Abstract
Background: Whether healthy metabolic status is stable or only temporary is still controversial. The aim of the present study was to determine the frequency of the transition from metabolically healthy to metabolically unhealthy status, or vice versa, over the long term. Methods: We examined 970 individuals of 18 to 45 years of age. The participants’ mean age was 33.1 ± 8.6 years and mean BP was 145.5 ± 10.6/93.5 ± 5.7 mmHg. Participants were classified into four groups according to whether they had normal weight or overweight/obesity (OwOb) and were metabolically healthy or unhealthy. After 7.5 years, 24.3% of men and 41.9% of women in the metabolically healthy normal-weight group remained metabolically healthy (p < 0.0001). Among the metabolically healthy OwOb participants, 31.9% remained metabolically healthy, with a similar frequency in men and women. However, more OwOb women (19.1%) than men (5.7%) achieved normal weight (p < 0.0001). Among the metabolically unhealthy OwOb subjects, 81.8% of men and 69.3% of women remained metabolically unhealthy, 7.4% of men and 12.0% of women transitioned to OwOb healthy status, and 10.7% of men and 18.7% of women achieved normal weight (men versus women, p < 0.0001). Predictors of transition to unhealthy status were high BP, high BMI, and smoking. Male sex was a borderline predictor of progression to unhealthy status in OwOb participants (p = 0.073). Conclusion: These data show that metabolically healthy status is a highly unstable condition in both normal-weight and OwOb individuals. The impairment of metabolic status was more frequent in men than in women. Lifestyle counseling produced beneficial effects in almost one-third of metabolically unhealthy OwOb women and in less than one-fifth of men.
1. Introduction
Overweight and obesity are linked to several chronic diseases and are major risk factors for the development of cardiometabolic complications [1,2]. However, over 40 years ago, some investigators described an obesity phenotype characterized by lack of hypertension, insulin resistance, lipid abnormalities, and diabetes, which was defined as a “benign obesity phenotype” [2,3,4,5,6]. This condition, later called metabolically healthy obesity (MHO), has been found to be present in up to 35% of overweight or obese individuals (OwOb) [5]. However, several recent studies have found that MHO may not be a completely innocuous clinical condition, as previously believed [2,3,6,7,8,9]. The conflicting data from the literature may be due to the different criteria used to define MHO. Although metabolically healthy individuals have a favorable metabolic profile compared to their metabolically unhealthy counterparts, many studies considered obese subjects with even two metabolic abnormalities as “healthy” [2,3,4,5,6,7]. Another issue not yet resolved is whether a healthy metabolic status is permanent or only temporary. According to a recent meta-analysis, about 50% of metabolically healthy subjects develop one or more abnormal metabolic parameters during 3 to 10 years of follow-up, transitioning to a metabolically unhealthy obese status [10]. An even higher risk of progressing to an unhealthy state has been reported in recent studies [11].
To prevent the deterioration of metabolic function in OwOb individuals without metabolic abnormalities, appropriate lifestyle measures may be of help in order to decrease the risk of cardiovascular complications. However, previous clinical trials of lifestyle intervention in MHO patients obtained conflicting results [12,13,14,15]. It is thus unclear whether metabolically healthy OwOb subjects actually benefit from traditional lifestyle measures. Conversion to a metabolically unhealthy phenotype may imply a considerable increase in cardiovascular risk. Our hypothesis was that in a population of mildly hypertensive subjects, a high percentage would progress from healthy to unhealthy metabolic status and that this conversion would be more frequent in female than male participants.
Thus, the aim of the present study was to investigate the frequency of the transition from metabolically healthy OwOb to metabolically unhealthy OwOb status, and vice versa, during a 7.5-year period and to ascertain whether progression to unhealthy metabolic status differed in men and women. The protocol included periodic counseling by healthcare personnel on how to adopt or maintain a healthy lifestyle. This investigation was conducted in the young to middle-aged participants from the Hypertension and Ambulatory Recording VEnetia STudy (HARVEST), a multicenter prospective observational study [16].
2. Material and Methods
2.1. Sample
HARVEST is a prospective study that was conducted in 17 hypertension units in Italy beginning on 1 April 1990 [16]. Subjects were never-treated 18 to 45 year olds screened for stage 1 hypertension (systolic blood pressure (BP) ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg) that were sent to the referral centers by their general practitioners. Subjects with diabetes, nephropathy, cardiovascular disease, neoplastic diseases, and any other serious clinical condition were excluded. More details on the procedures used in HARVEST can be found elsewhere [16]. A total of 970 participants for whom all metabolic data and 24-h BP were available at baseline and follow-up assessments were considered.
Patient data and blood and urine samples were periodically sent by the investigators to the coordinating center at the University of Padova, Italy, where they were processed.
2.2. Procedures
Data pertaining to the participants’ demographics, personal and family health, and medical history were collected at baseline [16]. A family history of cardiovascular disease was defined as stroke, myocardial infarction, or sudden death before the age of 60 in a first-degree relative [16]. All subjects underwent physical examination, anthropometric measurements, and blood chemistry including glucose, triglycerides, total cholesterol, and HDL-cholesterol. Body mass index (BMI) was considered as an index of adiposity (weight divided by height squared). Office BP was the average of six BP readings obtained with the auscultatory measurement during two visits performed two weeks apart. At the baseline and final examinations, participants underwent 24-h ambulatory BP measurement (ABPM), using the A&D TM2420 model 7 (A&D, Tokyo, Japan) or ICR Spacelabs 90207 monitor (Spacelabs, Redmond, WA) devices, which have been previously validated [17]. Measurements were taken using previously published procedures [16]. Average 24-h BP was calculated as the mean of the individual means calculated for each hour. The procedures followed were in accordance with institutional guidelines. The study was approved by the HARVEST ethics committee [18]. Written informed consent was obtained from the participants.
2.3. Assessment of Lifestyle Factors
A self-compiled questionnaire about smoking, alcohol and coffee consumption, and physical activity habits was collected. In keeping with previous analyses from HARVEST [16], smokers were classified into 4 categories according to the number of cigarettes smoked per day: nonsmokers; 1–5 cigarettes/day; 6–10 cigarettes/day; and >10 cigarettes/day. Heavy smokers (>20 cigarettes/day) were not included in the study [16]. Previous smoking was not considered in the present investigation. Coffee consumption was categorized according to the number of caffeine-containing cups of coffee drunk per day: only espresso and moka coffee brews are commonly consumed in Italy. Three categories of coffee drinkers were considered: nondrinkers (0 cups/day), moderate drinkers (1–3 cups/day), and heavy drinkers (>3 cups/day) [16]. Alcohol intake was calculated by summing the total number of milliliters of daily alcohol consumption of wine, beer, and liqueurs. Wine accounts for most of the alcohol intake in the Italian population and an accepted threshold level between mild and moderate drinking, according to Italian standards, is 0.50 g/day [16]. Thus, participants were divided into four categories of alcohol consumption: (1) nondrinkers, (2) those who drank <50 g/day (mild drinkers), (3) those who drank between 50 and 100 g/day (moderate drinkers), and (4) those who drank >100 g/day (heavy drinkers). As only a few subjects reported drinking > 100 g/day, groups 3 and 4 were combined to obtain three categories of alcohol consumption: 0 g/day, <50 g/day, and ≥50 g/day. Participants were grouped into four categories of physical activity: sedentary if they did not regularly perform any physical activity; mild exercisers if they performed light physical activities like walking, gardening, etc.; moderate exercisers if they engaged in leisure time sports activities; and athletes if they participated in competitive sports activities [16].
2.4. Combined BMI and Metabolic Status Definition
Subjects were grouped into 3 BMI categories: normal weight (BMI < 25 kg/m2), overweight (BMI from 25 to 29.9 kg/m2), and obesity (BMI ≥ 30 kg/m2). Metabolic status was defined using the criteria suggested by Lavie and colleagues [4]; however, to allow for a more precise identification of the subjects with normal BP, people with average 24-h BP < 130/80 mmHg were defined as normotensive [19]. Thus, healthy metabolic status was defined as an average ambulatory BP < 130/80 mmHg and the absence of any abnormal metabolic parameter (fasting glucose < 100 mg/dL, triglyceride < 150 mg/dL, and high-density lipoprotein cholesterol (HDL-cholesterol) ≥ 40 mg/dL in men and ≥50 mg/dL in women). Unhealthy metabolic status was defined as an ambulatory BP ≥ 130/80 mmHg and/or one or more abnormal metabolic parameters.
2.5. Follow-Up
After the two baseline visits, nonpharmacological measures were implemented following the recommendations of current international guidelines. All participants were followed closely during the first 6 months and thereafter at 6-month intervals until they developed hypertension requiring antihypertensive treatment according to current guidelines [18]. At each visit, recommendations about healthy lifestyle behavior were provided by the HARVEST investigators following current guidelines. If patients developed sustained hypertension needing antihypertensive treatment, the investigators performed a final clinical assessment before treatment was administered. Antihypertensive treatment was initiated following the guidelines or criteria for young subjects with low cardiovascular risk available at the time of patient assessment. Before initiating antihypertensive treatment, body weight measurement, ambulatory BP assessment, and biochemical tests were repeated. Only data obtained in untreated subjects were used. Other details on follow-up procedures in the HARVEST are reported elsewhere [16,18]. Mean duration of the present follow-up was 7.5 ± 4.5 years.
2.6. Statistics
Quantitative variables are reported as mean ± SD, unless specified. Categorical variables are reported as percentage and differences in the distribution and were tested by χ2 test. Differences across groups were tested by ANCOVA, adjusting for age and sex. Intra-individual comparisons of baseline and follow-up variables were performed with paired t-tests. Multivariable logistic regression was used to predict the likelihood of transitioning from healthy to unhealthy metabolic status. The reproducibility of metabolically healthy OwOb was evaluated using kappa statistics, according to Cohen’s method using linear weight [20]. The standard error and 95% confidence interval were calculated according to Fleiss et al. [21]. The strength of agreement was defined as poor if kappa was <0.20, fair if kappa was 0.21–0.40, moderate if kappa was 0.41–0.60, good if kappa was 0.61–0.80, and very good if kappa was 0.81–1.00 [22]. A two-tailed probability value ≤ 0.05 was considered significant. Analyses were performed using Systat version 12 (SPSS Inc., Evanston, IL, USA), and MedCalc version 20.218 (MedCalc Software Ltd., Ostend, Belgium).
3. Results
Of the 970 participants, 47.8% had normal weight, 42.3% were overweight, and 9.9% had obesity. At the end of follow-up, the percentages were 38.5%, 46.7%, and 14.8%, respectively (p < 0.001). The mean increase in body weight was 2.3 ± 6.8 kg/m2. Healthy metabolic status was present in 23.0% of the participants at baseline and in 19.7% at the end of follow-up (p < 0.001).
The clinical characteristics of the participants stratified by their metabolic health status and BMI group (<25 kg/m2 or ≥25 kg/m2) at baseline are reported in Table 1. OwOb subjects were older, more frequently male, alcohol and coffee consumers, and had higher diastolic BP and worse metabolic profile than people with normal weight. Metabolically unhealthy participants were older, heavier, were more frequently male, alcohol consumers and smokers, and had higher systolic and diastolic 24-h BP than their metabolically healthy counterparts. The clinical characteristics of the participants at follow-up end are displayed in Table 2. Compared with baseline, office systolic BP and heart rate declined after the observational period. In contrast, both systolic and diastolic ambulatory BPs significantly increased over time, as did all metabolic variables.

Table 1.
Characteristics of 970 HARVEST participants grouped according to metabolic status and body mass index at baseline.

Table 2.
Characteristics of 970 HARVEST participants grouped according to metabolic status and body mass index at the end of follow-up.
At baseline, 132 participants (13.6%) were metabolically healthy normal weight, 91 (9.4%) were metabolically healthy OwOb, 332 (34.2%) were metabolically unhealthy normal weight, and 415 (42.8%) were metabolically unhealthy OwOb (Figure 1). The prevalence of metabolically healthy normal weight subjects was higher among the women whereas the prevalence of metabolically unhealthy OwOb participants was higher among the men (p < 0.0001, Figure S1). At the end of follow-up, these percentages were 10.3%, 9.4%, 28.2%, and 52.1%, respectively (p < 0.0001 versus baseline). Again, the metabolically healthy normal-weight condition was more prevalent among the female participants and the metabolically unhealthy OwOb state among the male participants (p < 0.0001, Figure S2).
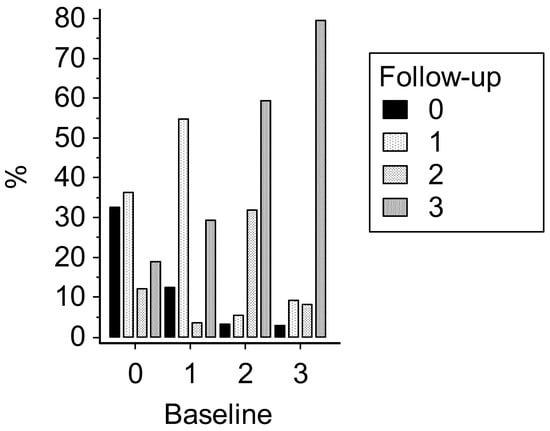
Figure 1.
Classification of 970 HARVEST participants grouped according to BMI (kg/m2) and metabolic status at baseline and end of follow-up. Subjects without any abnormal parameter were defined as being metabolically healthy (Metab −). Subjects with at least one abnormal parameter were defined as being metabolically unhealthy (Metab +). 0 = BMI < 25 kg/m2/Metab −; 1 = BMI < 25 kg/m2/Metab +; 2 = BMI ≥ 25 kg/m2/Metab −; 3 = BMI ≥ 25 kg/m2/Metab +.
After 7.5 years, only 32.6% (men, 24.3%; women, 41.9%) of metabolically healthy normal-weight subjects remained metabolically healthy, while 36.4% transitioned to unhealthy normal-weight status (men, 37.1%; women, 35.5%), and 31.1% to OwOb (men, 38.5%; women, 22.6%; men versus women, p < 0.0001). Follow-up changes in body weight (mean ± SEM) were +1.9 ± 0.8, 2.6 ± 0.7, and 8.6 ± 0.8 kg, respectively, in the three groups (age-and-sex-adjusted p < 0.001). Among the metabolically healthy OwOb participants, 31.9% (men, 32.9%; women, 28.6%) remained metabolically healthy, whereas 59.3% (men, 61.5%; women, 52.4%) transitioned to the OwOb unhealthy condition, and 8.8% (men, 5.7%; women, 19.1%) achieved normal weight (men versus women, p < 0.0001, Figure 2). Body weight changes in the three groups were +3.2 ± 1.7, +4.0 ± 1.2, and −13.3 ± 3.2 kg, respectively (p < 0.001).
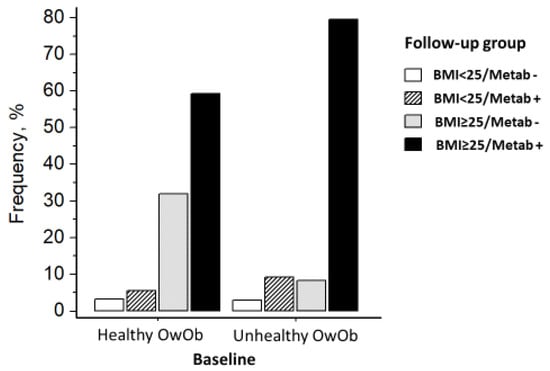
Figure 2.
Change in BMI/metabolic status from baseline to end of follow-up in 506 HARVEST participants with overweight or obesity at baseline. BMI indicates body mass index; OwOb, overweight or obesity; Metab −, metabolically healthy; Metab +, metabolically unhealthy.
At the end of follow-up, only 12.4% of metabolically unhealthy normal-weight subjects improved their metabolic status (men, 11.2%; women, 15.0%); 54.7% remained metabolically unhealthy (men, 50.4%; women, 63.6%) and 32.9% transitioned to the OwOb condition (men, 38.4%; women, 21.5%). Follow-up changes in body weight were +0.5 ± 0.6, 1.6 ± 0.3, and 7.4 ± 0.4 kg, respectively, in the three groups (p < 0.001).
Among the metabolically unhealthy OwOb subjects, 79.6% remained metabolically unhealthy (Men, 81.8%; women, 69.3%), 8.3% transitioned to OwOb healthy status (Men, 7.4%; women, 12.0%), and 12.1% achieved normal weight (Figure 2) (men, 10.7%; women, 18.7%). Body weight changes in the three groups were +2.3 ± 0.3, +2.2 ± 1.1, and −9.4 ± 0.9 kg, respectively (p < 0.001).
3.1. Reproducibility of Metabolically Healthy Status
Metabolically healthy status reproducibility evaluated with weighted Kappa (WK) in the whole sample was fair (WK, 0.25, 95%CI 0.15–0.34) and was better in men (WK, 0.27, 95%CI 0.16–0.38) than in women (WK, 0.18, 95%CI 0.01–0.36). In the normal-weight subjects, metabolically healthy status showed a similar agreement (WK, 0.23, 95%CI 0.13–0.32). In the OwOb participants, healthy status showed a slightly better agreement (WK, 0.28, 95%CI 0.17–0.39).
3.2. Logistic Regression Analysis
In a multivariable regression analysis of the whole sample, including several clinical and metabolic variables (see Table 3), only BMI and average 24-h systolic BP were independent predictors of the transition from healthy to unhealthy metabolic status. Smoking showed a borderline association with this outcome. Within the OwOb group, average 24-h systolic BP (p = 0.027) and smoking (p = 0.034) were the only independent predictors of transition to unhealthy metabolic status. Sex was not a significant predictor of transition to unhealthy metabolic status in the whole population (p = 0.51). However, in the OwOb subgroup, male sex had a borderline association with progression to unhealthy metabolic status (p = 0.073).

Table 3.
Logistic regression analysis showing the relationship of several clinical variables with the transition from healthy to unhealthy metabolic status during follow-up (dependent variable) in 970 HARVEST participants.
4. Discussion
In this population of young-to-middle-aged subjects screened for stage 1 hypertension, we found that metabolically healthy status at baseline was present in about one-quarter of the participants and that it was more prevalent in women than in men. However, healthy status appeared to be a highly unstable condition in both normal weight and OwOb individuals, as only one-third of people with this phenotype retained a metabolically healthy status after 7.5 years of observation. Progression from metabolically healthy to unhealthy status was more common in men than women. BMI, ambulatory systolic BP, and smoking were independent predictors of the transition to the unhealthy phenotype.
Previous studies have revealed that MHO may not be a stable condition as a large proportion of MHO individuals may transition to unhealthy metabolic phenotype over time [10,11,15,23,24,25,26,27,28]. According to a meta-analysis, about 50% of metabolically healthy subjects developed one or more abnormal metabolic parameters during 3 to 10 years of follow-up, transitioning to metabolically unhealthy obesity [10]. In a recent analysis of the Framingham Offspring study [11], only 29% of initially MHO participants (mean age, 57.3 years) retained their healthy metabolic status over a 12.9-year observational period. In the present study, a slightly greater proportion of metabolically healthy OwOb people retained this condition (31.9%), probably due to the shorter exposure time (7.5 years) and the younger age of the participants (33.8 years). It is noteworthy to observe that metabolically healthy individuals with normal BMI had similar risk of progressing to the metabolic abnormal state to their OwOb counterparts. This finding is in contrast with the results of previous investigations that found a higher proportion of resilient metabolic phenotypes in normal weight subjects than in obese subjects [10]. This is probably due to the peculiar characteristics of our population that included mostly young people with mildly elevated BP. Of note, the high rate of progression to unhealthy metabolic status in the present study was seen despite participants receiving detailed information about the advantages of keeping a healthy lifestyle.
Despite the large body of evidence indicating that MHO is not a stable condition, little attention has been paid by clinical researchers to the factors that can predict the transition to a metabolically unhealthy phenotype. Young age and being active in sports have been found to be more common in MHO subjects than in people with unhealthy obesity [10,29]. In agreement with previous research [10,29], in the present study, male sex was more common among the metabolically unhealthy participants and was a borderline predictor of progression to unhealthy status in OwOb individuals. Ambulatory 24-h BP load, degree of adiposity, and smoking were also predictive of progression to unhealthy OwOb phenotype, suggesting that medical attention should be focused on patients with these characteristics.
K-statistics showed that the long-term reproducibility of healthy metabolic status was only fair in both the normal-weight and OwOb groups. This low agreement was more frequently present among the women and may be partly due to the strict criteria we used to define healthy metabolic status, as only people without any abnormal metabolic parameter were defined as being metabolically healthy. However, despite the large number of the HARVEST participants transitioning to the unhealthy condition, in a previous analysis of HARVEST data [30] we showed that the group with healthy OwOb at baseline had a lower risk of adverse outcomes than the metabolically unhealthy OwOb group, which was in agreement with the results of previous investigations [24,27]. These findings suggest that also nonresilient MHO status is associated with lower cardiovascular risk than permanent metabolically unhealthy state.
Despite the general impairment of the 24-h BP load and all metabolic parameters, and the larger proportion of OwOb subjects with metabolically unhealthy status after the observational period, an interesting finding of the present study is that among the OwOb individuals, a transition to healthy metabolic status or to normal weight was observed in 18.1% of the previously metabolically unhealthy men and in 30.7% of the metabolically unhealthy women. These findings suggest that lifestyle counseling, as performed by the HARVEST investigators, can produce significant beneficial effects in a sizeable proportion of metabolically unhealthy overweight or obese patients and that the metabolic improvement occurs more frequently in women than men.
5. Study Limitations
Several limitations of the present study should be acknowledged. First, obesity was present only in a minority of our participants and thus the present results mainly apply to people with overweight. In the HARVEST cohort, there is a low prevalence of females because of the natural selection of people with stage 1 hypertension in this age range, which has been shown to occur across different ethnic groups [31,32,33]. However, the number of women was large enough to allow for meaningful between-sex comparisons. The present data were not obtained from a general population but from 18-to-45-year-old patients screened for stage 1 hypertension and thus they are applicable only to young-to-middle-aged patients with high BP. Finally, waist circumference, a better indicator of cardiometabolic risk than BMI, was not available.
6. Conclusions
Overweight and obesity may lead to adverse cardiovascular outcomes, especially when they are associated with metabolic abnormalities. Thus, the assessment of metabolic status is of paramount importance for identifying people who may benefit from interventions addressed to improve subjects’ lifestyle. In the present study, lifestyle counseling by the HARVEST investigators produced a significant weight loss and/or an improvement in metabolic status in a sizeable proportion of the metabolically unhealthy OwOb patients, especially women. However, our data also indicate that the presence of healthy metabolic status in people with overweight or obesity should not be considered an innocent condition. About 60% of our metabolically healthy OwOb participants gained body weight and lost their healthy status during follow-up, suggesting that counseling about diet and other lifestyle measures should also be provided to obese people without metabolic abnormalities to avoid the transition to a metabolically unhealthy condition.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcdd11020047/s1. Figure S1. Classification of 970 HARVEST participants grouped according to BMI (kg/m2) and metabolic status, stratified by sex. Subjects without any abnormal parameter were defined as being metabolically healthy (Metab −). Data at baseline. Figure S2. Classification of 970 HARVEST participants grouped according to BMI (kg/m2) and metabolic, stratified by sex. Subjects without any abnormal parameter were defined as being metabolically healthy (Metab −). Data at follow-up end.
Author Contributions
All authors have contributed to the work. Conceptualization, P.P.; Data curation, F.S. and M.R.; Formal analysis, P.P. and M.R.; Funding acquisition, L.M.; Investigation, A.E. and M.C.; Methodology, O.V., F.B., A.M. and M.C.; Resources, F.S.; Writing—original draft, P.P.; Writing—review and editing, P.P., F.S., L.M., O.V., A.E., F.B., A.M., M.C. and M.R. All authors have read and agreed to the published version of the manuscript.
Funding
All studies based on HARVEST data are funded by the Associazione “18 maggio 1370”, San Daniele del Friuli, Italy.
Institutional Review Board Statement
The study protocol followed the principles of the Declaration of Helsinki. The HARVEST study was approved by the HARVEST Ethics Committee (Ref. [16]) and by the Department of Clinical and Experimental Medicine of the University of Padova, Italy on 1 April 1990.
Informed Consent Statement
Written informed consent, including consent for future publication of data, was given by the participants.
Data Availability Statement
The data that support the findings of this study are available on reasonable request from the HARVEST study group.
Conflicts of Interest
The authors are not directly or indirectly related to the work submitted for publication.
References
- Kivimäki, M.; Kuosma, E.; E Ferrie, J.; Luukkonen, R.; Nyberg, S.T.; Alfredsson, L.; Batty, G.D.; Brunner, E.J.; Fransson, E.; Goldberg, M.; et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: Pooled analysis of individual-level data for 120,813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health 2017, 2, e277–e285. [Google Scholar] [CrossRef]
- Eckel, N.; Meidtner, K.; Kalle-Uhlmann, T.; Stefan, N.; Schulze, M.B. Metabolically healthy obesity and cardiovascular events: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2016, 23, 956–966. [Google Scholar] [CrossRef] [PubMed]
- Kramer, C.K.; Zinman, B.; Retnakaran, R. Are metabolically healthy overweight and obesity benign conditions? A systematic review and meta-analysis. Ann. Intern. Med. 2013, 159, 758–769. [Google Scholar] [CrossRef]
- Lavie, C.J.; Laddu, D.; Arena, R.; Ortega, F.B.; Alpert, M.A.; Kushner, R.F. Healthy Weight and Obesity Prevention: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1506–1531. [Google Scholar] [CrossRef]
- Magkos, F. Metabolically healthy obesity: Whats in a name? Am. J. Clin. Nutr. 2019, 110, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Song, Y.; Chen, Y.; Hui, R.; Zhang, W. Combined effect of obesity and cardio-metabolic abnormality on the risk of cardio-vascular disease: A meta-analysis of prospective cohort studies. Int. J. Cardiol. 2013, 168, 4761–4768. [Google Scholar] [CrossRef]
- Zheng, R.; Zhou, D.; Zhu, Y. The long-term prognosis of cardiovascular disease and all-cause mortality for metabolically healthy obesity: A systematic review and meta-analysis. J. Epidemiol. Community Health 2016, 70, 1024–1031. [Google Scholar] [CrossRef]
- Agius, R.; Pace, N.P.; Fava, S. Phenotyping obesity: A focus on metabolically healthy obesity and metabolically unhealthy normal weight. Diabetes/Metab. Res. Rev. 2023, e3725. [Google Scholar] [CrossRef]
- Lavie, C.J.; Neeland, I.J. Is Metabolically Healthy Obesity Really Healthy for the Heart? JACC Cardiovasc. Imaging 2023, 16, 902–904. [Google Scholar] [CrossRef]
- Lin, H.; Zhang, L.; Zheng, R.; Zheng, Y. The prevalence, metabolic risk and effects of lifestyle intervention for metabolically healthy obesity: A systematic review and meta-analysis: A PRISMA-compliant article. Medicine 2017, 96, e8838. [Google Scholar] [CrossRef]
- Kouvari, M.; D’Cunha, N.M.; Tsiampalis, T.; Zec, M.; Sergi, D.; Travica, N.; Marx, W.; McKune, A.J.; Panagiotakos, D.B.; Naumovski, N. Metabolically Healthy Overweight and Obesity, Transition to Metabolically Unhealthy Status and Cognitive Function: Results from the Framingham Offspring Study. Nutrients 2023, 15, 1289. [Google Scholar] [CrossRef] [PubMed]
- Janiszewski, P.M.; Ross, R. Effects of Weight Loss Among Metabolically Healthy Obese Men and Women. Diabetes Care 2010, 33, 1957–1959. [Google Scholar] [CrossRef] [PubMed]
- Karelis, A.D.; Messier, V.; Brochu, M.; Rabasa-Lhoret, R. Metabolically healthy but obese women: Effect of an energy-restricted diet. Diabetologia 2008, 51, 1752–1754. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Ortega, F.B.; Labayen, I. A weight loss diet intervention has a similar beneficial effect on both metabolically abnormal obese and metabolically healthy but obese premenopausal women. Ann. Nutr. Metab. 2013, 62, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Lei, L.; Changfa, W.; Ting, Y.; Xiaoling, Z.; Yaqin, W. Metabolically healthy transition and its association with body size change patterns among different adult age groups. Diabetes Res. Clin. Pr. 2022, 192, 110108. [Google Scholar] [CrossRef] [PubMed]
- Palatini, P.; Fania, C.; Mos, L.; Mazzer, A.; Saladini, F.; Casiglia, E. Alcohol Intake More than Doubles the Risk of Early Cardiovascular Events in Young Hypertensive Smokers. Am. J. Med. 2017, 130, 967–974.e1. [Google Scholar] [CrossRef]
- O’Brien, E.; Mee, F.; Atkins, N.; O’Malley, K. Accuracy of the SpaceLabs 90207 determined by the British Hypertension Society Protocol. J. Hypertens. 1991, 9, 573–574. [Google Scholar] [CrossRef]
- Palatini, P.; Pessina, A.C.; Dal Palù, C. The Hypertension and Ambulatory Recording Venetia Study (HARVEST): A trial on the predictive value of ambulatory blood pressure monitoring for the development of fixed hypertension in patients with borderline hypertension. High Blood Press 1993, 2, 11–18. [Google Scholar]
- Stergiou, G.S.; Palatini, P.; Parati, G.; O’Brien, E.; Januszewicz, A.; Lurbe, E.; Persu, A.; Mancia, G.; Kreutz, R. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J. Hypertens. 2021, 39, 1293–1302. [Google Scholar] [CrossRef]
- Cohen, J. Weighted kappa: Nominal scale agreement provision for scaled disagreement or partial credit. Psychol. Bull. 1968, 70, 213–220. [Google Scholar] [CrossRef]
- Fleiss, J.L.; Levin, B.; Paik, M.C. Statistical Methods for Rates and Proportions, 3rd ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2003. [Google Scholar]
- Altman, D.G. Practical Statistics for Medical Research; Chapman and Hall: London, UK, 1991. [Google Scholar]
- Abiri, B.; Koohi, F.; Ebadinejad, A.; Valizadeh, M.; Hosseinpanah, F. Transition from metabolically healthy to unhealthy overweight/obesity and risk of cardiovascular disease incidence: A systematic review and meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 2041–2051. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.S.; Ning, H.; Wilkins, J.T.; Allen, N.; Carnethon, M.; Berry, J.D.; Sweis, R.N.; Lloyd-Jones, D.M. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 2018, 3, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Mongraw-Chaffin, M.; Foster, M.C.; Anderson, C.A.; Burke, G.L.; Haq, N.; Kalyani, R.R.; Ouyang, P.; Sibley, C.T.; Tracy, R.; Woodward, M.; et al. Metabolically Healthy Obesity, Transition to Metabolic Syndrome, and Cardiovascular Risk. J. Am. Coll. Cardiol. 2018, 71, 1857–1865. [Google Scholar] [CrossRef] [PubMed]
- Fingeret, M.; Marques-Vidal, P.; Vollenweider, P. Incidence of type 2 diabetes, hypertension, and dyslipidemia in metabolically healthy obese and non-obese. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 1036–1044. [Google Scholar] [CrossRef] [PubMed]
- Kouvari, M.; Panagiotakos, D.B.; Yannakoulia, M.; Georgousopoulou, E.; Critselis, E.; Chrysohoou, C.; Tousoulis, D.; Pitsavos, C. Transition from metabol-ically benign to metabolically unhealthy obesity and 10-year cardiovascular disease incidence: The ATTICA cohort study. Metabolism 2019, 93, 18–24. [Google Scholar] [CrossRef]
- Kouvari, M.; Chrysohoou, C.; Skoumas, J.; Pitsavos, C.; Panagiotakos, D.B.; Mantzoros, C.S.; ATTICA Study Investigators. The presence of NAFLD influences the transition of metabolically healthy to metabolically unhealthy obesity and the ten-year cardiovascular disease risk: A population-based cohort study. Metabolism 2021, 128, 154893. [Google Scholar] [CrossRef]
- Zheng, R.; Yang, M.; Bao, Y.; Li, H.; Shan, Z.; Zhang, B.; Liu, J.; Lv, Q.; Wu, O.; Zhu, Y.; et al. Prevalence and Determinants of Metabolic Health in Subjects with Obesity in Chinese Population. Int. J. Environ. Res. Public Health 2015, 12, 13662–13677. [Google Scholar] [CrossRef] [PubMed]
- Palatini, P.; Saladini, F.; Mos, L.; Vriz, O.; Ermolao, A.; Battista, F.; Berton, G.; Canevari, M.; Rattazzi, M. Healthy overweight and obesity in the young: Prevalence and risk of major adverse cardiovascular events. Nutr. Metab. Cardiovasc. Dis. 2023, in press. [Google Scholar] [CrossRef]
- Parcha, V.; Patel, N.; Kalra, R.; Arora, G.; Arora, P. Prevalence, Awareness, Treatment, and Poor Control of Hypertension Among Young American Adults: Race-Stratified Analysis of the National Health and Nutrition Examination Survey. Mayo Clin. Proc. 2020, 95, 1390–1403. [Google Scholar] [CrossRef]
- Citoni, B.; Figliuzzi, I.; Presta, V.; Cesario, V.; Miceli, F.; Bianchi, F.; Ferrucci, A.; Volpe, M.; Tocci, G. Prevalence and clinical characteristics of isolated systolic hypertension in young: Analysis of 24 h ambulatory blood pressure monitoring database. J. Hum. Hypertens. 2021, 36, 40–50. [Google Scholar] [CrossRef]
- Sabapathy, K.; Mwita, F.C.; Dauya, E.; Bandason, T.; Simms, V.; Chikwari, C.D.; Doyle, A.M.; Ross, D.; Shah, A.; Hayes, R.J.; et al. Prevalence of hypertension and high-normal blood pressure among young adults in Zimbabwe: Findings from a large, cross-sectional population-based survey. Lancet Child Adolesc. Health 2024, 8, 101–111. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).