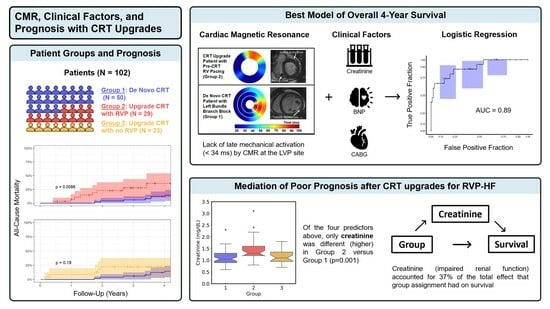
Cardiac Magnetic Resonance, Electromechanical Activation, Kidney Function, and Natriuretic Peptides in Cardiac Resynchronization Therapy Upgrades
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Baseline Characteristics and Response Measures of Entire Patient Cohort
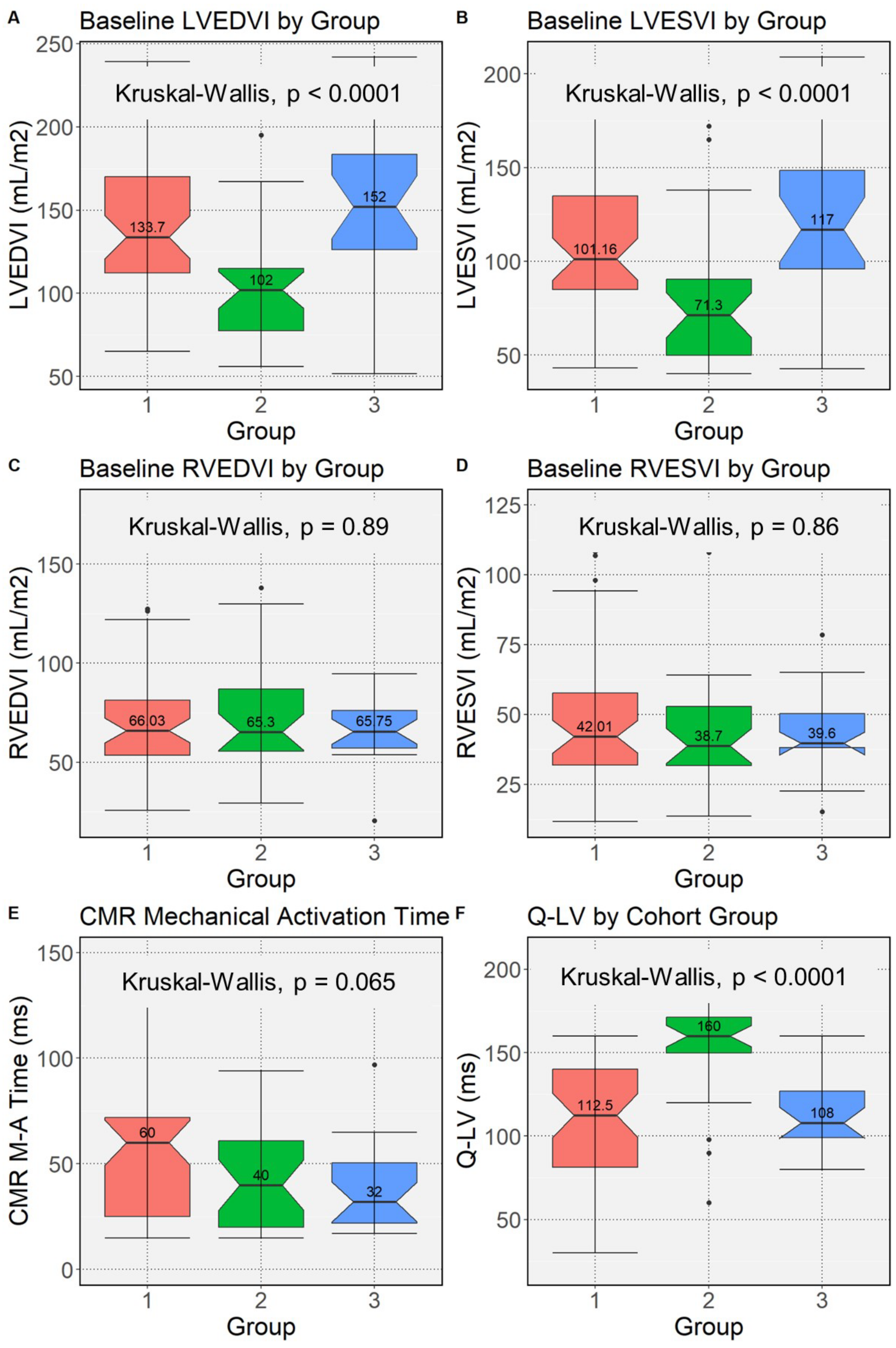
3.2. Mechanical and Electrical Activation at the Left Ventricular Pacing Site by Upgrade/De Novo Group
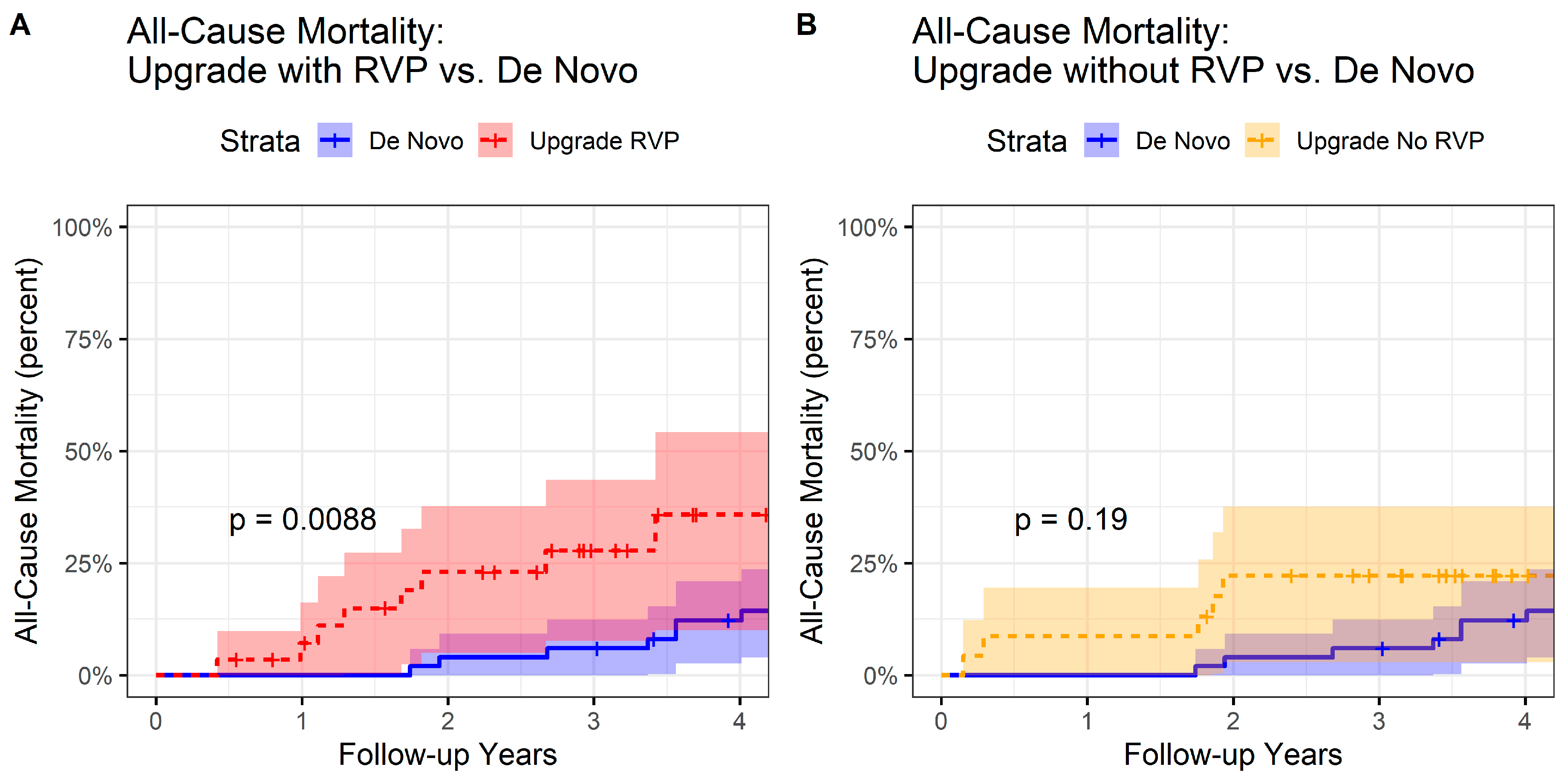
3.3. All-Cause Mortality by Group
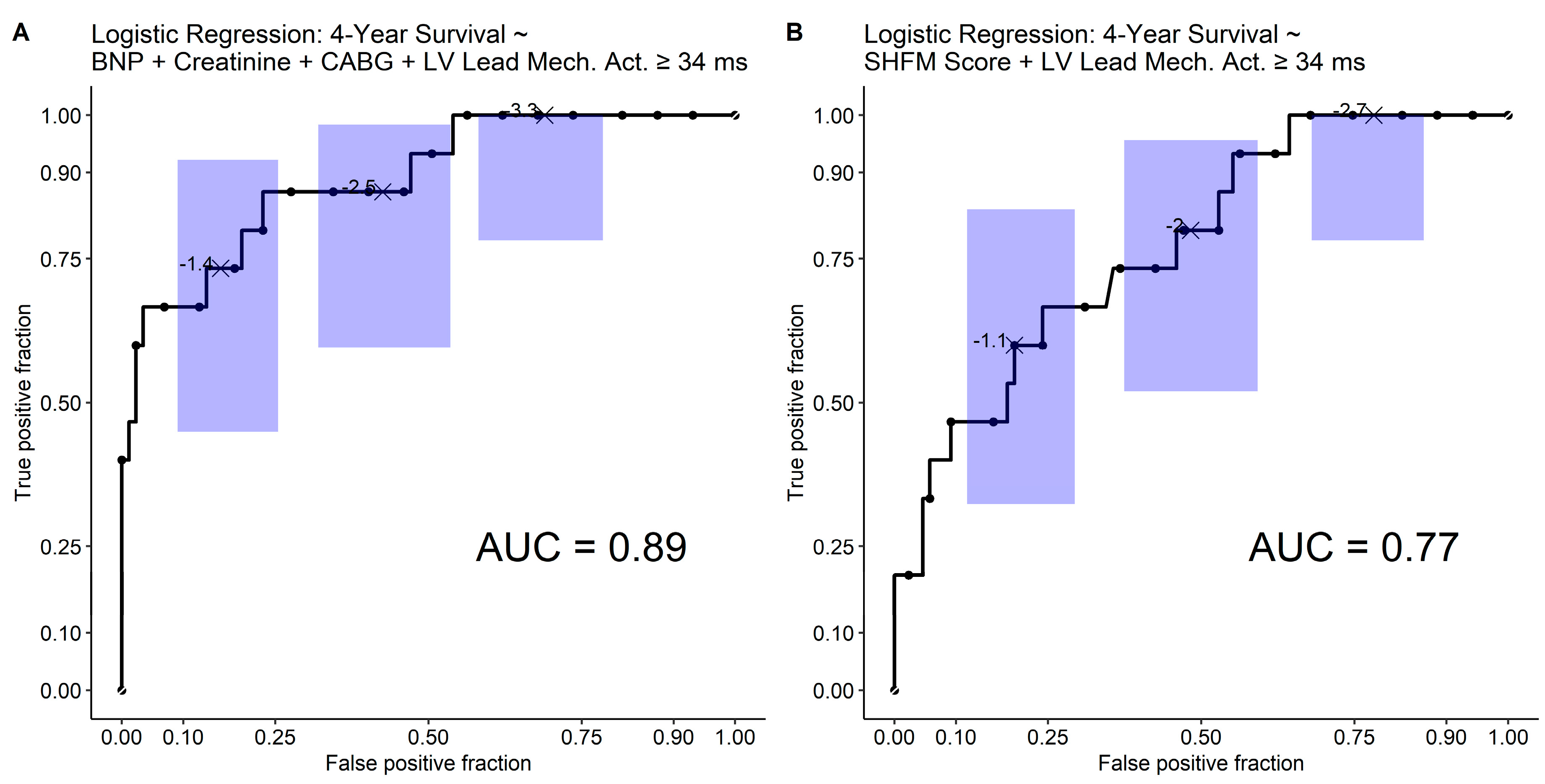
3.4. L1-Regularization for Selection of Covariates Associated with Survival
3.5. Training and Test Sets with Standard Logistic Regression
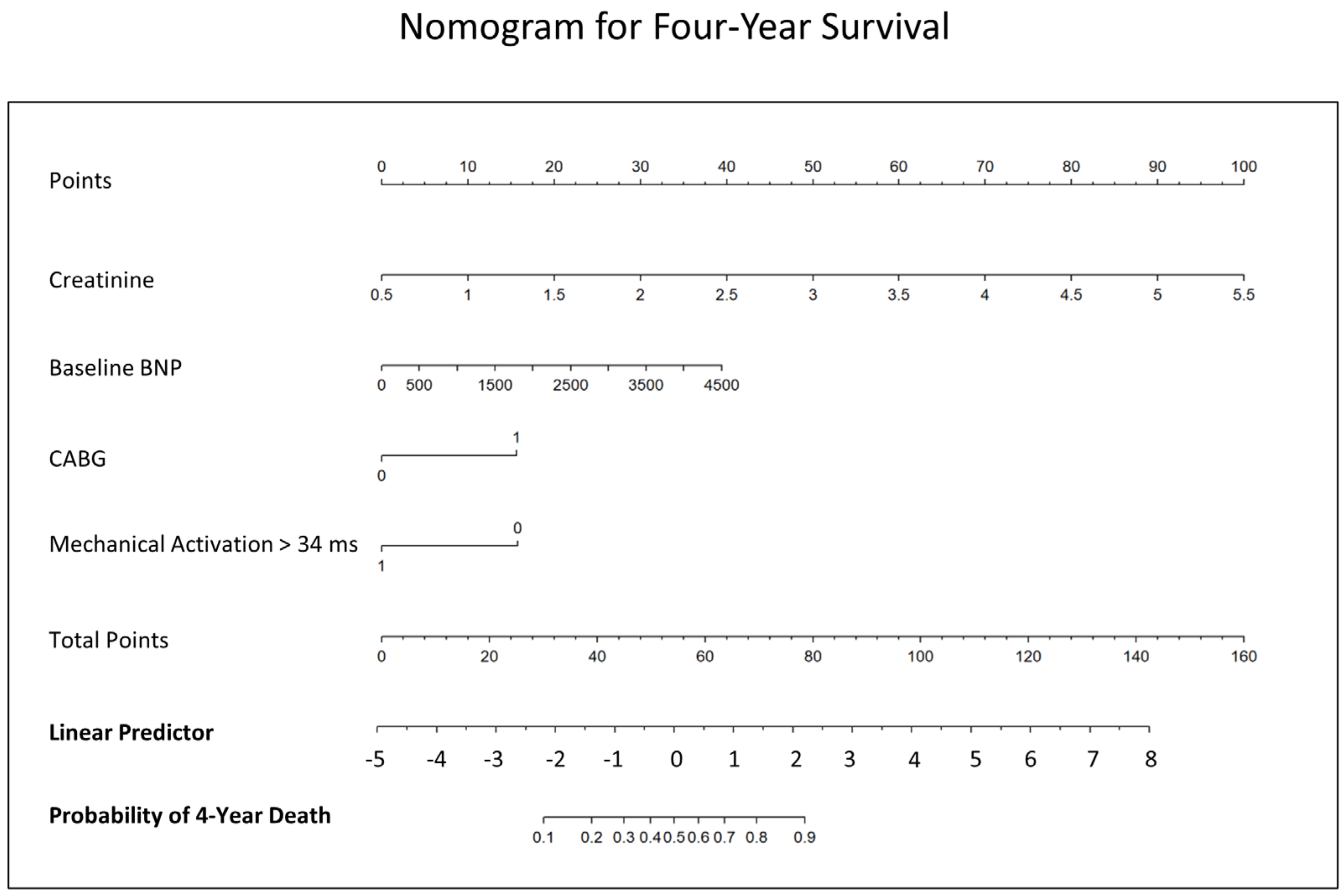
3.6. Receiver Operating Characteristic Analysis and Nomogram
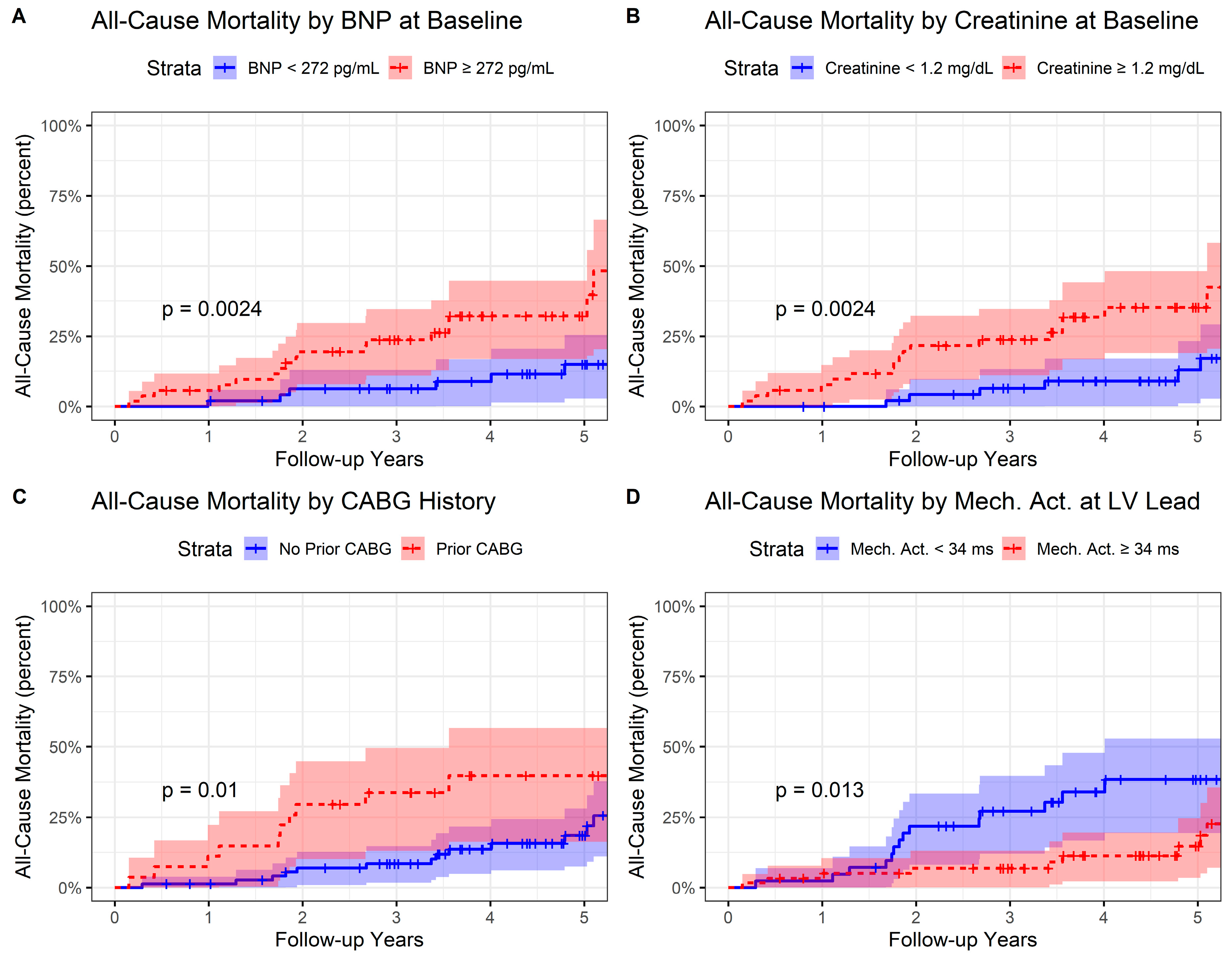
3.7. Kaplan–Meier Analysis and Cox Proportional Hazards Analysis
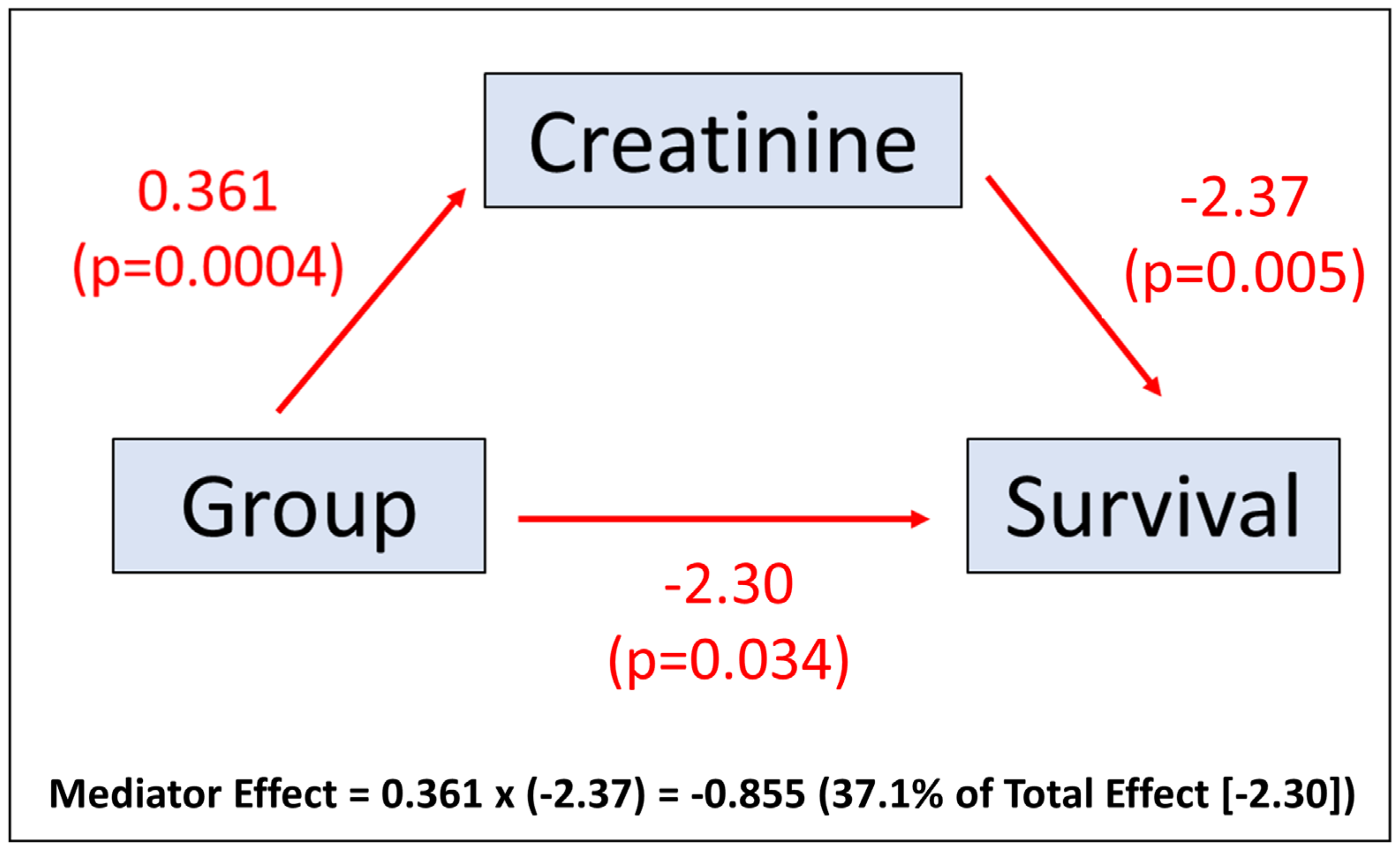
3.8. Mediation Effects
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Greenspon, A.J.; Patel, J.D.; Lau, E.; Frisch, D.; Ho, R.; Pavri, B.; Ochoa, J.; Kurtz, S. Trends in permanent pacemaker implantation in the United States from 1993 to 2009: Increasing complexity of patients and procedures. J. Am. Coll. Cardiol. 2012, 60, 1540–1545. [Google Scholar] [CrossRef]
- Bristow, M.R.; Feldman, A.M.; Saxon, L.A. Heart failure management using implantable devices for ventricular resynchronization: Comparison of Medical Therapy, Pacing, and Defibrillation in Chronic Heart Failure (COMPANION) trial. J. Card. Fail. 2000, 6, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Butter, C.; Auricchio, A.; Stellbrink, C.; Fleck, E.; Ding, J.; Yu, Y.; Huvelle, E.; Spinelli, J.; on behalf of the Pacing Therapy for Chronic Heart Failure II (PATH-CHF-II) Study Group. Effect of resynchronization therapy stimulation site on the systolic function of heart failure patients. Circulation 2001, 104, 3026–3029. [Google Scholar] [CrossRef] [PubMed]
- Auricchio, A.; Stellbrink, C.; Sack, S.; Block, M.; Vogt, J.; Bakker, P.; Huth, C.; Schöndube, F.; Wolfhard, U.; Böcker, D.; et al. Long-term clinical effect of hemodynamically optimized cardiac resynchronization therapy in patients with heart failure and ventricular conduction delay. J. Am. Coll. Cardiol. 2002, 39, 2026–2033. [Google Scholar] [CrossRef] [PubMed]
- Abraham, W.T.; Fisher, W.G.; Smith, A.L.; Delurgio, D.B.; Leon, A.R.; Loh, E.; Kocovic, D.Z.; Packer, M.; Clavell, A.L.; Hayes, D.L.; et al. Cardiac resynchronization in chronic heart failure. N. Engl. J. Med. 2002, 346, 1845–1853. [Google Scholar] [CrossRef]
- Higgins, S.L.; Hummel, J.D.; Niazi, I.K.; Giudici, M.C.; Worley, S.J.; A Saxon, L.; Boehmer, J.P.; Higginbotham, M.B.; De Marco, T.; Foster, E.; et al. Cardiac resynchronization therapy for the treatment of heart failure in patients with intraventricular conduction delay and malignant ventricular tachyarrhythmias. J. Am. Coll. Cardiol. 2003, 42, 1454–1459. [Google Scholar] [CrossRef]
- Young, J.B.; Abraham, W.T.; Smith, A.L.; Leon, A.R.; Lieberman, R.; Wilkoff, B.; Canby, R.C.; Schroeder, J.S.; Liem, L.B.; Hall, S.; et al. Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: The MIRACLE ICD Trial. JAMA 2003, 289, 2685–2694. [Google Scholar] [CrossRef]
- Bristow, M.R.; Saxon, L.A.; Boehmer, J.; Krueger, S.; Kass, D.A.; De Marco, T.; Carson, P.; DiCarlo, L.; DeMets, D.; White, B.G.; et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N. Engl. J. Med. 2004, 350, 2140–2150. [Google Scholar] [CrossRef]
- Ellenbogen, K.A. Clinical Cardiac Pacing, Defibrillation, and Resynchronization Therapy, 5th ed.; Elsevier: Amsterdam, The Netherlands, 2017. [Google Scholar]
- Cleland, J.G.; Daubert, J.C.; Erdmann, E.; Freemantle, N.; Gras, D.; Kappenberger, L.; Tavazzi, L. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N. Engl. J. Med. 2005, 352, 1539–1549. [Google Scholar] [CrossRef]
- Sutton, M.G.; Plappert, T.; Hilpisch, K.E.; Abraham, W.T.; Hayes, D.L.; Chinchoy, E. Sustained reverse left ventricular structural remodeling with cardiac resynchronization at one year is a function of etiology: Quantitative Doppler echocardiographic evidence from the Multicenter InSync Randomized Clinical Evaluation (MIRACLE). Circulation 2006, 113, 266–272. [Google Scholar] [CrossRef]
- Shimano, M.; Tsuji, Y.; Yoshida, Y.; Inden, Y.; Tsuboi, N.; Itoh, T.; Suzuki, H.; Muramatsu, T.; Okada, T.; Harata, S.; et al. Acute and chronic effects of cardiac resynchronization in patients developing heart failure with long-term pacemaker therapy for acquired complete atrioventricular block. Europace 2007, 9, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Gilliam, F.R., 3rd; Kaplan, A.J.; Black, J.; Chase, K.J.; Mullin, C.M. Changes in heart rate variability, quality of life, and activity in cardiac resynchronization therapy patients: Results of the HF-HRV registry. Pacing Clin. Electrophysiol. 2007, 30, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Lindenfeld, J.; Feldman, A.M.; Saxon, L.; Boehmer, J.; Carson, P.; Ghali, J.K.; Anand, I.; Singh, S.; Steinberg, J.S.; Jaski, B.; et al. Effects of cardiac resynchronization therapy with or without a defibrillator on survival and hospitalizations in patients with New York Heart Association class IV heart failure. Circulation 2007, 115, 204–212. [Google Scholar] [CrossRef] [PubMed]
- De Marco, T.; Wolfel, E.; Feldman, A.M.; Lowes, B.; Higginbotham, M.B.; Ghali, J.K.; Wagoner, L.; Kirlin, P.C.; Kennett, J.D.; Goel, S.; et al. Impact of cardiac resynchronization therapy on exercise performance, functional capacity, and quality of life in systolic heart failure with QRS prolongation: COMPANION trial sub-study. J. Card. Fail. 2008, 14, 9–18. [Google Scholar] [CrossRef]
- Linde, C.; Abraham, W.T.; Gold, M.R.; Sutton, M.S.J.; Ghio, S.; Daubert, C.; REVERSE (REsynchronization reVErses Remodeling in Systolic left vEntricular dysfunction) Study Group. Randomized trial of cardiac resynchronization in mildly symptomatic heart failure patients and in asymptomatic patients with left ventricular dysfunction and previous heart failure symptoms. J. Am. Coll. Cardiol. 2008, 52, 1834–1843. [Google Scholar] [CrossRef]
- Moss, A.J.; Hall, W.J.; Cannom, D.S.; Klein, H.; Brown, M.W.; Daubert, J.P.; Estes, N.A.M., III; Foster, E.; Greenberg, H.; Higgins, S.L.; et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N. Engl. J. Med. 2009, 361, 1329–1338. [Google Scholar] [CrossRef]
- Tang, A.S.; Wells, G.A.; Talajic, M.; Arnold, M.O.; Sheldon, R.; Connolly, S.; Hohnloser, S.H.; Nichol, G.; Birnie, D.H.; Sapp, J.L.; et al. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N. Engl. J. Med. 2010, 363, 2385–2395. [Google Scholar] [CrossRef]
- Ellenbogen, K.A.; Gold, M.R.; Meyer, T.E.; Lozano, I.F.; Mittal, S.; Waggoner, A.D.; Lemke, B.; Singh, J.P.; Spinale, F.G.; Van Eyk, J.E.; et al. Primary results from the SmartDelay determined AV optimization: A comparison to other AV delay methods used in cardiac resynchronization therapy (SMART-AV) trial: A randomized trial comparing empirical, echocardiography-guided, and algorithmic atrioventricular delay programming in cardiac resynchronization therapy. Circulation 2010, 122, 2660–2668. [Google Scholar] [CrossRef]
- Theuns, D.A.; Smith, T.; Hunink, M.G.; Bardy, G.H.; Jordaens, L. Effectiveness of prophylactic implantation of cardioverter-defibrillators without cardiac resynchronization therapy in patients with ischaemic or non-ischaemic heart disease: A systematic review and meta-analysis. Europace 2010, 12, 1564–1570. [Google Scholar] [CrossRef]
- Curtis, A.B.; Worley, S.J.; Chung, E.S.; Li, P.; Christman, S.A.; St. John Sutton, M. Improvement in Clinical Outcomes with Biventricular Versus Right Ventricular Pacing: The BLOCK HF Study. J. Am. Coll. Cardiol. 2016, 67, 2148–2157. [Google Scholar] [CrossRef]
- Schwertner, W.R.; Behon, A.; Merkel, E.D.; Tokodi, M.; Kovács, A.; Zima, E.; Osztheimer, I.; Molnár, L.; Király, Á.; Papp, R.; et al. Long-term survival following upgrade compared with de novo cardiac resynchronization therapy implantation: A single-centre, high-volume experience. Europace 2021, 23, 1310–1318. [Google Scholar] [CrossRef] [PubMed]
- Vamos, M.; Erath, J.W.; Bari, Z.; Vagany, D.; Linzbach, S.P.; Burmistrava, T.; Israel, C.W.; Duray, G.Z.; Hohnloser, S.H. Effects of Upgrade Versus De Novo Cardiac Resynchronization Therapy on Clinical Response and Long-Term Survival: Results from a Multicenter Study. Circ. Arrhythm. Electrophysiol. 2017, 10, e004471. [Google Scholar] [CrossRef]
- Wokhlu, A.; Rea, R.F.; Asirvatham, S.J.; Webster, T.; Brooke, K.; Hodge, D.O.; Wiste, H.J.; Dong, Y.; Hayes, D.L.; Cha, Y.-M. Upgrade and de novo cardiac resynchronization therapy: Impact of paced or intrinsic QRS morphology on outcomes and survival. Heart Rhythm. 2009, 6, 1439–1447. [Google Scholar] [CrossRef] [PubMed]
- Kanai, M.; Yagishita, D.; Shoda, M.; Ejima, K.; Hagiwara, N. Clinical outcomes of upgrade to versus de novo cardiac resynchronization therapy in mild heart failure patients with atrioventricular block. J. Cardiol. 2022, 79, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Nazarian, S.; Hansford, R.; Rahsepar, A.A.; Weltin, V.; McVeigh, D.; Ipek, E.G.; Kwan, A.; Berger, R.D.; Calkins, H.; Lardo, A.C.; et al. Safety of Magnetic Resonance Imaging in Patients with Cardiac Devices. N. Engl. J. Med. 2017, 377, 2555–2564. [Google Scholar] [CrossRef]
- Russo, R.J.; Costa, H.S.; Silva, P.D.; Anderson, J.L.; Arshad, A.; Biederman, R.W.; Boyle, N.G.; Frabizzio, J.V.; Birgersdotter-Green, U.; Higgins, S.L.; et al. Assessing the Risks Associated with MRI in Patients with a Pacemaker or Defibrillator. N. Engl. J. Med. 2017, 376, 755–764. [Google Scholar] [CrossRef]
- McCrohon, J.A.; Moon, J.C.C.; Prasad, S.K.; McKenna, W.; Lorenz, C.; Coats, A.; Pennell, D. Differentiation of heart failure related to dilated cardiomyopathy and coronary artery disease using gadolinium-enhanced cardiovascular magnetic resonance. Circulation 2003, 108, 54–59. [Google Scholar] [CrossRef]
- Senthilkumar, A.; Majmudar, M.D.; Shenoy, C.; Kim, H.W.; Kim, R.J. Identifying the etiology: A systematic approach using delayed-enhancement cardiovascular magnetic resonance. Heart Fail. Clin. 2009, 5, 349–367. [Google Scholar] [CrossRef]
- Bilchick, K.C.; Kuruvilla, S.; Hamirani, Y.S.; Ramachandran, R.; Clarke, S.A.; Parker, K.M.; Stukenborg, G.J.; Mason, P.; Ferguson, J.D.; Moorman, J.R.; et al. Impact of mechanical activation, scar, and electrical timing on cardiac resynchronization therapy response and clinical outcomes. J. Am. Coll. Cardiol. 2014, 63, 1657–1666. [Google Scholar] [CrossRef]
- Bivona, D.J.; Tallavajhala, S.; Abdi, M.; Oomen, P.J.; Gao, X.; Malhotra, R.; Darby, A.E.; Monfredi, O.J.; Mangrum, J.M.; Mason, P.K.; et al. Machine learning for multidimensional response and survival after cardiac resynchronization therapy using features from cardiac magnetic resonance. Heart Rhythm. O2 2022, 3, 542–552. [Google Scholar] [CrossRef]
- Epstein, A.E.; DiMarco, J.P.; Ellenbogen, K.A.; Estes, N.M., III; Freedman, R.A.; Gettes, L.S.; Gillinov, A.M.; Gregoratos, G.; Hammill, S.C.; Hayes, D.L.; et al. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2013, 61, e6–e75. [Google Scholar] [PubMed]
- Levy, W.C.; Mozaffarian, D.; Linker, D.T.; Sutradhar, S.C.; Anker, S.D.; Cropp, A.B.; Anand, I.; Maggioni, A.; Burton, P.; Sullivan, M.D.; et al. The Seattle Heart Failure Model: Prediction of survival in heart failure. Circulation 2006, 113, 1424–1433. [Google Scholar] [CrossRef]
- Do, D.H.; Eyvazian, V.; Bayoneta, A.J.; Hu, P.; Finn, J.P.; Bradfield, J.S.; Shivkumar, K.; Boyle, N.G. Cardiac magnetic resonance imaging using wideband sequences in patients with nonconditional cardiac implanted electronic devices. Heart Rhythm. 2018, 15, 218–225. [Google Scholar] [CrossRef]
- Mangion, K.; Carrick, D.; Carberry, J.; Mahrous, A.; McComb, C.; Oldroyd, K.G.; Eteiba, H.; Lindsay, M.; McEntegart, M.; Hood, S.; et al. Circumferential strain predicts major adverse cardiovascular events following an acute ST-segment-elevation myocardial infarction. Radiology 2019, 290, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Sun, C.; Ghadimi, S.; Auger, D.C.; Croisille, P.; Viallon, M.; Mangion, K.; Berry, C.; Haggerty, C.M.; Jing, L.; et al. StrainNet: Improved Myocardial Strain Analysis of Cine MRI by Deep Learning from DENSE. Radiol. Cardiothorac. Imaging 2023, 5, e220196. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, R.; Chen, X.; Kramer, C.M.; Epstein, F.H.; Bilchick, K.C. Singular value decomposition applied to cardiac strain from MR imaging for selection of optimal cardiac resynchronization therapy candidates. Radiology 2015, 275, 413–420. [Google Scholar] [CrossRef]
- Auger, D.A.; Bilchick, K.C.; Gonzalez, J.A.; Cui, S.X.; Holmes, J.W.; Kramer, C.M.; Salerno, M.; Epstein, F.H. Imaging left-ventricular mechanical activation in heart failure patients using cine DENSE MRI: Validation and implications for cardiac resynchronization therapy. J. Magn. Reson. Imaging 2017, 46, 887–896. [Google Scholar] [CrossRef]
- Parker, K.M.; Bunting, E.; Malhotra, R.; Clarke, S.A.; Mason, P.; Darby, A.E.; Kramer, C.M.; Salerno, M.; Holmes, J.W.; Bilchick, K.C. Postprocedure mapping of cardiac resynchronization lead position using standard fluoroscopy systems: Implications for the nonresponder with scar. Pacing Clin. Electrophysiol. 2014, 37, 757–767. [Google Scholar] [CrossRef]
- Albertsen, A.E.; Nielsen, J.C.; Pedersen, A.K.; Hansen, P.S.; Jensen, H.K.; Mortensen, P.T. Left ventricular lead performance in cardiac resynchronization therapy: Impact of lead localization and complications. Pacing Clin. Electrophysiol. 2005, 28, 483–488. [Google Scholar] [CrossRef]
- Rabbat, M.G.; Kwong, R.Y.; Heitner, J.F.; Young, A.A.; Shanbhag, S.M.; Petersen, S.E.; Selvanayagam, J.B.; Berry, C.; Nagel, E.; Heydari, B.; et al. The Future of Cardiac Magnetic Resonance Clinical Trials. JACC Cardiovasc. Imaging 2022, 15, 2127–2138. [Google Scholar] [CrossRef]
- Tibshirani, R. Regression Shrinkage and Selection via the Lasso. J. R. Stat. Soc. 1996, 58, 267–288. [Google Scholar] [CrossRef]
- Merkely, B.; Hatala, R.; Wranicz, J.K.; Duray, G.; Földesi, C.; Som, Z.; Németh, M.; Goscinska-Bis, K.; Gellér, L.; Zima, E.; et al. Upgrade of right ventricular pacing to cardiac resynchronisation therapy in heart failure: A randomised trial. Eur. Heart J. 2023, ehad591. [Google Scholar] [CrossRef] [PubMed]



| All (N = 102) | De Novo CRT (N = 50) | CRT Upgrade with RVP (N = 29) | CRT Upgrade w/o RVP (N = 23) | p Value (All Groups) | p Value (Group 1 vs. 2) | |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age, years | 66.5 (58.3–72.9) | 65.4 (60.4–70.8) | 74.0 (64.0–79.0) | 62.0 (56.0–70.0) | 0.02 | 0.03 |
| BMI, kg/m2 | 28.3 (24.2–33.2) | 28.0 (24.0–31.7) | 28.2 (23.3–33.1) | 29.1 (25.4–35.5) | 0.8 | |
| Weight, kg | 85.3 (75.3–103.0) | 82.6 (73.6–99.8) | 91.6 (73.9–103.0) | 93.8 (80.2–103.9) | 0.5 | |
| Female | 24 (23.5) | 15 (30.0) | 3 (10.3) | 6 (26.1) | 0.1 | |
| NYHA Heart Failure Class | <0.0001 | <0.0001 | ||||
| II | 35 (34.3) | 3 (6.0) | 18 (62.1) | 14 (60.9) | ||
| III | 67 (65.7) | 47 (94.0) | 11 (37.9) | 9 (39.1) | ||
| Race | 0.5 | |||||
| Black | 16 (15.7) | 6 (12.0) | 5 (17.2) | 5 (21.7) | ||
| White/Other | 86 (84.3) | 44 (88.0) | 24 (82.8) | 18 (78.3) | ||
| SHFM Score | 0.38 (0.005–0.81) | 0.55 (0.22–0.89) | 0.19 (−0.01–0.79) | 0.2 (−0.015–0.41) | 0.1 | |
| Comorbid Conditions | ||||||
| Ischemic Cardiomyopathy | 49 (48.0) | 23 (46.0) | 11 (37.9) | 15 (65.2) | 0.1 | |
| Atrial Fibrillation | 33 (32.4) | 11 (22.0) | 18 (62.1) | 4 (17.4) | 0.0004 | 0.0006 |
| Chronic Kidney Disease | 36 (35.3) | 14 (28.0) | 14 (48.3) | 8 (34.8) | 0.2 | |
| Prior CABG | 27 (26.5) | 11 (22.0) | 7 (24.1) | 9 (39.1) | 0.3 | |
| Medications | ||||||
| Beta-Blocker | 96 (94.1) | 49 (98.0) | 25 (86.2) | 22 (95.7) | 0.07 | |
| ACE Inhibitor/ARB | 85 (83.3) | 46 (92.0) | 19 (65.5) | 20 (87.0) | 0.01 | 0.005 |
| Loop Diuretic | 79 (77.5) | 40 (80.0) | 18 (62.1) | 21 (91.3) | 0.04 | 0.1 |
| Statin | 67 (65.7) | 28 (56.0) | 19 (65.5) | 20 (87.0) | 0.04 | 0.5 |
| Laboratory Studies, Vital Signs & Exercise Testing | ||||||
| Systolic BP, mmHg | 118.5 (102.0–130.0) | 118.0 (108.0–129.8) | 127.0 (110.0–138.0) | 107.0 (96.5–120.0) | 0.01 | 0.2 |
| Sodium, mEq/L | 138.0 (136.3–140.0) | 138.0 (137.0–139.8) | 139.0 (138.0–141.0) | 137.0 (136.0–139.0) | 0.1 | |
| Creatinine, mg/dL | 1.2 (0.96–1.4) | 1.05 (0.9–1.3) | 1.3 (1.2–1.6) | 1.1 (0.95–1.4) | 0.004 | 0.002 |
| Hemoglobin, g/dL | 13.3 (12.3–14.5) | 13.6 (12.3–14.4) | 13.1 (12.3–14.5) | 13.1 (12.4–14.6) | 0.9 | |
| GFR, mL/min/1.72 m2 | 64.1 (51.5–82.6) | 72.2 (59.1–87.0) | 58.0 (43.0–74.0) | 63.0 (54.0–77.0) | 0.02 | 0.006 |
| BNP, pg/mL | 272.0 (137.3–752.8) | 210.5 (118.3–699.0) | 272.0 (124.0–879.0) | 304.0 (262.0–642.0) | 0.2 | |
| Peak VO2, mL/kg/min | 0.075 (−0.88–1.4) | 14.3 (12.2–16.1) | 14.4 (13.4–14.8) | 14.4 (12.7–14.6) | 0.9 | |
| CMR/Echocardiography Assessment Parameters | ||||||
| LVEF, % | 23.7 (17.4–29.8) | 23.2 (18.9–28.0) | 29.0 (20.0–35.0) | 19.0 (16.5–26.0) | 0.02 | 0.06 |
| LVEDVI, mL/m2 | 127.9 (104.8–165.0) | 133.7 (112.2–170.2) | 102.0 (77.4–115.0) | 152.0 (126.2–183.5) | <0.0001 | 0.0002 |
| LVESVI, mL/m2 | 97.2 (73.6–127.0) | 101.2 (84.9–134.9) | 71.3 (49.9–90.4) | 117.0 (95.9–148.5) | <0.0001 | 0.0005 |
| RVEF, % | 36.1 (26.0–45.5) | 36.1 (24.4–48.7) | 37.5 (32.0–44.6) | 35.1 (27.8–40.1) | 0.7 | |
| RVEDVI, mL/m2 | 65.8 (55.3–83.7) | 66.0 (53.5–81.2) | 65.3 (55.5–86.9) | 65.8 (57.3–79.3) | 0.9 | |
| RVESVI, mL/m2 | 40.2 (32.7–55.2) | 42.0 (31.8–57.7) | 38.7 (31.6–52.8) | 39.6 (38.1–50.3) | 0.9 | |
| LGE Presence | 55 (53.9) | 27 (54.0) | 14 (48.3) | 14 (60.9) | 0.7 | |
| CURE-SVD | 0.57 (0.45–0.72) | 0.60 (0.45–0.78) | 0.55 (0.50–0.69) | 0.55 (0.37–0.67) | 0.4 | |
| Scar at LV Free Wall | 29 (28.4) | 15 (30.0) | 5 (17.2) | 9 (39.1) | 0.2 | |
| Electrical Parameters | ||||||
| Paced QRS | 31 (30.4) | 0 (0.0) | 29 (100.0) | 0 (0.0) | <0.0001 | <0.0001 |
| QRS, ms | 161.0 (147.0–180.0) | 160.0 (146.3–180.0) | 179.0 (164.0–200.0) | 152.0 (136.0–168.0) | 0.0004 | 0.002 |
| QLV, ms | 130.0 (98.0–154.3) | 112.5 (81.3–140.0) | 160.0 (150.0–172.0) | 108.0 (99.0–127.0) | <0.0001 | <0.0001 |
| QLV/QRS Ratio | 0.78 (0.67–0.89) | 0.74 (0.58–0.81) | 0.89 (0.84–0.96) | 0.76 (0.69–0.79) | <0.0001 | <0.001 |
| LBBB | 67 (65.7) | 48 (96.0) | 0 (0) | 16 (69.6) | <0.0001 | <0.0001 |
| RBBB | 7 (6.9) | 3 (6.0) | 0 (0) | 3 (13.0) | 0.5 | |
| TOS at LV Lead, ms | 87.5 (69.0–114.8) | 106.0 (72.3–118.0) | 86.0 (66.0–107.0) | 78.0 (68.0–96.5) | 0.06 | 0.1 |
| TOS at Latest Activated LV Segment, ms | 119.5 (101.0–136.0) | 124.0 (97.3–136.0) | 112.0 (100.0–134.0) | 119.0 (104.0–141.0) | 0.7 | |
| Response Measures at 6 Months Post-CRT | ||||||
| Fractional Change in LVESVI | −0.2 (−0.32–−0.08) | −0.18 (−0.36–−0.023) | −0.21 (−0.36–−0.09) | −0.2 (−0.265–−0.135) | 0.7 | |
| BNP, pg/mL | 172.5 (63.8–442.8) | 132.5 (51.8–451.8) | 172.5 (70.0–526.0) | 195.0 (150.5–238.0) | 0.6 | |
| Change in Peak VO2, mL/kg/min | 0.075 (−0.88–1.37) | 0.40 (−1.5–2.3) | −0.26 (−0.9–0.4) | 0.075 (−0.03–0.3) | 0.3 | |
| Survival Status at 4 Years | 0.2 | |||||
| Alive | 83 (81.4) | 44 (88.0) | 21 (72.4) | 18 (78.2) | ||
| Dead | 19 (18.6) | 6 (12.0) | 8 (27.6) | 5 (21.8) |
| De Novo CRT (N = 50) | CRT Upgrade with RVP (N = 29) | CRT Upgrade w/o RVP (N = 23) | p Value (All Groups) | p Value (Group 1 vs. 2) | |
|---|---|---|---|---|---|
| LV Lead Location | |||||
| Longitudinal | 0.4 | ||||
| Basal | 9 (18.0) | 7 (24.1) | 9 (39.1) | ||
| Mid-ventricular | 29 (58.0) | 17 (58.6) | 11 (47.8) | ||
| Apical | 12 (24.0) | 5 (17.2) | 3 (13.0) | ||
| Circumferential | 0.6 | ||||
| Anterior | 8 (16.0) | 1 (3.4) | 2 (8.7) | ||
| Anteroseptal | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Inferoseptal | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Inferior | 1 (2.0) | 0 (0.0) | 1 (4.3) | ||
| Inferolateral | 12 (24.0) | 7 (24.1) | 5 (21.7) | ||
| Anterolateral | 29 (58) | 21 (72.4) | 15 (65.2) | ||
| Location of Latest Mechanical Activation | |||||
| Longitudinal | <0.0001 | ||||
| Basal | 14 (28.0) | 25 (86.2) | 16 (69.6) | <0.0001 | <0.0001 |
| Mid-ventricular | 31 (62.0) | 4 (13.8) | 6 (26.1) | <0.0001 | <0.0001 |
| Apical | 5 (10.0) | 0 (0.0) | 1 (4.3) | 0.6 | |
| Circumferential | 0.003 | ||||
| Anterior | 5 (10.0) | 14 (48.3) | 9 (39.1) | 0.0002 | 0.0002 |
| Anteroseptal | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Inferoseptal | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Inferior | 1 (2.0) | 1 (3.4) | 1 (4.3) | 0.8 | |
| Inferolateral | 17 (34.0) | 2 (6.9) | 7 (30.4) | 0.02 | 0.007 |
| Anterolateral | 27 (54) | 12 (41.4) | 6 (26.1) | 0.08 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bivona, D.J.; Oomen, P.J.A.; Wang, Y.; Morales, F.L.; Abdi, M.; Gao, X.; Malhotra, R.; Darby, A.; Mehta, N.; Monfredi, O.J.; et al. Cardiac Magnetic Resonance, Electromechanical Activation, Kidney Function, and Natriuretic Peptides in Cardiac Resynchronization Therapy Upgrades. J. Cardiovasc. Dev. Dis. 2023, 10, 409. https://doi.org/10.3390/jcdd10100409
Bivona DJ, Oomen PJA, Wang Y, Morales FL, Abdi M, Gao X, Malhotra R, Darby A, Mehta N, Monfredi OJ, et al. Cardiac Magnetic Resonance, Electromechanical Activation, Kidney Function, and Natriuretic Peptides in Cardiac Resynchronization Therapy Upgrades. Journal of Cardiovascular Development and Disease. 2023; 10(10):409. https://doi.org/10.3390/jcdd10100409
Chicago/Turabian StyleBivona, Derek J., Pim J. A. Oomen, Yu Wang, Frances L. Morales, Mohamad Abdi, Xu Gao, Rohit Malhotra, Andrew Darby, Nishaki Mehta, Oliver J. Monfredi, and et al. 2023. "Cardiac Magnetic Resonance, Electromechanical Activation, Kidney Function, and Natriuretic Peptides in Cardiac Resynchronization Therapy Upgrades" Journal of Cardiovascular Development and Disease 10, no. 10: 409. https://doi.org/10.3390/jcdd10100409
APA StyleBivona, D. J., Oomen, P. J. A., Wang, Y., Morales, F. L., Abdi, M., Gao, X., Malhotra, R., Darby, A., Mehta, N., Monfredi, O. J., Mangrum, J. M., Mason, P. K., Levy, W. C., Mazimba, S., Patel, A. R., Epstein, F. H., & Bilchick, K. C. (2023). Cardiac Magnetic Resonance, Electromechanical Activation, Kidney Function, and Natriuretic Peptides in Cardiac Resynchronization Therapy Upgrades. Journal of Cardiovascular Development and Disease, 10(10), 409. https://doi.org/10.3390/jcdd10100409