Oral Frailty as a Risk Factor for Fall Incidents among Community-Dwelling People
Abstract
1. Introduction
2. Materials and Methods
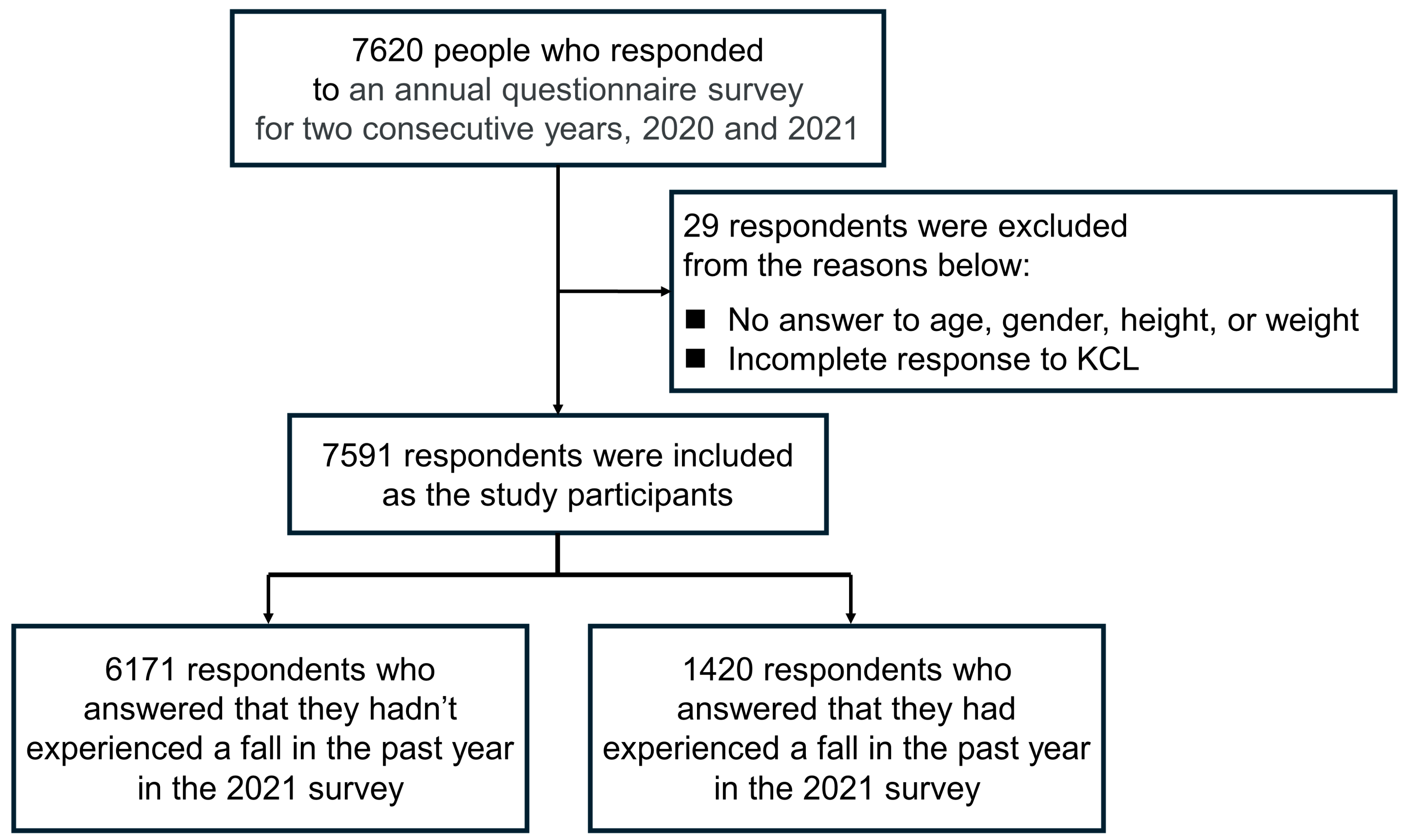
2.1. Participants
2.2. Procedure
2.3. Kihon Checklist
2.4. Other Items
2.5. Step Counts
2.6. Data Acquisition from Osaka Prefecture
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yu, W.Y.; Hwang, H.F.; Chen, C.Y.; Lin, M.R. Situational risk factors for fall-related vertebral fractures in older men and women. Osteoporos. Int. 2021, 32, 1061–1070. [Google Scholar] [CrossRef] [PubMed]
- Al-Ani, A.N.; Cederholm, T.; Saaf, M.; Neander, G.; Blomfeldt, R.; Ekstrom, W.; Hedstrom, M. Low bone mineral density and fat-free mass in younger patients with a femoral neck fracture. Eur. J. Clin. Investig. 2015, 45, 800–806. [Google Scholar] [CrossRef] [PubMed]
- Orimo, H.; Yaegashi, Y.; Hosoi, T.; Fukushima, Y.; Onoda, T.; Hashimoto, T.; Sakata, K. Hip fracture incidence in Japan: Estimates of new patients in 2012 and 25-year trends. Osteoporos. Int. 2016, 27, 1777–1784. [Google Scholar] [CrossRef] [PubMed]
- Hagino, H.; Furukawa, K.; Fujiwara, S.; Okano, T.; Katagiri, H.; Yamamoto, K.; Teshima, R. Recent trends in the incidence and lifetime risk of hip fracture in Tottori, Japan. Osteoporos. Int. 2009, 20, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Kenyon-Smith, T.; Nguyen, E.; Oberai, T.; Jarsma, R. Early Mobilization Post-Hip Fracture Surgery. Geriatr. Orthop. Surg. Rehabil. 2019, 10, 2151459319826431. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 16. Diabetes Care in the Hospital: Standards of Care in Diabetes-2024. Diabetes Care 2024, 47, S295–S306. [Google Scholar] [CrossRef] [PubMed]
- Meng, Y.; Liu, Y.; Fu, M.; Hou, Z.; Wang, Z. Clinical characteristics of elderly hip fracture patients with chronic cerebrovascular disease and construction of a clinical predictive model for perioperative pneumonia. Orthop. Traumatol. Surg. Res. 2024, 103821. [Google Scholar] [CrossRef] [PubMed]
- Government’s Industrial Accident Prevention Plan. Available online: https://www.jisha.or.jp/english/govs_plan.html (accessed on 26 February 2024).
- Social Media Posted by the Japanese Ministry of Health, Labour and Welfare. Available online: https://www.youtube.com/watch?v=VogUNCH7Oss (accessed on 26 February 2024).
- Hellyer, P. Oral frailty. Br. Dent. J. 2023, 235, 513. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.Y.; Chen, W.L. Prognostic significance of subjective oral dysfunction on the all-cause mortality. J. Oral. Rehabil. 2022, 49, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Kato, Y.; Kikutani, T.; Sagawa, K.; Tamura, F. Association between masticatory movement and oral and physical function in healthy older women. J. Prosthodont. Res. 2022, 66, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Imaoka, M.; Nakao, H.; Hida, M.; Tazaki, F.; Imai, R.; Utsunomiya, H.; Hashizume, H. Association between subjective oral dysfunction and locomotive syndrome in community-dwelling older adults. Sci. Rep. 2021, 11, 12591. [Google Scholar] [CrossRef] [PubMed]
- Moriya, S.; Tei, K.; Yamazaki, Y.; Hata, H.; Shinkai, S.; Yoshida, H.; Muramatsu, M.; Kitagawa, Y.; Inoue, N.; Yamada, H.; et al. Relationships between perceived chewing ability and muscle strength of the body among the elderly. J. Oral. Rehabil. 2011, 38, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Sheiham, A.; Steele, J.G.; Marcenes, W.; Lowe, C.; Finch, S.; Bates, C.J.; Prentice, A.; Walls, A.W. The relationship among dental status, nutrient intake, and nutritional status in older people. J. Dent. Res. 2001, 80, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Takahashi, K.; Hirano, H.; Kikutani, T.; Watanabe, Y.; Ohara, Y.; Furuya, H.; Tetsuo, T.; Akishita, M.; Iijima, K. Oral Frailty as a Risk Factor for Physical Frailty and Mortality in Community-Dwelling Elderly. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 1661–1667. [Google Scholar] [CrossRef] [PubMed]
- Murakami, M.; Hirano, H.; Watanabe, Y.; Sakai, K.; Kim, H.; Katakura, A. Relationship between chewing ability and sarcopenia in Japanese community-dwelling older adults. Geriatr. Gerontol. Int. 2015, 15, 1007–1012. [Google Scholar] [CrossRef] [PubMed]
- Padilha, D.M.; Hilgert, J.B.; Hugo, F.N.; Bos, A.J.; Ferrucci, L. Number of teeth and mortality risk in the Baltimore Longitudinal Study of Aging. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 739–744. [Google Scholar] [CrossRef] [PubMed]
- Tsai, A.C.; Chang, T.L. Association of dental prosthetic condition with food consumption and the risk of malnutrition and follow-up 4-year mortality risk in elderly Taiwanese. J. Nutr. Health Aging 2011, 15, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.S.; Huang, Y.C.; Wahlqvist, M.L. Chewing ability in conjunction with food intake and energy status in later life affects survival in Taiwanese with the metabolic syndrome. J. Am. Geriatr. Soc. 2010, 58, 1072–1080. [Google Scholar] [CrossRef]
- Alexander, B.H.; Rivara, F.P.; Wolf, M.E. The cost and frequency of hospitalization for fall-related injuries in older adults. Am. J. Public. Health 1992, 82, 1020–1023. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E. Clinical practice. Preventing falls in elderly persons. N. Engl. J. Med. 2003, 348, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Rubenstein, L.Z. Falls in older people: Epidemiology, risk factors and strategies for prevention. Age Ageing 2006, 35 (Suppl. S2), ii37–ii41. [Google Scholar] [CrossRef] [PubMed]
- Osaka Prefecture’s Health App “ASMILE”. Available online: https://www.asmile.pref.osaka.jp (accessed on 18 January 2024).
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Arai, H. Combined effect of lower muscle quality and quantity on incident falls and fall-related fractures in community-dwelling older adults: A 3-year follow-up study. Bone 2022, 162, 116474. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, M.; Yoshida, T.; Yamada, Y.; Watanabe, Y.; Nanri, H.; Yokoyama, K.; Date, H.; Miyake, M.; Itoi, A.; Yamagata, E.; et al. Sociodemographic and physical predictors of non-participation in community based physical checkup among older neighbors: A case-control study from the Kyoto-Kameoka longitudinal study, Japan. BMC Public. Health 2018, 18, 568. [Google Scholar] [CrossRef] [PubMed]
- Manual on Daily-Living Function Assessment for Long-Term Care Prevention (Revised Edition). Available online: https://www.mhlw.go.jp/topics/2009/05/dl/tp0501-1c_0001.pdf (accessed on 23 January 2024).
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Sewo Sampaio, P.Y.; Sampaio, R.A.; Yamada, M.; Arai, H. Systematic review of the Kihon Checklist: Is it a reliable assessment of frailty? Geriatr. Gerontol. Int. 2016, 16, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Arai, H.; Satake, S. English translation of the Kihon Checklist. Geriatr. Gerontol. Int. 2015, 15, 518–519. [Google Scholar] [CrossRef]
- Kusama, T.; Takeuchi, K.; Kiuchi, S.; Aida, J.; Osaka, K. Poor oral health and dementia risk under time-varying confounding: A cohort study based on marginal structural models. J. Am. Geriatr. Soc. 2023, 72, 729–741. [Google Scholar] [CrossRef] [PubMed]
- Weiner, D.K.; Duncan, P.W.; Chandler, J.; Studenski, S.A. Functional reach: A marker of physical frailty. J. Am. Geriatr. Soc. 1992, 40, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Duncan, P.W.; Studenski, S.; Chandler, J.; Prescott, B. Functional reach: Predictive validity in a sample of elderly male veterans. J. Gerontol. 1992, 47, M93–M98. [Google Scholar] [CrossRef]
- Williams, B.; Allen, B.; Hu, Z.; True, H.; Cho, J.; Harris, A.; Fell, N.; Sartipi, M. Real-Time Fall Risk Assessment Using Functional Reach Test. Int. J. Telemed. Appl. 2017, 2017, 2042974. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [PubMed]
- Kassebaum, N.J.; Smith, A.G.C.; Bernabe, E.; Fleming, T.D.; Reynolds, A.E.; Vos, T.; Murray, C.J.L.; Marcenes, W.; GBD 2015 Oral Health Collaborators. Global, Regional, and National Prevalence, Incidence, and Disability-Adjusted Life Years for Oral Conditions for 195 Countries, 1990–2015: A Systematic Analysis for the Global Burden of Diseases, Injuries, and Risk Factors. J. Dent. Res. 2017, 96, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Takata, Y.; Ansai, T.; Awano, S.; Hamasaki, T.; Yoshitake, Y.; Kimura, Y.; Sonoki, K.; Wakisaka, M.; Fukuhara, M.; Takehara, T. Relationship of physical fitness to chewing in an 80-year-old population. Oral. Dis. 2004, 10, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Kosaka, S.; Ohara, Y.; Naito, S.; Iimori, S.; Kado, H.; Hatta, T.; Yanishi, M.; Uchida, S.; Tanaka, M. Association among kidney function, frailty, and oral function in patients with chronic kidney disease: A cross-sectional study. BMC Nephrol. 2020, 21, 357. [Google Scholar] [CrossRef] [PubMed]
- Tagami, Y.; Fujimoto, K.; Goto, T.; Suito, H.; Nagao, K.; Ichikawa, T. Can Measurement of Ultrasonic Echo Intensity Predict Physical Frailty in Older Adults? Diagnostics 2023, 13, 675. [Google Scholar] [CrossRef] [PubMed]
- Long-Term Care Prevention Manual (March 2012 Revised Edition). Available online: https://www.mhlw.go.jp/topics/2009/05/tp0501-1.html (accessed on 6 March 2024).
- Azzolino, D.; Passarelli, P.C.; De Angelis, P.; Piccirillo, G.B.; D’Addona, A.; Cesari, M. Poor Oral Health as a Determinant of Malnutrition and Sarcopenia. Nutrients. 2019, 11, 2898. [Google Scholar] [CrossRef] [PubMed]
- Walls, A.W.; Steele, J.G. The relationship between oral health and nutrition in older people. Mech. Ageing Dev. 2004, 125, 853–857. [Google Scholar] [CrossRef] [PubMed]
- Moynihan, P.J.; Teo, J.L. Exploring Oral Function, Protein Intake, and Risk of Sarcopenia: A Scoping Review. JDR Clin. Trans. Res. 2024, 9, 4–20. [Google Scholar] [CrossRef] [PubMed]
- Wysokinski, A.; Sobow, T.; Kloszewska, I.; Kostka, T. Mechanisms of the anorexia of aging—A review. Age 2015, 37, 9821. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Yoshihara, A.; Miyazaki, H. Association between masticatory performance and one-leg standing time with eyes open in community-dwelling elderly women. J. Dent. Health 2012, 62, 289–295. [Google Scholar]
- Moriya, S.; Notani, K.; Miura, H.; Inoue, N. Relationship between masticatory ability and physical performance in community-dwelling edentulous older adults wearing complete dentures. Gerodontology 2014, 31, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, M.; Kikutani, T.; Okada, G.; Kawamura, T.; Kimura, M.; Akagawa, Y. The effect of tooth loss on body balance control among community-dwelling elderly persons. Int. J. Prosthodont. 2009, 22, 136–139. [Google Scholar]
- Cesanelli, L.; Cesaretti, G.; Ylaite, B.; Iovane, A.; Bianco, A.; Messina, G. Occlusal Splints and Exercise Performance: A Systematic Review of Current Evidence. Int. J. Environ. Res. Public. Health 2021, 18, 10338. [Google Scholar] [CrossRef] [PubMed]
- Miyahara, T.; Hagiya, N.; Ohyama, T.; Nakamura, Y. Modulation of human soleus H reflex in association with voluntary clenching of the teeth. J. Neurophysiol. 1996, 76, 2033–2041. [Google Scholar] [CrossRef]
- Tuncer, M.; Tucker, K.J.; Turker, K.S. Influence of tooth clench on the soleus H-reflex. Arch. Oral. Biol. 2007, 52, 374–376. [Google Scholar] [CrossRef] [PubMed]
- Phelan, E.A.; Mahoney, J.E.; Voit, J.C.; Stevens, J.A. Assessment and management of fall risk in primary care settings. Med. Clin. North Am. 2015, 99, 281–293. [Google Scholar] [CrossRef] [PubMed]
- Odhiambo, F.O.; Beynon, C.M.; Ogwang, S.; Hamel, M.J.; Howland, O.; van Eijk, A.M.; Norton, R.; Amek, N.; Slutsker, L.; Laserson, K.F.; et al. Trauma-related mortality among adults in Rural Western Kenya: Characterising deaths using data from a health and demographic surveillance system. PLoS ONE 2013, 8, e79840. [Google Scholar] [CrossRef] [PubMed]
- Moncada, L.V.V.; Mire, L.G. Preventing Falls in Older Persons. Am. Fam. Physician 2017, 96, 240–247. [Google Scholar] [PubMed]
- Park, I.S.J.; Kim, D.J. Home safety assessment for fall prevention in elderly people in a rural community. J. Korean Gerontol. Nurs. 2002, 4, 178–186. [Google Scholar]
- Huang, J.W.; Lin, Y.Y.; Wu, N.Y.; Chen, Y.C. Rural older people had lower mortality after accidental falls than non-rural older people. Clin. Interv. Aging 2017, 6, 97–102. [Google Scholar] [CrossRef]
- Japanese Cabinet Office. Survey Results on Housing and Living Environment for Elderly People. Available online: https://www8.cao.go.jp/kourei/ishiki/h17_sougou/19html/2syou-2.html (accessed on 4 April 2024).
- Talbot, L.A.; Musiol, R.J.; Witham, E.K.; Metter, E.J. Falls in young, middle-aged and older community dwelling adults: Perceived cause, environmental factors and injury. BMC Public. Health 2005, 5, 86. [Google Scholar] [CrossRef] [PubMed]
- Kool, B.; Ameratunga, S.; Jackson, R. The role of alcohol in unintentional falls among young and middle-aged adults: A systematic review of epidemiological studies. Inj. Prev. 2009, 15, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Stenbacka, M.; Jansson, B.; Leifman, A.; Romelsjo, A. Association between use of sedatives or hypnotics, alcohol consumption, or other risk factors and a single injurious fall or multiple injurious falls: A longitudinal general population study. Alcohol 2002, 28, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Callis, N. Falls prevention: Identification of predictive fall risk factors. Appl. Nurs. Res. 2016, 29, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Fuller, G.F. Falls in the elderly. Am. Fam. Physician 2000, 61, 2159–2168. [Google Scholar] [PubMed]
- Wei, Y.; Guo, X. Impact of smart device use on objective and subjective health of older adults: Findings from four provinces in China. Front. Public Health 2023, 11, 1118207. [Google Scholar] [CrossRef]


| Total | 50–59 yrs. | 60–69 yrs. | 70 or Older | p Value | ||
|---|---|---|---|---|---|---|
| n | 7591 | 3224 | 3096 | 1271 | ||
| Age | (yrs.) | 61.6 ± 7.3 | 54.5 ± 2.8 | 64.6 ± 2.8 # (95% CI: 9.9–10.2) | 72.5 ± 2.7 # (95% CI: 17.7–18.1) | <0.001 |
| (range) | 50–88 | 50–59 | 60–69 | 70–88 | ||
| Gender | (male/female) | 3021/4570 (39.8%/60.2%) | 1121/2103 (34.8%/65.2%) | 1247/1849 (40.3%/59.7%) | 653/618 (51.4%/48.6%) | <0.001 * |
| BMI | (kg/m2) | 22.4 ± 3.1 | 22.5 ± 3.4 | 22.4 ± 3.0 (95% CI: −0.3–0.1) | 22.4 ± 2.7 (95% CI: −0.3–0.2) | 0.377 |
| Number of steps | (steps/day) | 6940 ± 4383 | 6852 ± 4242 | 6956 ± 4363 (95% CI: −148–355) | 7123 ± 4767 (95% CI: −62–603) | 0.188 |
| Exercise habits | (yes/no) | 6124/1467 (80.7%/19.3%) | 2295/929 (71.2%/28.8%) | 2675/421 (86.4%/13.6%) | 1154/117 (90.8%/9.2%) | <0.001 * |
| Awareness of frailty | (do not know/have heard the word before /know a little /know well) | 3837/1305/1324/1125 (50.5%/17.2%/17.4%/14.8%) | 1801/508/507/408 (55.9%/15.8%/15.7%/12.7%) | 1505/555/556/480 (48.6%/17.9%/18.0%/15.5%) | 531/242/261/237 (41.8%/19.0%/20.5%/18.6%) | <0.001 * |
| Comprehensive frailty | (yes/no) | 2131/5460 (28.1%/71.9%) | 967/2257 (30.0%/70.0%) | 832/2264 (26.9%/73.1%) | 332/939 (26.1%/73.9%) | 0.005 * |
| Physical frailty | (yes/no) | 504/7087 (6.6%/93.4%) | 194/3030 (6.0%/94.0%) | 198/2898 (6.4%/93.6%) | 112/1159 (8.8%/91.2%) | 0.002 * |
| Oral frailty | (yes/no) | 1275/6316 (16.8%/83.2%) | 478/2746 (14.8%/85.2%) | 537/2559 (17.3%/82.7%) | 260/1011 (20.5%/79.5%) | <0.001 * |
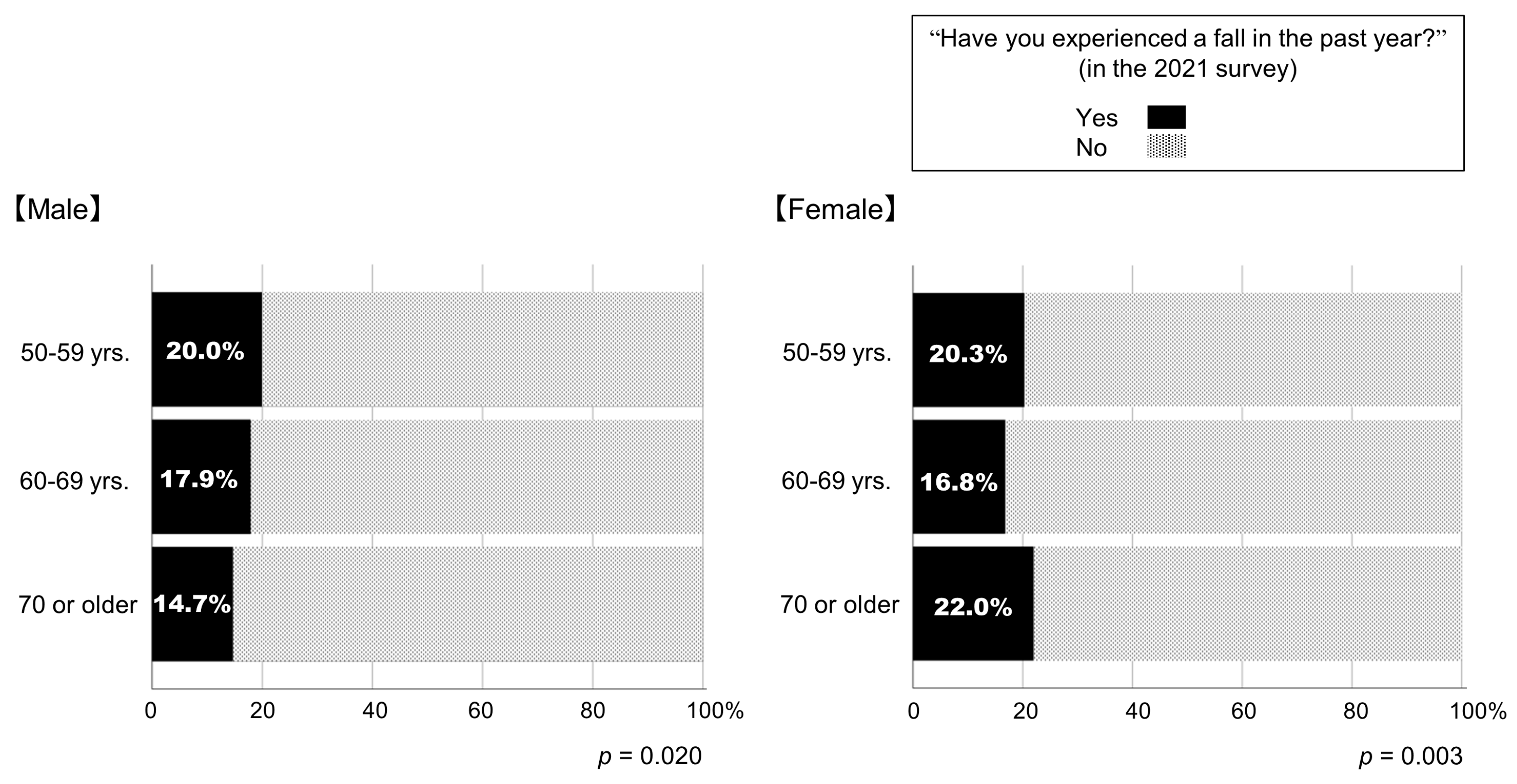
| Fall incidence in the past year | (yes/no) | 1417/6174 (18.7%/81.3%) | 651/2573 (20.2%/79.8%) | 534/2562 (17.2%/82.8%) | 232/1039 (18.3%/81.7%) | 0.010 * |
| Fall Incidents in the Past Year | |||||
|---|---|---|---|---|---|
| No (No-Fall Group) | Yes (Fall-Group) | p Value | Cohen’s d | ||
| Age | (yrs.) | 61.7 ± 7.3 | 61.2 ± 7.2 | 0.022 | −0.067 |
| Gender | (male/female) | 2478/3696 | 543/874 | 0.208 * | --- |
| BMI | (kg/m2) | 22.4 ± 3.1 | 22.6 ± 3.3 | 0.001 | 0.095 |
| Number of steps | (steps/day) | 6845 ± 4262 | 7355 ± 4858 | <0.001 | 0.117 |
| Exercise habits | (yes/no) | 5018/1156 | 1106/311 | 0.006 * | --- |
| Awareness of frailty | (do not know/have heard the word before/know a little/know well) | 3035/1082/1104/953 | 802/223/220/172 | <0.001 * | --- |
| Number of applicable items in KCL | (items/25 items) | 4.8 ± 3.0 | 6.4 ± 3.6 | <0.001 | 0.493 |
| Physical frailty | (yes/no) | 294/5880 | 210/1207 | <0.001 * | --- |
| Oral frailty | (yes/no) | 937/5237 | 338/1079 | <0.001 * | --- |
| aOR | 95% CI | p Value | ||
|---|---|---|---|---|
| Age | yrs. | 0.990 | 0.982–0.998 | 0.019 |
| Gender (female) | 1 = male, 2 = female | 1.135 | 0.998–1.290 | 0.053 |
| BMI | kg/m2 | 1.018 | 0.998–1.038 | 0.073 |
| Exercise habit | 0 = no 1 = yes | 1.010 | 0.869–1.174 | 0.897 |
| Awareness of frailty | 1 = do not know 2 = have heard the word before 3 = know a little 4 = know well | (1 as the reference) 0.801 0.799 0.754 | 0.678–0.947 0.675–0.945 0.627–0.908 | 0.009 0.009 0.003 |
| Physical frailty | 0 = no 1 = yes | 3.057 | 2.514–3.718 | <0.001 |
| Oral frailty | 0 = no 1 = yes | 1.553 | 1.342–1.797 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yokoyama, H.; Kitano, Y. Oral Frailty as a Risk Factor for Fall Incidents among Community-Dwelling People. Geriatrics 2024, 9, 54. https://doi.org/10.3390/geriatrics9020054
Yokoyama H, Kitano Y. Oral Frailty as a Risk Factor for Fall Incidents among Community-Dwelling People. Geriatrics. 2024; 9(2):54. https://doi.org/10.3390/geriatrics9020054
Chicago/Turabian StyleYokoyama, Hisayo, and Yugo Kitano. 2024. "Oral Frailty as a Risk Factor for Fall Incidents among Community-Dwelling People" Geriatrics 9, no. 2: 54. https://doi.org/10.3390/geriatrics9020054
APA StyleYokoyama, H., & Kitano, Y. (2024). Oral Frailty as a Risk Factor for Fall Incidents among Community-Dwelling People. Geriatrics, 9(2), 54. https://doi.org/10.3390/geriatrics9020054






