Bridging the Gender Gap in Cardiovascular Medicine: Addressing Drug Intolerances and Personalized Care for Women with Angina/Ischemia with Non-Obstructive Coronary Artery Disease
Abstract
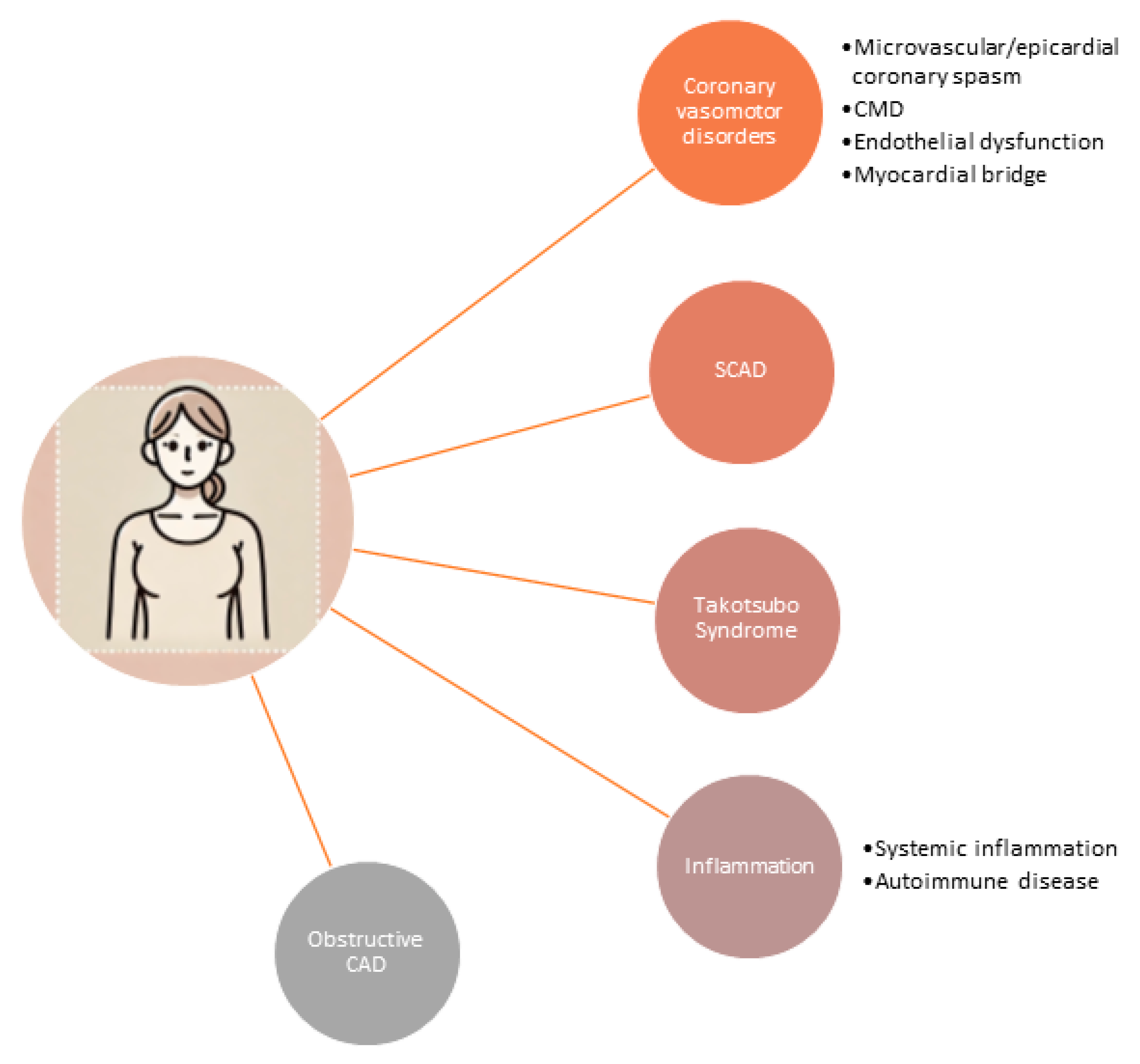
1. Gender Differences in Cardiovascular Medicine
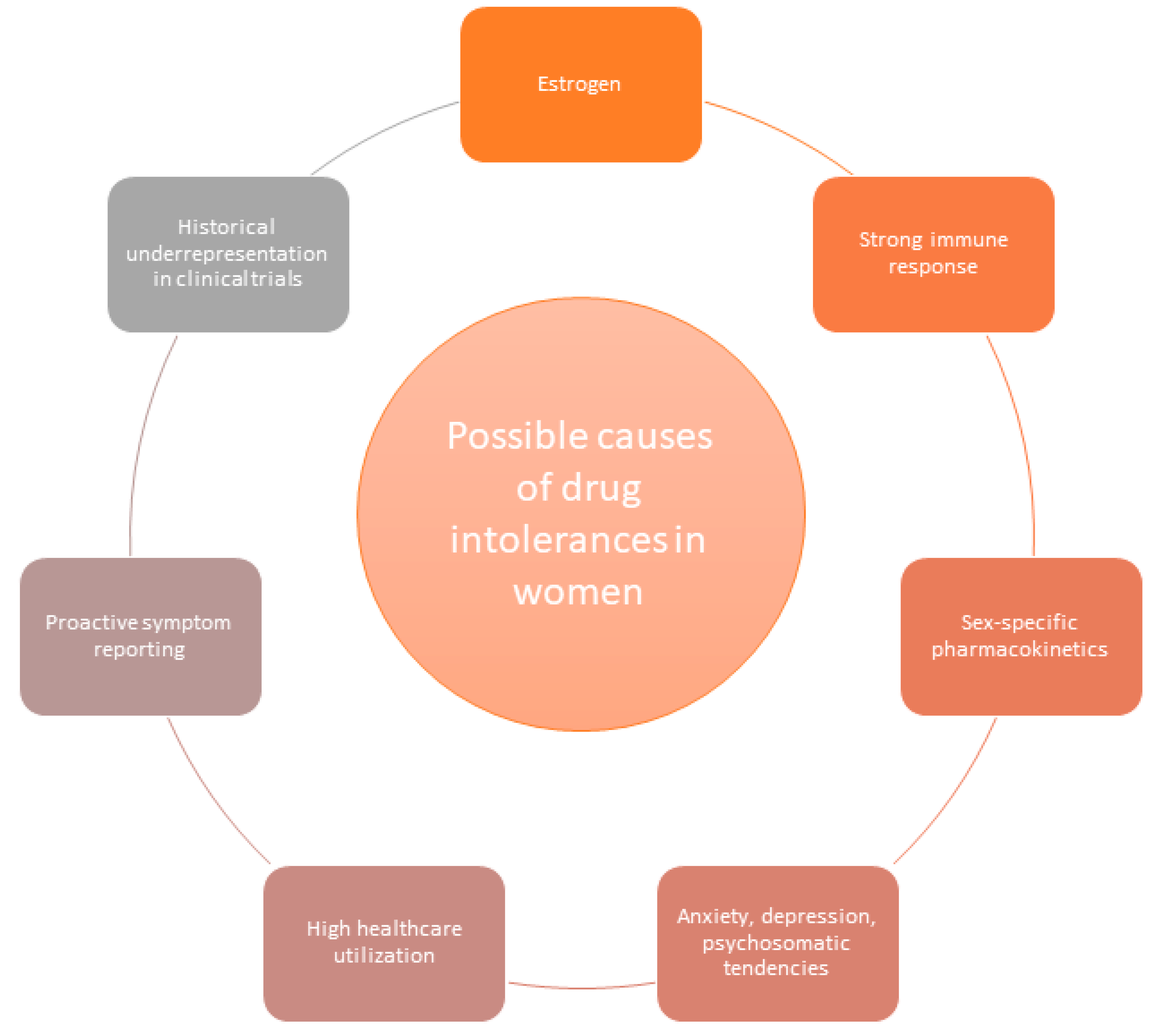
2. Multiple Drug Intolerance Syndrome
3. Possible Causes of High Prevalence of MDIS in Women
4. Drug Intolerances in ANOCA/INOCA Therapy
- Initiate lower drug doses in women, gradually increasing the dosage over a longer period to improve drug tolerance [48].
- Consider ranolazine for patients experiencing adverse reactions like bradycardia or hypotension, as it does not significantly lower heart rate or blood pressure [49].
- Incorporate supplements, such as magnesium, especially for patients with coronary spasm, to promote vascular relaxation without significant side effects [50].
- Explore alternative therapies to improve quality of life, such as repurposing drugs like endothelin receptor antagonists or sGC stimulators/activators [46].
5. Outlook: Addressing Drug Intolerances in Women and Closing the Gender Gap
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Oertelt-Prigione, S.; Regitz-Zagrosek, V. Sex and Gender Aspects in Clinical Medicine; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- Chander, M.P.; Kartick, C.; Gangadhar, J.; Vijayachari, P. Ethno medicine and healthcare practices among Nicobarese of Car Nicobar—An indigenous tribe of Andaman and Nicobar Islands. J. Ethnopharmacol. 2014, 158, 18–24. [Google Scholar] [CrossRef]
- Baessler, A.; Bauer, P.; Becker, M.; Berrisch-Rahmel, S.; Goldmann, B.; Grünig, E.; Hamm, C.; Meder, B.; Kindermann, I.; Ong, P.; et al. Geschlechterspezifische Aspekte kardiovaskulärer Erkrankungen. Die Kardiol. 2024, 18, 293–321. [Google Scholar] [CrossRef]
- Shaw, L.J.; Bugiardini, R.; Merz, C.N.B. Women and ischemic heart disease: Evolving knowledge. J. Am. Col-Lege Cardiol. 2009, 54, 1561–1575. [Google Scholar] [CrossRef]
- Reis, S.E.; Holubkov, R.; Smith, A.; Kelsey, S.F.; Sharaf, B.L.; Reichek, N.; Rogers, W.J.; Merz, C.B.; Sopko, G.; Pepine, C.J. Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: Results from the NHLBI WISE study. Am. Heart J. 2001, 141, 735–741. [Google Scholar] [CrossRef]
- Xu, X.; Bao, H.; Strait, K.; Spertus, J.A.; Lichtman, J.H.; D’onofrio, G.; Spatz, E.; Bucholz, E.M.; Geda, M.; Lorenze, N.P.; et al. Sex Differences in perceived stress and early recovery in Young and middle-aged patients with acute myocardial infarction. Circulation 2015, 131, 614–623. [Google Scholar] [CrossRef]
- Donahue, R.P.; Rejman, K.; Rafalson, L.B.; Dmochowski, J.; Stranges, S.; Trevisan, M. Sex differences in endothelial function markers before conversion to pre-diabetes: Does the clock start ticking earlier among women? The Western New York Study. Diabetes Care 2007, 30, 354–359. [Google Scholar] [CrossRef]
- EUGenMed, Cardiovascular Clinical Study Group; Regitz-Zagrosek, V.; Oertelt-Prigione, S.; Prescott, E.; Franconi, F.; Gerdts, E.; Foryst-Ludwig, A.; Maas, A.H.; Kautzky-Willer, A.; Knappe-Wegner, D. Gender in cardi-ovascular diseases: Impact on clinical manifestations, management, and outcomes. Eur. Heart J. 2016, 37, 24–34. [Google Scholar]
- Pacheco, C.; Luu, J.; Mehta, P.K.; Wei, J.; Gulati, M.; Merz, C.N.B. INOCA and MINOCA: Are women’s heart centres the answer to under-standing and management of these increasing populations of women (and men)? Can. J. Cardiol. 2022, 38, 1611–1614. [Google Scholar] [CrossRef]
- Parvand, M.; Cai, L.; Ghadiri, S.; Humphries, K.H.; Starovoytov, A.; Daniele, P.; Prodan-Bhalla, N.; Sedlak, T.L. One-year prospective follow-up of women with INOCA and MINOCA at a canadian women’s heart centre. Can. J. Cardiol. 2022, 38, 1600–1610. [Google Scholar] [CrossRef]
- Agrawal, S.; van Eyk, J.; Sobhani, K.; Wei, J.; Bairey Merz, C.N. Sex, myocardial infarction, and the failure of risk scores in women. J. Women’s Health 2015, 24, 859–861. [Google Scholar] [CrossRef]
- Siak, J.; Shufelt, C.L.; Cook-Wiens, G.; Samuels, B.; Petersen, J.W.; Anderson, R.D.; Handberg, E.M.; Pepine, C.J.; Merz, C.N.; Wei, J. Relationship between coronary function testing and mi-graine: Results from the Women’s Ischemia Syndrome Evaluation-Coronary Vascular Dysfunction project. Vessel. Plus 2021, 5, 45. [Google Scholar] [CrossRef]
- Omer, H.M.R.B.; Hodson, J.; Thomas, S.K.; Coleman, J.J. Multiple drug intolerance syndrome: A large-scale retrospective study. Drug Saf. 2014, 37, 1037–1045. [Google Scholar] [CrossRef]
- Blumenthal, K.G.; Li, Y.; Acker, W.W.; Chang, Y.; Banerji, A.; Ghaznavi, S.; Camargo, C.A.; Zhou, L. Multiple drug intolerance syndrome and multiple drug allergy syndrome: Epidemiology and associations with anxiety and depression. Allergy 2018, 73, 2012–2023. [Google Scholar] [CrossRef]
- Hassel, J.C.; Danner, D.; Hassel, A.J. Psychosomatic or allergic symptoms? High levels for somatization in patients with drug intolerance. J. Dermatol. 2011, 38, 959–965. [Google Scholar] [CrossRef]
- Macy, E.; Ho, N.J. Multiple drug intolerance syndrome: Prevalence, clinical characteristics, and management. Ann. Allergy Asthma Immunol. 2011, 108, 88–93. [Google Scholar] [CrossRef]
- Stürzebecher, P.E.; Gouni-Berthold, I.; Mateev, C.; Frenzel, O.; Erbe, S.; Boeckel, J.N.; Scholz, M.; Schatz, U.; Weingärtner, O.; Kassner, U.; et al. Quality of life in patients with statin intolerance: A multicentre prospective registry study. Lancet Reg. Health–Eur. 2024, 43, 100981. [Google Scholar] [CrossRef]
- Smiderle, L.; Lima, L.O.; Hutz, M.H.; Sand, C.R.V.D.; Van der Sand, L.C.; Ferreira, M.E.W.; Pires, R.C.; Almeida, S.; Fiegenbaum, M. Evaluation of sexual dimorphism in the efficacy and safety of simvastatin/atorvastatin therapy in a southern Brazilian cohort. Arq. Bras. De Cardiol. 2014, 103, 33–40. [Google Scholar] [CrossRef]
- Fan, X.; Han, Y.; Sun, K.; Wang, Y.; Xin, Y.; Bai, Y.; Li, W.; Yang, T.; Song, X.; Wang, H.; et al. Sex differences in blood pressure response to antihypertensive therapy in Chinese patients with hypertension. Ann. Pharmacother. 2008, 42, 1772–1781. [Google Scholar] [CrossRef]
- Tamargo, J.; Rosano, G.; Walther, T.; Duarte, J.; Niessner, A.; Kaski, J.C.; Ceconi, C.; Drexel, H.; Kjeldsen, K.; Savarese, G.; et al. Gender differences in the effects of cardiovascular drugs. Eur. Heart J.–Cardiovasc. Pharmacother. 2017, 3, 163–182. [Google Scholar] [CrossRef]
- Seeland, U.; Regitz-Zagrosek, V. Sex and gender differences in cardiovascular drug therapy. In Sex and Gender Differences in Pharmacology; Springer Nature: Berlin/Heidelberg, Germany, 2012; pp. 211–236. [Google Scholar]
- Os, I.; Bratland, B.; Dahlöf, B.; Gisholt, K.; Syvertsen, J.O.; Tretli, S. Female preponderance for lisinopril-induced cough in hypertension. Am. J. Hypertens. 1994, 7, 1012–1015. [Google Scholar] [CrossRef]
- Sportiello, L.; Rafaniello, C.; Sullo, M.G.; Nica, M.; Scavone, C.; Bernardi, F.F.; Colombo, D.M.; Rossi, F. No substantial gender differences in suspected adverse reactions to ACE inhibitors and ARBs: Results from spontaneous reporting system in Campania Region. Expert Opin. Drug Saf. 2016, 15, 101–107. [Google Scholar] [CrossRef]
- Rydberg, D.M.; Mejyr, S.; Loikas, D.; Schenck-Gustafsson, K.; von Euler, M.; Malmström, R.E. Sex differences in spontaneous reports on adverse drug events for common antihypertensive drugs. Eur. J. Clin. Pharmacol. 2018, 74, 1165–1173. [Google Scholar] [CrossRef]
- Okada, K.; Inamori, M.; Imajyo, K.; Chiba, H.; Nonaka, T.; Shiba, T.; Sakaguchi, T.; Atsukawa, K.; Takahashi, H.; Hoshino, E.; et al. Gender differences of low-dose aspirin-associated gastroduodenal ulcer in Japanese patients. World J. Gastroenterol. WJG 2010, 16, 1896. [Google Scholar] [CrossRef]
- Berger, J.S.; Bhatt, D.L.; Cannon, C.P.; Chen, Z.; Jiang, L.; Jones, J.B.; Mehta, S.R.; Sabatine, M.S.; Steinhubl, S.R.; Topol, E.J.; et al. The relative efficacy and safety of clopidogrel in women and men: A sex-specific collaborative meta-analysis. J. Am. Coll. Cardiol. 2009, 54, 1935–1945. [Google Scholar] [CrossRef]
- Essebag, V.; Reynolds, M.R.; Hadjis, T.; Lemery, R.; Olshansky, B.; Buxton, A.E.; Josephson, M.E.; Zimetbaum, P. Sex differences in the relationship between amiodarone use and the need for permanent pacing in patients with atrial fibrillation. Arch. Intern. Med. 2007, 167, 1648–1653. [Google Scholar] [CrossRef]
- Roten, L.; Rimoldi, S.F.; Schwick, N.; Sakata, T.; Heimgartner, C.; Fuhrer, J.; Delacrétaz, E.; Tanner, H. Gender differences in patients referred for atrial fibrillation management to a tertiary center. Pacing Clin. Electrophysiol. 2009, 32, 622–626. [Google Scholar] [CrossRef]
- Klein, S.L.; Flanagan, K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef]
- Waxman, D.J.; Holloway, M.G. Sex Differences in the Expression of Hepatic Drug Metabolizing Enzymes. Mol. Pharmacol. 2009, 76, 215–228. [Google Scholar] [CrossRef]
- Luzier, A.B.; Killian, A.; Wilton, J.H.; Wilson, M.F.; Forrest, A.; Kazierad, D.J. Gender-related effects on metoprolol pharmacokinetics and pharmacodynamics in healthy volunteers. Clin. Pharmacol. Ther. 1999, 66, 594–601. [Google Scholar] [CrossRef]
- Labbé, L.; Sirois, C.; Pilote, S.; Arseneault, M.; Robitaille, N.M.; Turgeon, J.; Hamelin, B.A. Effect of gender, sex hormones, time variables and physio-logical urinary pH on apparent CYP2D6 activity as assessed by metabolic ratios of marker substrates. Pharmacogenetics Genom. 2000, 10, 425–438. [Google Scholar] [CrossRef]
- Altemus, M.; Sarvaiya, N.; Epperson, C.N. Sex differences in anxiety and depression clinical perspectives. Front. Neuroendocr. 2014, 35, 320–330. [Google Scholar] [CrossRef]
- Hiller, W.; Rief, W.; Brähler, E. Somatization in the population: From mild bodily misperceptions to disabling symptoms. Chest 2006, 41, 704–712. [Google Scholar] [CrossRef]
- Bertakis, K.D.; Azari, R.; Helms, L.J.; Callahan, E.J.; Robbins, J.A. Gender differences in the utilization of health care services. J. Fam. Pract. 2000, 49, 147–152. [Google Scholar]
- Taha, Y.K.; Dungan, J.R.; Weaver, M.T.; Xu, K.; Handberg, E.M.; Pepine, C.J.; Bairey Merz, C.N. Symptom Presentation among Women with Suspected Ische-mia and No Obstructive Coronary Artery Disease (INOCA). J. Clin. Med. 2023, 12, 5836. [Google Scholar] [CrossRef]
- Vrints, C.; Andreotti, F.; Koskinas, K.C.; Rossello, X.; Adamo, M.; Ainslie, J.; Winther, S. 2024 ESC Guidelines for the management of chronic coro-nary syndromes: Developed by the task force for the management of chronic coronary syndromes of the European Society of Cardiology (ESC) Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2024, 36, ehae177. [Google Scholar]
- McChord, J.; Hubert, A.; Sechtem, U.; Bekeredjian, R.; Ong, P.; Seitz, A. Diagnostic Yield of Comprehensive Coronary Function Testing in Patients with Angina and Unobstructed Coronary Arteries: Endotype Characterisation and Clinical Implications. Eur. Cardiol. 2024, 19, e19. [Google Scholar] [CrossRef]
- Konst, R.E.; Damman, P.; Pellegrini, D.; Hartzema-Meijer, M.J.; van Uden, B.J.; Jansen, T.P.; Elias-Smale, S.E. Vasomotor dysfunction in patients with an-gina and nonobstructive coronary artery disease is dominated by vasospasm. Int. J. Cardiol. 2021, 333, 14–20. [Google Scholar] [CrossRef]
- Ford, T.J.; Stanley, B.; Sidik, N.; Good, R.; Rocchiccioli, P.; McEntegart, M.; Berry, C. 1-year outcomes of angina management guided by invasive coro-nary function testing (CorMicA). Cardiovasc. Interv. 2020, 13, 33–45. [Google Scholar]
- Kaski, J.-C.; Crea, F.; Gersh, B.J.; Camici, P.G. Reappraisal of ischemic heart disease: Fundamental role of coronary microvascular dysfunction in the pathogenesis of angina pectoris. Circulation 2018, 138, 1463–1480. [Google Scholar] [CrossRef]
- Sinha, A.; Rahman, H.; Douiri, A.; Demir, O.M.; De Silva, K.; Clapp, B.; Perera, D. ChaMP-CMD: A phenotype-blinded, randomized controlled, cross-over trial. Circulation 2024, 149, 36–47. [Google Scholar] [CrossRef]
- Jansen, T.P.J.; Konst, R.E.; De Vos, A.; Paradies, V.; Teerenstra, S.; Van den Oord, S.C.; Elias-Smale, S.E. Efficacy of diltiazem to improve coronary vasomotor dys-function in ANOCA: The EDIT-CMD randomized clinical trial. Cardiovasc. Imaging 2022, 15, 1473–1484. [Google Scholar]
- Guarini, G.; Huqi, A.; Morrone, D.; Capozza, P.; Todiere, G.; Marzilli, M. Pharmacological approaches to coronary microvascular dys-function. Pharmacol. Ther. 2014, 144, 283–302. [Google Scholar] [CrossRef]
- Cattaneo, M.; Porretta, A.P.; Gallino, A. Ranolazine: Drug overview and possible role in primary microvascular angina man-agement. Int. J. Cardiol. 2015, 181, 376–381. [Google Scholar] [CrossRef]
- McChord, J.; Pereyra, V.M.; Froebel, S.; Bekeredjian, R.; Schwab, M.; Ong, P. Drug repurposing—A promising approach for patients with angina but non-obstructive coronary artery disease (ANOCA). Front. Cardiovasc. Med. 2023, 10, 1156456. [Google Scholar] [CrossRef]
- Seitz, A.; Feenstra, R.G.T.; Konst, R.E.; Martínez Pereyra, V.; Beck, S.; Beijk, M.A.; Ong, P. Acetylcholine rechallenge: A first step toward tailored treatment in patients with coronary artery spasm. Cardiovasc. Interv. 2022, 15, 65–75. [Google Scholar]
- Franconi, F.; Campesi, I. Sex and gender influences on pharmacological response: An overview. Expert Rev. Clin. Pharmacol. 2014, 7, 469–485. [Google Scholar] [CrossRef]
- Nash, D.T.; Nash, S.D. Ranolazine for chronic stable angina. Lancet 2008, 372, 1335–1341. [Google Scholar] [CrossRef]
- Teragawa, H.; Kato, M.; Yamagata, T.; Matsuura, H.; Kajiyama, G. The preventive effect of magnesium on coronary spasm in pa-tients with vasospastic angina. Chest 2000, 118, 1690–1695. [Google Scholar] [CrossRef]
- Pan, X.; Bao, H.; Si, Y.; Xu, C.; Chen, H.; Gao, X.; Zeng, L. Spinal cord stimulation for refractory angina pectoris: A systematic review and me-ta-analysis. Clin. J. Pain 2017, 33, 543–551. [Google Scholar] [CrossRef]
- Tebaldi, M.; Campo, G.; Ugo, F.; Guarracini, S.; Marrone, A.; Clò, S.; Abdirashid, M.; Di Mauro, M.; Rametta, F.; Di Marco, M.; et al. Coronary sinus narrowing improves coronary microcirculation function in patients with refractory angina: A multicenter prospective inroad study. Circ. Cardiovasc. Interv. 2024, 17, e013481. [Google Scholar] [CrossRef]
- Ashokprabhu, N.D.; Quesada, O.; Alvarez, Y.R.; Henry, T.D. INOCA/ANOCA: Mechanisms and novel treatments. Am. Heart J. Plus Cardiol. Res. Pract. 2023, 30, 100302. [Google Scholar] [CrossRef]
- Abbott, J.D.; Curtis, J.P. More than one way to close the gender gap. J. Am. Coll. Cardiol. 2018, 71, 2133–2135. [Google Scholar] [CrossRef]
- Sgraja, S.; Mollenhauer, J.; Seeland, U.; Kloepfer, M.; Kurscheid, C.; Amelung, V. Closing the Gap: Implementing Gender-Sensitive Care to Address Healthcare Disparities. Eur. J. Public Health 2024, 34, 607. [Google Scholar] [CrossRef]
- DeLaet, D.L. Closing the gender gap in global health. In Women’s Global Health: Norms and State Policies; Lexington Books: Lanham, MD, USA, 2013; p. 13. [Google Scholar]
- Ghadri, J.R.; Sarcon, A.; Jaguszewski, M.; Diekmann, J.; Bataiosu, R.D.; Hellermann, J.; Templin, C. Gender disparities in acute coronary syndrome: A closing gap in the short-term outcome. J. Cardiovasc. Med. 2015, 16, 355–362. [Google Scholar] [CrossRef]
| Drug Class | Common Adverse Drug Reactions | Sex Differences in Adverse Drug Reactions | References |
|---|---|---|---|
| Statins | Muscle pain, myopathy, liver enzyme elevation, fatigue, gastrointestinal symptoms | Women have a higher risk of statin-associated muscle symptoms and higher rates of discontinuation due to adverse effects | [17,18] |
| Dihydropyridine Calcium Channel Blockers (CCBs) (amlodipine, nifedipine) | Edema, constipation, headache, dizziness, flushing | Edema more common in women | [19,20] |
| β-Blockers | Fatigue, bradycardia, cold extremities, depression, sexual dysfunction | Greater reduction in blood pressure and heart rate in women treated with metoprolol and propranolol | [19] |
| ACE Inhibitors | Cough, angioedema, hypotension, dizziness, renal impairment | Dry cough is 2-3 times more frequent in women; no sex difference for angioedema | [19,20,21,22] |
| Angiotensin II Receptor Blockers (ARBs) | Dizziness, hyperkalemia, hypotension, headache | Limited data on sex-specific intolerance rates; one analysis suggests no substantial gender difference | [23] |
| Diuretics | Electrolyte imbalances, dehydration, dizziness, gout | Greater risk of hypo-osmolarity, hypokalemia, hyponatremia, and arrhythmias in women, especially with thiazides | [19,24] |
| Antiplatelet Agents (e.g., aspirin, clopidogrel) | Gastrointestinal bleeding, dyspepsia | Increased risk of GI bleeding in older women (>70 yo) with aspirin; no evidence on sex differences with clopidogrel | [25,26] |
| Anticoagulants (e.g., warfarin, DOACs) | Bleeding, bruising, anemia | Increased bleeding risk in women; women need less warfarin per week than men | [19] |
| Class III antiarrhythmic drug (amiodarone) | thyroid dysfunction, photosensitivity, visual disturbance, bradyarrhythmia, sinus arrest, and hepatotoxicity | increased risk of bradyarrhythmia requiring pacemaker insertion and phototoxicity in women | [27,28] |
| Condition | First-Line Treatment | Additional Notes |
|---|---|---|
| MVA with Reduced CFR and/or Increased IMR | β-blockers, CCBs, ranolazine, ACE-Is | Ranolazine improves exercise capacity [42] |
| Epicardial or Microvascular Coronary Spasm | CCBs (may be combined with long-acting nitrates and/or ranolazine) | Study showed diltiazem reduced epicardial spasm but did not substantially improve symptoms or quality of life [43] |
| Severe Vasospastic Angina (VSA) | Higher dosages of CCBs (e.g., diltiazem up to 960 mg daily) or combination of non-dihydropyridine and dihydropyridine CCBs | Sublingual nitroglycerin spray may alleviate acute angina pectoris episodes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McChord, J.; Ong, P. Bridging the Gender Gap in Cardiovascular Medicine: Addressing Drug Intolerances and Personalized Care for Women with Angina/Ischemia with Non-Obstructive Coronary Artery Disease. J. Cardiovasc. Dev. Dis. 2024, 11, 381. https://doi.org/10.3390/jcdd11120381
McChord J, Ong P. Bridging the Gender Gap in Cardiovascular Medicine: Addressing Drug Intolerances and Personalized Care for Women with Angina/Ischemia with Non-Obstructive Coronary Artery Disease. Journal of Cardiovascular Development and Disease. 2024; 11(12):381. https://doi.org/10.3390/jcdd11120381
Chicago/Turabian StyleMcChord, Johanna, and Peter Ong. 2024. "Bridging the Gender Gap in Cardiovascular Medicine: Addressing Drug Intolerances and Personalized Care for Women with Angina/Ischemia with Non-Obstructive Coronary Artery Disease" Journal of Cardiovascular Development and Disease 11, no. 12: 381. https://doi.org/10.3390/jcdd11120381
APA StyleMcChord, J., & Ong, P. (2024). Bridging the Gender Gap in Cardiovascular Medicine: Addressing Drug Intolerances and Personalized Care for Women with Angina/Ischemia with Non-Obstructive Coronary Artery Disease. Journal of Cardiovascular Development and Disease, 11(12), 381. https://doi.org/10.3390/jcdd11120381






