The David Versus the Bentall Procedure for Acute Type A Aortic Dissection
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Population
2.2. Study Outcomes
2.3. Statistical Analysis
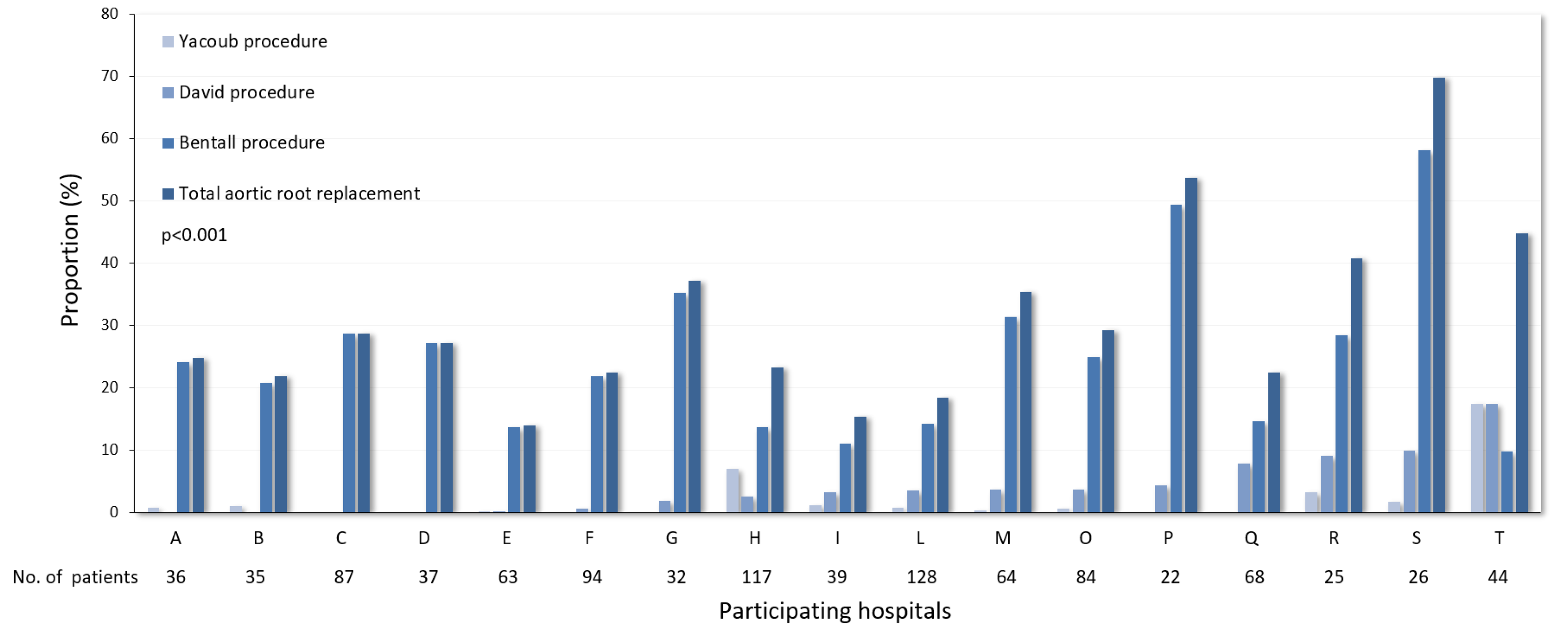
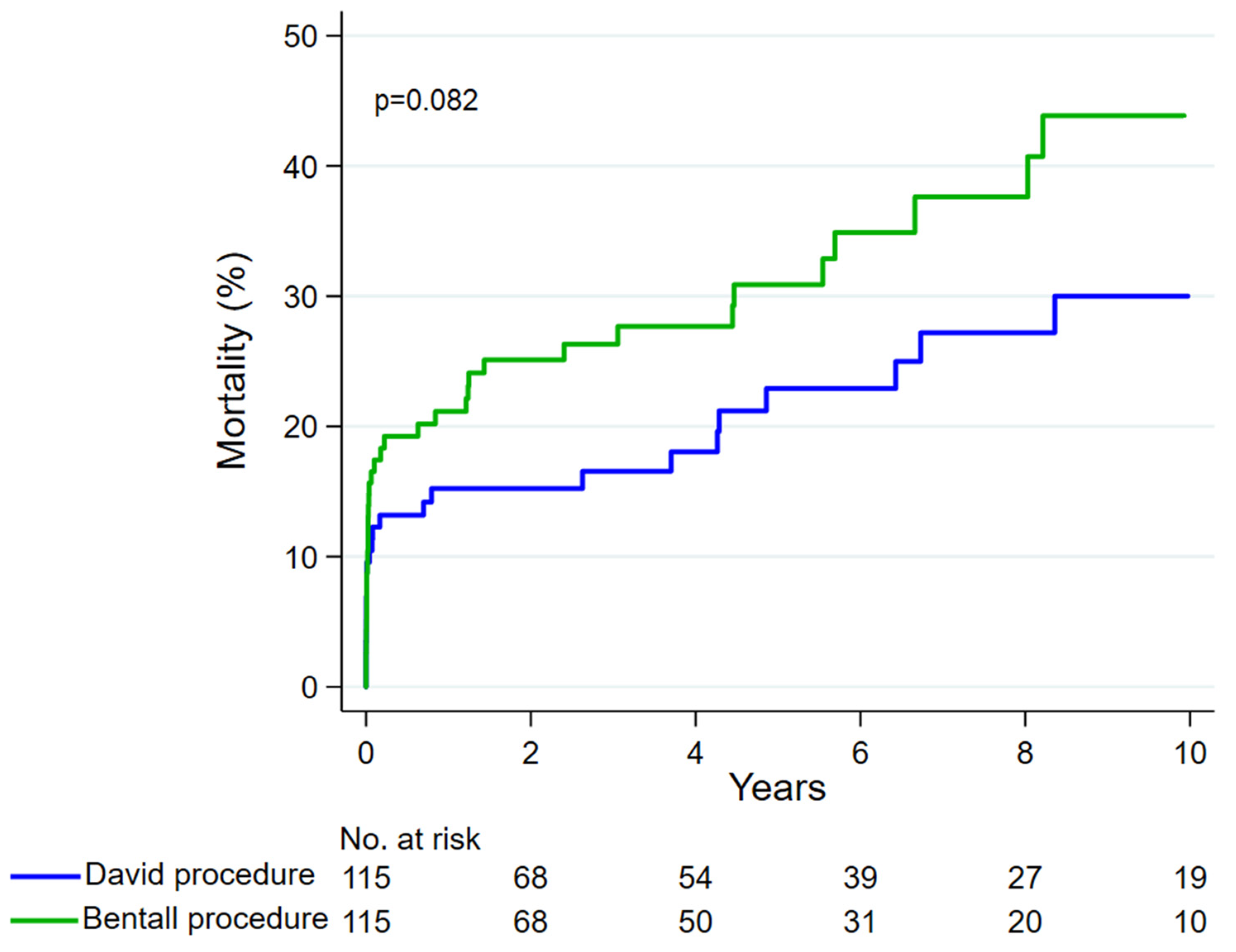
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Elsayed, R.S.; Cohen, R.G.; Fleischman, F.; Bowdish, M.E. Acute type A aortic dissection. Cardiol. Clin. 2017, 35, 331–345. [Google Scholar] [CrossRef] [PubMed]
- Isselbacher, E.M.; Preventza, O.; Hamilton Black Iii, J.; Augoustides, J.G.; Beck, A.W.; Bolen, M.A.; Braverman, A.C.; Bray, B.E.; Brown-Zimmerman, M.M.; Chen, E.P.; et al. 2022 ACC/AHA Guideline for the diagnosis and management of aortic disease: A report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2022, 80, e223–e393. [Google Scholar] [CrossRef] [PubMed]
- Arabkhani, B.; Verhoef, J.; Tomšič, A.; van Brakel, T.J.; Hjortnaes, J.; Klautz, R.J.M. The aortic root in acute type A dissection: Repair or replace? Ann. Thorac. Surg. 2023, 115, 1396–1402. [Google Scholar] [CrossRef] [PubMed]
- Khachatryan, Z.; Herajärvi, J.; Leontyev, S.; Borger, M.A. Valve-sparing aortic root replacement can be done safely and effectively in acute type A aortic dissection. J. Thorac. Cardiovasc. Surg. 2022, 164, 814–819. [Google Scholar] [CrossRef] [PubMed]
- Khachatryan, Z.; Leontyev, S.; Magomedov, K.; Haunschild, J.; Holzhey, D.M.; Misfeld, M.; Etz, C.D.; Borger, M.A. Management of aortic root in type A dissection: Bentall approach. J. Card. Surg. 2021, 36, 1779–1785. [Google Scholar] [CrossRef] [PubMed]
- Biancari, F.; Mariscalco, G.; Yusuff, H.; Tsang, G.; Luthra, S.; Onorati, F.; Francica, A.; Rossetti, C.; Perrotti, A.; Chocron, S.; et al. European registry of type A aortic dissection (ERTAAD)—Rationale, design and definition criteria. J. Cardiothorac. Surg. 2021, 16, 171. [Google Scholar] [CrossRef] [PubMed]
- Halstead, J.C.; Spielvogel, D.; Meier, D.M.; Rinke, S.; Bodian, C.; Malekan, R.; Arisanergin, M.; Griepp, R. Composite aortic root replacement in acute type A dissection: Time to rethink the indications? Eur. J. Cardiothorac. Surg. 2005, 27, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Leshnower, B.G.; Myung, R.J.; McPherson, L.; Chen, E.P. Midterm results of David V valve-sparing aortic root replacement in acute type A aortic dissection. Ann. Thorac. Surg. 2015, 99, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Rosenblum, J.M.; Leshnower, B.G.; Moon, R.C.; Lasanajak, Y.; Binongo, J.; McPherson, L.; Chen, E.P. Durability and safety of David V valve-sparing root replacement in acute type A aortic dissection. J. Thorac. Cardiovasc. Surg. 2019, 157, 14–23.e1. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Patel, H.J.; Sorek, C.; Hornsby, W.E.; Wu, X.; Ward, S.; Thomas, M.; Driscoll, A.; Waidley, V.A.; Norton, E.L.; et al. Sixteen-Year Experience of David and Bentall procedures in acute type A aortic dissection. Ann. Thorac. Surg. 2018, 105, 779–784. [Google Scholar] [CrossRef] [PubMed]
- Mosbahi, S.; Stak, D.; Gravestock, I.; Burgstaller, J.M.; Steurer, J.; Eckstein, F.; Ferrari, E.; A Berdajs, D. A systemic review and meta-analysis: Bentall versus David procedure in acute type A aortic dissection. Eur. J. Cardiothorac. Surg. 2019, 55, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Chikwe, J.; Cavallaro, P.; Itagaki, S.; Seigerman, M.; Diluozzo, G.; Adams, D.H. National outcomes in acute aortic dissection: Influence of surgeon and institutional volume on operative mortality. Ann. Thorac. Surg. 2013, 95, 1563–1569. [Google Scholar] [CrossRef] [PubMed]
- Levy, G.; DeAnda, A., Jr. Valve-sparing root replacement in type A dissection: Age and experience matter. J. Thorac. Cardiovasc. Surg. 2019, 157, 24–25. [Google Scholar] [CrossRef] [PubMed]

| Unmatched Cohorts | Propensity Score-Matched Cohorts | |||||
|---|---|---|---|---|---|---|
| Baseline and Operative Variables | David Procedure N = 139 | Bentall Procedure N = 862 | Standardized Differences | David Procedure N = 115 | Bentall Procedure N = 115 | Standardized Differences |
| Baseline variables | ||||||
| Age, years | 54.8 (12.7) | 58.8 (13.4) | −0.31 | 55.62 (12.7) | 55 (14.6) | 0.04 |
| Females | 23 (16.5) | 182 (21.1) | 0.12 | 20 (17.4) | 19 (16.5) | 0.02 |
| eGFR, mL/min 1.73 m2 | 75 (26) | 73 (23) | 0.10 | 73 (26) | 76 (25) | −0.12 |
| Bicuspid aortic valve | 5 (3.6) | 93 (10.8) | 0.28 | 5 (4.3) | 6 (5.2) | 0.04 |
| Genetic syndrome | 13 (9.4) | 42 (4.9) | 0.17 | 6 (5.2) | 9 (7.8) | 0.10 |
| Prior cardiac surgery | 3 (2.2) | 24 (2.8) | 0.04 | 3 (2.6) | 2 (2.7) | 0.06 |
| Iatrogenic dissection | 1 (0.7) | 12 (1.4) | 0.06 | 0 (0) | 0 (0) | 0.0 |
| Diabetes | 3 (2.2) | 44 (5.1) | 0.15 | 3 (2.6) | 2 (1.7) | 0.6 |
| Prior stroke | 3 (2.2) | 32 (3.7) | 0.09 | 3 (2.6) | 1 (0.9) | 0.13 |
| Pulmonary disease | 7 (5) | 72 (8.4) | 0.13 | 6 (5.2) | 6 (5.2) | 0.0 |
| Extracardiac arteriopathy | 2 (1.4) | 31 (3.6) | 0.14 | 2 (1.7) | 1 (0.9) | 0.08 |
| Preoperative malperfusion | ||||||
| Cerebral malperfusion | 25 (18) | 170 (19.7) | 0.04 | 21 (18.3) | 20 (17.4) | 0.02 |
| Spinal malperfusion | 2 (1.4) | 15 (1.7) | 0.02 | 2 (1.7) | 1 (0.9) | 0.08 |
| Renal malperfusion | 9 (6.5) | 63 (7.3) | 0.03 | 7 (6.1) | 5 (4.3) | 0.08 |
| Mesenteric malperfusion | 5 (3.6) | 28 (3.2) | 0.02 | 4 (3.5) | 4 (3.5) | 0.0 |
| Peripheral malperfusion | 16 (11.5) | 129 (15) | 0.10 | 12 (10.4) | 13 (11.3) | 0.03 |
| Preoperative cardiac massage | 4 (2.9) | 43 (5) | 0.10 | 4 (3.5) | 5 (4.3) | 0.04 |
| Invasive mechanical ventilation | 2 (1.4) | 81 (9.4) | 0.35 | 2 (1.7) | 1 (0.9) | 0.08 |
| Moderate-to-severe aortic valve insufficiency | 72 (51.8) | 626 (73.1) | 0.45 | 67 (58.3) | 58 (50.8) | 0.16 |
| Operative variables | ||||||
| Salvage procedure | 4 (2.9) | 43 (5) | 0.10 | 4 (3.5) | 5 (4.3) | 0.04 |
| Coronary artery bypass grafting | 11 (7.9) | 155 (18) | 0.30 | 9 (7.8) | 10 (8.7) | 0.03 |
| Partial/total aortic arch replacement | 37 (26.6) | 153 (17.7) | 0.22 | 28 (24.3) | 33 (28.7) | 0.10 |
| Aortic cross-clamping time, min | 170 (65) | 168 (62) | 0.02 | 170 (65) | 173 (77) | −0.05 |
| Cardiopulmonary bypass time, min | 256 (94) | 272 (100) | −0.17 | 260 (95) | 278 (100) | −0.18 |
| Unmatched Cohorts | Propensity Score-Matched Cohorts | |||||
|---|---|---|---|---|---|---|
| Postoperative Outcomes | David Procedure N = 139 | Bentall Procedure N = 862 | p-Values | David Procedure N = 115 | Bentall Procedure N = 115 | p-Values |
| Early outcomes | ||||||
| Hospital death | 16 (11.5) | 170 (19.7) | 0.021 | 13 (11.3) | 18 (15.7) | 0.334 |
| Any stroke or global brain ischemia | 18 (12.9) | 154 (17.9) | 0.154 | 14 (12.2) | 18 (15.7) | 0.446 |
| Any stroke | 16 (11.5) | 127 (14.7) | 0.314 | 13 (11.3) | 17 (14.8) | 0.434 |
| Global brain ischemia | 4 (2.9) | 39 (4.5) | 0.5 | 3 (2.6) | 3 (2.6) | 1 |
| Paraparesis or paraplegia | 3 (2.2) | 45 (5.2) | 0.136 | 2 (1.7) | 2 (1.7) | 1 |
| Tetraplegia or tetraparesis | 0 | 0 | - | 0 | 0 | - |
| Mesenteric ischemia | 5 (3.6) | 32 (3.7) | 1 | 3 (2.6) | 2 (1.7) | 1 |
| Sepsis | 13 (9.4) | 120 (13.9) | 0.141 | 9 (7.8) | 6 (5.2) | 0.423 |
| Dialysis | 9 (6.5) | 114 (13.2) | 0.024 | 8 (7.0) | 20 (17.4) | 0.016 |
| Reoperation for intrathoracic bleeding | 22 (15.8) | 153 (17.7) | 0.580 | 19 (16.5) | 13 (11.3) | 0.253 |
| Deep sternal wound infection/mediastinitis | 0 (0) | 28 (3.2) | 0.024 | 0 (0) | 2 (1.7) | 0.498 |
| Heart failure | 15 (10.8) | 153 (17.7) | 0.042 | 10 (8.7) | 16 (13.9) | 0.212 |
| Mechanical circulatory support | 4 (2.9) | 47 (5.5) | 0.296 | 4 (3.5) | 8 (7) | 0.375 |
| VA-ECMO | 2 (1.4) | 40 (4.6) | 0.107 | 2 (1.7) | 7 (6.1) | 0.171 |
| Surgery for intestinal complications | 0 (0) | 4 (0.5) | 1 | 0 | 0 | - |
| 10-year outcomes | ||||||
| Mortality | 29 (30.1) | 295 (45.6) | 0.004 | 25 (30.0) | 37 (43.9) | 0.082 |
| Proximal aortic reoperation | 4 (3.9) | 25 (4.1) | 0.954 | 2 (2.8) | 2 (1.8) | 0.994 |
| No. | Primary Procedure | No. of Reoperations | Types of Proximal Aortic Reoperation |
|---|---|---|---|
| 1 | Bentall procedure | 4 | Local repair twice, replacement of the ascending aortic prosthesis, Bentall procedure |
| 2 | Bentall procedure | 2 | Bentall procedure twice |
| 3 | Bentall procedure | 1 | Replacement of the ascending aortic prosthesis |
| 4 | Bentall procedure | 1 | Local repair |
| 5 | Bentall procedure | 1 | Local repair |
| 6 | Bentall procedure | 1 | Local repair |
| 7 | Bentall procedure | 1 | Local repair |
| 8 | Bentall procedure | 1 | Local repair |
| 9 | Bentall procedure | 1 | Local repair |
| 10 | Bentall procedure | 1 | Local repair |
| 11 | Bentall procedure | 1 | Local repair |
| 12 | Bentall procedure | 1 | Bentall procedure |
| 13 | Bentall procedure | 1 | Bentall procedure |
| 14 | Bentall procedure | 1 | Bentall procedure |
| 15 | Bentall procedure | 1 | Bentall procedure |
| 16 | Bentall procedure | 1 | Bentall procedure |
| 17 | Bentall procedure | 1 | Bentall procedure |
| 18 | Bentall procedure | 1 | Bentall procedure |
| 19 | Bentall procedure | 1 | Bentall procedure |
| 20 | Bentall procedure | 1 | Bentall procedure |
| 21 | Bentall procedure | 1 | Bentall procedure |
| 22 | Bentall procedure | 1 | Bentall procedure |
| 23 | Bentall procedure | 1 | Bentall procedure |
| 24 | Bentall procedure | 1 | Bentall procedure |
| 25 | Bentall procedure | 1 | Surgical aortic valve replacement |
| 26 | Bentall procedure | 1 | Surgical aortic valve replacement |
| 27 | David procedure | 2 | Bentall procedure, transcatheter aortic valve replacement |
| 28 | David procedure | 1 | Bentall procedure |
| 29 | David procedure | 1 | Surgical aortic valve replacement |
| 30 | David procedure | 1 | Aortic valve repair |
| 31 | David procedure | 1 | Local repair |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biancari, F.; Mastroiacovo, G.; Rinaldi, M.; Ferrante, L.; Mäkikallio, T.; Juvonen, T.; Mariscalco, G.; El-Dean, Z.; Pettinari, M.; Rodriguez Lega, J.; et al. The David Versus the Bentall Procedure for Acute Type A Aortic Dissection. J. Cardiovasc. Dev. Dis. 2024, 11, 370. https://doi.org/10.3390/jcdd11110370
Biancari F, Mastroiacovo G, Rinaldi M, Ferrante L, Mäkikallio T, Juvonen T, Mariscalco G, El-Dean Z, Pettinari M, Rodriguez Lega J, et al. The David Versus the Bentall Procedure for Acute Type A Aortic Dissection. Journal of Cardiovascular Development and Disease. 2024; 11(11):370. https://doi.org/10.3390/jcdd11110370
Chicago/Turabian StyleBiancari, Fausto, Giorgio Mastroiacovo, Mauro Rinaldi, Luisa Ferrante, Timo Mäkikallio, Tatu Juvonen, Giovanni Mariscalco, Zein El-Dean, Matteo Pettinari, Javier Rodriguez Lega, and et al. 2024. "The David Versus the Bentall Procedure for Acute Type A Aortic Dissection" Journal of Cardiovascular Development and Disease 11, no. 11: 370. https://doi.org/10.3390/jcdd11110370
APA StyleBiancari, F., Mastroiacovo, G., Rinaldi, M., Ferrante, L., Mäkikallio, T., Juvonen, T., Mariscalco, G., El-Dean, Z., Pettinari, M., Rodriguez Lega, J., Pinto, A. G., Perrotti, A., Onorati, F., Wisniewski, K., Demal, T., Kacer, P., Rocek, J., Di Perna, D., Vendramin, I., ... Peterss, S. (2024). The David Versus the Bentall Procedure for Acute Type A Aortic Dissection. Journal of Cardiovascular Development and Disease, 11(11), 370. https://doi.org/10.3390/jcdd11110370











