Weight Change and Risk of Atherosclerosis Measured by Carotid Intima–Media Thickness (cIMT) from a Prospective Cohort—Analysis of the First-Wave Follow-Up Data of the Canadian Longitudinal Study on Aging (CLSA)
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants from the Canadian Longitudinal Study on Aging (CLSA)
2.2. Measurement of cIMT
2.3. Weight Change
2.4. Measurements of Demographic Variables and Other Cardiovascular Risk Factors at Baseline
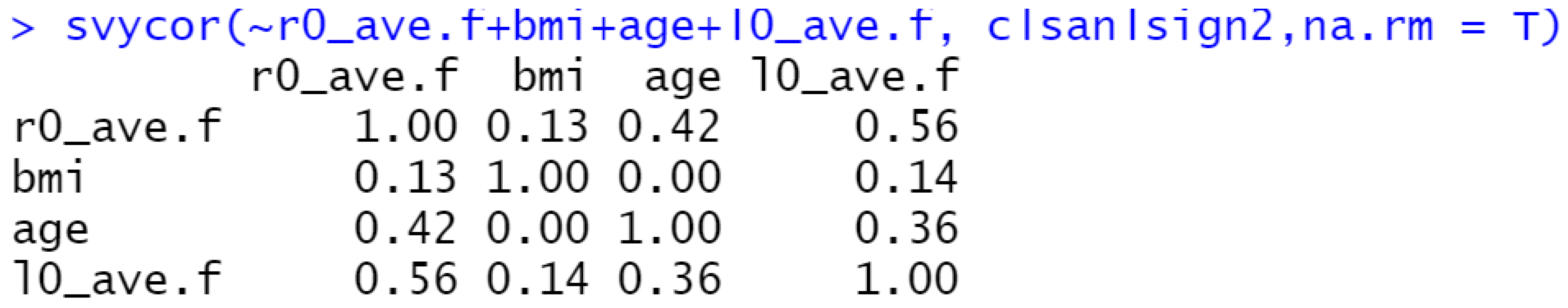
2.5. Statistical Analysis
3. Results
3.1. Summaries of the Descriptive Statistics
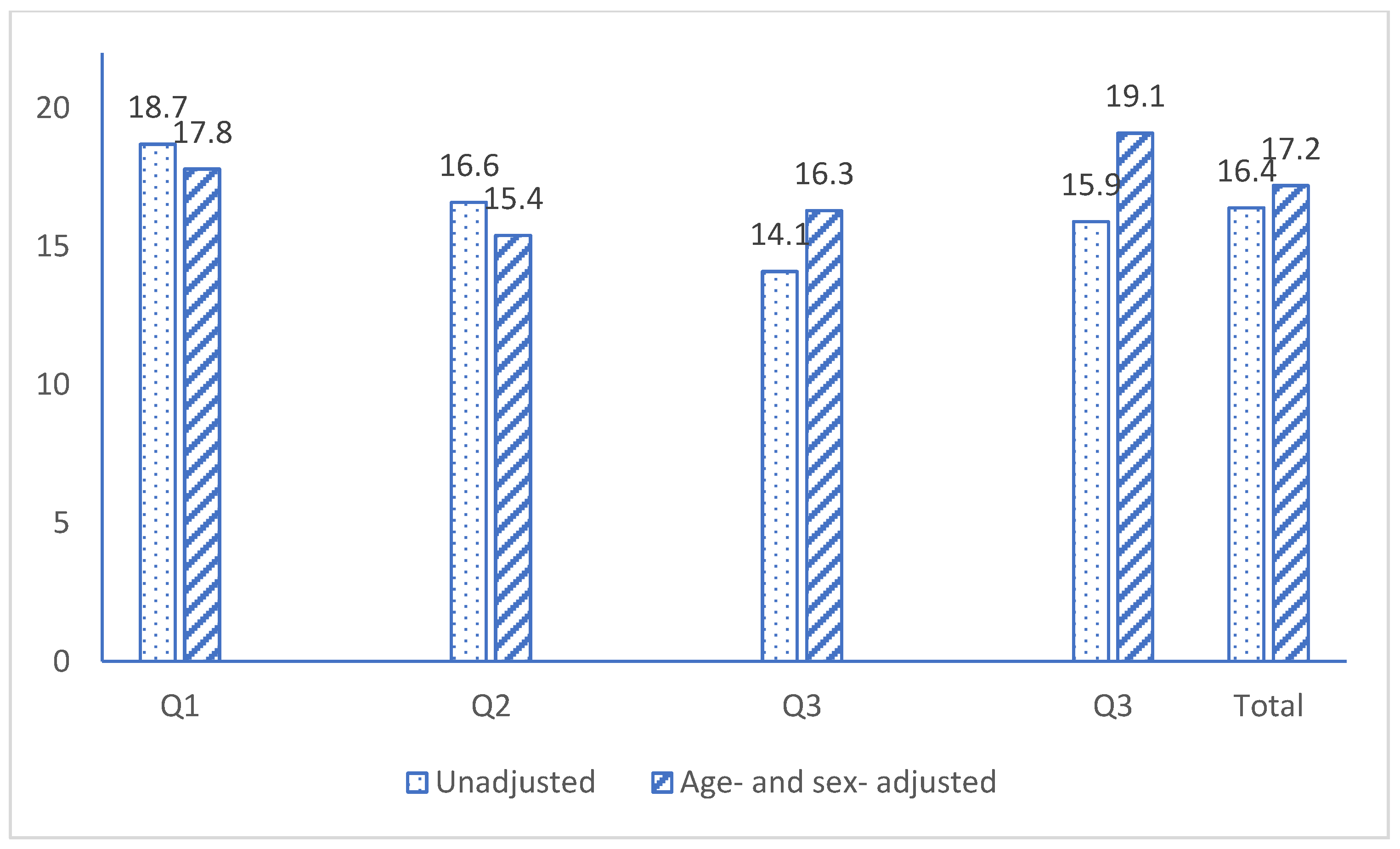
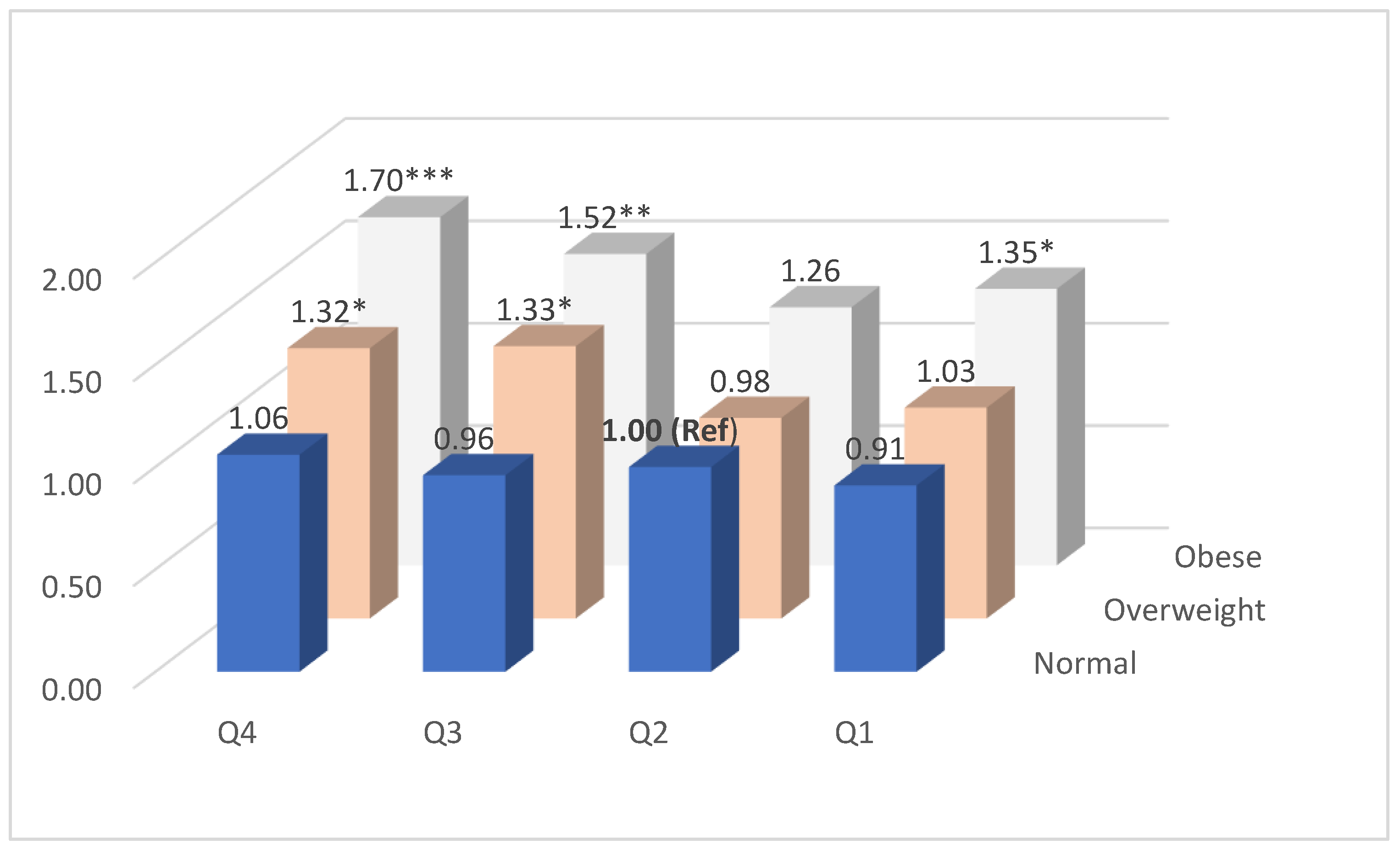
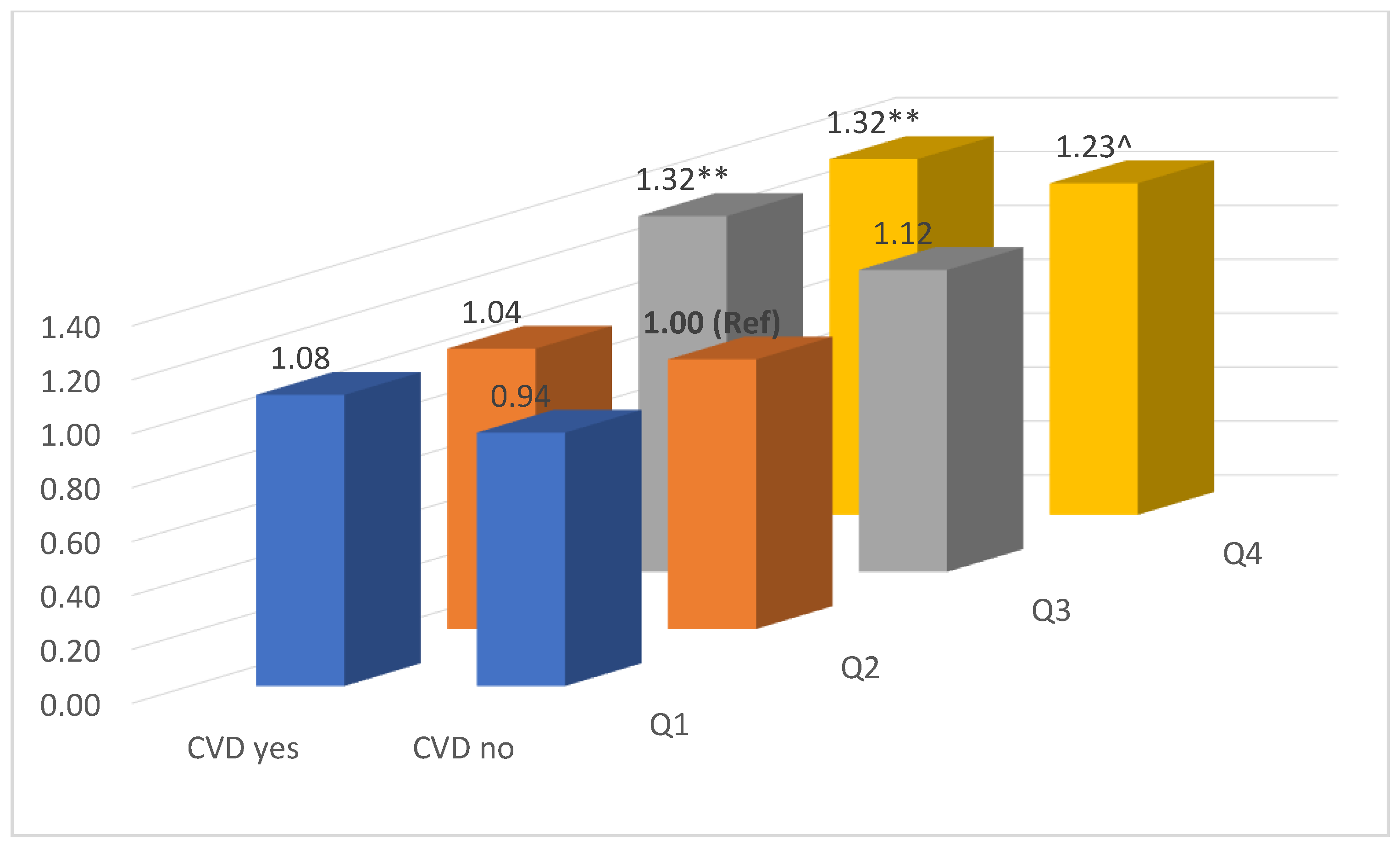
3.2. Adjusted ORs of cIMT > 1.0 mm for Weight Change in Different Situations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Ravani, A.; Werba, J.P.; Frigerio, B.; Sansaro, D.; Amato, M.; Tremoli, E.; Baldassarre, D. Assessment and relevance of carotid intima-media thickness (C-IMT) in primary and secondary cardiovascular prevention. Curr. Pharm. Des. 2015, 21, 1164–1171. [Google Scholar] [CrossRef] [PubMed]
- Den Ruijter, H.M.; Peters, S.A.; Anderson, T.J.; Britton, A.R.; Dekker, J.M.; Eijkemans, M.J.; Engstrom, G.; Evans, G.W.; de Graaf, J.; Grobbee, D.E.; et al. Common carotid intima-media thickness measurements in cardiovascular risk prediction: A meta-analysis. JAMA 2012, 308, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Willeit, P.; Tschiderer, L.; Allara, E.; Reuber, K.; Seekircher, L.; Gao, L.; Liao, X.; Lonn, E.; Gerstein, H.C.; Yusuf, S.; et al. Carotid Intima-Media Thickness Progression as Surrogate Marker for Cardiovascular Risk: Meta-Analysis of 119 Clinical Trials Involving 100,667 Patients. Circulation 2020, 142, 621–642. [Google Scholar] [CrossRef]
- Lee, J.S.; Kritchevsky, S.B.; Harris, T.B.; Tylavsky, F.; Rubin, S.M.; Newman, A.B. Short-term weight changes in community-dwelling older adults: The Health, Aging, and Body Composition Weight Change Substudy. Am. J. Clin. Nutr. 2005, 82, 644–650. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Suh, J.; Cho, Y.J.; Kim, H.J.; Choi, S.S. Age-Related Difference in Weight Change and All-Cause Mortality in Middle-Aged and Older Korean Populations: Korean Longitudinal Study of Aging. Korean J. Fam. Med. 2021, 42, 297–302. [Google Scholar] [CrossRef]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Despres, J.P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef]
- James, W.P.T. Obesity: A Global Public Health Challenge. Clin. Chem. 2018, 64, 24–29. [Google Scholar] [CrossRef]
- Charakida, M.; Khan, T.; Johnson, W.; Finer, N.; Woodside, J.; Whincup, P.H.; Sattar, N.; Kuh, D.; Hardy, R.; Deanfield, J. Lifelong patterns of BMI and cardiovascular phenotype in individuals aged 60-64 years in the 1946 British birth cohort study: An epidemiological study. Lancet Diabetes Endocrinol. 2014, 2, 648–654. [Google Scholar] [CrossRef]
- Magnussen, C.G.; Venn, A.; Thomson, R.; Juonala, M.; Srinivasan, S.R.; Viikari, J.S.; Berenson, G.S.; Dwyer, T.; Raitakari, O.T. The association of pediatric low- and high-density lipoprotein cholesterol dyslipidemia classifications and change in dyslipidemia status with carotid intima-media thickness in adulthood evidence from the cardiovascular risk in Young Finns study, the Bogalusa Heart study, and the CDAH (Childhood Determinants of Adult Health) study. J. Am. Coll. Cardiol. 2009, 53, 860–869. [Google Scholar]
- Gentile, M.; Iannuzzi, A.; Iannuzzo, G.; Covetti, G.; Panico, S.; Mattiello, A.; De Michele, M.; Rubba, P. Relation of body mass index with carotid intima-media thickness and diameter is independent of metabolic syndrome in postmenopausal Mediterranean women. Menopause 2012, 19, 1104–1108. [Google Scholar] [CrossRef]
- Peters, S.A.; Lind, L.; Palmer, M.K.; Grobbee, D.E.; Crouse, J.R., 3rd; O’Leary, D.H.; Evans, G.W.; Raichlen, J.; Bots, M.L.; den Ruijter, H.M.; et al. Increased age, high body mass index and low HDL-C levels are related to an echolucent carotid intima-media: The METEOR study. J. Intern. Med. 2012, 272, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Skilton, M.R.; Yeo, S.Q.; Ne, J.Y.; Celermajer, D.S.; Caterson, I.D.; Lee, C.M. Weight loss and carotid intima-media thickness-a meta-analysis. Obesity 2017, 25, 357–362. [Google Scholar] [CrossRef]
- Look, A.R.G.; Wing, R.R.; Bolin, P.; Brancati, F.L.; Bray, G.A.; Clark, J.M.; Coday, M.; Crow, R.S.; Curtis, J.M.; Egan, C.M.; et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N. Engl. J. Med. 2013, 369, 145–154. [Google Scholar]
- Bots, M.L.; Groenewegen, K.A.; Anderson, T.J.; Britton, A.R.; Dekker, J.M.; Engstrom, G.; Evans, G.W.; de Graaf, J.; Grobbee, D.E.; Hedblad, B.; et al. Common carotid intima-media thickness measurements do not improve cardiovascular risk prediction in individuals with elevated blood pressure: The USE-IMT collaboration. Hypertension 2014, 63, 1173–1181. [Google Scholar] [CrossRef]
- Gardin, J.M.; Bartz, T.M.; Polak, J.F.; O’Leary, D.H.; Wong, N.D. What do carotid intima-media thickness and plaque add to the prediction of stroke and cardiovascular disease risk in older adults? The cardiovascular health study. J. Am. Soc. Echocardiogr. 2014, 27, 998–1005.e2. [Google Scholar] [CrossRef] [PubMed]
- Raina, P.S.; Wolfson, C.; Kirkland, S.A.; Griffith, L.E.; Oremus, M.; Patterson, C.; Tuokko, H.; Penning, M.; Balion, C.M.; Hogan, D.; et al. The Canadian longitudinal study on aging (CLSA). Can. J. Aging 2009, 28, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Raina, P.; Wolfson, C.; Kirkland, S.; Griffith, L.E.; Balion, C.; Cossette, B.; Dionne, I.; Hofer, S.; Hogan, D.; van den Heuvel, E.R.; et al. Cohort Profile: The Canadian Longitudinal Study on Aging (CLSA). Int. J. Epidemiol. 2019, 48, 1752j–1753j. [Google Scholar] [CrossRef]
- CLSA. Canadian Longitudinal Study on Aging: SOP_DCS_0011 Carotid Intima Media Thickness; CLSA: Hamilton, ON, Canada, 2015. [Google Scholar]
- CLSA. Canadian Longitudinal Study on Aging: SOP_DCS_0006 Standing Height and Weight Measurement; CLSA: Hamilton, ON, Canada, 2016. [Google Scholar]
- Yano, T.; Godai, K.; Kabayama, M.; Akasaka, H.; Takeya, Y.; Yamamoto, K.; Yasumoto, S.; Masui, Y.; Arai, Y.; Ikebe, K.; et al. Factors associated with weight loss by age among community-dwelling older people. BMC Geriatr. 2023, 23, 277. [Google Scholar] [CrossRef]
- CLSA. CLSA Technical Document (Version 1.2) Sampling and Computation of Response Rates and Sample Weights for the Tracking (Telephone Interview) Participants and Comprehensive Participants; CLSA: Hamilton, ON, Canada, 2020. [Google Scholar]
- Asaleye, A.A.; Braimoh, K.T.; Oyinloye, O.I.; Asaleye, C.M.; Omisore, A.D. Variation of Carotid Intima Media Thickness With Body Mass Index in Healthy Adults of Black African Descent. J. Ultrasound Med. 2019, 38, 123–130. [Google Scholar] [CrossRef]
- Bosch, X.; Monclus, E.; Escoda, O.; Guerra-Garcia, M.; Moreno, P.; Guasch, N.; Lopez-Soto, A. Unintentional weight loss: Clinical characteristics and outcomes in a prospective cohort of 2677 patients. PLoS ONE 2017, 12, e0175125. [Google Scholar] [CrossRef]
- Nicholson, B.D.; Hamilton, W.; O’Sullivan, J.; Aveyard, P.; Hobbs, F.R. Weight loss as a predictor of cancer in primary care: A systematic review and meta-analysis. Br. J. Gen. Pract. 2018, 68, e311–e322. [Google Scholar] [CrossRef] [PubMed]
- McGill, H.C., Jr.; McMahan, C.A.; Herderick, E.E.; Malcom, G.T.; Tracy, R.E.; Strong, J.P. Origin of atherosclerosis in childhood and adolescence. Am. J. Clin. Nutr. 2000, 72, 1307S–1315S. [Google Scholar] [CrossRef] [PubMed]
- van den Munckhof, I.C.L.; Jones, H.; Hopman, M.T.E.; de Graaf, J.; Nyakayiru, J.; van Dijk, B.; Eijsvogels, T.M.H.; Thijssen, D.H.J. Relation between age and carotid artery intima-medial thickness: A systematic review. Clin. Cardiol. 2018, 41, 698–704. [Google Scholar] [CrossRef]
- Rodgers, J.L.; Jones, J.; Bolleddu, S.I.; Vanthenapalli, S.; Rodgers, L.E.; Shah, K.; Karia, K.; Panguluri, S.K. Cardiovascular Risks Associated with Gender and Aging. J. Cardiovasc. Dev. Dis. 2019, 6, 19. [Google Scholar] [CrossRef] [PubMed]
| Weight Change Quartiles (kg) | |||||
|---|---|---|---|---|---|
| <−2.25 | ~0.10 | ~2.35 | ≥2.35 | p-Value | |
| n | 4967 | 5336 | 5263 | 5134 | |
| Age (yrs. mean (SE)) | 60.9 (0.3) | 61.0 (0.3) | 59.0 (0.3) | 56.6 (0.2) | *** |
| Male (%) | 51.2 | 46.1 | 46.5 | 48.4 | ^ |
| Married (%) | 72.7 | 75.4 | 79.4 | 75.6 | *** |
| Country of birth as Canada (%) | 82.0 | 78.2 | 80.4 | 83.7 | ** |
| Bachelor’s degree received (%) | 40.6 | 44.3 | 45.5 | 41.6 | *** |
| General health^ (%) | 89.2 | 92.0 | 93.5 | 90.6 | *** |
| Current smoking (%) | 12.3 | 8.2 | 8.8 | 12.1 | *** |
| Alcohol (%) | 84.8 | 87.9 | 87.7 | 86.9 | *** |
| CESD10^ (mean (SE)) | 5.83 (0.14) | 5.21 (0.14) | 5.12 (0.14) | 5.67 (0.12) | ns |
| Total cholesterol (mol/L, mean (SE)) | 5.16 (0.03) | 5.22 (0.03) | 5.23 (0.03) | 5.16 (0.03) | ns |
| HDL cholesterol (mol/L, mean (SE)) | 1.42 (0.01) | 1.52 (0.01) | 1.52 (0.01) | 1.46 (0.01) | *** |
| Non-HDL cholesterol (mol/L, mean (SE)) | 3.74 (0.03) | 3.70 (0.03) | 3.71 (0.03) | 3.70 (0.03) | ns |
| SBP (mmHg, mean (SE)) | 122.9 (0.6) | 120.1 (0.4) | 118.3 (0.4) | 118.9 (0.4) | *** |
| DBP (mmHg, mean (SE)) | 75.9 (0.3) | 74.5 (0.3) | 74.3 (0.2) | 75.5 (0.3) | * |
| BMI (kg/m2, mean (SE)) | 29.7 (0.2) | 27.1 (0.1) | 26.9 (0.1) | 28.6 (0.2) | *** |
| Waist circumference (cm, mean (SE)) | 98.7 (0.5) | 91.3 (0.4) | 90.7 (0.4) | 94.7 (0.5) | *** |
| Height (m, mean (SE)) | 1.691 (0.003) | 1.675 (0.003) | 1.680 (0.003) | 1.693 (0.003) | * |
| Weight (kg, mean (SE)) | 85.1 (0.6) | 76.2 (0.4) | 76.2 (0.4) | 82.2 (0.5) | *** |
| Weight change at the first follow-up (kg, mean (SE)) | −5.79 (0.12) | −0.95 (0.02) | 1.18 (0.02) | 5.29 (0.09) | *** |
| Cardiovascular diseases (%) | 50.7 | 40.6 | 38.4 | 42.2 | *** |
| Weight Change at the First Follow-Up | ||||||||
|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 (Ref) | Q3 | Q4 | |||||
| OR | 95% CI | OR | OR | 95% CI | OR | 95% CI | ||
| Model 1 | n = 17,828 | 1.14 | (1.01, 129) | 1.00 | 1.09 | (0.96, 1.23) | 1.29 | (1.14, 1.46) |
| Model 2 | n = 17,458 | 1.12 | (0.98, 1.27) | 1.00 | 1.09 | (0.96, 1.23) | 1.28 | (1.13, 1.46) |
| Model 3 | n = 13,731 | 1.07 | (0.92, 1.23) | 1.00 | 1.19 | (1.03, 1.37) | 1.31 | (1.13, 1.51) |
| Model 4 | n = 13,715 | 1.00 | (0.86, 1.15) | 1.00 | 1.19 | (1.03, 1.38) | 1.25 | (1.08, 1.45) |
| Weight Change Quartile at Follow-Up | |||||
|---|---|---|---|---|---|
| Q1 | Q2 (Ref) | Q3 | Q4 | Total | |
| Age | |||||
| <65 years (n = 8718) | |||||
| Right cIMT (mm, mean (SE)) | 0.729 (0.005) | 0.716 (0.005) | 0.715 (0.005) | 0.718 (0.005) | 0.720 (0.005) |
| Left cIMT (mm, mean (SE)) | 0.751 (0.005) | 0.746 (0.006) | 0.744 (0.005) | 0.749 (0.005) | 0.749 (0.005) |
| cIMT > 1.0 mm (%) | 11.6 | 9.6 | 9.3 | 12.3 | 11.0 |
| OR^ (95% CI) | 1.20 (0.98, 1.48) | 1.00 | 1.36 (1.11, 1.66) | 1.41 (1.17, 1.72) | |
| 65 + years (n = 4977) | |||||
| Right cIMT (mm, mean (SE)) | 0.867 (0.008) | 0.849 (0.007) | 0.838 (0.007) | 0.861 (0.010) | 0.853 (0.008) |
| Left cIMT (mm, mean (SE)) | 0.886 (0.007) | 0.872 (0.008) | 0.868 (0.007) | 0.870 (0.010) | 0.874 (0.008) |
| cIMT > 1.0 mm (%) | 32.9 | 29.7 | 26.7 | 30.9 | 30.0 |
| OR (95% CI) | 0.98 (0.81, 1.15) | 1.00 | 1.09 (0.91, 1.30) | 1.21 (1.00, 1.48) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Sze, N.S.K.; Narushima, M.; O’Leary, D. Weight Change and Risk of Atherosclerosis Measured by Carotid Intima–Media Thickness (cIMT) from a Prospective Cohort—Analysis of the First-Wave Follow-Up Data of the Canadian Longitudinal Study on Aging (CLSA). J. Cardiovasc. Dev. Dis. 2023, 10, 435. https://doi.org/10.3390/jcdd10100435
Liu J, Sze NSK, Narushima M, O’Leary D. Weight Change and Risk of Atherosclerosis Measured by Carotid Intima–Media Thickness (cIMT) from a Prospective Cohort—Analysis of the First-Wave Follow-Up Data of the Canadian Longitudinal Study on Aging (CLSA). Journal of Cardiovascular Development and Disease. 2023; 10(10):435. https://doi.org/10.3390/jcdd10100435
Chicago/Turabian StyleLiu, Jian, Newman Siu Kwan Sze, Miya Narushima, and Deborah O’Leary. 2023. "Weight Change and Risk of Atherosclerosis Measured by Carotid Intima–Media Thickness (cIMT) from a Prospective Cohort—Analysis of the First-Wave Follow-Up Data of the Canadian Longitudinal Study on Aging (CLSA)" Journal of Cardiovascular Development and Disease 10, no. 10: 435. https://doi.org/10.3390/jcdd10100435
APA StyleLiu, J., Sze, N. S. K., Narushima, M., & O’Leary, D. (2023). Weight Change and Risk of Atherosclerosis Measured by Carotid Intima–Media Thickness (cIMT) from a Prospective Cohort—Analysis of the First-Wave Follow-Up Data of the Canadian Longitudinal Study on Aging (CLSA). Journal of Cardiovascular Development and Disease, 10(10), 435. https://doi.org/10.3390/jcdd10100435






