V.; Mattesi, G.; Cozza, E.; Pradegan, N.; Tessari, C.; Dellino, C.M.; Savo, M.T.; Amato, F.; Cecere, A.; Perazzolo Marra, M.; et al. New Non-Invasive Imaging Technologies in Cardiac Transplant Follow-Up: Acquired Evidence and Future Options. Diagnostics 2023, 13, 2818. [Google Scholar] [CrossRef] [PubMed]
- Vermes, E.; Pantaléon, C.; Auvet, A.; Cazeneuve, N.; Machet, M.C.; Delhommais, A.; Bourguignon, T.; Aupart, M.; Brunereau, L. Cardiovascular magnetic resonance in heart transplant patients: Diagnostic value of quantitative tissue markers: T2 mapping and extracellular volume fraction, for acute rejection diagnosis. J. Cardiovasc. Magn. Reson. 2018, 20, 59. [Google Scholar] [CrossRef] [PubMed]
- Anthony, C.; Imran, M.; Pouliopoulos, J.; Emmanuel, S.; Iliff, J.; Liu, Z.; Moffat, K.; Qiu, M.R.; McLean, C.A.; Stehning, C.; et al. Cardiovascular Magnetic Resonance for Rejection Surveillance After Cardiac Transplantation. Circulation 2022, 145, 1811–1824. [Google Scholar] [CrossRef]
- Brunetti, G.; Barile, B.; Nicchia, G.P.; Onorati, F.; Luciani, G.B.; Galeone, A. The ST2/IL-33 Pathway in Adult and Paediatric Heart Disease and Transplantation. Biomedicines 2023, 11, 1676. [Google Scholar] [CrossRef] [PubMed]
- Galeone, A.; Salem, J.E.; Lebreton, G.; Coutance, G.; Nguyen, L.; Hulot, J.S.; Atassi, F.; Bega, M.; Leprince, P.; Varnous, S. Suppression of tumorigenicity-2 (ST2) is a promising biomarker in heart transplantation. Clin. Transplant. 2022, 36, e14616. [Google Scholar] [CrossRef] [PubMed]
- Pascual-Figal, D.A.; Garrido, I.P.; Blanco, R.; Minguela, A.; Lax, A.; Ordoñez-Llanos, J.; Bayes-Genis, A.; Valdés, M.; Moore, S.A.; Januzzi, J.L. Soluble ST2 is a marker for acute cardiac allograft rejection. Ann. Thorac. Surg. 2011, 92, 2118–2124. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L.; Horne, B.D.; Moore, S.A.; Galenko, O.; Snow, G.L.; Brunisholz, K.D.; Muhlestein, J.B.; Alharethi, R.; Carlquist, J.F.; Budge, D.; et al. Interleukin receptor family member ST2 concentrations in patients following heart transplantation. Biomarkers 2013, 18, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Coutance, G.; Desiré, E.; Duong Van Huyen, J.-P. A Review of Biomarkers of Cardiac Allograft Rejection: Toward an Integrated Diagnosis of Rejection. Biomolecules 2022, 12, 1135. [Google Scholar] [CrossRef]
- Fitzsimons, S.; Evans, J.; Parameshwar, J.; Pettit, S.J. Utility of Troponin Assays for Exclusion of Acute Cellular Rejection after Heart Transplantation: A Systematic Review. J. Heart Lung Transplant. 2018, 37, 631–638. [Google Scholar] [CrossRef]
- Agbor-Enoh, S.; Shah, P.; Tunc, I.; Hsu, S.; Russell, S.; Feller, E.; Shah, K.; Rodrigo, M.E.; Najjar, S.S.; Kong, H.; et al. Cell-Free DNA to Detect Heart Allograft Acute Rejection. Circulation 2021, 143, 1184–1197. [Google Scholar] [CrossRef] [PubMed]
- Kobashigawa, J.; Hall, S.; Shah, P.; Fine, B.; Halloran, P.; Jackson, A.M.; Khush, K.K.; Margulies, K.B.; Sani, M.M.; Patel, J.K.; et al. The evolving use of biomarkers in heart transplantation: Consensus of an expert panel. Am. J. Transplant. 2023, 23, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Velleca, A.; Shullo, M.A.; Dhital, K.; Azeka, E.; Colvin, M.; DePasquale, E.; Farrero, M.; García-Guereta, L.; Jamero, G.; Khush, K.; et al. The International Society for Heart and Lung Transplantation (ISHLT) guidelines for the care of heart transplant recipients. J. Heart Lung Transplant. 2023, 42, e1–e141. [Google Scholar] [CrossRef] [PubMed]
- Deng, M.C.; Eisen, H.J.; Mehra, M.R.; Billingham, M.; Marboe, C.C.; Berry, G.; Kobashigawa, J.; Johnson, F.L.; Starling, R.C.; Murali, S.; et al. Noninvasive Discrimination of Rejection in Cardiac Allograft Recipients Using Gene Expression Profiling. Am. J. Transplant. 2006, 6, 150–160. [Google Scholar] [CrossRef] [PubMed]
- Pham, M.X.; Teuteberg, J.J.; Kfoury, A.G.; Starling, R.C.; Deng, M.C.; Cappola, T.P.; Kao, A.; Anderson, A.S.; Cotts, W.G.; Ewald, G.A.; et al. Gene-Expression Profiling for Rejection Surveillance after Cardiac Transplantation. N. Engl. J. Med. 2010, 362, 1890–1900. [Google Scholar] [CrossRef]
- Kobashigawa, J.; Patel, J.; Azarbal, B.; Kittleson, M.; Chang, D.; Czer, L.; Daun, T.; Luu, M.; Trento, A.; Cheng, R.; et al. Randomized Pilot Trial of Gene Expression Profiling versus Heart Biopsy in the First Year after Heart Transplant: Early Invasive Monitoring Attenuation through Gene Expression Trial. Circ. Heart Fail. 2015, 8, 557–564. [Google Scholar] [CrossRef]
- Crespo-Leiro, M.G.; Stypmann, J.; Schulz, U.; Zuckermann, A.; Mohacsi, P.; Bara, C.; Ross, H.; Parameshwar, J.; Zakliczyński, M.; Fiocchi, R.; et al. Clinical Usefulness of Gene-Expression Profile to Rule out Acute Rejection after Heart Transplantation: CARGO II. Eur. Heart J. 2016, 37, 2591–2601. [Google Scholar] [CrossRef] [PubMed]
- Novák, J.; Macháčková, T.; Krejčí, J.; Bienertová-Vašků, J.; Slabý, O. MicroRNAs as Theranostic Markers in Cardiac Allograft Transplantation: From Murine Models to Clinical Practice. Theranostics 2021, 11, 6058–6073. [Google Scholar] [CrossRef] [PubMed]
- Grankvist, R.; Chireh, A.; Sandell, M.; Mukarram, A.K.; Jaff, N.; Berggren, I.; Persson, H.; Linde, C.; Arnberg, F.; Lundberg, J.; et al. Myocardial micro-biopsy procedure for molecular characterization with increased precision and reduced trauma. Sci. Rep. 2020, 10, 8029. [Google Scholar] [CrossRef]
- Halloran, P.F.; Potena, L.; Van Huyen, J.D.; Bruneval, P.; Leone, O.; Kim, D.H.; Jouven, X.; Reeve, J.; Loupy, A. Building a tissue-based molecular diagnostic system in heart transplant rejection: The heart Molecular Microscope Diagnostic (MMDx) System. J. Heart Lung Transplant. 2017, 36, 1192–1200. [Google Scholar] [CrossRef]





| Characteristics | Heart Recipients (n = 212) |
|---|---|
| Male sex, n (%) | 158 (75%) |
| Age at time of HT, years | 57 (49–65) |
| Dilated cardiomyopathy, n (%) | 86 (41%) |
| Ischemic cardiomyopathy, n (%) | 85 (40%) |
| Valvular cardiomyopathy, n (%) | 11 (5%) |
| Myocarditis, n (%) | 9 (4%) |
| Peri-partum cardiomyopathy | 5 (2%) |
| Hypertrophic cardiomyopathy, n (%) | 3 (1%) |
| Radiation- or chemotherapy-induced cardiomyopathy | 3 (1%) |
| Arrhythmogenic right ventricular dysplasia | 3 (1%) |
| Other cardiomyopathies | 7 (3%) |
| Endomyocardial biopsy, n (interquartile range) | 9 (2–12) |
| Characteristics | Total EMBs (n = 1698) | Trans-Jugular EMBs (n = 927) | Trans-Femoral EMBs (n = 771) | p |
|---|---|---|---|---|
| Male sex, n (%) | 1309 (77%) | 744 (80%) | 565 (73%) | <0.001 |
| Age at time of EMB, years | 57 (49–63) | 57 (50–64) | 56 (47–63) | 0.003 |
| Time from HT, years | 0.4 (0.1–0.9) | 0.2 (0.1–0.5) | 0.7 (0.3–2.8) | <0.001 |
| Total Complications, n (%) | 60 (3.5%) | 38 (4%) | 22 (3%) | 0.16 |
| Major complications, n (%) | 9 (0.5%) | 6 (1%) | 3 (0.4%) | 0.65 |
| Cardiac tamponade n (%) | 6 (0.4%) | 4 (0.4%) | 2 (0.3%) | 0.55 |
| Pneumothorax, n (%) | 2 (0.1%) | 2 (0.2%) | 0 | - |
| Retroperitoneal bleeding | 1 (0.05%) | 0 | 1 (0.1%) | - |
| Minor complications, n (%) | 51 (3%) | 32 (3%) | 19 (2%) | 0.23 |
| Coronary artery fistulae, n (%) | 7 (0.4%) | 0 | 7 (1%) | - |
| De novo tricuspid regurgitation, n (%) | 5 (0.3%) | 3 (0.3%) | 2 (0.3%) | 0.8 |
| Arrhythmias, n (%) | 4 (0.2%) | 3 (0.3%) | 1 (0.1%) | 0.4 |
| Vascular access site, n (%) | 35 (2%) | 26 (3%) | 9 (1%) | 0.02 |
| Hematoma, n (%) | 13 (1%) | 5 (1%) | 8 (1%) | 0.24 |
| Accidental arterial puncture | 22 (1%) | 21 (2%) | 1 (0.1%) | <0.001 |
| Characteristics | Total EMBs (n = 1698) | Not Complicated EMBs (n = 1638) | Complicated EMBs (n = 60) | p |
|---|---|---|---|---|
| Male sex, n (%) | 1309 (77%) | 1267 (77%) | 42 (70%) | 0.17 |
| Age at time of EMB, years | 57 (49–63) | 57 (49–63) | 57 (46–64) | 0.78 |
| Time from HT, years | 0.4 (0.1–0.9) | 0.4 (0.1–0.9) | 0.3 (0.1–1.2) | 0.9 |
| Characteristics | All (n = 60) | Trans-Jugular (n = 38) | Trans-Femoral (n = 22) | p |
|---|---|---|---|---|
| Male sex, n (%) | 42 (70%) | 27 (71%) | 15 (68%) | 0.8 |
| Age at time of EMB, years | 57 (46–64) | 60 (47–65) | 54 (46–60) | 0.2 |
| Time from HT, years | 0.3 (0.1–1.2) | 0.2 (0.1–0.5) | 1.2 (0.5–14) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galeone, A.; Bernabei, A.; Pesarini, G.; Raimondi Lucchetti, M.; Onorati, F.; Luciani, G.B. Ten-Year Experience with Endomyocardial Biopsy after Orthotopic Heart Transplantation: Comparison between Trans-Jugular and Trans-Femoral Approach. J. Cardiovasc. Dev. Dis. 2024, 11, 115. https://doi.org/10.3390/jcdd11040115
Galeone A, Bernabei A, Pesarini G, Raimondi Lucchetti M, Onorati F, Luciani GB. Ten-Year Experience with Endomyocardial Biopsy after Orthotopic Heart Transplantation: Comparison between Trans-Jugular and Trans-Femoral Approach. Journal of Cardiovascular Development and Disease. 2024; 11(4):115. https://doi.org/10.3390/jcdd11040115
Chicago/Turabian StyleGaleone, Antonella, Annalisa Bernabei, Gabriele Pesarini, Marcello Raimondi Lucchetti, Francesco Onorati, and Giovanni Battista Luciani. 2024. "Ten-Year Experience with Endomyocardial Biopsy after Orthotopic Heart Transplantation: Comparison between Trans-Jugular and Trans-Femoral Approach" Journal of Cardiovascular Development and Disease 11, no. 4: 115. https://doi.org/10.3390/jcdd11040115
APA StyleGaleone, A., Bernabei, A., Pesarini, G., Raimondi Lucchetti, M., Onorati, F., & Luciani, G. B. (2024). Ten-Year Experience with Endomyocardial Biopsy after Orthotopic Heart Transplantation: Comparison between Trans-Jugular and Trans-Femoral Approach. Journal of Cardiovascular Development and Disease, 11(4), 115. https://doi.org/10.3390/jcdd11040115









