Impact of Antibiotics Used for Acute Aspiration Bronchitis on the Prevention of Pneumonia
Abstract
1. Introduction
2. Material and Methods
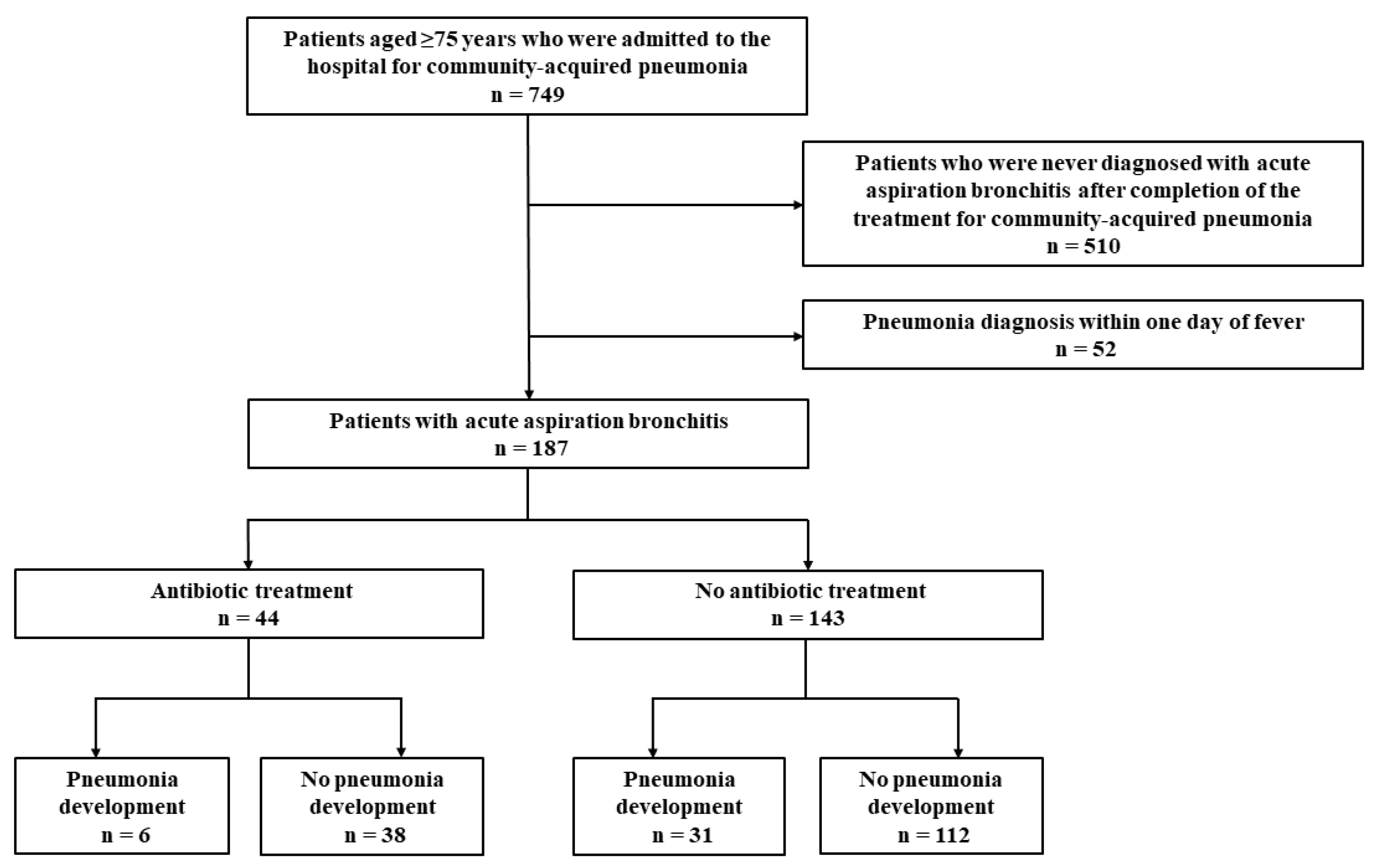
2.1. Patients and Study Design
2.2. Definitions and Outcomes
2.3. Data Collection
2.4. Statistical Analyses
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AMR | Antimicrobial resistance |
| CAP | Community-acquired pneumonia |
| CI | Confidence intervals |
| CRP | C-reactive protein |
| eGFR | Estimated glomerular filtration rate |
| WBC | White blood cell |
| WHO | World Health Organization |
References
- Neill, J.O. Antimicrobial Resistance Tackling a Crisis for the Health and Wealth of Nations; Review on Antimicrobial Resistance: London, UK, 2014. [Google Scholar]
- WHO. Global Action Plan on Antimicrobial Resistance; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Bronzwaer, S.L.; Cars, O.; Buchholz, U.; Mölstad, S.; Goettsch, W.; Veldhuijzen, I.K.; Kool, J.L.; Sprenger, M.J.; Degener, J.E. A European study on the relationship between antimicrobial use and antimicrobial resistance. Emerg. Infect. Dis. 2002, 8, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Lepper, P.M.; Grusa, E.; Reichl, H.; Högel, J.; Trautmann, M. Consumption of imipenem correlates with beta-lactam resistance in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2002, 46, 2920–2925. [Google Scholar] [CrossRef] [PubMed]
- United Nations Population Division. Available online: https://population.un.org/wpp/Graphs/DemographicProfiles/Line/900 (accessed on 21 September 2023).
- Teramoto, S.; Fukuchi, Y.; Sasaki, H.; Sato, K.; Sekizawa, K.; Matsuse, T. High incidence of aspiration pneumonia in community- and hospital-acquired pneumonia in hospitalized patients: A multicenter, prospective study in Japan. J. Am. Geriatr. Soc. 2008, 56, 577–579. [Google Scholar] [CrossRef] [PubMed]
- Komiya, K.; Ishii, H.; Kadota, J. Healthcare-associated Pneumonia and Aspiration Pneumonia. Aging Dis. 2015, 6, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Mandell, L.A.; Niederman, M.S. Aspiration Pneumonia. N. Engl. J. Med. 2019, 380, 651–663. [Google Scholar] [CrossRef] [PubMed]
- Zaloga, G.P. Aspiration-related illnesses: Definitions and diagnosis. JPEN J. Parenter. Enter. Nutr. 2002, 26, S2–S8. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, R.; Sande, M.A. Uncomplicated acute bronchitis. Ann. Intern. Med. 2000, 133, 981–991. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, R.P.; Fowler, A.A.; 3rd. Clinical practice. Acute bronchitis. N. Engl. J. Med. 2006, 355, 2125–2130. [Google Scholar] [CrossRef]
- Smith, S.M.; Fahey, T.; Smucny, J.; Becker, L.A. Antibiotics for acute bronchitis. Cochrane Database Syst. Rev. 2017, 6, Cd000245. [Google Scholar] [CrossRef]
- Gonzales, R.; Bartlett, J.G.; Besser, R.E.; Cooper, R.J.; Hickner, J.M.; Hoffman, J.R.; Sande, M.A. Principles of appropriate antibiotic use for treatment of uncomplicated acute bronchitis: Background. Ann. Emerg. Med. 2001, 37, 720–727. [Google Scholar] [CrossRef]
- Sethi, S.; Murphy, T.F. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N. Engl. J. Med. 2008, 359, 2355–2365. [Google Scholar] [CrossRef]
- Ram, F.S.; Rodriguez-Roisin, R.; Granados-Navarrete, A.; Garcia-Aymerich, J.; Barnes, N.C. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2006, 2, CD004403. [Google Scholar] [CrossRef]
- Stockley, R.A.; O’Brien, C.; Pye, A.; Hill, S.L. Relationship of sputum color to nature and outpatient management of acute exacerbations of COPD. Chest 2000, 117, 1638–1645. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, K.; Yoshii, Y.; Morozumi, M.; Chiba, N.; Ubukata, K.; Uruga, H.; Hanada, S.; Saito, N.; Kadota, T.; Wakui, H.; et al. Pathogens in COPD exacerbations identified by comprehensive real-time PCR plus older methods. Int. J. Chronic Obstruct. Pulm. Dis. 2015, 10, 2009–2016. [Google Scholar] [CrossRef]
- Yamamoto, T.; Komiya, K.; Fujita, N.; Okabe, E.; Hiramatsu, K.; Kadota, J.I. COVID-19 pandemic and the incidence of community-acquired pneumonia in elderly people. Respir. Investig. 2020, 58, 435–436. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, H.; Komiya, K.; Yamamoto, T.; Fujita, N.; Oka, H.; Okabe, E.; Yamasue, M.; Umeki, K.; Rubin, B.K.; Hiramatsu, K.; et al. Quantitative assessment of erector spinae muscles and prognosis in elderly patients with pneumonia. Sci. Rep. 2021, 11, 4319. [Google Scholar] [CrossRef] [PubMed]
- Goto, A.; Komiya, K.; Yamasue, M.; Yoshikawa, H.; Umeki, K.; Hiramatsu, K.; Kadota, J.-I. Methicillin-resistant Staphylococcus aureus among elderly patients with community-acquired pneumonia. J. Infect. Chemother. 2022, 28, 1138–1142. [Google Scholar] [CrossRef]
- Goto, A.; Komiya, K.; Umeki, K.; Hiramatsu, K.; Kadota, J.I. Impact of Pseudomonas aeruginosa coverage on the prognosis of elderly patients with community-acquired pneumonia. J. Infect. Chemother. 2023, 29, 55–60. [Google Scholar] [CrossRef]
- Mandell, L.A.; Wunderink, R.G.; Anzueto, A.; Bartlett, J.G.; Campbell, G.D.; Dean, N.C.; Dowell, S.F.; File, T.M., Jr.; Musher, D.M.; Niederman, M.S.; et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. 2007, 44 (Suppl. S2), S27–S72. [Google Scholar] [CrossRef]
- Mann, G.; Hankey, G.J. Initial clinical and demographic predictors of swallowing impairment following acute stroke. Dysphagia 2001, 16, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, S.; Imai, E.; Horio, M.; Yasuda, Y.; Tomita, K.; Nitta, K.; Yamagata, K.; Tomino, Y.; Yokoyama, H.; Hishida, A.; et al. Revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. 2009, 53, 982–992. [Google Scholar] [CrossRef]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The barthel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Granger, C.V.; Dewis, L.S.; Peters, N.C.; Sherwood, C.C.; Barrett, J.E. Stroke rehabilitation: Analysis of repeated Barthel index measures. Arch. Phys. Med. Rehabil. 1979, 60, 14–17. [Google Scholar] [PubMed]
- Silveyra, P.; Fuentes, N.; Rodriguez Bauza, D.E. Sex and Gender Differences in Lung Disease. Adv. Exp. Med. Biol. 2021, 1304, 227–258. [Google Scholar] [CrossRef] [PubMed]
- Rello, J.; Valenzuela-Sánchez, F.; Ruiz-Rodriguez, M.; Moyano, S. Sepsis: A Review of Advances in Management. Adv. Ther. 2017, 34, 2393–2411. [Google Scholar] [CrossRef]
- Lim, W.S.; van der Eerden, M.M.; Laing, R.; Boersma, W.G.; Karalus, N.; Town, G.I.; Lewis, S.; Macfarlane, J.T. Defining community acquired pneumonia severity on presentation to hospital: An international derivation and validation study. Thorax 2003, 58, 377–382. [Google Scholar] [CrossRef]
- Abisheganaden, J.; Ding, Y.Y.; Chong, W.F.; Heng, B.H.; Lim, T.K. Predicting mortality among older adults hospitalized for community-acquired pneumonia: An enhanced confusion, urea, respiratory rate and blood pressure score compared with pneumonia severity index. Respirology 2012, 17, 969–975. [Google Scholar] [CrossRef]
- Komiya, K.; Kadota, J. C-reactive protein as a prognostic factor in elderly patients with aspiration pneumonia. Eur. J. Intern. Med. 2013, 24, e88–e89. [Google Scholar] [CrossRef]
- Simon, L.; Gauvin, F.; Amre, D.K.; Saint-Louis, P.; Lacroix, J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: A systematic review and meta-analysis. Clin. Infect. Dis. 2004, 39, 206–217. [Google Scholar] [CrossRef] [PubMed]
- Alves, A.E.; Pereira, J.M. Antibiotic therapy in ventilator-associated tracheobronchitis: A literature review. Rev. Bras. De Ter. Intensiv. 2018, 30, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; Muscedere, J.; Sweeney, D.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Carratala, J.; et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111. [Google Scholar] [CrossRef] [PubMed]
- Nseir, S.; Favory, R.; Jozefowicz, E.; Decamps, F.; Dewavrin, F.; Brunin, G.; Di Pompeo, C.; Mathieu, D.; Durocher, A. Antimicrobial treatment for ventilator-associated tracheobronchitis: A randomized, controlled, multicenter study. Crit. Care 2008, 12, R62. [Google Scholar] [CrossRef] [PubMed]
- Nseir, S.; Di Pompeo, C.; Pronnier, P.; Beague, S.; Onimus, T.; Saulnier, F.; Grandbastien, B.; Mathieu, D.; Delvallez-Roussel, M.; Durocher, A. Nosocomial tracheobronchitis in mechanically ventilated patients: Incidence, aetiology and outcome. Eur. Respir. J. 2002, 20, 1483–1489. [Google Scholar] [CrossRef]
- Nseir, S.; Di Pompeo, C.; Soubrier, S.; Delour, P.; Onimus, T.; Saulnier, F.; Durocher, A. Outcomes of ventilated COPD patients with nosocomial tracheobronchitis: A case-control study. Infection 2004, 32, 210–216. [Google Scholar] [CrossRef]
- Dallas, J.; Skrupky, L.; Abebe, N.; Boyle, W.A., 3rd; Kollef, M.H. Ventilator-associated tracheobronchitis in a mixed surgical and medical ICU population. Chest 2011, 139, 513–518. [Google Scholar] [CrossRef]
- Groenwold, R.H.; White, I.R.; Donders, A.R.; Carpenter, J.R.; Altman, D.G.; Moons, K.G. Missing covariate data in clinical research: When and when not to use the missing-indicator method for analysis. CMAJ 2012, 184, 1265–1269. [Google Scholar] [CrossRef]
- Miyashita, N.; Kawai, Y.; Tanaka, T.; Akaike, H.; Teranishi, H.; Wakabayashi, T.; Nakano, T.; Ouchi, K.; Okimoto, N. Detection failure rate of chest radiography for the identification of nursing and healthcare-associated pneumonia. J. Infect. Chemother. 2015, 21, 492–496. [Google Scholar] [CrossRef] [PubMed]
| Antibiotic Treatment (n = 44) | No Antibiotic Treatment (n = 143) | p-Value | |
|---|---|---|---|
| Female (number with percentage) | 13 (30) | 78 (55) | 0.004 |
| Age (years, median with interquartile range) | 84 (82–90) | 89 (84–93) | 0.003 |
| BMI (kg/m2, median with interquartile range) | 19.3 (16.4–21.1) | 17.7 (15.4–20.6) | 0.028 |
| Barthel Index (median with interquartile range) | 0 (0–10) | 0 (0–10) | 0.664 |
| Barthel Index < 60 (number with percentage) | 41 (93) | 141 (99) | 0.086 |
| Systolic blood pressure (mmHg, median with interquartile range) | 117 (99–128) | 116 (99–129) | 0.878 |
| Impaired consciousness (number with percentage) | 24 (55) | 94 (66) | 0.179 |
| Respiratory failure (number with percentage) | 14 (32) | 31 (22) | 0.169 |
| WBC count (/μL, median with interquartile range) | 9070 (6450–10,380) | 6240 (5320–7460) | 0.003 |
| Hemoglobin (g/dL, median with interquartile range) | 11.1 (9.6–11.9) | 11.1 (9.7–11.9) | 0.968 |
| Albumin (g/dL, median with interquartile range) | 2.6 (2.2–3.0) | 2.7 (2.4–3.1) | 0.285 |
| ALT (IU/L, median with interquartile range) | 12 (10–16) | 14 (10–21) | 0.194 |
| eGFR (mL/min/1.73 m2, median with interquartile range) | 72.4 (45.2–96.9) | 67.4 (49.8–95.9) | 0.995 |
| CRP (mg/dL, median with interquartile range) | 3.4 (2.0–7.4) | 1.2 (0.5–4.2) | 0.009 |
| COPD (number with percentage) | 5 (11) | 18 (13) | 0.829 |
| Cardiac disease (number with percentage) | 15 (34) | 40 (28) | 0.436 |
| Cerebrovascular disease (number with percentage) | 17 (39) | 47 (33) | 0.481 |
| Diabetes mellitus (number with percentage) | 10 (23) | 28 (20) | 0.650 |
| Pneumonia development (number with percentage) | 6 (14) | 31 (22) | 0.242 |
| 30-day mortality after the diagnosis of acute aspiration bronchitis (number with percentage) | 5 (11) | 15 (10) | 1.000 |
| Patients Who Developed Pneumonia (n = 37) | Patients Who Did Not Develop Pneumonia (n = 150) | Crude Odds Ratio | p-Value | |
|---|---|---|---|---|
| Female (number with percentage) | 16 (43) | 75 (50) | 0.762 (0.369–1.573) | 0.462 |
| Age (years, median with interquartile range) | 87 (84–92) | 88 (83–92) | 0.989 (0.928–1.054) | 0.732 |
| BMI (kg/m2, median with interquartile range) | 18.0 (15.0–20.2) | 18.2 (15.8–20.8) | 0.958 (0.863–1.062) | 0.414 |
| Barthel Index (median with interquartile range) | 0 (0–15) | 0 (0–10) | 0.999 (0.978–1.020) | 0.914 |
| Barthel Index < 60 (number with percentage) | 37 (100) | 145 (97) | NA | 0.999 |
| Systolic blood pressure (mmHg, median with interquartile range) | 109 (97–121) | 118 (101–131) | 0.984 (0.965–1.003) | 0.092 |
| Impaired consciousness (number with percentage) | 22 (59) | 96 (64) | 0.825 (0.395–1.722) | 0.609 |
| Respiratory failure (number with percentage) | 11 (30) | 34 (23) | 1.443 (0.647–3.219) | 0.370 |
| WBC count (/μL, median with interquartile range) | 7215 (5870–9715) | 6490 (5378–9070) | 1.000 (1.000–1.000) | 0.145 |
| Hemoglobin (g/dL, median with interquartile range) | 10.6 (9.1–11.0) | 11.2 (9.7–11.9) | 0.900 (0.575–1.408) | 0.644 |
| Albumin (g/dL, median with interquartile range) | 2.9 (2.6–3.2) | 2.7 (2.4–3.0) | 2.306 (0.284–18.703) | 0.434 |
| ALT (IU/L, median with interquartile range) | 12 (11–14) | 14 (10–20) | 0.980 (0.880–1.091) | 0.706 |
| eGFR (mL/min/1.73 m2, median with interquartile range) | 27.3 (15.1–56.4) | 71.2 (50.0–98.4) | 0.957 (0.922–0.993) | 0.019 |
| CRP (mg/dL, median with interquartile range) | 8.1 (3.6–9.6) | 2.0 (0.9–5.4) | 1.178 (0.981–1.414) | 0.079 |
| COPD (number with percentage) | 4 (11) | 19 (13) | 0.836 (0.266–2.623) | 0.758 |
| Cardiac diseases (number with percentage) | 9 (24) | 46 (31) | 0.727 (0.318–1.662) | 0.449 |
| Cerebrovascular disease (number with percentage) | 10 (27) | 54 (36) | 0.658 (0.296–1.463) | 0.305 |
| Diabetes mellitus (number with percentage) | 7 (19) | 31 (21) | 0.896 (0.360–2.231) | 0.813 |
| Use of antibiotics (number with percentage) | 6 (16) | 38 (25) | 0.570 (0.221–1.473) | 0.246 |
| Adjusted Odds Ratio | p-Value | |
|---|---|---|
| Systolic blood pressure (mmHg) | 0.990 (0.946–1.038) | 0.687 |
| eGFR (mL/min/1.73 m2) | 0.956 (0.920–0.993) | 0.020 |
| CRP (mg/dL) | 1.190 (0.976–1.452) | 0.086 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goto, A.; Komiya, K.; Umeki, K.; Hiramatsu, K.; Kadota, J.-i. Impact of Antibiotics Used for Acute Aspiration Bronchitis on the Prevention of Pneumonia. Geriatrics 2024, 9, 26. https://doi.org/10.3390/geriatrics9020026
Goto A, Komiya K, Umeki K, Hiramatsu K, Kadota J-i. Impact of Antibiotics Used for Acute Aspiration Bronchitis on the Prevention of Pneumonia. Geriatrics. 2024; 9(2):26. https://doi.org/10.3390/geriatrics9020026
Chicago/Turabian StyleGoto, Akihiko, Kosaku Komiya, Kenji Umeki, Kazufumi Hiramatsu, and Jun-ichi Kadota. 2024. "Impact of Antibiotics Used for Acute Aspiration Bronchitis on the Prevention of Pneumonia" Geriatrics 9, no. 2: 26. https://doi.org/10.3390/geriatrics9020026
APA StyleGoto, A., Komiya, K., Umeki, K., Hiramatsu, K., & Kadota, J.-i. (2024). Impact of Antibiotics Used for Acute Aspiration Bronchitis on the Prevention of Pneumonia. Geriatrics, 9(2), 26. https://doi.org/10.3390/geriatrics9020026






