Percutaneous Coronary Intervention Outcomes in Patients with Liver Cirrhosis: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
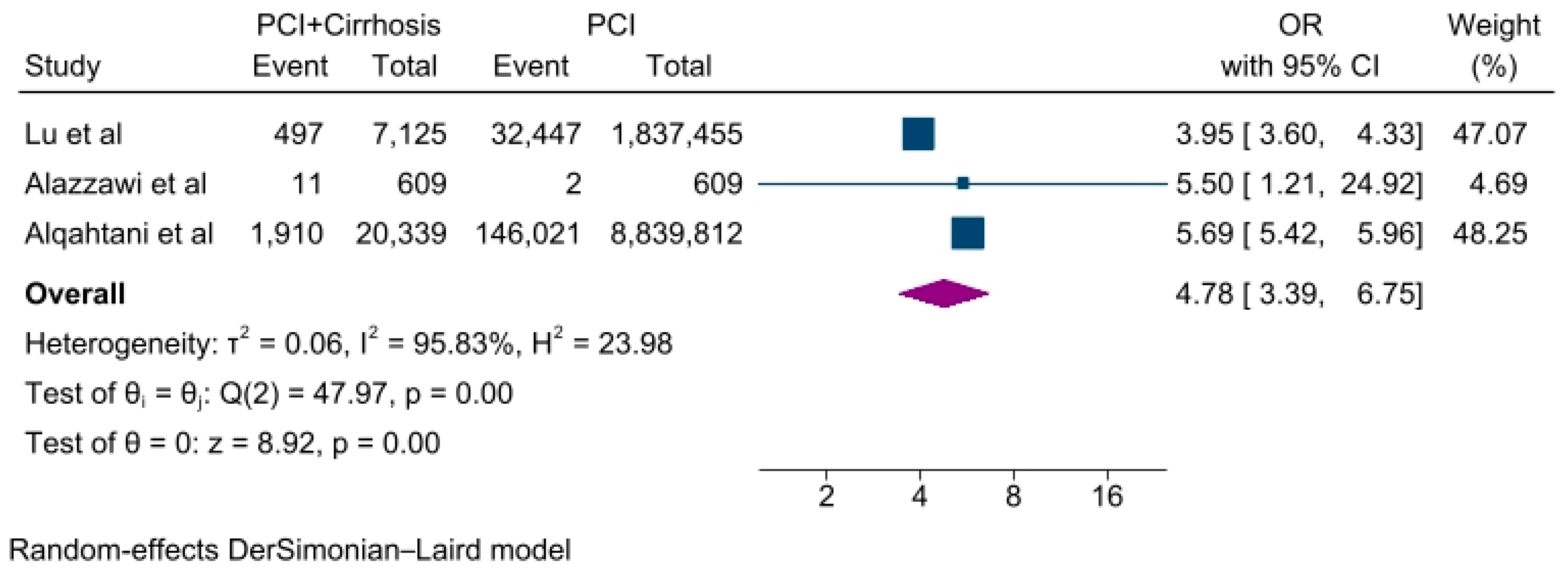
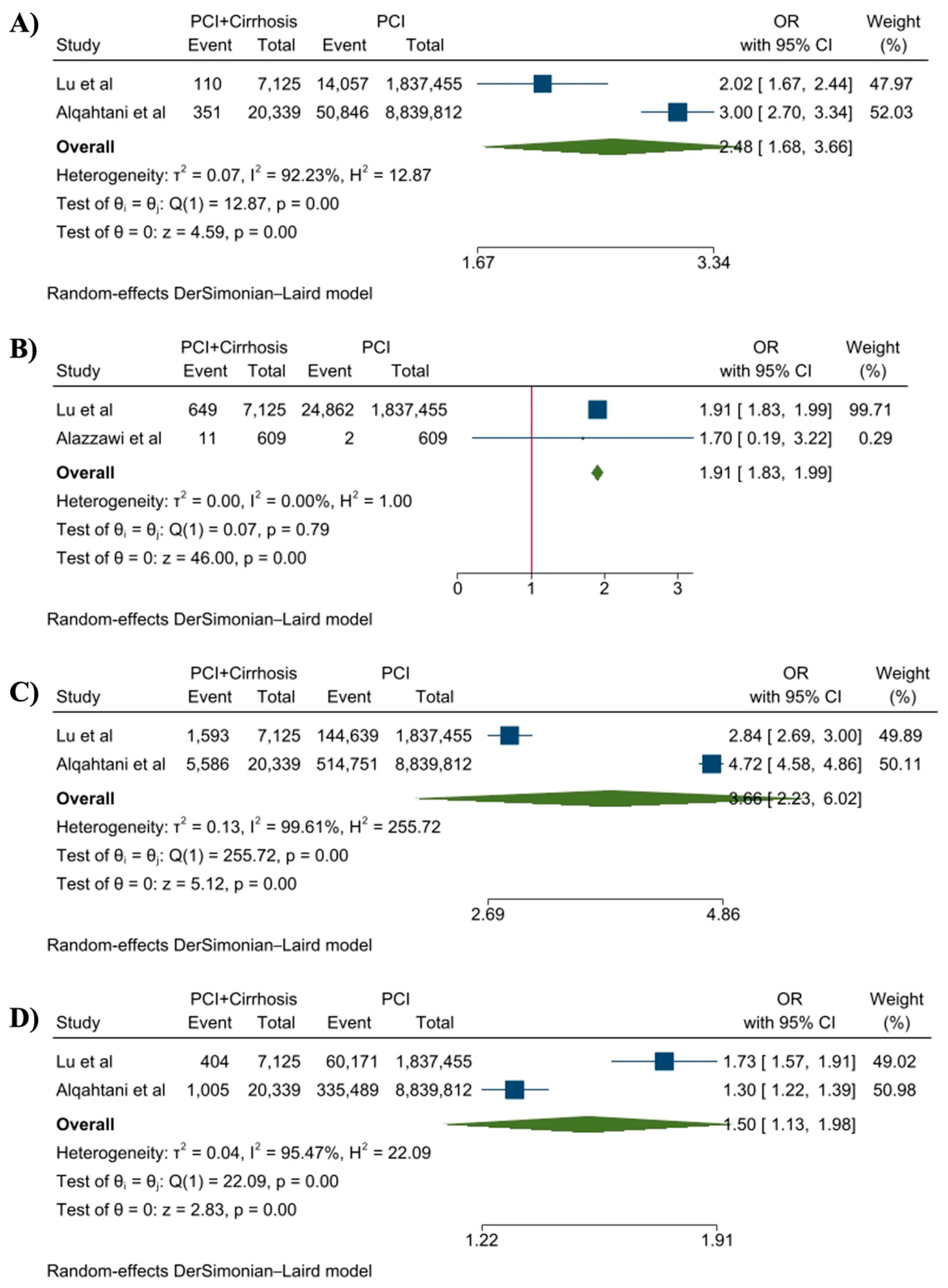
2. Materials and Methods
2.1. Outcomes of Interest
2.2. Search Strategy and Study Selection
- Patients with diagnosed cirrhosis;
- Studies with patients > 18 years;
- Two-arm studies comparing the PCI patients with cirrhosis and PCI patients without cirrhosis;
- Studies reporting at least one of the desired outcomes;
- Prospective and retrospective studies were eligible.
2.3. Data Extraction and Statistical Analysis
2.4. Quality Assessment
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Disclosure
Conflicts of Interest
References
- Murray, C.J.L.; Barber, R.M.; Foreman, K.J.; Ozgoren, A.A.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Abraham, J.P.; Abubakar, I.; Abu-Raddad, L.J.; et al. Global, Regional, and National Disability-Adjusted Life Years (DALYs) for 306 Diseases and Injuries and Healthy Life Expectancy (HALE) for 188 Countries, 1990–2013: Quantifying the Epidemiological Transition. Lancet 2015, 386, 2145–2191. [Google Scholar] [CrossRef] [PubMed]
- Masoudi, F.A.; Ponirakis, A.; de Lemos, J.A.; Jollis, J.G.; Kremers, M.; Messenger, J.C.; Moore, J.W.M.; Moussa, I.; Oetgen, W.J.; Varosy, P.D.; et al. Trends in U.S. Cardiovascular Care. J. Am. Coll. Cardiol. 2017, 69, 1427–1450. [Google Scholar] [CrossRef] [PubMed]
- Potts, J.; Kwok, C.S.; Ensor, J.; Rashid, M.; Kadam, U.; Kinnaird, T.; Curzen, N.; Pancholy, S.B.; Van der Windt, D.; Riley, R.D.; et al. Temporal Changes in Co-Morbidity Burden in Patients Having Percutaneous Coronary Intervention and Impact on Prognosis. Am. J. Cardiol. 2018, 122, 712–722. [Google Scholar] [CrossRef] [PubMed]
- Valle, J.A.; Kaltenbach, L.A.; Bradley, S.M.; Yeh, R.W.; Rao, S.V.; Gurm, H.S.; Armstrong, E.J.; Messenger, J.C.; Waldo, S.W. Variation in the Adoption of Transradial Access for ST-Segment Elevation Myocardial Infarction. JACC Cardiovasc. Interv. 2017, 10, 2242–2254. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Huang, J. The Growing Burden of Liver Cirrhosis: Implications for Preventive Measures. Hepatol. Int. 2018, 12, 201–203. [Google Scholar] [CrossRef]
- Kanwal, F.; Hoang, T.; Kramer, J.R.; Asch, S.M.; Goetz, M.B.; Zeringue, A.; Richardson, P.; El–Serag, H.B. Increasing Prevalence of HCC and Cirrhosis in Patients With Chronic Hepatitis C Virus Infection. Gastroenterology 2011, 140, 1182–1188.e1. [Google Scholar] [CrossRef]
- Udompap, P.; Mannalithara, A.; Heo, N.-Y.; Kim, D.; Kim, W.R. Increasing Prevalence of Cirrhosis among U.S. Adults Aware or Unaware of Their Chronic Hepatitis C Virus Infection. J. Hepatol. 2016, 64, 1027–1032. [Google Scholar] [CrossRef]
- An, J.; Shim, J.H.; Kim, S.-O.; Lee, D.; Kim, K.M.; Lim, Y.-S.; Lee, H.C.; Chung, Y.-H.; Lee, Y.S. Prevalence and Prediction of Coronary Artery Disease in Patients With Liver Cirrhosis: A Registry-Based Matched Case–Control Study. Circulation 2014, 130, 1353–1362. [Google Scholar] [CrossRef]
- Kadayifci, A.; Tan, V.; Ursell, P.C.; Merriman, R.B.; Bass, N.M. Clinical and Pathologic Risk Factors for Atherosclerosis in Cirrhosis: A Comparison between NASH-Related Cirrhosis and Cirrhosis Due to Other Aetiologies. J. Hepatol. 2008, 49, 595–599. [Google Scholar] [CrossRef]
- Baker, S.; Chambers, C.; McQuillan, P.; Janicki, P.; Kadry, Z.; Bowen, D.; Bezinover, D. Myocardial Perfusion Imaging Is an Effective Screening Test for Coronary Artery Disease in Liver Transplant Candidates. Clin. Transplant. 2015, 29, 319–326. [Google Scholar] [CrossRef]
- Charlton, M. Nonalcoholic Fatty Liver Disease: A Review of Current Understanding and Future Impact. Clin. Gastroenterol. Hepatol. 2004, 2, 1048–1058. [Google Scholar] [CrossRef]
- Shaheen, A.A.M.; Kaplan, G.G.; Hubbard, J.N.; Myers, R.P. Morbidity and Mortality Following Coronary Artery Bypass Graft Surgery in Patients with Cirrhosis: A Population-Based Study. Liver Int. 2009, 29, 1141–1151. [Google Scholar] [CrossRef]
- Suman, A.; Barnes, D.S.; Zein, N.N.; Levinthal, G.N.; Connor, J.T.; Carey, W.D. Predicting Outcome after Cardiac Surgery in Patients with Cirrhosis: A Comparison of Child-Pugh and MELD Scores. Clin. Gastroenterol. Hepatol. 2004, 2, 719–723. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, E.; Singh, V.; Damluji, A.; Shah, N.R.; Warsch, J.L.; Ghanta, R.; Martin, P.; Alfonso, C.E.; Martinez, C.A.; Moscucci, M.; et al. Safety of Transradial Cardiac Catheterization in Patients with End-Stage Liver Disease: Transradial Catheterization in ESLD. Catheter. Cardiovasc. Interv. 2014, 83, 360–366. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, V.; Ishak, A.; Peng Ang, S.; Babu Pokhrel, N.; Shama, N.; Lnu, K.; Susan Varghese, J.; Storozhenko, T.; Ee Chia, J.; Naz, S.; et al. Hypovitaminosis D and Cardiovascular Outcomes: A Systematic Review and Meta-Analysis. IJC Heart Vasc. 2022, 40, 101019. [Google Scholar] [CrossRef]
- Jaiswal, V.; Ang, S.P.; Yaqoob, S.; Ishak, A.; Chia, J.E.; Nasir, Y.M.; Anjum, Z.; Alraies, M.C.; Jaiswal, A.; Biswas, M. Cardioprotective Effects of Influenza Vaccination among Patients with Established Cardiovascular Disease or at High Cardiovascular Risk: A Systematic Review and Meta-Analysis. Eur. J. Prev. Cardiol. 2022, 29, 1881–1892. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. A Basic Introduction to Fixed-Effect and Random-Effects Models for Meta-Analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying Heterogeneity in a Meta-Analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 23 February 2022).
- Lu, D.Y.; Steitieh, D.; Feldman, D.N.; Cheung, J.W.; Wong, S.C.; Halazun, H.; Halazun, K.J.; Amin, N.; Wang, J.; Chae, J.; et al. Impact Of Cirrhosis On 90-Day Outcomes After Percutaneous Coronary Intervention (from A Nationwide Database). Am. J. Cardiol. 2020, 125, 1295–1304. [Google Scholar] [CrossRef] [PubMed]
- Alazzawi, Y.; Alabboodi, Y.; Fasullo, M.; Ridha, A.; Naguib, T. The Morbidity and Mortality Risks Following Percutaneous Coronary Interventions in Cirrhosis. J. Liver 2017, 6. [Google Scholar] [CrossRef]
- Alqahtani, F.; Balla, S.; AlHajji, M.; Chaudhary, F.; Albeiruti, R.; Kawsara, A.; Alkhouli, M. Temporal Trends in the Utilization and Outcomes of Percutaneous Coronary Interventions in Patients with Liver Cirrhosis. Catheter. Cardiovasc. Interv. 2020, 96, 802–810. [Google Scholar] [CrossRef] [PubMed]
- Kolte, D.; Khera, S.; Sharma, N.; Aronow, W.; Mujib, M.; Palaniswamy, C.; Jain, D.; Sule, S.; Frishman, W.; Ahmed, A.; et al. Outcomes of percutaneous coronary intervention in patients with cirrhosis. J. Am. Coll. Cardiol. 2014, 63, A1849. [Google Scholar] [CrossRef]
- Marui, A.; Kimura, T.; Tanaka, S.; Miwa, S.; Yamazaki, K.; Minakata, K.; Nakata, T.; Ikeda, T.; Furukawa, Y.; Kita, T.; et al. Coronary Revascularization in Patients With Liver Cirrhosis. Ann. Thorac. Surg. 2011, 91, 1393–1399. [Google Scholar] [CrossRef]
- Feng, K.; Gupta, V.; Terrazas, E.; Yeghiazarians, Y.; Ports, T.; Gregoratos, G.; Tavakol, M.; Roberts, J.P.; Boyle, A. Trans-Radial versus Trans-Femoral Access in Patients with End-Stage Liver Disease Undergoing Cardiac Catheterization. Am. J. Cardiovasc. Dis. 2014, 4, 133–139. [Google Scholar] [PubMed]
- Singh, V.; Patel, N.J.; Rodriguez, A.P.; Shantha, G.; Arora, S.; Deshmukh, A.; Cohen, M.G.; Grines, C.; De Marchena, E.; Badheka, A.; et al. Percutaneous Coronary Intervention in Patients With End-Stage Liver Disease. Am. J. Cardiol. 2016, 117, 1729–1734. [Google Scholar] [CrossRef]
- Istanbuly, S.; Matetic, A.; Mohamed, M.O.; Panaich, S.; Velagapudi, P.; Elgendy, I.Y.; Paul, T.K.; Alkhouli, M.; Mamas, M.A. Comparison of Outcomes of Patients With Versus Without Chronic Liver Disease Undergoing Percutaneous Coronary Intervention. Am. J. Cardiol. 2021, 156, 32–38. [Google Scholar] [CrossRef]
- Ostojic, Z.; Ostojic, A.; Bulum, J.; Mrzljak, A. Safety and Efficacy of Dual Antiplatelet Therapy after Percutaneous Coronary Interventions in Patients with End-Stage Liver Disease. World J. Cardiol. 2021, 13, 599–607. [Google Scholar] [CrossRef]
- Lisman, T.; Porte, R.J. Pathogenesis, Prevention, and Management of Bleeding and Thrombosis in Patients with Liver Diseases. Res. Pract. Thromb. Haemost. 2017, 1, 150–161. [Google Scholar] [CrossRef]
| Author | Sample, n (PCI-Cirrhosis/PCI) | Female, n | Age, Years | DM, n | HTN, n | HLD, n | AF, n | MI, n | Stroke, n |
|---|---|---|---|---|---|---|---|---|---|
| Lu et al., 2020 [21] | 7125/1,837,455 | 2183/605,115 | 63.9/64.7 | 3658/668,513 | 5145/1,364,546 | 3684/1,314,543 | 1125/214,220 | 1050/256,047 | 102/16,636 |
| Alazzawi et al., 2017 [22] | 609/609 | 256/329 | 60.16/60 | - | - | - | - | - | - |
| Alqahtani et al., 2020 [23] | 20,366/8,839,812 | 5386/2,965,457 | 63/64 | 8882/2,962,452 | 13,064/6,139,439 | 6797/5,451,654 | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khandait, H.; Jaiswal, V.; Hanif, M.; Shrestha, A.B.; Iturburu, A.; Shah, M.; Ishak, A.; Garimella, V.; Ang, S.P.; Mathew, M. Percutaneous Coronary Intervention Outcomes in Patients with Liver Cirrhosis: A Systematic Review and Meta-Analysis. J. Cardiovasc. Dev. Dis. 2023, 10, 92. https://doi.org/10.3390/jcdd10030092
Khandait H, Jaiswal V, Hanif M, Shrestha AB, Iturburu A, Shah M, Ishak A, Garimella V, Ang SP, Mathew M. Percutaneous Coronary Intervention Outcomes in Patients with Liver Cirrhosis: A Systematic Review and Meta-Analysis. Journal of Cardiovascular Development and Disease. 2023; 10(3):92. https://doi.org/10.3390/jcdd10030092
Chicago/Turabian StyleKhandait, Harshwardhan, Vikash Jaiswal, Muhammad Hanif, Abhigan Babu Shrestha, Alisson Iturburu, Maitri Shah, Angela Ishak, Vamsi Garimella, Song Peng Ang, and Midhun Mathew. 2023. "Percutaneous Coronary Intervention Outcomes in Patients with Liver Cirrhosis: A Systematic Review and Meta-Analysis" Journal of Cardiovascular Development and Disease 10, no. 3: 92. https://doi.org/10.3390/jcdd10030092
APA StyleKhandait, H., Jaiswal, V., Hanif, M., Shrestha, A. B., Iturburu, A., Shah, M., Ishak, A., Garimella, V., Ang, S. P., & Mathew, M. (2023). Percutaneous Coronary Intervention Outcomes in Patients with Liver Cirrhosis: A Systematic Review and Meta-Analysis. Journal of Cardiovascular Development and Disease, 10(3), 92. https://doi.org/10.3390/jcdd10030092