Monoclonal Gammopathy of Undetermined Cardiovascular Significance; Current Evidence and Novel Insights
Abstract
:1. Introduction
2. MGUS and CVD
2.1. Cardiovascular Risk Factors in Patients with MGUS
2.1.1. Diabetes Mellitus
2.1.2. Obesity
2.1.3. Cigarette Smoking
2.1.4. Arterial Hypertension
2.1.5. Dyslipidemia
2.1.6. Chronic Kidney Disease
2.2. Cardiovascular Disease Endpoints
2.3. Clinical CVD in Patients with MGUS
| Study | Study Design | Population | Outcome—Effect Estimate |
|---|---|---|---|
| Hamadi et al., 2023 [15] | Retrospective study | 9007 MGUS 2404 MGUS + AF 6603 MGUS without AF | 2920 (32.4%) of people with MGUS had CAD 748 (8.3%) of people with MGUS had stroke |
| Schwartz et al., 2022 [10] | Prospective study | 8189 MGUS 81,890 controls | Acute MI infarction (HR (95%CI): 1.22 (95% CI: 1.06–1.40)) Ischemic stroke (HR (95% CI): 1.16 (1.03–1.30)) PAD (HR (95% CI): 1.69 (1.47–1.95)) |
| El Khoury et al., 2022 [39] | Cohort study | 592 MGUS 3615 controls | Coronary artery disease MGUS (OR (95% CI): 1.22 (0.97–1.53)) Acute myocardial infarction MGUS (OR (95% CI): 1.39 (1.07–1.80)) |
| Kang et al., 2021 [14] | South Korea nationwide registry-based study | 470 MGUS 405 MGUS without comorbidities at the time of MGUS diagnosis | 73 (18%) myocardial infarction events 67 (16.1%) stroke events |
| Kristinsson et al., 2010 [38] | Swedish nationwide retrospective cohort study | 5326 MGUS 20,161 controls | Coronary artery disease 1-year follow-up: HR (95% CI): 2.0 (1.7–2.4) 5-year follow-up: HR (95% CI): 1.5 (1.3–1.7) 10-year follow-up: HR (95% CI): 1.5 (1.3–1.6) Cerebrovascular disease 1-year follow-up: HR (95% CI): 1.4 (1.0–1.7) 5-year follow-up: HR (95% CI): 1.1 (1.0–1.3) 10-year follow-up: HR (95% CI): 1.1 (1.0–1.3) |
2.4. MGUS and CVD Outcomes
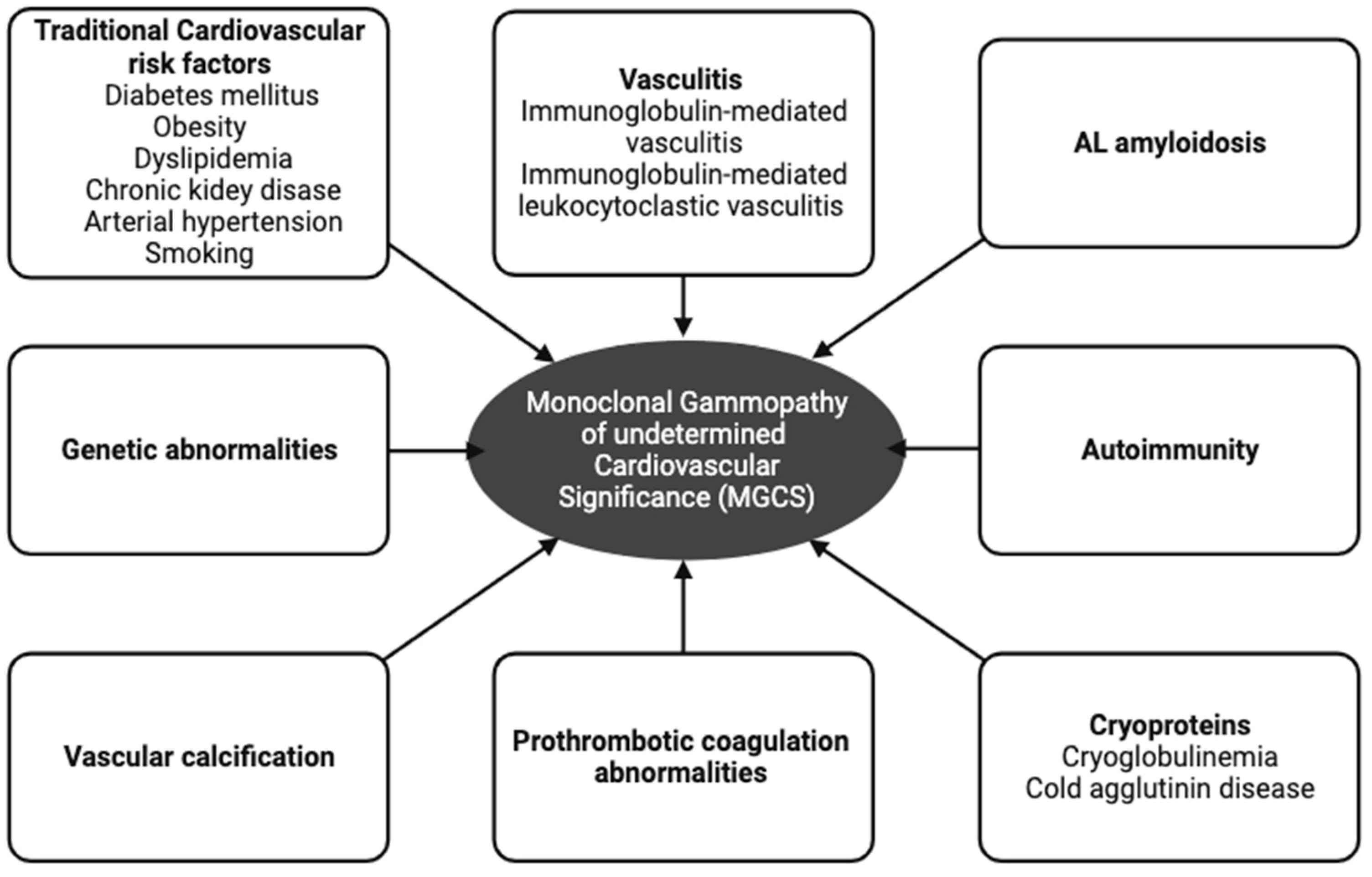
3. Pathophysiological Mechanisms between MGUS and CVD
3.1. Genetic Abnormalities
3.2. Vascular Calcification
3.3. AL Amyloidosis
3.4. Cryoproteins
3.4.1. Cryoglobulinemia
3.4.2. Cold Agglutinin Disease
3.5. Autoimmunity in MGUS
3.6. Other Factors
4. Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rajkumar, S.V.; Dimopoulos, M.A.; Palumbo, A.; Blade, J.; Merlini, G.; Mateos, M.V.; Kumar, S.; Hillengass, J.; Kastritis, E.; Richardson, P.; et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014, 15, e538–e548. [Google Scholar] [CrossRef] [PubMed]
- Kyle, R.A.; Larson, D.R.; Therneau, T.M.; Dispenzieri, A.; Kumar, S.; Cerhan, J.R.; Rajkumar, S.V. Long-Term Follow-up of Monoclonal Gammopathy of Undetermined Significance. N. Engl. J. Med. 2018, 378, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Fermand, J.P.; Bridoux, F.; Dispenzieri, A.; Jaccard, A.; Kyle, R.A.; Leung, N.; Merlini, G. Monoclonal gammopathy of clinical significance: A novel concept with therapeutic implications. Blood 2018, 132, 1478–1485. [Google Scholar] [CrossRef] [PubMed]
- Khwaja, J.; D’Sa, S.; Minnema, M.C.; Kersten, M.J.; Wechalekar, A.; Vos, J.M. IgM monoclonal gammopathies of clinical significance: Diagnosis and management. Haematologica 2022, 107, 2037–2050. [Google Scholar] [CrossRef]
- Jain, A.; Haynes, R.; Kothari, J.; Khera, A.; Soares, M.; Ramasamy, K. Pathophysiology and management of monoclonal gammopathy of renal significance. Blood Adv. 2019, 3, 2409–2423. [Google Scholar] [CrossRef]
- Leung, N.; Bridoux, F.; Batuman, V.; Chaidos, A.; Cockwell, P.; D’Agati, V.D.; Dispenzieri, A.; Fervenza, F.C.; Fermand, J.P.; Gibbs, S.; et al. The evaluation of monoclonal gammopathy of renal significance: A consensus report of the International Kidney and Monoclonal Gammopathy Research Group. Nat. Rev. Nephrol. 2019, 15, 45–59. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Plummer, C.; Driessen, C.; Szabo, Z.; Mateos, M.V. Management of cardiovascular risk in patients with multiple myeloma. Blood Cancer J. 2019, 9, 26. [Google Scholar] [CrossRef]
- Gkalea, V.; Fotiou, D.; Dimopoulos, M.A.; Kastritis, E. Monoclonal Gammopathy of Thrombotic Significance. Cancers 2023, 15, 480. [Google Scholar] [CrossRef]
- Schwartz, B.; Schou, M.; Ruberg, F.L.; Rucker, D.; Choi, J.; Siddiqi, O.; Monahan, K.; Kober, L.; Gislason, G.; Torp-Pedersen, C.; et al. Cardiovascular Morbidity in Monoclonal Gammopathy of Undetermined Significance: A Danish Nationwide Study. JACC CardioOncol 2022, 4, 313–322. [Google Scholar] [CrossRef]
- Kapoor, P.; Rajkumar, S.V. Cardiovascular Associations with Monoclonal Gammopathy of Undetermined Significance: Real or Coincidental? JACC CardioOncol 2022, 4, 323–325. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Back, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. IDF Diabetes Atlas 10th Edition. 2021. Available online: https://diabetesatlas.org (accessed on 1 July 2023).
- Kang, K.W.; Song, J.E.; Lee, B.H.; Jeon, M.J.; Yu, E.S.; Kim, D.S.; Lee, S.R.; Sung, H.J.; Choi, C.W.; Park, Y.; et al. A nationwide study of patients with monoclonal gammopathy of undetermined significance with a 10-year follow-up in South Korea. Sci. Rep. 2021, 11, 18449. [Google Scholar] [CrossRef] [PubMed]
- Hamadi, R.; Alameddine, Z.; Asmar, S.; Sakr, F.; Aridi, H.; Dimachkie, R.; Skouri, H. Outcomes of Patients with Monoclonal Gammopathy of Undetermined Significance with and without Atrial Fibrillation: A Retrospective Cohort Analysis of the Nationwide Inpatient Sample Database. J. Clin. Med. 2023, 12, 4436. [Google Scholar] [CrossRef] [PubMed]
- Tentolouris, A.; Ntanasis-Stathopoulos, I.; Eleftheriadou, I.; Malandrakis, P.; Tzeravini, E.; Gavriatopoulou, M. Diabetes mellitus and multiple myeloma; common features of two distinct entities. Diabetes Metab. Res. Rev. 2022, 38, e3535. [Google Scholar] [CrossRef] [PubMed]
- Shah, U.A.; Moshier, E.L.; Derkach, A.; Huang, Y.; Mailankody, S.; Tan, C.R.; Maclachlan, K.H.; Hultcrantz, M.; Korde, N.; Hassoun, H.; et al. Prevalence and impact of diabetes on survival of patients with multiple myeloma in different racial groups. Blood Adv. 2023; Online ahead of print. [Google Scholar] [CrossRef]
- Castaneda-Avila, M.A.; Ulbricht, C.M.; Epstein, M.M. Risk factors for monoclonal gammopathy of undetermined significance: A systematic review. Ann. Hematol. 2021, 100, 855–863. [Google Scholar] [CrossRef] [PubMed]
- Shah, U.A.; Rognvaldsson, S.; Derkach, A.; Bjorkholm, M.; Turesson, I.; David, Y.; Hultcrantz, M.; Tan, C.; Hassoun, H.; Korde, N.; et al. Diabetes mellitus and risk of plasma cell and lymphoproliferative disorders in 94,579 cases and 368,348 matched controls. Haematologica 2022, 107, 284–286. [Google Scholar] [CrossRef] [PubMed]
- Boursi, B.; Weiss, B.M.; Haynes, K.; Mamtani, R.; Yang, Y.X. Reappraisal of risk factors for monoclonal gammopathy of undetermined significance. Am. J. Hematol. 2016, 91, 581–584. [Google Scholar] [CrossRef]
- Landgren, O.; Rajkumar, S.V.; Pfeiffer, R.M.; Kyle, R.A.; Katzmann, J.A.; Dispenzieri, A.; Cai, Q.; Goldin, L.R.; Caporaso, N.E.; Fraumeni, J.F.; et al. Obesity is associated with an increased risk of monoclonal gammopathy of undetermined significance among black and white women. Blood 2010, 116, 1056–1059. [Google Scholar] [CrossRef]
- Grant, B.; Ratnayake, G.; Williams, C.L.; Long, A.; Halsall, D.J.; Semple, R.K.; Cavenagh, J.D.; Drake, W.M.; Church, D.S. Resolution of dysglycaemia after treatment of monoclonal gammopathy of endocrine significance. Eur. J. Endocrinol. 2023, lvad138. [Google Scholar] [CrossRef]
- Landgren, O.; Graubard, B.I.; Katzmann, J.A.; Kyle, R.A.; Ahmadizadeh, I.; Clark, R.; Kumar, S.K.; Dispenzieri, A.; Greenberg, A.J.; Therneau, T.M.; et al. Racial disparities in the prevalence of monoclonal gammopathies: A population-based study of 12,482 persons from the National Health and Nutritional Examination Survey. Leukemia 2014, 28, 1537–1542. [Google Scholar] [CrossRef] [PubMed]
- Georgakopoulou, R.; Andrikopoulou, A.; Sergentanis, T.N.; Fiste, O.; Zagouri, F.; Gavriatopoulou, M.; Psaltopoulou, T.; Kastritis, E.; Terpos, E.; Dimopoulos, M.A. Overweight/Obesity and Monoclonal Gammopathy of Undetermined Significance. Clin. Lymphoma Myeloma Leuk. 2021, 21, 361–367. [Google Scholar] [CrossRef]
- Thordardottir, M.; Lindqvist, E.K.; Lund, S.H.; Costello, R.; Burton, D.; Korde, N.; Mailankody, S.; Eiriksdottir, G.; Launer, L.J.; Gudnason, V.; et al. Obesity and risk of monoclonal gammopathy of undetermined significance and progression to multiple myeloma: A population-based study. Blood Adv. 2017, 1, 2186–2192. [Google Scholar] [CrossRef]
- Tentolouris, A.; Ntanasis-Stathopoulos, I.; Terpos, E. Obesity and multiple myeloma: Emerging mechanisms and perspectives. Semin. Cancer Biol. 2023, 92, 45–60. [Google Scholar] [CrossRef]
- Pasqualetti, P.; Collacciani, A.; Casale, R. Risk of monoclonal gammopathy of undetermined significance: A case-referent study. Am. J. Hematol. 1996, 52, 217–220. [Google Scholar] [CrossRef]
- Pasqualetti, P.; Festuccia, V.; Acitelli, P.; Collacciani, A.; Giusti, A.; Casale, R. Tobacco smoking and risk of haematological malignancies in adults: A case-control study. Br. J. Haematol. 1997, 97, 659–662. [Google Scholar] [CrossRef]
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef]
- National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke Prevention. Available online: https://www.cdc.gov/bloodpressure/facts.htm#:~:text=Nearly%20half%20of%20adults%20haveatmfhtAia.CDCHypertension (accessed on 8 July 2023).
- Epstein, M.M.; Zhou, Y.; Castaneda-Avila, M.A.; Cohen, H.J. Multimorbidity in patients with monoclonal gammopathy of undetermined significance. Int. J. Cancer 2023, 152, 2485–2492. [Google Scholar] [CrossRef]
- Pirillo, A.; Casula, M.; Olmastroni, E.; Norata, G.D.; Catapano, A.L. Global epidemiology of dyslipidaemias. Nat. Rev. Cardiol. 2021, 18, 689–700. [Google Scholar] [CrossRef] [PubMed]
- Dimopoulos, M.A.; Sonneveld, P.; Leung, N.; Merlini, G.; Ludwig, H.; Kastritis, E.; Goldschmidt, H.; Joshua, D.; Orlowski, R.Z.; Powles, R.; et al. International Myeloma Working Group Recommendations for the Diagnosis and Management of Myeloma-Related Renal Impairment. J. Clin. Oncol. 2016, 34, 1544–1557. [Google Scholar] [CrossRef]
- Dimopoulos, M.A.; Merlini, G.; Bridoux, F.; Leung, N.; Mikhael, J.; Harrison, S.J.; Kastritis, E.; Garderet, L.; Gozzetti, A.; van de Donk, N.; et al. Management of multiple myeloma-related renal impairment: Recommendations from the International Myeloma Working Group. Lancet Oncol. 2023, 24, e293–e311. [Google Scholar] [CrossRef] [PubMed]
- Gozzetti, A.; Guarnieri, A.; Zamagni, E.; Zakharova, E.; Coriu, D.; Bittrich, M.; Pika, T.; Tovar, N.; Schutz, N.; Ciofini, S.; et al. Monoclonal gammopathy of renal significance (MGRS): Real-world data on outcomes and prognostic factors. Am. J. Hematol. 2022, 97, 877–884. [Google Scholar] [CrossRef] [PubMed]
- Hicks, K.A.; Mahaffey, K.W.; Mehran, R.; Nissen, S.E.; Wiviott, S.D.; Dunn, B.; Solomon, S.D.; Marler, J.R.; Teerlink, J.R.; Farb, A.; et al. 2017 Cardiovascular and Stroke Endpoint Definitions for Clinical Trials. Circulation 2018, 137, 961–972. [Google Scholar] [CrossRef] [PubMed]
- Cefalu, W.T.; Kaul, S.; Gerstein, H.C.; Holman, R.R.; Zinman, B.; Skyler, J.S.; Green, J.B.; Buse, J.B.; Inzucchi, S.E.; Leiter, L.A.; et al. Cardiovascular Outcomes Trials in Type 2 Diabetes: Where Do We Go from Here? Reflections from a Diabetes Care Editors’ Expert Forum. Diabetes Care 2018, 41, 14–31. [Google Scholar] [CrossRef] [PubMed]
- Kristinsson, S.Y.; Pfeiffer, R.M.; Bjorkholm, M.; Goldin, L.R.; Schulman, S.; Blimark, C.; Mellqvist, U.H.; Wahlin, A.; Turesson, I.; Landgren, O. Arterial and venous thrombosis in monoclonal gammopathy of undetermined significance and multiple myeloma: A population-based study. Blood 2010, 115, 4991–4998. [Google Scholar] [CrossRef]
- El-Khoury, H.; Lee, D.J.; Alberge, J.B.; Redd, R.; Cea-Curry, C.J.; Perry, J.; Barr, H.; Murphy, C.; Sakrikar, D.; Barnidge, D.; et al. Prevalence of monoclonal gammopathies and clinical outcomes in a high-risk US population screened by mass spectrometry: A multicentre cohort study. Lancet Haematol. 2022, 9, e340–e349. [Google Scholar] [CrossRef]
- Kristinsson, S.Y.; Bjorkholm, M.; Andersson, T.M.; Eloranta, S.; Dickman, P.W.; Goldin, L.R.; Blimark, C.; Mellqvist, U.H.; Wahlin, A.; Turesson, I.; et al. Patterns of survival and causes of death following a diagnosis of monoclonal gammopathy of undetermined significance: A population-based study. Haematologica 2009, 94, 1714–1720. [Google Scholar] [CrossRef]
- Kyle, R.A.; Therneau, T.M.; Rajkumar, S.V.; Larson, D.R.; Plevak, M.F.; Melton, L.J., 3rd. Long-term follow-up of 241 patients with monoclonal gammopathy of undetermined significance: The original Mayo Clinic series 25 years later. Mayo Clin. Proc. 2004, 79, 859–866. [Google Scholar] [CrossRef]
- Gregersen, H.; Ibsen, J.; Mellemkjoer, L.; Dahlerup, J.; Olsen, J.; Sorensen, H.T. Mortality and causes of death in patients with monoclonal gammopathy of undetermined significance. Br. J. Haematol. 2001, 112, 353–357. [Google Scholar] [CrossRef]
- Pasqualetti, P.; Festuccia, V.; Collacciani, A.; Casale, R. The natural history of monoclonal gammopathy of undetermined significance. A 5- to 20-year follow-up of 263 cases. Acta Haematol. 1997, 97, 174–179. [Google Scholar] [CrossRef]
- Xu, Z.; Sun, Y.; Xu, T.; Shi, Y.; Liang, L.; Liu, P.; Ge, J. MGUS Predicts Worse Prognosis in Patients with Coronary Artery Disease. J. Cardiovasc. Transl. Res. 2020, 13, 806–812. [Google Scholar] [CrossRef]
- Jaiswal, S.; Natarajan, P.; Silver, A.J.; Gibson, C.J.; Bick, A.G.; Shvartz, E.; McConkey, M.; Gupta, N.; Gabriel, S.; Ardissino, D.; et al. Clonal Hematopoiesis and Risk of Atherosclerotic Cardiovascular Disease. N. Engl. J. Med. 2017, 377, 111–121. [Google Scholar] [CrossRef]
- Testa, S.; Kumar, J.; Goodell, A.J.; Zehnder, J.L.; Alexander, K.M.; Sidana, S.; Arai, S.; Witteles, R.M.; Liedtke, M. Prevalence, mutational spectrum and clinical implications of clonal hematopoiesis of indeterminate potential in plasma cell dyscrasias. Semin. Oncol. 2022, 49, 465–475. [Google Scholar] [CrossRef]
- Da Via, M.C.; Lionetti, M.; Matera, A.; Travaglino, E.; Lucca, U.; Riva, E.; Tettamanti, M.; Baldini, L.; Neri, A.; Della Porta, M.G.; et al. MGUS and Chip: Two Faces, but Not of the Same Medal. Blood 2021, 138, 3800. [Google Scholar] [CrossRef]
- Lanzer, P.; Boehm, M.; Sorribas, V.; Thiriet, M.; Janzen, J.; Zeller, T.; St Hilaire, C.; Shanahan, C. Medial vascular calcification revisited: Review and perspectives. Eur. Heart J. 2014, 35, 1515–1525. [Google Scholar] [CrossRef]
- Lee, S.J.; Lee, I.K.; Jeon, J.H. Vascular Calcification-New Insights Into Its Mechanism. Int. J. Mol. Sci. 2020, 21, 2685. [Google Scholar] [CrossRef]
- Jeffcoate, W.J.; Rasmussen, L.M.; Hofbauer, L.C.; Game, F.L. Medial arterial calcification in diabetes and its relationship to neuropathy. Diabetologia 2009, 52, 2478–2488. [Google Scholar] [CrossRef]
- Terpos, E.; Ntanasis-Stathopoulos, I. Controversies in the use of new bone-modifying therapies in multiple myeloma. Br. J. Haematol. 2021, 193, 1034–1043. [Google Scholar] [CrossRef]
- Politou, M.; Terpos, E.; Anagnostopoulos, A.; Szydlo, R.; Laffan, M.; Layton, M.; Apperley, J.F.; Dimopoulos, M.A.; Rahemtulla, A. Role of receptor activator of nuclear factor-kappa B ligand (RANKL), osteoprotegerin and macrophage protein 1-alpha (MIP-1a) in monoclonal gammopathy of undetermined significance (MGUS). Br. J. Haematol. 2004, 126, 686–689. [Google Scholar] [CrossRef] [PubMed]
- Lipe, B.; Kambhampati, S.; Veldhuizen, P.V.; Yacoub, A.; Aljitawi, O.; Mikhael, J. Correlation between markers of bone metabolism and vitamin D levels in patients with monoclonal gammopathy of undetermined significance (MGUS). Blood Cancer J. 2017, 7, 646. [Google Scholar] [CrossRef] [PubMed]
- Merlini, G.; Dispenzieri, A.; Sanchorawala, V.; Schonland, S.O.; Palladini, G.; Hawkins, P.N.; Gertz, M.A. Systemic immunoglobulin light chain amyloidosis. Nat. Rev. Dis. Primers 2018, 4, 38. [Google Scholar] [CrossRef]
- Fotiou, D.; Theodorakakou, F.; Malandrakis, P.; Ntanasis-Stathopoulos, I.; Gavriatopoulou, M.; Kanellias, N.; Migkou, M.; Eleutherakis-Papaiakovou, E.; Papanikolaou, A.; Gakiopoulou, C.; et al. Patterns of target organ amyloid deposition in patients with AL amyloidosis; role for diagnosis and prognosis. Leuk. Lymphoma 2023, 64, 1212–1215. [Google Scholar] [CrossRef]
- Bellavia, D.; Pellikka, P.A.; Al-Zahrani, G.B.; Abraham, T.P.; Dispenzieri, A.; Miyazaki, C.; Lacy, M.; Scott, C.G.; Oh, J.K.; Miller, F.A., Jr. Independent predictors of survival in primary systemic (Al) amyloidosis, including cardiac biomarkers and left ventricular strain imaging: An observational cohort study. J. Am. Soc. Echocardiogr. 2010, 23, 643–652. [Google Scholar] [CrossRef]
- Tahir, U.A.; Doros, G.; Kim, J.S.; Connors, L.H.; Seldin, D.C.; Sam, F. Predictors of Mortality in Light Chain Cardiac Amyloidosis with Heart Failure. Sci. Rep. 2019, 9, 8552. [Google Scholar] [CrossRef]
- Theodorakakou, F.; Fotiou, D.; Spiliopoulou, V.; Roussou, M.; Malandrakis, P.; Ntanasis-Stathopoulos, I.; Migkou, M.; Eleutherakis-Papaiakovou, E.; Kanellias, N.; Papanikolaou, A.; et al. Outcomes of patients with light chain (AL) amyloidosis after failure of daratumumab-based therapy. Br. J. Haematol. 2023, 203, 411–415. [Google Scholar] [CrossRef]
- Kastritis, E.; Gavriatopoulou, M.; Roussou, M.; Bagratuni, T.; Migkou, M.; Fotiou, D.; Ziogas, D.C.; Kanellias, N.; Eleutherakis-Papaiakovou, E.; Dialoupi, I.; et al. Efficacy of lenalidomide as salvage therapy for patients with AL amyloidosis. Amyloid 2018, 25, 234–241. [Google Scholar] [CrossRef]
- Kastritis, E.; Dialoupi, I.; Gavriatopoulou, M.; Roussou, M.; Kanellias, N.; Fotiou, D.; Ntanasis-Stathopoulos, I.; Papadopoulou, E.; Ziogas, D.C.; Stamatelopoulos, K.; et al. Primary treatment of light-chain amyloidosis with bortezomib, lenalidomide, and dexamethasone. Blood Adv. 2019, 3, 3002–3009. [Google Scholar] [CrossRef]
- Nicol, M.; Siguret, V.; Vergaro, G.; Aimo, A.; Emdin, M.; Dillinger, J.G.; Baudet, M.; Cohen-Solal, A.; Villesuzanne, C.; Harel, S.; et al. Thromboembolism and bleeding in systemic amyloidosis: A review. ESC Heart Fail. 2022, 9, 11–20. [Google Scholar] [CrossRef]
- Cappelli, F.; Tini, G.; Russo, D.; Emdin, M.; Del Franco, A.; Vergaro, G.; Di Bella, G.; Mazzeo, A.; Canepa, M.; Volpe, M.; et al. Arterial thrombo-embolic events in cardiac amyloidosis: A look beyond atrial fibrillation. Amyloid 2021, 28, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Kastritis, E.; Fotiou, D.; Theodorakakou, F.; Dialoupi, I.; Migkou, M.; Roussou, M.; Karatrasoglou, E.A.; Tselegkidi, M.I.; Ntalianis, A.; Kanellias, N.; et al. Timing and impact of a deep response in the outcome of patients with systemic light chain (AL) amyloidosis. Amyloid 2021, 28, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Theodorakakou, F.; Briasoulis, A.; Fotiou, D.; Petropoulos, I.; Georgiopoulos, G.; Lama, N.; Kelekis, N.; Repasos, E.; Migkou, M.; Stamatelopoulos, K.; et al. Outcomes for patients with systemic light chain amyloidosis and Mayo stage 3B disease. Hematol. Oncol. 2023, 41, 725–732. [Google Scholar] [CrossRef]
- Napodano, C.; Gulli, F.; Rapaccini, G.L.; Marino, M.; Basile, U. Cryoglobulins: Identification, classification, and novel biomarkers of mysterious proteins. Adv. Clin. Chem. 2021, 104, 299–340. [Google Scholar]
- DynaMed. Cryoglobulinemia Type I. EBSCO Information Services. Available online: https://www.dynamed.com/condition/cryoglobulinemia-type-i-1 (accessed on 3 October 2023).
- Sidana, S.; Rajkumar, S.V.; Dispenzieri, A.; Lacy, M.Q.; Gertz, M.A.; Buadi, F.K.; Hayman, S.R.; Dingli, D.; Kapoor, P.; Gonsalves, W.I.; et al. Clinical presentation and outcomes of patients with type 1 monoclonal cryoglobulinemia. Am. J. Hematol. 2017, 92, 668–673. [Google Scholar] [CrossRef]
- He, K.; Zhang, Y.; Wang, W.; Wang, Y.; Sha, Y.; Zeng, X. Clinical Characteristics of Cryoglobulinemia with Cardiac Involvement in a Single Center. Front. Cardiovasc. Med. 2021, 8, 744648. [Google Scholar] [CrossRef]
- Berentsen, S. Cold agglutinin disease. Hematol. Am. Soc. Hematol. Educ. Program. 2016, 2016, 226–231. [Google Scholar] [CrossRef]
- Broome, C.M.; Cunningham, J.M.; Mullins, M.; Jiang, X.; Bylsma, L.C.; Fryzek, J.P.; Rosenthal, A. Increased risk of thrombotic events in cold agglutinin disease: A 10-year retrospective analysis. Res. Pract. Thromb. Haemost. 2020, 4, 628–635. [Google Scholar] [CrossRef]
- Bolla, E.; Tentolouris, N.; Sfikakis, P.P.; Tektonidou, M.G. Cardiovascular risk management in antiphospholipid syndrome: Trends over time and comparison with rheumatoid arthritis and diabetes mellitus. Lupus Sci. Med. 2021, 8, e000579. [Google Scholar] [CrossRef]
- Drosos, G.C.; Vedder, D.; Houben, E.; Boekel, L.; Atzeni, F.; Badreh, S.; Boumpas, D.T.; Brodin, N.; Bruce, I.N.; Gonzalez-Gay, M.A.; et al. EULAR recommendations for cardiovascular risk management in rheumatic and musculoskeletal diseases, including systemic lupus erythematosus and antiphospholipid syndrome. Ann. Rheum. Dis. 2022, 81, 768–779. [Google Scholar] [CrossRef] [PubMed]
- Tait, R.C.; Oogarah, P.K.; Houghton, J.B.; Farrand, S.E.; Haeney, M.R. Waldenstrom’s macroglobulinaemia secreting a paraprotein with lupus anticoagulant activity: Possible association with gastrointestinal tract disease and malabsorption. J. Clin. Pathol. 1993, 46, 678–680. [Google Scholar] [CrossRef] [PubMed]
- Hara, Y.; Makita, M.; Ishikawa, T.; Saeki, K.; Yamamoto, K.; Imajo, K.; Shima, M.; Ieko, M. Lupus anticoagulant hypoprothrombinemia syndrome in Bence-Jones protein kappa-type multiple myeloma patient with phosphatidylserine-dependent antiprothrombin antibody. Ann. Hematol. 2013, 92, 563–564. [Google Scholar] [CrossRef] [PubMed]
- von Landenberg, P.; Scholmerich, J.; Andreesen, R.; Vogelhuber, M.; Lackner, K.J. A case of Waldenstroem’s disease with a monoclonal IgM antiphospholipid antibody. Rheumatol. Int. 2002, 22, 129–131. [Google Scholar] [CrossRef] [PubMed]
- Stern, J.J.; Ng, R.H.; Triplett, D.A.; McIntyre, J.A. Incidence of antiphospholipid antibodies in patients with monoclonal gammopathy of undetermined significance. Am. J. Clin. Pathol. 1994, 101, 471–474. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.Y.; Yin, Y.F.; Teng, J.L.; Zhang, L.W.; Yang, C.D. IgMk paraprotein from gammopathy patient can bind to cardiolipin and interfere with coagulation assay: A case report. BMC Immunol. 2017, 18, 32. [Google Scholar] [CrossRef] [PubMed]
- Doyle, A.J.; Breen, K.A.; Hunt, B.J. Antiphospholipid Syndrome with Monoclonal Gammopathy-A Mechanism for Recurrent Thrombosis? Thromb. Haemost. 2021, 121, 1387–1390. [Google Scholar] [CrossRef] [PubMed]
- Drerup, C.; Metze, D.; Ehrchen, J.; Mitschang, C.; Neufeld, M.; Sunderkotter, C. Evidence for immunoglobulin-mediated vasculitis caused by monoclonal gammopathy in monoclonal gammopathy of unclear significance prompting oncologic treatment. JAAD Case Rep. 2019, 5, 288–291. [Google Scholar] [CrossRef]
- Umemura, H.; Yamasaki, O.; Iwatsuki, K. Leukocytoclastic vasculitis associated with immunoglobulin A lambda monoclonal gammopathy of undetermined significance: A case report and review of previously reported cases. J. Dermatol. 2018, 45, 1009–1012. [Google Scholar] [CrossRef] [PubMed]
- Cohen, I.; Amir, J.; Ben-Shaul, Y.; Pick, A.; De Vries, A. Plasma cell myeloma associated with an unusual myeloma protein causing impairment of fibrin aggregation and platelet function in a patient with multiple malignancy. Am. J. Med. 1970, 48, 766–776. [Google Scholar] [CrossRef]
- Auwerda, J.J.; Sonneveld, P.; de Maat, M.P.; Leebeek, F.W. Prothrombotic coagulation abnormalities in patients with paraprotein-producing B-cell disorders. Clin. Lymphoma Myeloma 2007, 7, 462–466. [Google Scholar] [CrossRef]
- Crowley, M.P.; Quinn, S.; Coleman, E.; Eustace, J.A.; Gilligan, O.M.; O’Shea, S.I. Differing coagulation profiles of patients with monoclonal gammopathy of undetermined significance and multiple myeloma. J. Thromb. Thrombolysis 2015, 39, 245–249. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tentolouris, A.; Ntanasis-Stathopoulos, I.; Gavriatopoulou, M.; Andreadou, I.; Terpos, E. Monoclonal Gammopathy of Undetermined Cardiovascular Significance; Current Evidence and Novel Insights. J. Cardiovasc. Dev. Dis. 2023, 10, 484. https://doi.org/10.3390/jcdd10120484
Tentolouris A, Ntanasis-Stathopoulos I, Gavriatopoulou M, Andreadou I, Terpos E. Monoclonal Gammopathy of Undetermined Cardiovascular Significance; Current Evidence and Novel Insights. Journal of Cardiovascular Development and Disease. 2023; 10(12):484. https://doi.org/10.3390/jcdd10120484
Chicago/Turabian StyleTentolouris, Anastasios, Ioannis Ntanasis-Stathopoulos, Maria Gavriatopoulou, Ioanna Andreadou, and Evangelos Terpos. 2023. "Monoclonal Gammopathy of Undetermined Cardiovascular Significance; Current Evidence and Novel Insights" Journal of Cardiovascular Development and Disease 10, no. 12: 484. https://doi.org/10.3390/jcdd10120484
APA StyleTentolouris, A., Ntanasis-Stathopoulos, I., Gavriatopoulou, M., Andreadou, I., & Terpos, E. (2023). Monoclonal Gammopathy of Undetermined Cardiovascular Significance; Current Evidence and Novel Insights. Journal of Cardiovascular Development and Disease, 10(12), 484. https://doi.org/10.3390/jcdd10120484








