Dietary Adherence and Cognitive Performance in Older Adults by Nativity Status: Results from the National Health and Nutrition Examination Survey (NHANES), 2011–2014
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Study Population
2.2. Cognitive Performance
2.3. Diet Score (HEI-2015)
2.4. Demographic-, Socioeconomic-, and Health-Related Variables
2.5. Statistical Analysis
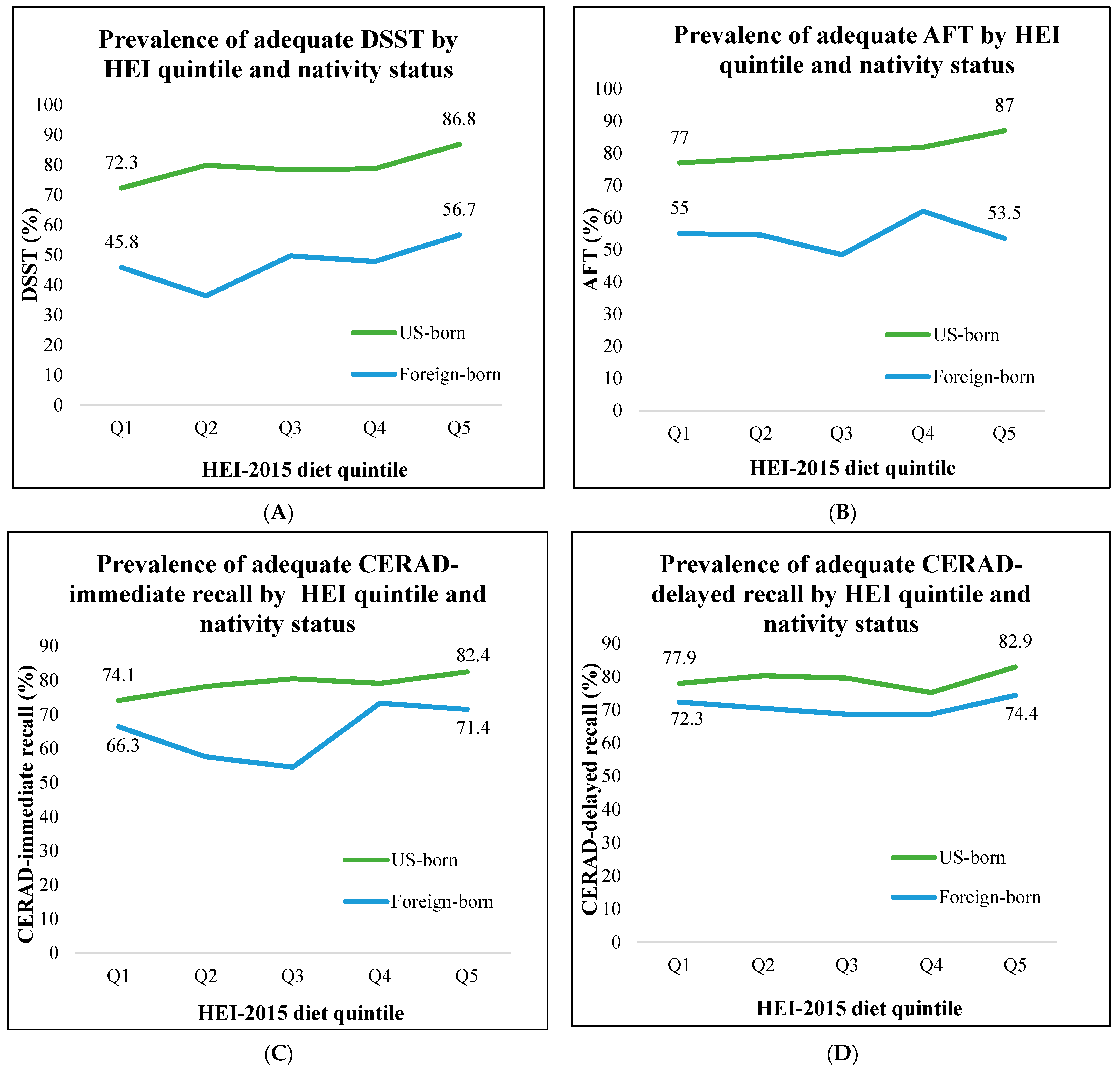
3. Results
| Characteristics | US Born (n = 2322) | Foreign Born (n = 743) | p-Value |
|---|---|---|---|
| % (weighted frequency), n | |||
| Age group (years) | 0.09 | ||
| 60–69 | 54.4 (1126) | 57.1 (477) | |
| 70–79 | 29.2 (714) | 31.0 (198) | |
| 80 and over | 16.4 (482) | 11.9 (68) | |
| Sex | 0.43 | ||
| Male | 46.2 (1131) | 44.3 (376) | |
| Female | 53.8 (1191) | 55.7 (367) | |
| Income | <0.001 | ||
| $0–$24,999 | 23.3 (784) | 36.5 (277) | |
| $25,000–$74,999 | 46.9 (971) | 44.3 (294) | |
| $75,000+ | 29.9 (489) | 19.1 (124) | |
| Education level | <0.001 | ||
| <High school | 14.9 (530) | 41.1 (329) | |
| High school | 22.7 (577) | 17.7 (130) | |
| Some college | 32.8 (706) | 17.0 (124) | |
| College degree+ | 29.7 (508) | 24.2 (158) | |
| Race | <0.001 | ||
| Non-Hispanic White | 87.7 (1404) | 23.2 (59) | |
| Black | 9.0 (667) | 7.0 (73) | |
| Latino | 2.8 (181) | 43.3 (390) | |
| Asian | 0.5 (31) | 26.5 (211) | |
| LTPA | 0.19 | ||
| Ideal | 29.6 (587) | 25.4 (184) | |
| Non-ideal | 70.4 (1735) | 74.6 (559) | |
| HEI quintile | <0.001 | ||
| Lowest quintile (Q1) | 20.5 (555) | 15.9 (115) | |
| 2nd quintile (Q2) | 21.0 (482) | 13.1 (109) | |
| 3rd quintile (Q3) | 19.8 (476) | 20.7 (158) | |
| 4th quintile (Q4) | 19.7 (424) | 22.6 (161) | |
| Highest quintile (Q5) | 19.0 (384) | 27.7 (199) | |
| DSST | <0.001 | ||
| Low CP | 20.9 (709) | 51.0 (355) | |
| Adequate CP | 79.1 (1429) | 49.0 (285) | |
| AFT | <0.001 | ||
| Low CP | 19.2 (609) | 45.3 (278) | |
| Adequate CP | 80.8 (1580) | 54.7 (375) | |
| CERAD-IR | <0.001 | ||
| Low CP | 21.2 (611) | 34.4 (245) | |
| Adequate CP | 78.8 (1585) | 65.6 (416) | |
| CERAD-DR | <0.01 | ||
| Low CP | 20.9 (568) | 29 (188) | |
| Adequate CP | 79.1 (1629) | 71.0 (480) | |
| US Born (n = 2322) | Foreign Born (n = 743) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Diet Q5 | CP Tests | n | Model 1 | Model 2 | Model 3 | n | Model 1 | Model 2 | Model 3 |
| OR, (95% CI) | OR, (95% CI) | ||||||||
| Highest | DSST | 359 | 2.51 (1.50, 4.21) * | 2.14 (1.24, 3.68) * | 1.95 (1.15, 3.28) * | 171 | 1.55 (0.70, 3.45) | 0.73 (0.23, 2.27) | 0.61 (0.20, 1.85) |
| 4th | 401 | 1.42 (1.07, 1.88) * | 1.25 (0.83, 1.89) | 1.21 (0.81, 1.80) | 142 | 1.08 (0.50, 2.36) | 0.65 (0.24, 1.71) | 0.57 (0.21, 1.54) | |
| 3rd | 433 | 1.38 (1.01, 1.88) * | 1.32 (0.98, 1.79) | 1.29 (0.96, 1.74) | 139 | 1.17 (0.58, 2.37) | 0.83 (0.31, 2.26) | 0.73 (0.28, 1.94) | |
| 2nd | 443 | 1.51 (1.02, 2.24) * | 1.51 (0.92, 2.48) | 1.48 (0.91, 2.42) | 94 | 0.68 (0.32, 1.44) | 0.70 (0.28, 1.73) | 0.64 (0.27, 1.53) | |
| Lowest | 501 | Ref. | Ref. | Ref. | 93 | Ref. | Ref. | Ref. | |
| Highest | AFT | 361 | 2.01 (1.25, 3.21) * | 1.56 (0.95, 2.55) | 1.42 (0.88, 2.30) | 170 | 0.94 (0.49, 1.81) | 0.97 (0.43, 2.15) | 0.91 (0.41, 2.01) |
| 4th | 404 | 1.34 (1.01, 1.79) * | 1.17 (0.83, 1.66) | 1.13 (0.80, 1.60) | 143 | 1.34 (0.63, 2.81) | 1.75 (0.68, 4.53) | 1.68 (0.66, 4.31) | |
| 3rd | 445 | 1.23 (0.83, 1.80) | 1.15 (0.73, 1.82) | 1.13 (0.72, 1.77) | 144 | 0.77 (0.38, 1.56) | 0.97 (0.37, 2.51) | 0.92 (0.36, 2.39) | |
| 2nd | 458 | 1.08 (0.72, 1.62) | 0.89 (0.57, 1.41) | 0.88 (0.55, 1.39) | 94 | 0.99 (0.43, 2.25) | 1.14 (0.45, 2.90) | 1.09 (0.44, 2.75) | |
| Lowest | 520 | Ref. | Ref. | Ref. | 101 | Ref. | Ref. | Ref. | |
| Highest | CERAD-IR | 362 | 1.65 (1.06, 2.55) * | 1.43 (0.92, 2.21) | 1.42 (0.90, 2.24) | 173 | 1.27 (0.70, 2.29) | 0.89 (0.54, 1.49) | 0.89 (0.50, 1.58) |
| 4th | 403 | 1.33 (0.96, 1.83) | 1.25 (0.86, 1.84) | 1.25 (0.85, 1.84) | 143 | 1.39 (0.81, 2.40) | 1.15 (0.65, 2.04) | 1.15 (0.64, 2.08) | |
| 3rd | 445 | 1.44 (1.02, 2.03) * | 1.37 (0.95, 1.98) | 1.37 (0.94, 2.00) | 148 | 0.61 (0.35, 1.06) | 0.57 (0.27, 1.22) | 0.57 (0.26, 1.28) | |
| 2nd | 459 | 1.25 (0.89, 1.76) | 1.16 (0.77, 1.76) | 1.16 (0.77, 1.75) | 97 | 0.69 (0.40, 1.17) | 0.88 (0.44, 1.74) | 0.88 (0.41, 1.85) | |
| Lowest | 526 | Ref. | Ref. | Ref. | 99 | Ref. | Ref. | Ref. | |
| Highest | CERAD-DR | 363 | 1.37 (0.89, 2.12) | 1.32 (0.80, 2.17) | 1.26 (0.75, 2.11) | 172 | 1.10 (0.60, 2.06) | 0.78 (0.43, 1.39) | 0.77 (0.42, 1.38) |
| 4th | 403 | 0.86 (0.69, 1.06) | 0.79 (0.57, 1.10) | 0.78 (0.56, 1.08) | 143 | 0.84 (0.40, 1.75) | 0.64 (0.30, 1.38) | 0.63 (0.28, 1.41) | |
| 3rd | 445 | 1.10 (0.75, 1.60) | 1.03 (0.68, 1.55) | 1.01 (0.67, 1.53) | 147 | 0.84 (0.39, 1.78) | 0.71 (0.37, 1.34) | 0.70 (0.36, 1.37) | |
| 2nd | 459 | 1.15 (0.79, 1.68) | 1.11 (0.74, 1.65) | 1.09 (0.73, 1.64) | 96 | 0.91 (0.53, 1.57) | 0.68 (0.32, 1.41) | 0.67 (0.32, 1.41) | |
| Lowest | 526 | Ref. | Ref. | Ref. | 99 | Ref. | Ref. | Ref. | |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alzheimer’s Association. 2021 Alzheimer’s Disease Facts and Figures. Alzheimer’s Dement. 2021, 17, 327–406. [Google Scholar] [CrossRef]
- Hardman, R.J.; Kennedy, G.; Macpherson, H.; Scholey, A.B.; Pipingas, A. Adherence to a Mediterranean-Style Diet and Effects on Cognition in Adults: A Qualitative Evaluation and Systematic Review of Longitudinal and Prospective Trials. Front. Nutr. 2016, 3, 22. [Google Scholar] [CrossRef]
- Houston, D.K. The Role of Diet on Life and Health Span—Lessons Learned Over the Past 75 Years. J. Gerontol. Ser. A 2020, 75, 1499–1501. [Google Scholar] [CrossRef]
- Morris, M.C.; Tangney, C.C.; Wang, Y.; Sacks, F.M.; Barnes, L.L.; Bennett, D.A.; Aggarwal, N.T. MIND Diet Slows Cognitive Decline with Aging. Alzheimer’s Dement. 2015, 11, 1015–1022. [Google Scholar] [CrossRef]
- van de Rest, O.; Berendsen, A.A.; Haveman-Nies, A.; de Groot, L.C. Dietary Patterns, Cognitive Decline, and Dementia: A Systematic Review. Adv. Nutr. 2015, 6, 154–168. [Google Scholar] [CrossRef]
- Koh, F.; Charlton, K.; Walton, K.; McMahon, A.-T. Role of Dietary Protein and Thiamine Intakes on Cognitive Function in Healthy Older People: A Systematic Review. Nutrients 2015, 7, 2415–2439. [Google Scholar] [CrossRef]
- Parletta, N.; Milte, C.M.; Meyer, B.J. Nutritional Modulation of Cognitive Function and Mental Health. J. Nutr. Biochem. 2013, 24, 725–743. [Google Scholar] [CrossRef]
- Rathod, R.; Kale, A.; Joshi, S. Novel Insights into the Effect of Vitamin B12 and Omega-3 Fatty Acids on Brain Function. J. Biomed. Sci. 2016, 23, 17. [Google Scholar] [CrossRef]
- US DHHS & USDA 2015–2020 Dietary Guidelines|Health.Gov. Available online: https://health.gov/our-work/nutrition-physical-activity/dietary-guidelines/previous-dietary-guidelines/2015 (accessed on 8 October 2021).
- Hu, F.B. Dietary Pattern Analysis: A New Direction in Nutritional Epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef]
- Flanagan, E.; Lamport, D.; Brennan, L.; Burnet, P.; Calabrese, V.; Cunnane, S.C.; de Wilde, M.C.; Dye, L.; Farrimond, J.A.; Emerson Lombardo, N.; et al. Nutrition and the Ageing Brain: Moving towards Clinical Applications. Ageing Res. Rev. 2020, 62, 101079. [Google Scholar] [CrossRef]
- Jennings, A.; Cunnane, S.C.; Minihane, A.M. Can Nutrition Support Healthy Cognitive Ageing and Reduce Dementia Risk? BMJ 2020, 369, m2269. [Google Scholar] [CrossRef]
- Kirkpatrick, S.I.; Reedy, J.; Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Wilson, M.M.; Lerman, J.L.; Tooze, J.A. Applications of the Healthy Eating Index for Surveillance, Epidemiology, and Intervention Research: Considerations and Caveats. J. Acad. Nutr. Diet. 2018, 118, 1603–1621. [Google Scholar] [CrossRef]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef]
- Haring, B.; Wu, C.; Mossavar-Rahmani, Y.; Snetselaar, L.; Brunner, R.; Wallace, R.B.; Neuhouser, M.L.; Wassertheil-Smoller, S. No Association between Dietary Patterns and Risk for Cognitive Decline in Older Women with 9-Year Follow-Up: Data from the Women’s Health Initiative Memory Study. J. Acad. Nutr. Diet. 2016, 116, 921–930.e1. [Google Scholar] [CrossRef]
- Hu, E.A.; Steffen, L.M.; Coresh, J.; Appel, L.J.; Rebholz, C.M. Adherence to the Healthy Eating Index–2015 and Other Dietary Patterns May Reduce Risk of Cardiovascular Disease, Cardiovascular Mortality, and All-Cause Mortality. J. Nutr. 2020, 150, 312–321. [Google Scholar] [CrossRef]
- Mizoguchi, N.; Walker, L.; Trevelyan, E.; Ahmed, B. The Older Foreign-Born Population in the United States 2012–2016; United States Census Bureau: Washington, DC, USA, 2019; p. 42.
- Xu, H.; Zhang, Y.; Wu, B. Association between Migration and Cognitive Status among Middle-Aged and Older Adults: A Systematic Review. BMC Geriatr. 2017, 17, 184. [Google Scholar] [CrossRef]
- Mehta, K.M.; Yeo, G.W. Systematic Review of Dementia Prevalence and Incidence in United States Race/Ethnic Populations. Alzheimer’s Dement. 2017, 13, 72–83. [Google Scholar] [CrossRef] [PubMed]
- Engelhardt, H.; Buber, I.; Skirbekk, V.; Prskawetz, A. Social Involvement, Behavioural Risks and Cognitive Functioning among Older People. Ageing Soc. 2010, 30, 779–809. [Google Scholar] [CrossRef]
- Peterson, R.L.; George, K.M.; Gilsanz, P.; Mayeda, E.R.; Glymour, M.M.; Meyer, O.L.; Mungas, D.M.; DeCarli, C.; Whitmer, R.A. Lifecourse Socioeconomic Changes and Late-Life Cognition in a Cohort of U.S.-Born and U.S. Immigrants: Findings from the KHANDLE Study. BMC Public Health 2021, 21, 920. [Google Scholar] [CrossRef] [PubMed]
- Marks, A.K.; Ejesi, K.; McCullough, M.B.; Coll, C.G. Developmental Implications of Discrimination. In Handbook of Child Psychology and Developmental Science; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2015; pp. 1–42. ISBN 978-1-118-96341-8. [Google Scholar]
- Robertson, A.; Tirado, M.C.; Lobstein, T.; Knai, C.; Jensen, J.; Ferro-Luzzi, A.; James, W. Food and Health in Europe: A New Basis for Action (European Series No 96); World Health Organization: Geneva, Switzerland, 2004.
- Garcia, M.A.; Saenz, J.L.; Downer, B.; Chiu, C.-T.; Rote, S.; Wong, R. Age of Migration Differentials in Life Expectancy With Cognitive Impairment: 20-Year Findings From the Hispanic-EPESE. Gerontologist 2018, 58, 894–903. [Google Scholar] [CrossRef] [PubMed]
- Markides, K.S.; Gerst, K. Immigration, Aging, and Health in the United States. In Handbook of Sociology of Aging; Settersten, R.A., Angel, J.L., Eds.; Handbooks of Sociology and Social Research; Springer: New York, NY, USA, 2011; pp. 103–116. ISBN 978-1-4419-7374-0. [Google Scholar]
- Ayala, G.X.; Baquero, B.; Klinger, S. A Systematic Review of the Relationship between Acculturation and Diet among Latinos in the United States: Implications for Future Research. J. Am. Diet. Assoc. 2008, 108, 1330–1344. [Google Scholar] [CrossRef]
- Miller, S.; de la Haye, K.; Bell, B.; Gálvez, A.; Rupp, S.; Flórez, K.R. Food Insecurity, Dietary Quality, and the Role of Social Network Support and Barriers Among Immigrant Latino Adults in New York City. J. Hunger. Environ. Nutr. 2023, 1–18. [Google Scholar] [CrossRef]
- Rabbitt, M.P. Food Security Among Hispanic Adults in the United States, 2011–2014. Food Secur. 2016. [Google Scholar] [CrossRef]
- Viladrich, A.; Tagliaferro, B. Picking Fruit from Our Backyard’s Trees: The Meaning of Nostalgia in Shaping Latinas’ Eating Practices in the United States. Appetite 2016, 97, 101–110. [Google Scholar] [CrossRef] [PubMed]
- National Center for Health Statistics NHANES Survey Methods and Analytic Guidelines. Available online: https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx (accessed on 12 April 2023).
- Brody, D.J.; Kramarow, E.A.; Taylor, C.A.; McGuire, L.C. Cognitive Performance in Adults Aged 60 and Over: National Health and Nutrition Examination Survey, 2011–2014. Natl. Health Stat. Rep. 2019, 126, 1–23. [Google Scholar]
- Blaum, C.S.; Ofstedal, M.B.; Liang, J. Low Cognitive Performance, Comorbid Disease, and Task-Specific Disability: Findings from a Nationally Representative Survey. J. Gerontol. A Biol. Sci. Med. Sci. 2002, 57, M523–M531. [Google Scholar] [CrossRef] [PubMed]
- Kuo, H.-K.; Leveille, S.G.; Yu, Y.-H.; Milberg, W.P. Cognitive Function, Habitual Gait Speed, and Late-Life Disability in the National Health and Nutrition Examination Survey (NHANES) 1999–2002. Gerontology 2007, 53, 102–110. [Google Scholar] [CrossRef]
- National Cancer Institute 24-Hour Dietary Recall (24HR) At a Glance|Dietary Assessment Primer. Available online: https://dietassessmentprimer.cancer.gov/profiles/recall/ (accessed on 5 April 2022).
- Shams-White, M.M.; Pannucci, T.E.; Lerman, J.L.; Herrick, K.A.; Zimmer, M.; Meyers Mathieu, K.; Stoody, E.E.; Reedy, J. Healthy Eating Index-2020: Review and Update Process to Reflect the Dietary Guidelines for Americans, 2020–2025. J. Acad. Nutr. Diet. 2023, 123, 1280–1288. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K.; Livingstone, M.B.E.; Fujiwara, A.; Sasaki, S. Application of the Healthy Eating Index-2015 and the Nutrient-Rich Food Index 9.3 for Assessing Overall Diet Quality in the Japanese Context: Different Nutritional Concerns from the US. PLoS ONE 2020, 15, e0228318. [Google Scholar] [CrossRef]
- Yoshida, Y.; Scribner, R.; Chen, L.; Broyles, S.; Phillippi, S.; Tseng, T.-S. Diet Quality and Its Relationship with Central Obesity among Mexican Americans: Findings from National Health and Nutrition Examination Survey (NHANES) 1999–2012. Public Health Nutr. 2017, 20, 1193–1202. [Google Scholar] [CrossRef]
- Food Patterns Equivalents Database (FPED). FPED Overview: USDA ARS. Available online: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fped-overview/ (accessed on 23 June 2021).
- George, S.M.; Reedy, J.; Cespedes Feliciano, E.M.; Aragaki, A.; Caan, B.J.; Kahle, L.; Manson, J.E.; Rohan, T.E.; Snetselaar, L.G.; Tinker, L.F.; et al. Alignment of Dietary Patterns With the Dietary Guidelines for Americans 2015–2020 and Risk of All-Cause and Cause-Specific Mortality in the Women’s Health Initiative Observational Study. Am. J. Epidemiol. 2021, 190, 886–892. [Google Scholar] [CrossRef]
- Reedy, J.; Lerman, J.L.; Krebs-Smith, S.M.; Kirkpatrick, S.I.; Pannucci, T.E.; Wilson, M.M.; Subar, A.F.; Kahle, L.L.; Tooze, J.A. Evaluation of the Healthy Eating Index-2015. J. Acad. Nutr. Diet. 2018, 118, 1622–1633. [Google Scholar] [CrossRef]
- Kaye, E.A.; Sohn, W.; Garcia, R.I. The Healthy Eating Index and Coronal Dental Caries in US Adults: National Health and Nutrition Examination Survey 2011–2014. J. Am. Dent. Assoc. 2020, 151, 78–86. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Wright, R.S.; Waldstein, S.R.; Kuczmarski, M.F.; Pohlig, R.T.; Gerassimakis, C.S.; Gaynor, B.; Evans, M.K.; Zonderman, A.B. Diet Quality and Cognitive Function in an Urban Sample: Findings from the Healthy Aging in Neighborhoods of Diversity across the Life Span (HANDLS) Study. Public Health Nutr. 2017, 20, 92–101. [Google Scholar] [CrossRef]
- Fan, Y.; Zhang, Y.; Li, J.; Liu, Y.; Chang, H.; Jiang, Y.; Tuo, X.; Zhou, L.; Yu, Y. Association between Healthy Eating Index-2015 and Various Cognitive Domains in US Adults Aged 60 Years or Older: The National Health and Nutrition Examination Survey (NHANES) 2011–2014. BMC Public Health 2021, 21, 1862. [Google Scholar] [CrossRef]
- Abbatecola, A.M.; Russo, M.; Barbieri, M. Dietary Patterns and Cognition in Older Persons. Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 10–13. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Smith, P.J.; Mabe, S.; Hinderliter, A.; Lin, P.-H.; Liao, L.; Welsh-Bohmer, K.A.; Browndyke, J.N.; Kraus, W.E.; Doraiswamy, P.M.; et al. Lifestyle and Neurocognition in Older Adults with Cognitive Impairments. Neurology 2019, 92, e212. [Google Scholar] [CrossRef]
- Dallo, F.J.; Kindratt, T.B.; Zahodne, L. Prevalence of Self-Reported Cognitive Impairment Among Arab American Immigrants in the United States. Innov. Aging 2021, 5, igaa058. [Google Scholar] [CrossRef]
- Gómez-Pinilla, F. Brain Foods: The Effects of Nutrients on Brain Function. Nat. Rev. Neurosci. 2008, 9, 568–578. [Google Scholar] [CrossRef]
- Smyth, A.; Dehghan, M.; O’Donnell, M.; Anderson, C.; Teo, K.; Gao, P.; Sleight, P.; Dagenais, G.; Probstfield, J.L.; Mente, A.; et al. Healthy Eating and Reduced Risk of Cognitive Decline: A Cohort from 40 Countries. Neurology 2015, 84, 2258–2265. [Google Scholar] [CrossRef] [PubMed]
- Spencer, S.J.; Korosi, A.; Layé, S.; Shukitt-Hale, B.; Barrientos, R.M. Food for Thought: How Nutrition Impacts Cognition and Emotion. npj Sci. Food 2017, 1, 7. [Google Scholar] [CrossRef]
- Estrella, M.L.; Durazo-Arvizu, R.A.; Mattei, J.; Mossavar-Rahmani, Y.; Perreira, K.M.; Siega-Riz, A.M.; Sotres-Alvarez, D.; González, H.M.; Gallo, L.C.; Daviglus, M.L.; et al. Alternate Healthy Eating Index Is Positively Associated with Cognitive Function Among Middle-Aged and Older Hispanics/Latinos in the HCHS/SOL. J. Nutr. 2020, 150, 1478–1487. [Google Scholar] [CrossRef]
- Gu, Y.; Guo, J.; Moshfegh, A.J. Race/Ethnicity and Gender Modify the Association between Diet and Cognition in U.S. Older Adults: National Health and Nutrition Examination Survey 2011–2014. Alzheimer’s Dement. 2021, 7, e12128. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.P.; Bhattacharya, J.; Pershing, S. Association of Vision Loss With Cognition in Older Adults. JAMA Ophthalmol. 2017, 135, 963–970. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alam, M.T.; Vásquez, E.; Etnier, J.L.; Echeverria, S. Dietary Adherence and Cognitive Performance in Older Adults by Nativity Status: Results from the National Health and Nutrition Examination Survey (NHANES), 2011–2014. Geriatrics 2024, 9, 25. https://doi.org/10.3390/geriatrics9020025
Alam MT, Vásquez E, Etnier JL, Echeverria S. Dietary Adherence and Cognitive Performance in Older Adults by Nativity Status: Results from the National Health and Nutrition Examination Survey (NHANES), 2011–2014. Geriatrics. 2024; 9(2):25. https://doi.org/10.3390/geriatrics9020025
Chicago/Turabian StyleAlam, Md Towfiqul, Elizabeth Vásquez, Jennifer L. Etnier, and Sandra Echeverria. 2024. "Dietary Adherence and Cognitive Performance in Older Adults by Nativity Status: Results from the National Health and Nutrition Examination Survey (NHANES), 2011–2014" Geriatrics 9, no. 2: 25. https://doi.org/10.3390/geriatrics9020025
APA StyleAlam, M. T., Vásquez, E., Etnier, J. L., & Echeverria, S. (2024). Dietary Adherence and Cognitive Performance in Older Adults by Nativity Status: Results from the National Health and Nutrition Examination Survey (NHANES), 2011–2014. Geriatrics, 9(2), 25. https://doi.org/10.3390/geriatrics9020025





