The Effect of Daylight-Saving Time on Percutaneous Coronary Intervention Outcomes in Acute Coronary Syndrome Patients—Data from the Polish National Registry of Percutaneous Coronary Interventions (ORPKI) in the Years 2014–2022
Abstract
:1. Introduction
2. Patients and Methods
2.1. Study Cohort
2.2. Statistical Analysis
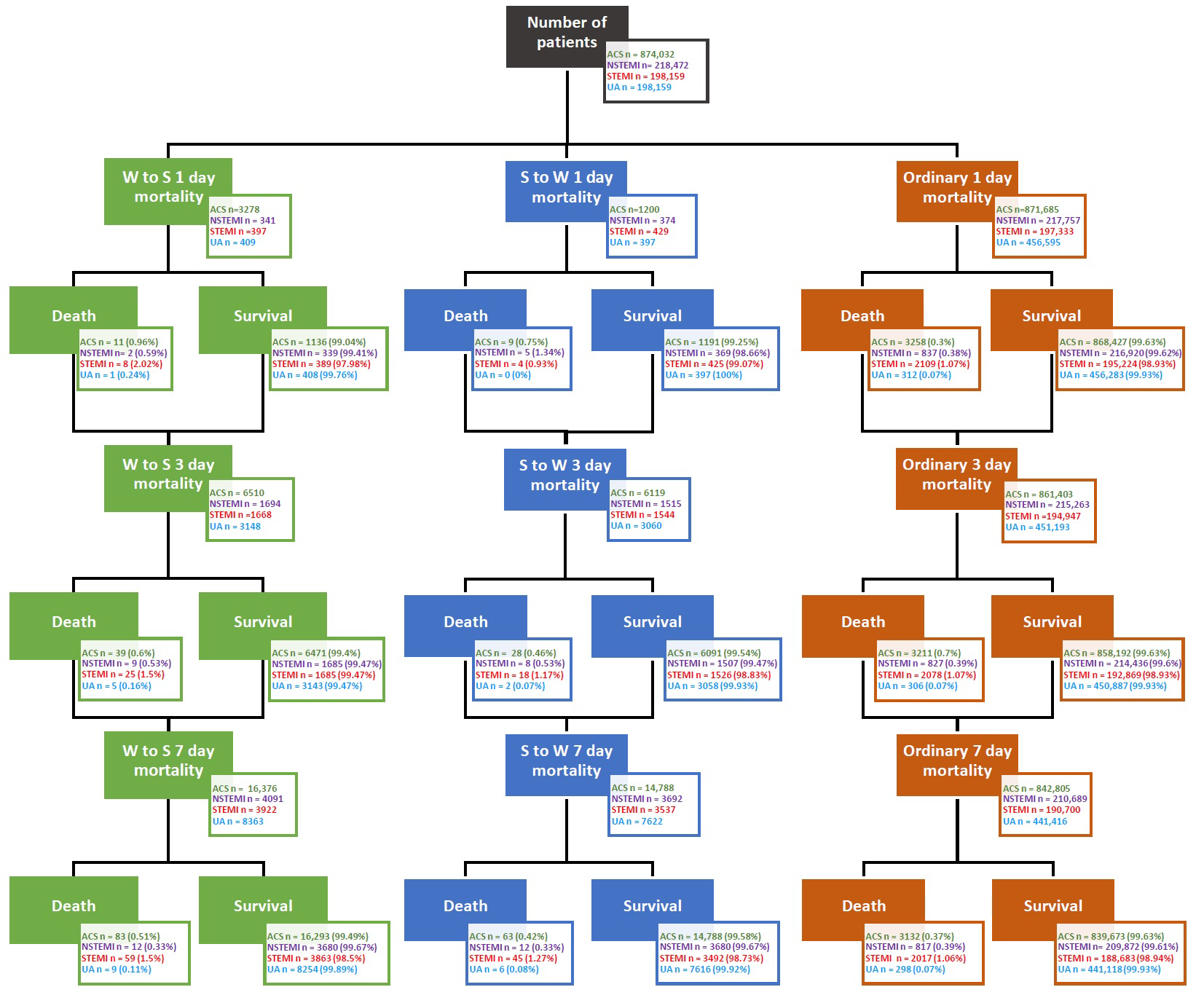
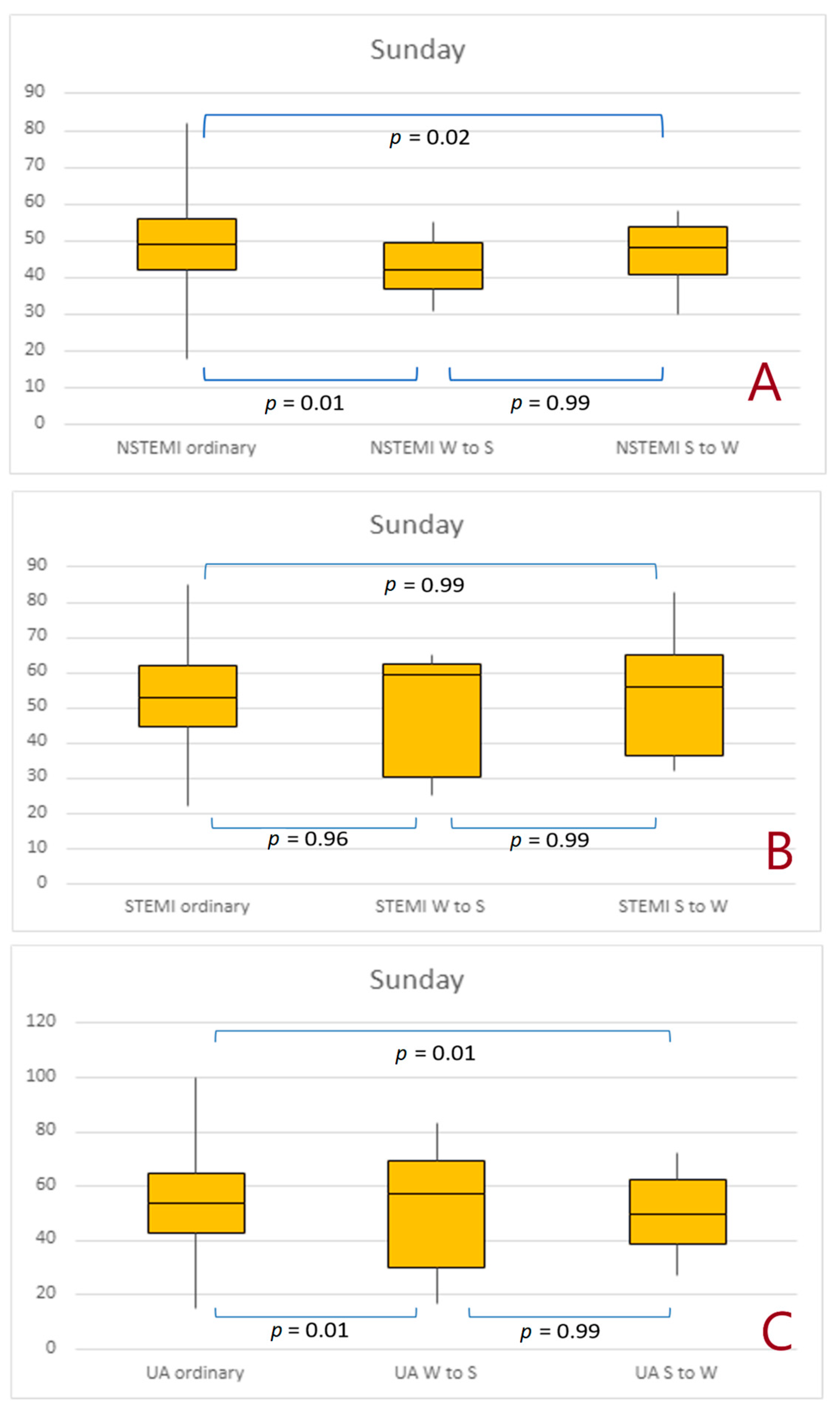
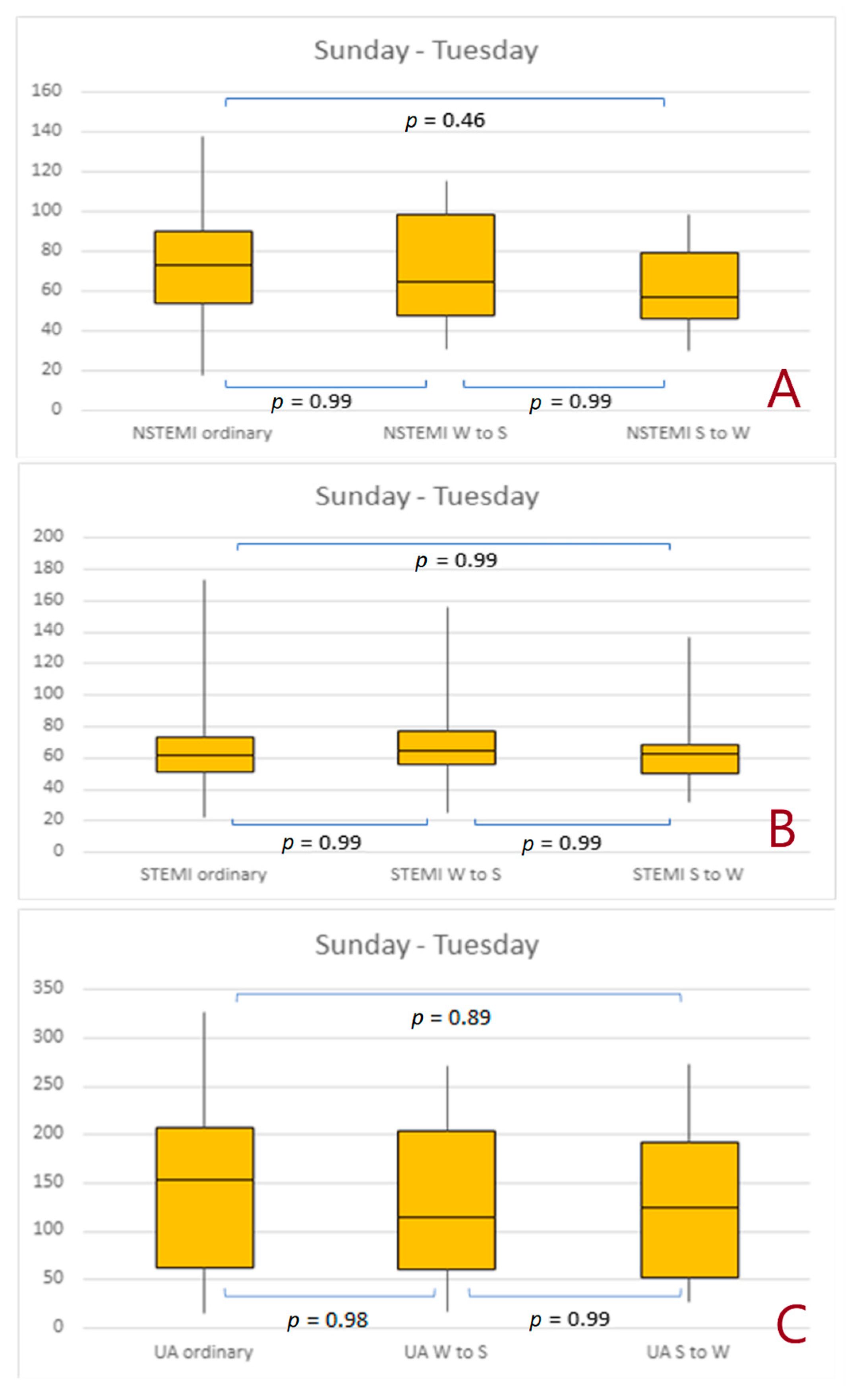
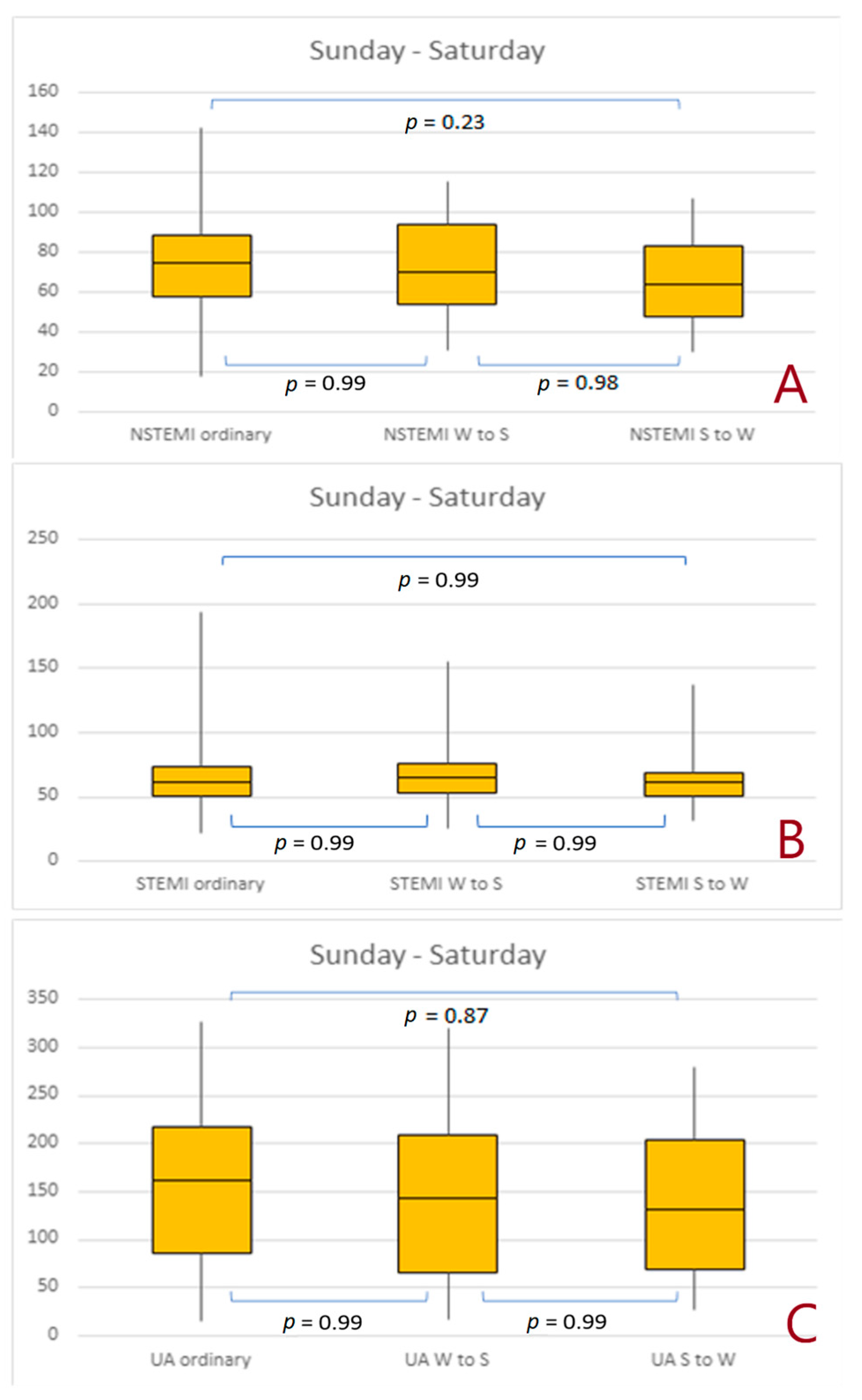
3. Results
4. Discussion
5. Conclusions
- The analysis of the differences in the number of ACS from the first day to 7 days revealed that the number of ACS was lower for both changes over time; moreover, the autumn time change statistically significantly reduced the number of treatments, also in the analysis from the first day to 3 days.
- In the analysis of the influence of both time changes on the occurrence of STEMI, no statistically significant seasonal differences were found.
- The autumn time change is associated with a less frequent occurrence of NSTEMI within 7 days.
- A change in time may contribute to the increase in periprocedural mortality in ACS (STEMI and NSTEMI).
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Manfredini, R.; Fabbian, F.; Cappadona, R.; Modesti, P.A. Daylight-saving time, circadian rhythms, and cardiovascular health. Intern. Emerg. Med. 2018, 13, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Hemmer, A.; Mareschal, J.; Dibner, C.; Pralong, J.A.; Dorribo, V.; Perrig, S.; Genton, L.; Pichard, C.; Collet, T.H. Effects of Shift Work on Cardio-Metabolic Diseases and Eating Patterns. Nutrients 2021, 13, 4178. [Google Scholar] [CrossRef] [PubMed]
- Lamia, K.A. Ticking time bombs: Connections between circadian clocks and cancer. F1000Res 2017, 6, 1910. [Google Scholar] [CrossRef] [PubMed]
- Suárez-Barrientos, A.; López-Romero, P.; Vivas, D.; Castro-Ferreira, F.; Núñez-Gil, I.; Franco, E.; Ruiz-Mateos, B.; García-Rubira, J.C.; Fernández-Ortiz, A.; Macaya, C.; et al. Circadian variations of infarct size in acute myocardial infarction. Heart 2011, 97, 970–976. [Google Scholar] [CrossRef] [PubMed]
- Torquati, L.; Mielke, G.I.; Brown, W.J.; Kolbe-Alexander, T. Shift work and the risk of cardiovascular disease. A systematic review and meta-analysis including dose-response relationship. Scand. J. Work. Environ. Health 2018, 44, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, A.; Seth, M.; Gurm, H.S. Daylight savings time and myocardial infarction. Open Heart 2014, 1, e000019. [Google Scholar] [CrossRef] [PubMed]
- Derks, L.; Houterman, S.; Geuzebroek, G.S.C.; van der Harst, P.; Smits, P.C.; PCI Registration Committee of the Netherlands Heart Registration. Daylight-saving time does not seem to be associated with number of percutaneous coronary interventions for acute myocardial infarction in the Netherlands. Neth. Heart J. 2021, 29, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Sielski, J.; Kaziród-Wolski, K.; Jurys, K.; Wałek, P.; Siudak, Z. The Effect of Periprocedural Clinical Factors Related to the Course of STEMI in Men and Women Based on the National Registry of Invasive Cardiology Procedures (ORPKI) between 2014 and 2019. J. Clin. Med. 2021, 10, 5716. [Google Scholar] [CrossRef]
- Sielski, J.; Kaziród-Wolski, K.; Siudak, Z. Risk of perioperative death and sudden cardiac arrest: A study of 113,456 cases from the National Registry of Invasive Cardiology Procedures (ORPKI) for estimation of the perioperative prognosis. Kardiol. Pol. 2021, 79, 1328–1334. [Google Scholar] [CrossRef]
- Čulić, V. Daylight saving time transitions and acute myocardial infarction. Chronobiol. Int. 2013, 30, 662–668. [Google Scholar] [CrossRef]
- Sipilä, J.O.; Rautava, P.; Kytö, V. Association of daylight-saving time transitions with incidence and in-hospital mortality of myocardial infarction in Finland. Ann. Med. 2016, 48, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, R.; Fabbian, F.; De Giorgi, A.; Zucchi, B.; Cappadona, R.; Signani, F.; Katsiki, N.; Mikhailidis, D.P. Daylight-saving time and myocardial infarction: Should we be worried? A review of the evidence. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 750–755. [Google Scholar] [PubMed]
- Culić, V.; Eterović, D.; Mirić, D. Meta-analysis of possible external triggers of acute myocardial infarction. Int. J. Cardiol. 2005, 99, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Medina, D.; Ebben, M.; Milrad, S.; Atkinson, B.; Krieger, A.C. Adverse Effects of Daylight-Saving Time on Adolescents’ Sleep and Vigilance. J. Clin. Sleep. Med. 2015, 11, 879–884. [Google Scholar] [CrossRef] [PubMed]
- Lusardi, P.; Zoppi, A.; Preti, P.; Pesce, R.M.; Piazza, E.; Fogari, R. Effects of insufficient sleep on blood pressure in hypertensive patients: A 24-h study. Am. J. Hypertens. 1999, 12, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.; Lange, T.; Hallqvist, J.; Jennum, P.; Rod, N.H. Sleep impairment and prognosis of acute myocardial infarction: A prospective cohort study. Sleep 2014, 37, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Jiddou, M.R.; Pica, M.; Boura, J.; Qu, L.; Franklin, B.A. Incidence of myocardial infarction with shifts to and from daylight savings time. Am. J. Cardiol. 2013, 111, 631–635. [Google Scholar] [CrossRef] [PubMed]
- Meier-Ewert, H.K.; Ridker, P.M.; Rifai, N.; Regan, M.M.; Price, N.J.; Dinges, D.F.; Mullington, J.M. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J. Am. Coll. Cardiol. 2004, 43, 678–683. [Google Scholar] [CrossRef]
- Crea, F.; Libby, P. Acute coronary syndromes: The way forward from mechanisms to precision treatment. Circulation 2017, 136, 1155–1166. [Google Scholar] [CrossRef]
- Čulić, V.; Kantermann, T. Acute Myocardial Infarction and Daylight Saving Time Transitions: Is There a Risk? Clocks Sleep 2021, 3, 547–557. [Google Scholar] [CrossRef]
- Valdez, P.; Ramirez, C.; Garcia, A. Adjustment of the sleep-wake cycle to small (1–2 h) changes in schedule. Biol. Rhythm. Res. 2003, 34, 145–155. [Google Scholar] [CrossRef]
- Harrison, Y. The impact of daylight saving time on sleep and related behaviours. Sleep. Med. Rev. 2013, 17, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.C.; Qi, X.; Hu, Y.H.; Zheng, W.J.; Wang, Q.Q.; Yao, H.Y. Overview of multivariate regression model analysis and application. Zhonghua Yu Fang Yi Xue Za Zhi 2019, 53, 334–336. [Google Scholar] [CrossRef] [PubMed]

| Sunday (1 Day) | Sunday–Tuesday (3 Days) | Sunday–Saturday (7 Days) | ||||
|---|---|---|---|---|---|---|
| Rate Ratio (95% CI) | p-Value | Rate Ratio (95% CI) | p-Value | Rate Ratio (95% CI) | p-Value | |
| ACS | ||||||
| Winter to Summer | 0.91 (0.72–1.14) | 0.45 | 0.95 (0.86–1.05) | 0.30 | 0.98 (0.92–1.04) | 0.45 |
| Summer to Winter | 0.96 (0.75–1.20) | 0.73 | 0.89 (0.81–0.98) | 0.02 | 0.88 (0.83–0.93) | <0.001 |
| Any | 0.94 (0.74–1.18) | 0.60 | 0.92 (0.83–1.01) | 0.09 | 0.93 (0.87–0.99) | 0.02 |
| STEMI | ||||||
| Winter to Summer | 0.94 (0.63–1.42) | 0.84 | 1.01 (0.83–1.24) | 0.92 | 1.03 (0.91–1.17) | 0.65 |
| Summer to Winter | 1.02 (0.68–1.52) | 1 | 0.94 (0.77–1.15) | 0.55 | 0.93 (0.81–1.06) | 0.28 |
| Any | 0.98 (0.66–1.47) | 0.98 | 0.98 (0.80–1.19) | 0.84 | 0.98 (0.86–1.11) | 0.77 |
| NSTEMI | ||||||
| Winter to Summer | 0.88 (0.57–1.35) | 0.60 | 0.97 (0.80–1.17) | 0.77 | 0.97 (0.86–1.1) | 0.71 |
| Summer to Winter | 0.96 (0.63–1.46) | 0.91 | 0.86 (0.71–1.05) | 1.51 | 0.88 (0.77–1.0) | 0.048 |
| Any | 0.92 (0.60–1.41) | 0.76 | 0.92 (0.75–1.12) | 0.41 | 0.93 (0.82–1.05) | 0.23 |
| UA | ||||||
| Winter to Summer | 0.94 (0.63–1.41) | 0.85 | 0.91 (0.79–1.04) | 0.20 | 0.95 (0.87–1.04) | 0.26 |
| Summer to Winter | 0.93 (0.62–1.39) | 0.93 | 0.89 (0.77–1.02) | 0.09 | 0.87 (0.79–0.95) | 0.001 |
| Any | 0.93 (0.62–1.39) | 0.77 | 0.90 (0.78–1.03) | 0.12 | 0.91 (0.83–0.99) | 0.03 |
| Sunday (1 Day) | Sunday–Tuesday (3 Days) | Sunday–Saturday (7 Days) | ||||
|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | |
| ACS | ||||||
| Winter to Summer | 2.58 (1.42–1.67) | 0.002 | 1.61 (1.17–2.21) | 0.003 | 1.36 (1.1–1.7) | 0.006 |
| Summer to Winter | 2.01 (1.04–3.88) | 0.037 | 1.22 (0.84–1.78) | 0.29 | 1.13 (0.88–1.46) | 0.32 |
| Any | 2.29 (1.47–3.56) | 0.0002 | 1.43 (1.12–1.82) | 0.004 | 1.26 (1.07–1.49) | 0.007 |
| STEMI | ||||||
| Winter to Summer | 1.9 (0.94–3.84) | 0.07 | 1.41 (0.95–2.1) | 0.09 | 1.42 (1.1–1.85) | 0.008 |
| Summer to Winter | 0.87 (3.2–2.33) | 0.78 | 1.09 (0.68–1.74) | 0.71 | 1.2 (0.89–1.61) | 0.24 |
| Any | 1.36 (0.77–2.42) | 0.29 | 1.26 (0.93–1.7) | 0.14 | 1.32 (1.08–1.61) | 0.006 |
| NSTEMI | ||||||
| Winter to Summer | 1.52 (0.38–6.12) | 0.55 | 1.38 (0.72–2.67) | 0.34 | 0.95 (0.57–1.58) | 0.84 |
| Summer to Winter | 3.51 (1.45–8.5) | 0.005 | 1.37 (0.68–2.76) | 0.37 | 0.84 (0.47–1.48) | 0.55 |
| Any | 2.56 (1.21–5.41) | 0.01 | 1.38 (0.85–2.24) | 0.19 | 0.89 (0.61–1.31) | 0.57 |
| UA | ||||||
| Winter to Summer | 3.59 (0.5–25.61) | 0.2 | 2.34 (0.97–5.68) | 0.06 | 1.59 (0.82–3.09) | 0.17 |
| Summer to Winter | 0.0001 (0.0000–1.18 × 10137) | 0.96 | 0.95 (0.24–3.84) | 0.95 | 1.15 (0.51–2.59) | 0.73 |
| Any | 1.82 (0.25–12.95) | 0.55 | 1.66 (0.79–3.52) | 0.18 | 1.39 (0.83–2.34) | 0.21 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaziród-Wolski, K.; Piotrowska, A.; Sielski, J.; Zając, P.; Malinowski, K.P.; Zabojszcz, M.; Pytlak, K.; Wolska, M.; Kołodziej, A.; Mamas, M.A.; et al. The Effect of Daylight-Saving Time on Percutaneous Coronary Intervention Outcomes in Acute Coronary Syndrome Patients—Data from the Polish National Registry of Percutaneous Coronary Interventions (ORPKI) in the Years 2014–2022. J. Cardiovasc. Dev. Dis. 2023, 10, 375. https://doi.org/10.3390/jcdd10090375
Kaziród-Wolski K, Piotrowska A, Sielski J, Zając P, Malinowski KP, Zabojszcz M, Pytlak K, Wolska M, Kołodziej A, Mamas MA, et al. The Effect of Daylight-Saving Time on Percutaneous Coronary Intervention Outcomes in Acute Coronary Syndrome Patients—Data from the Polish National Registry of Percutaneous Coronary Interventions (ORPKI) in the Years 2014–2022. Journal of Cardiovascular Development and Disease. 2023; 10(9):375. https://doi.org/10.3390/jcdd10090375
Chicago/Turabian StyleKaziród-Wolski, Karol, Aleksandra Piotrowska, Janusz Sielski, Patrycja Zając, Krzysztof P. Malinowski, Michał Zabojszcz, Kamil Pytlak, Magdalena Wolska, Agnieszka Kołodziej, Mamas A. Mamas, and et al. 2023. "The Effect of Daylight-Saving Time on Percutaneous Coronary Intervention Outcomes in Acute Coronary Syndrome Patients—Data from the Polish National Registry of Percutaneous Coronary Interventions (ORPKI) in the Years 2014–2022" Journal of Cardiovascular Development and Disease 10, no. 9: 375. https://doi.org/10.3390/jcdd10090375
APA StyleKaziród-Wolski, K., Piotrowska, A., Sielski, J., Zając, P., Malinowski, K. P., Zabojszcz, M., Pytlak, K., Wolska, M., Kołodziej, A., Mamas, M. A., Mizera, P., & Siudak, Z. (2023). The Effect of Daylight-Saving Time on Percutaneous Coronary Intervention Outcomes in Acute Coronary Syndrome Patients—Data from the Polish National Registry of Percutaneous Coronary Interventions (ORPKI) in the Years 2014–2022. Journal of Cardiovascular Development and Disease, 10(9), 375. https://doi.org/10.3390/jcdd10090375






