Risk Factors Analysis for 90-Day Mortality of Adult Patients with Mild Traumatic Brain Injury in an Italian Emergency Department
Abstract
:1. Introduction
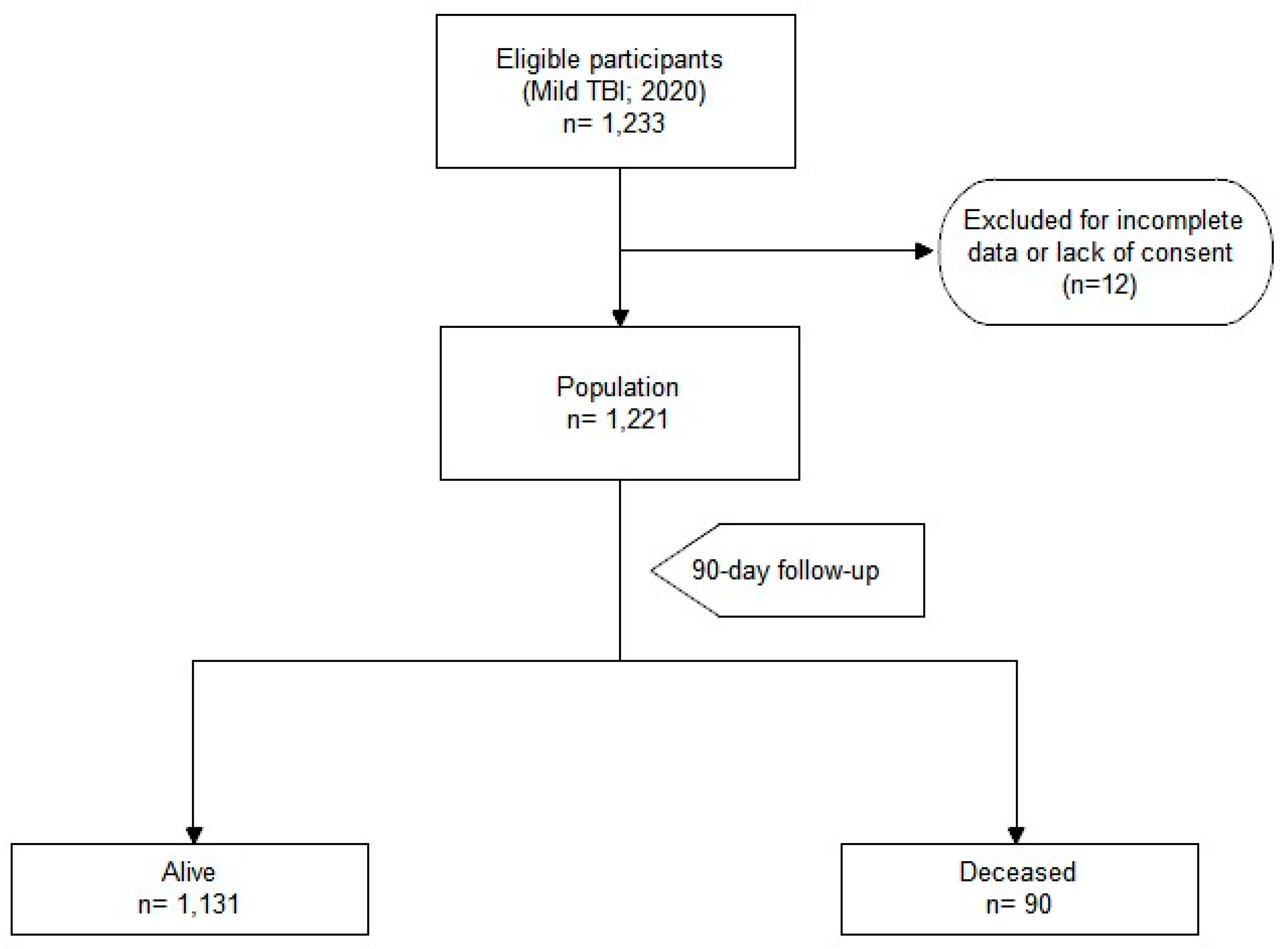
2. Materials and Methods
2.1. Study Design
2.2. Study Setting and Population
2.3. Study Variables
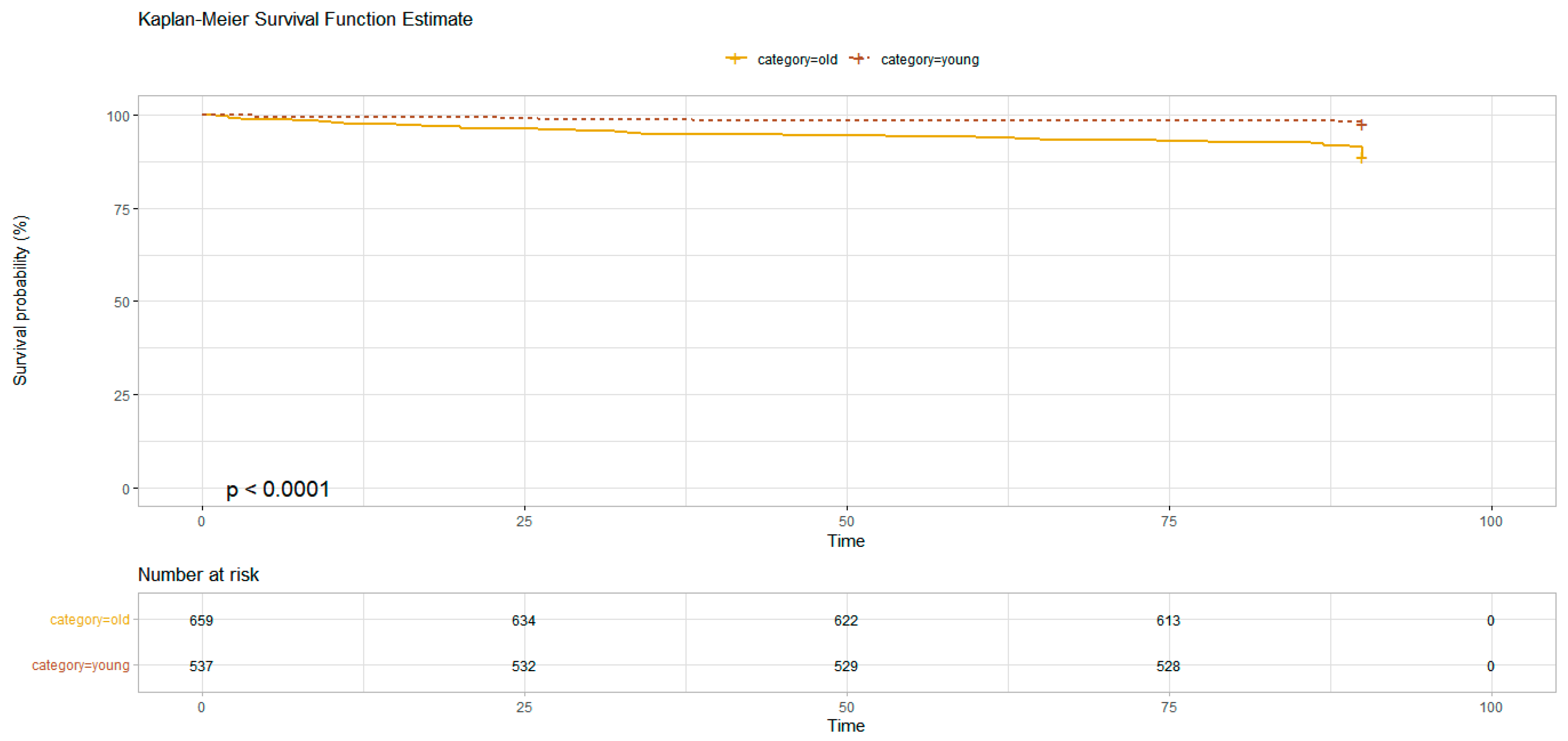
2.4. Age-Based Population Analysis
2.5. Statistical Analysis
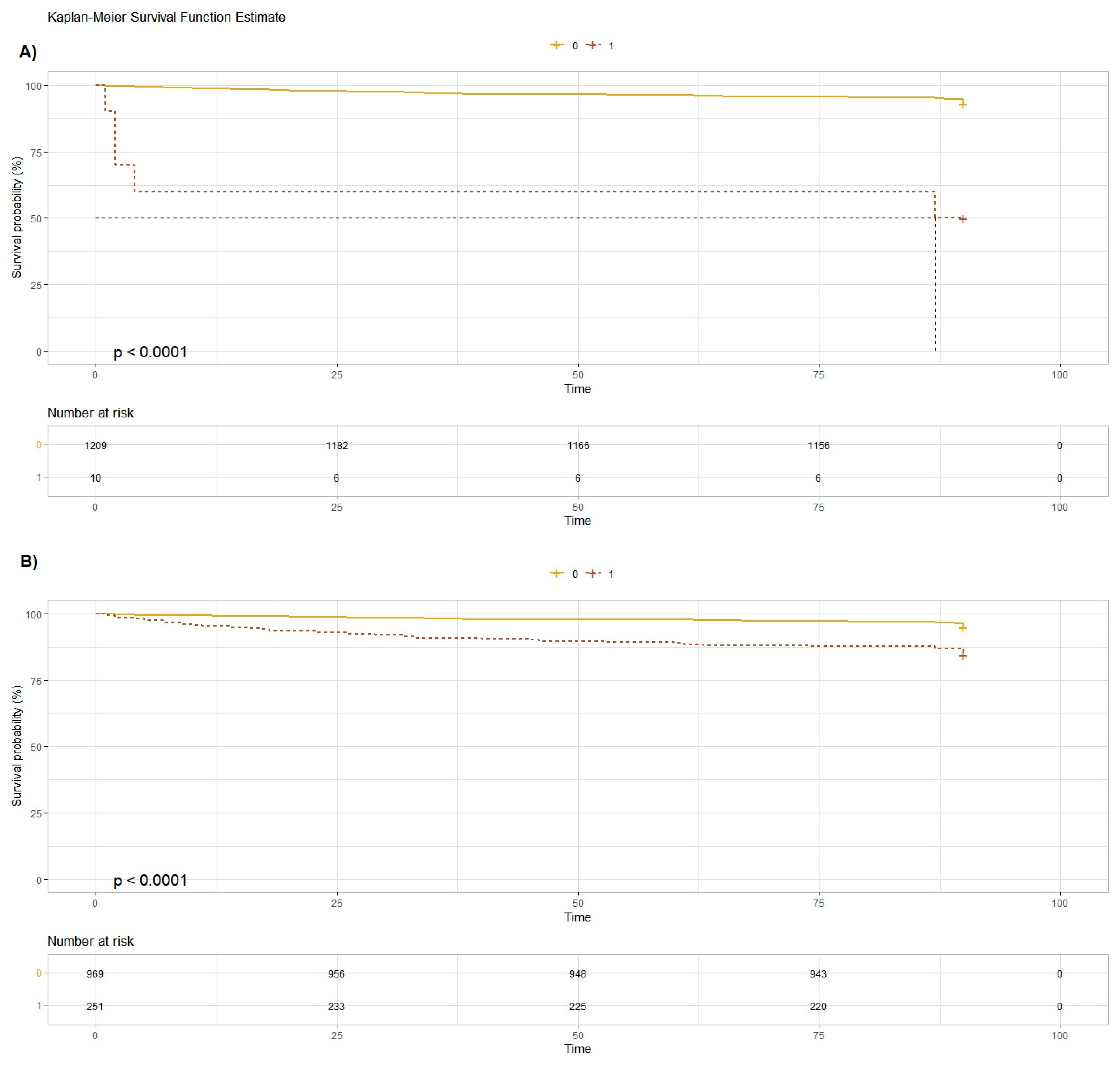
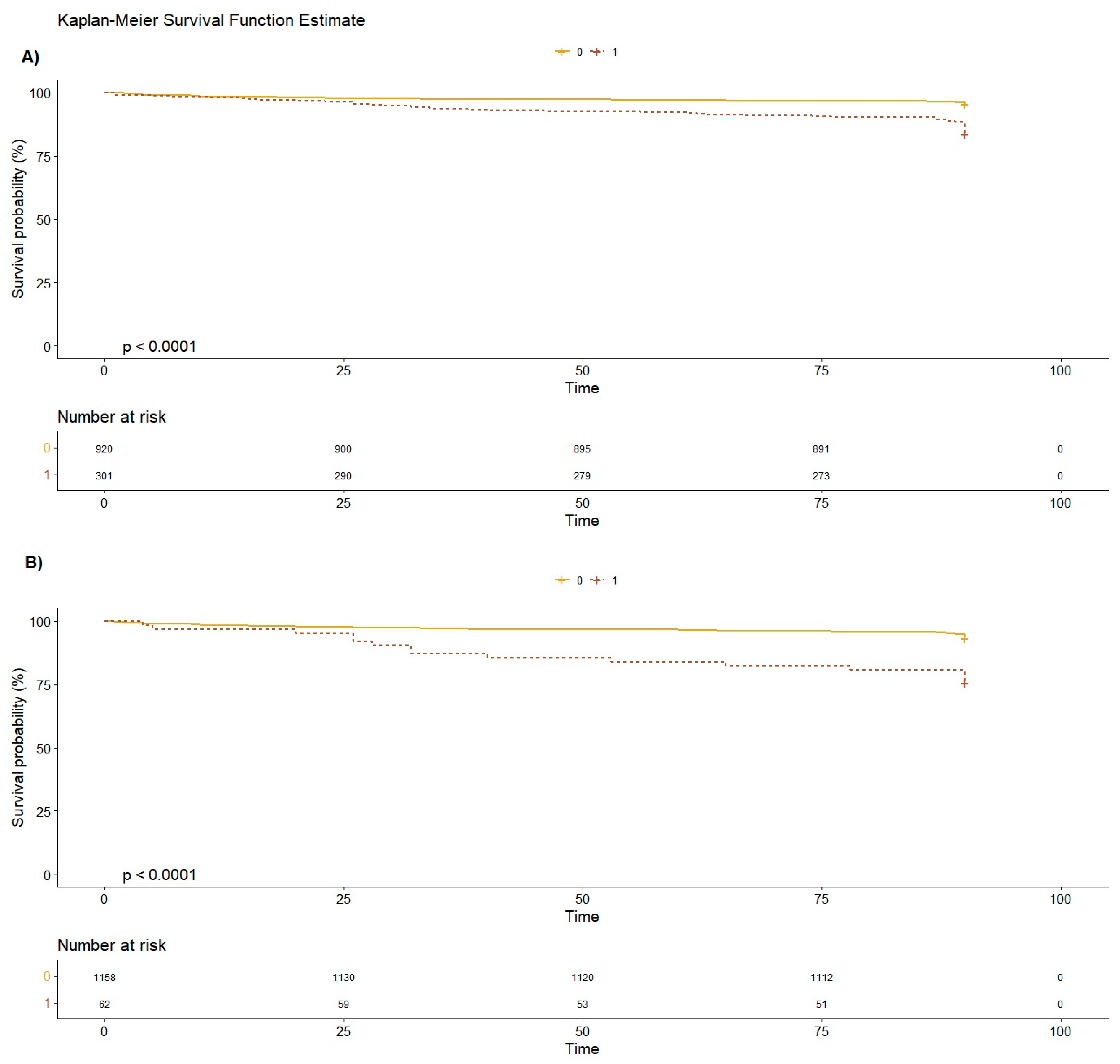
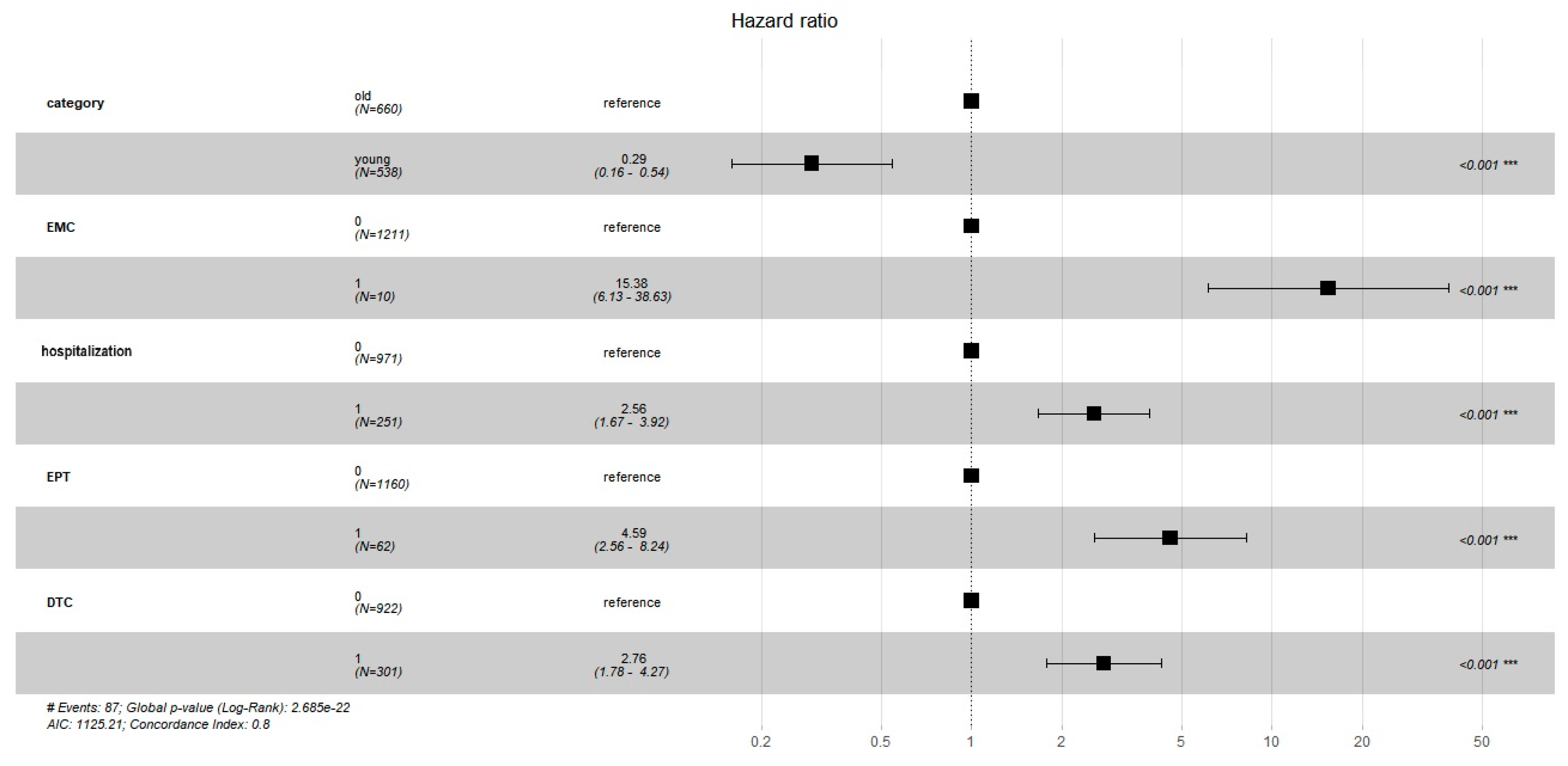
3. Results
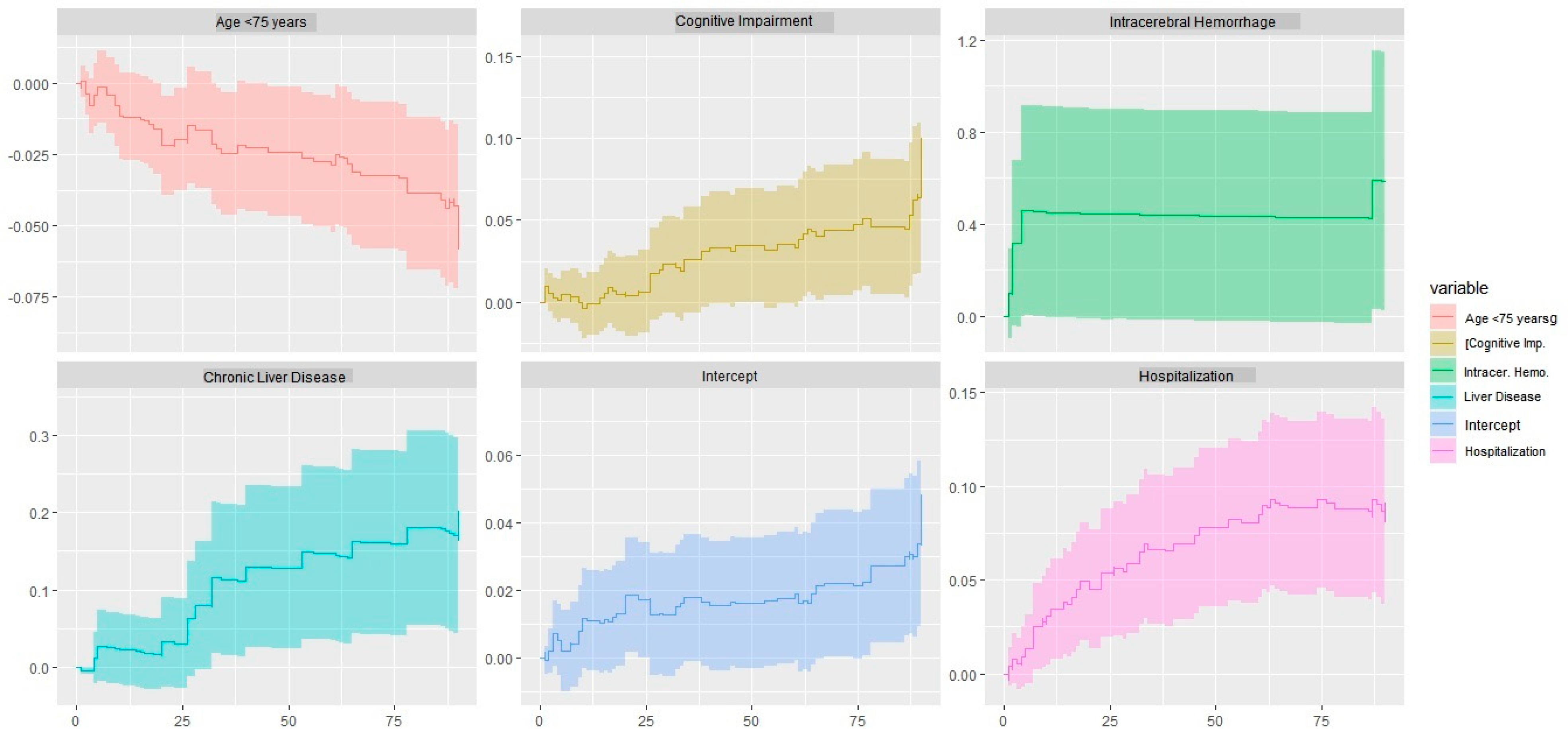
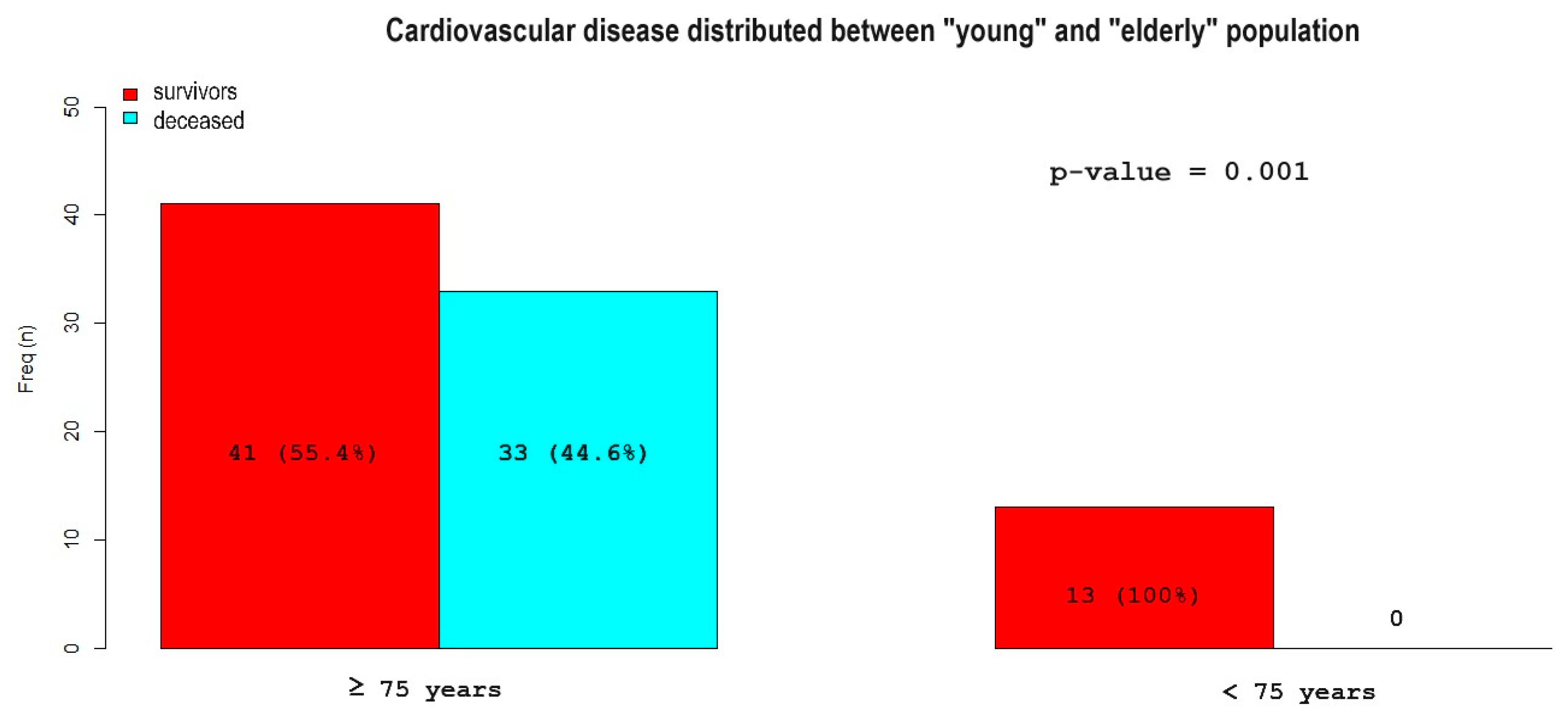
Age-Based Population Analysis
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Menon, D.K.; Schwab, K.; Wright, D.W.; Maas, A.I. Demographics and Clinical Assessment Working Group of the International and Interagency Initiative toward Common Data Elements for Research on Traumatic Brain Injury and Psychological Health. Position statement: Definition of traumatic brain injury. Arch. Phys. Med. Rehabil. 2010, 91, 1637–1640. [Google Scholar] [CrossRef] [PubMed]
- Sussman, E.S.; Pendharkar, A.V.; Ho, A.L.; Ghajar, J. Mild traumatic brain injury and concussion: Terminology and classification. Handb. Clin. Neurol. 2018, 158, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Kaur, P.; Sharma, S. Recent Advances in Pathophysiology of Traumatic Brain Injury. Curr. Neuropharmacol. 2018, 16, 1224–1238. [Google Scholar] [CrossRef] [PubMed]
- Mckee, A.C.; Daneshvar, D.H. The neuropathology of traumatic brain injury. Handb. Clin. Neurol. 2015, 127, 45–66. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.nice.org.uk/guidance/cg176/resources/head-injury-assessment-and-early-management-pdf-35109755595493 (accessed on 10 May 2021).
- Stiell, I.G.; Wells, G.A.; Vandemheen, K.; Clement, C.; Lesiuk, H.; Laupacis, A.; McKnight, R.D.; Verbeek, R.; Brison, R.; Cass, D.; et al. The Canadian CT Head Rule for patients with minor head injury. Lancet 2001, 357, 1391–1396. [Google Scholar] [CrossRef]
- Repplinger, M.D.; Li, A.J.; Svenson, J.E.; Ehlenbach, W.J.; Westergaard, R.P.; Reeder, S.B.; Jacobs, E.A. Emergency Department Patients’ Perceptions of Radiation From Medical Imaging. WMJ 2016, 115, 22–28. [Google Scholar]
- Steyerberg, E.W.; Wiegers, E.; Sewalt, C.; Buki, A.; Citerio, G.; De Keyser, V.; Ercole, A.; Kunzmann, K.; Lanyon, L.; Lecky, F.; et al. Case-mix, care pathways, and outcomes in patients with traumatic brain injury in CENTER-TBI: A European prospective, multicentre, longitudinal, cohort study. Lancet Neurol. 2019, 18, 923–934. [Google Scholar] [CrossRef]
- Groswasser, Z.; Peled, I. Survival and mortality following TBI. Brain Inj. 2018, 32, 149–157. [Google Scholar] [CrossRef]
- Leitner, L.; El-Shabrawi, J.H.; Bratschitsch, G.; Eibinger, N.; Klim, S.; Leithner, A.; Puchwein, P. Risk adapted diagnostics and hospitalization following mild traumatic brain injury. Arch. Orthop. Trauma Surg. 2021, 141, 619–627. [Google Scholar] [CrossRef]
- Ottochian, M.; Benfield, R.; Inaba, K.; Chan, L.S.; Demetriades, D. Prospective evaluation of a predictive model of mortality in patients with isolated head injury. J. Trauma 2009, 67, 81–84. [Google Scholar] [CrossRef]
- McMillan, T.M.; Weir, C.J.; Wainman-Lefley, J. Mortality and morbidity 15 years after hospital admission with mild head injury: A prospective case-controlled population study. J. Neurol. Neurosurg. Psychiatry 2014, 85, 1214–1220. [Google Scholar] [CrossRef]
- Popp, D.; Frankewycz, B.; Lang, S.; Ernstberger, A.; Alt, V.; Worlicek, M.; Kerschbaum, M. Are There Any Red Flag Injuries in Severely Injured Patients in Older Age? J. Clin. Med. 2021, 10, 185. [Google Scholar] [CrossRef]
- Castillo-Angeles, M.; Seshadri, A.J.; Benedict, L.A.; Patel, N.; Ramsis, R.; Askari, R.; Salim, A.; Nehra, D. Traumatic Brain Injury: Does Admission Service Matter? J. Surg. Res. 2021, 259, 211–216. [Google Scholar] [CrossRef]
- Naylor, R.M.; Henry, K.A.; Peters, P.A.; Bauman, M.M.J.; Lakomkin, N.; Van Gompel, J.J. High Long-Term Mortality Rate in Elderly Patients with Mild Traumatic Brain Injury and Subdural Hematoma due to Ground-Level Fall: Neurosurgery’s Hip Fracture? World Neurosurg. 2022, 167, e1122–e1127. [Google Scholar] [CrossRef]
- Lim, B.L.; Manaus, C.; Asians-Tan, M.L. Outcomes of warfarinized patients with minor head injury and normal initial CT scan. Am. J. Emerg. Med. 2016, 34, 75–78. [Google Scholar] [CrossRef]
- Afaneh, A.; Ford, J.; Gharzeddine, J.; Mazar, A.; Hayward, R.D.; Buck, J. Head injury on Warfarin: Likelihood of delayed intracranial bleeding in patients with negative initial head CT. BMC Res. Notes 2018, 11, 183. [Google Scholar] [CrossRef]
- Menditto, V.G.; Lucci, M.; Polonara, S.; Pomponio, G.; Gabrielli, A. Management of minor head injury in patients receiving oral anticoagulant therapy: A prospective study of a 24-hour observation protocol. Ann. Emerg. Med. 2012, 59, 451–455. [Google Scholar] [CrossRef]
- Stippler, M.; Smith, C.; McLean, A.R.; Carlson, A.; Morley, S.; Murray-Krizan, C.; Kraynik, J.; Kennedy, G. Utility of routine follow-up head CT scanning after mild traumatic brain injury: A systematic review of the literature. Emerg. Med. J. 2012, 29, 528–532. [Google Scholar] [CrossRef]
- Uccella, L.; Zoia, C.; Perlasca, F.; Bonetta, D.; Codecà, R.; Gaetani, P. Mild Traumatic Brain Injury in Patients on Long-Term Anticoagulation Therapy: Do They Really Need Repeated Head CT Scan? World Neurosurg. 2016, 93, 100–103. [Google Scholar] [CrossRef]
- Eroglu, S.E.; Onur, O.; Ozkaya, S.; Denızbasi, A.; Demır, H.; Ozpolat, C. Analysis of Repeated CT Scan Need in Blunt Head Trauma. Emerg. Med. Int. 2013, 2013, 916253. [Google Scholar] [CrossRef]
- Howlett, J.R.; Nelson, L.D.; Stein, M.B. Mental Health Consequences of Traumatic Brain Injury. Biol. Psychiatry 2022, 91, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Stocchetti, N.; Zanier, E.R. Chronic impact of traumatic brain injury on outcome and quality of life: A narrative review. Crit. Care 2016, 20, 148. [Google Scholar] [CrossRef] [PubMed]
- Elder, G.A. Update on TBI and Cognitive Impairment in Military Veterans. Curr. Neurol. Neurosci. Rep. 2015, 15, 68. [Google Scholar] [CrossRef] [PubMed]
- Pentland, B.; Hutton, L.S.; Jones, P.A. Late mortality after head injury. J. Neurol. Neurosurg. Psychiatry 2005, 76, 395–400. [Google Scholar] [CrossRef]
- Xiong, C.; Hanafy, S.; Chan, V.; Hu, Z.J.; Sutton, M.; Escobar, M.; Colantonio, A.; Mollayeva, T. Comorbidity in adults with traumatic brain injury and all-cause mortality: A systematic review. BMJ Open 2019, 9, e029072. [Google Scholar] [CrossRef] [PubMed]
- Hanafy, S.; Xiong, C.; Chan, V.; Sutton, M.; Escobar, M.; Colantonio, A.; Mollayeva, T. Comorbidity in traumatic brain injury and functional outcomes: A systematic review. Eur. J. Phys. Rehabil. Med. 2021, 57, 535–550. [Google Scholar] [CrossRef]
- Chandi, S.; Dekeseredy, P.; Brandmeir, N.J.; Fang, W.; Sedney, C.L. Traumatic brain injury in college students and the influence of alcohol consumption: A retrospective review from a rural state. J. Neurosci. Rural Pract. 2023, 14, 298–301. [Google Scholar] [CrossRef]
- Kornblith, E.; Bahorik, A.; Li, Y.; Peltz, C.B.; Barnes, D.E.; Yaffe, K. Traumatic brain injury, cardiovascular disease, and risk of dementia among older US Veterans. Brain Inj. 2022, 36, 628–632. [Google Scholar] [CrossRef]
- Cheng, P.L.; Lin, H.Y.; Lee, Y.K.; Hsu, C.Y.; Lee, C.C.; Su, Y.C. Higher mortality rates among the elderly with mild traumatic brain injury: A nationwide cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 7. [Google Scholar] [CrossRef]
- Lu, Y.; Jarrahi, A.; Moore, N.; Bartoli, M.; Brann, D.W.; Baban, B.; Dhandapani, K.M. Inflammaging, cellular senescence, and cognitive aging after traumatic brain injury. Neurobiol. Dis. 2023, 180, 106090. [Google Scholar] [CrossRef]
- Ostermann, R.C.; Joestl, J.; Tiefenboeck, T.M.; Lang, N.; Platzer, P.; Hofbauer, M. Risk factors predicting prognosis and outcome of elderly patients with isolated traumatic brain injury. J. Orthop. Surg. Res. 2018, 13, 277. [Google Scholar] [CrossRef] [PubMed]
- Selassie, A.W.; Fakhry, S.M.; Ford, D.W. Population-based study of the risk of in-hospital death after traumatic brain injury: The role of sepsis. J. Trauma 2011, 71, 1226–1234. [Google Scholar] [CrossRef] [PubMed]
- Gioffrè-Florio, M.; Murabito, L.M.; Visalli, C.; Pergolizzi, F.P.; Famà, F. Trauma in elderly patients: A study of prevalence, comorbidities, and gender differences. G. Chir. 2018, 39, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Elkbuli, A.; Smith, Z.; Shaikh, S.; Hai, S.; McKenney, M.; Boneva, D. Mild and Moderate Traumatic Brain Injury and Gender-Based Critical Care Outcomes. World J. Surg. 2020, 44, 1492–1497. [Google Scholar] [CrossRef]
- Nederpelt, C.J.; van der Aalst, S.J.M.; Rosenthal, M.G.; Krijnen, P.; Huisman, M.V.; Peul, W.C.; Schipper, I.B. Consequences of pre-injury utilization of direct oral anticoagulants in patients with traumatic brain injury: A systematic review and meta-analysis. J. Trauma Acute Care Surg. 2020, 88, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Santing, J.A.L.; Lee, Y.X.; van der Naalt, J.; van den Brand, C.L.; Jellema, K. Mild Traumatic Brain Injury in Elderly Patients Receiving Direct Oral Anticoagulants: A Systematic Review and Meta-Analysis. J. Neurotrauma 2022, 39, 458–472. [Google Scholar] [CrossRef]
- Hickey, S.; Hickman, Z.L.; Conway, J.; Giwa, A. The Effect of Direct Oral Anti-Coagulants on Delayed Traumatic Intracranial Hemorrhage After Mild Traumatic Brain Injury: A Systematic Review. J. Emerg. Med. 2021, 60, 321–330. [Google Scholar] [CrossRef]
- O’Brien, T.; Mitra, B.; Le Sage, N.; Tardif, P.A.; Emond, M.; D’Astous, M.; Mercier, E. Clinically significant traumatic intracranial hemorrhage following minor head trauma in older adults: A retrospective cohort study. Brain Inj. 2020, 34, 834–839. [Google Scholar] [CrossRef]
- Vehviläinen, J.; Virta, J.J.; Skrifvars, M.B.; Reinikainen, M.; Bendel, S.; Ala-Kokko, T.; Hoppu, S.; Laitio, R.; Siironen, J.; Raj, R. Effect of antiplatelet and anticoagulant medication use on injury severity and mortality in patients with traumatic brain injury treated in the intensive care unit. Acta Neurochir. 2023, 165, 4003–4012. [Google Scholar] [CrossRef] [PubMed]
- Fakhry, S.M.; Morse, J.L.; Garland, J.M.; Wilson, N.Y.; Shen, Y.; Wyse, R.J.; Watts, D.D. Antiplatelet and anticoagulant agents have minimal impact on traumatic brain injury incidence, surgery, and mortality in geriatric ground level falls: A multi-institutional analysis of 33,710 patients. J. Trauma Acute Care Surg. 2021, 90, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Hussein, W.; Mullins, P.M.; Alghamdi, K.; Sarani, B.; Pines, J.M. Trends in advanced computed tomography use for injured patients in United States emergency departments: 2007–2010. Acad. Emerg. Med. 2015, 22, 663–669. [Google Scholar] [CrossRef]
- Yun, B.J.; Borczuk, P.; Zachrison, K.S.; Goldstein, J.N.; Berlyand, Y.; Raja, A.S. Utilization of head CT during injury visits to United States emergency departments: 2012–2015. Am. J. Emerg. Med. 2018, 36, 1463–1466. [Google Scholar] [CrossRef]
- Pandor, A.; Goodacre, S.; Harnan, S.; Holmes, M.; Pickering, A.; Fitzgerald, P.; Rees, A.; Stevenson, M. Diagnostic management strategies for adults and children with minor head injury: A systematic review and an economic evaluation. Health Technol. Assess. 2011, 15, 1–202. [Google Scholar] [CrossRef]
- Holmes, M.W.; Goodacre, S.; Stevenson, M.D.; Pandor, A.; Pickering, A. The cost-effectiveness of diagnostic management strategies for adults with minor head injury. Injury 2012, 43, 1423–1431. [Google Scholar] [CrossRef] [PubMed]
- Smits, M.; Dippel, D.W.; Nederkoorn, P.J.; Dekker, H.M.; Vos, P.E.; Kool, D.R.; van Rijssel, D.A.; Hofman, P.A.; Twijnstra, A.; Tanghe, H.L.; et al. Minor head injury: CT-based strategies for management—A cost-effectiveness analysis. Radiology 2010, 254, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Easter, J.S.; Haukoos, J.S.; Meehan, W.P.; Novack, V.; Edlow, J.A. Will Neuroimaging Reveal a Severe Intracranial Injury in This Adult With Minor Head Trauma?: The Rational Clinical Examination Systematic Review. JAMA 2015, 314, 2672–2681, Erratum in JAMA 2017, 317, 2021. [Google Scholar] [CrossRef] [PubMed]
| Alive | Deceased | Hazard Ratio (95%CI) | p-Value | ||
|---|---|---|---|---|---|
| N = 1131 | N = 90 | ||||
| Demographic characteristics | |||||
| Age (years) [IQR] | 77 (57–85) | 88 (80–91) | 1.07 (1.05–1.09) | <0.001 | |
| Sex (males) (%) | 504 (45%) | 38 (42%) | 0.92 (0.60–1.40) | 0.696 | |
| Clinical history | |||||
| Arterial Hypertension (%) | 499 (44%) | 54 (60%) | 1.85 (1.21–2.82) | 0.004 | |
| Diabetes Mellitus (%) | 162 (14%) | 25 (28%) | 2.17 (1.37–3.44) | 0.001 | |
| Chronic Kidney Disease (%) | 111 (10%) | 19 (21%) | 2.38 (1.43–3.95) | 0.001 | |
| Alcoholism (%) | 83 (7%) | 6 (7%) | 0.90 (0.39–2.05) | 0.790 | |
| Chronic obstructive pulmonary disease (%) | 63 (6%) | 11 (12%) | 2.26 (1.20–4.25) | 0.009 | |
| Chronic Liver Disease (%) | 47 (4%) | 15 (17%) | 4.12 (2.37–7.18) | <0.001 | |
| Cardiac Disease (%) | 336 (30%) | 34 (38%) | 1.41 (0.92–2.15) | 0.116 | |
| Frequent Falls (%) | 236 (21%) | 38 (42%) | 2.59 (1.71–3.94) | <0.001 | |
| Cognitive Impairment (%) | 252 (22%) | 49 (54%) | 3.83 (2.53–5.81) | <0.001 | |
| Blood thinning medication | |||||
| Vitamin K antagonists (%) | 112 (10%) | 7 (8%) | 0.77 (0.36–1.67) | 0.515 | |
| Direct oral anticoagulants (%) | 57 (5%) | 3 (3%) | 0.65 (0.21–2.06) | 0.458 | |
| Low molecular weight heparin (or fondaparinux) (%) | 9 (1%) | 3 (3%) | 3.81 (1.20–12.0) | 0.015 | |
| Acetylsalicylic acid (%) | 191 (17%) | 16 (18%) | 1.07 (0.62–1.83) | 0.807 | |
| Clopidogrel (%) | 38 (3%) | 3 (3%) | 1.00 (0.32–1.83) | 0.998 | |
| Blood tests | |||||
| INR [IQR] | 1.07 [1.00–1.26] | 1.13 [1.03–1.28] | 0.97 (0.60–1.56) | 0.896 | |
| Platelets (count × 103/mm3) [IQR] | 218 [178–264] | 226 [184–286] | 1.00 (1.00–1.01) | 0.131 | |
| Blood Alcohol (g/L) [IQR] | 1.31 [0.10–2.84] | 0.10 [0.10–0.10] | 0.40 (0.12–1.39) | 0.151 | |
| Level of consciousness | |||||
| Glasgow Coma Scale [IQR] | 15 [15–15] | 15 [15–15] | 0.59 (0.28–1.21) | 0.149 | |
| Symptoms | |||||
| Amnesia (%) | 91 (8%) | 8 (9%) | 1.13 (0.55–2.34) | 0.741 | |
| Loss of Consciousness (%) | 92 (8%) | 4 (4%) | 0.54 (0.20–1.46) | 0.214 | |
| Vomiting (%) | 27 (2%) | 1 (1%) | 0.48 (0.07–3.43) | 0.453 | |
| Headache (%) | 85 (8%) | 0 (0%) | 0 | 0.008 | |
| Focal Neurological Deficit (%) | 13 (1%) | 1 (1%) | 1.01 (0.14–7.27) | 0.989 | |
| Confusion (%) | 113 (10%) | 23 (26%) | 2.98 (1.85–4.79) | <0.001 | |
| High Energy Impact | |||||
| High Energy Impact * (%) | 59 (5%) | 1 (1%) | 0.21 (0.03–1.54) | 0.092 | |
| Associated injuries | |||||
| Distal Upper Limb Fracture (%) | 46 (4%) | 4 (4%) | 1.09 (0.40–2.97) | 0.866 | |
| Proximal Upper Limb Fracture (%) | 43 (4%) | 1 (1%) | 0.29 (0.04–2.12) | 0.196 | |
| Rib fractures (%) | 36 (3%) | 2 (2%) | 0.71 (0.17–2.87) | 0.626 | |
| 1 rib (%) | 15 (1%) | 1 (1%) | |||
| 2 ribs (%) | 10 (1%) | 0 (0%) | |||
| ≥3 ribs (%) | 10 (1%) | 1 (1%) | |||
| Spine fracture (%) | 25 (2%) | 3 (3%) | 1.55 (0.49–4.89) | 0.452 | |
| Shoulder Girdle Fracture (%) | 9 (1%) | 1 (1%) | 1.45 (0.20–10.4) | 0.711 | |
| Pelvic fracture (%) | 12 (1%) | 3 (3%) | 2.89 (0.92–9.15) | 0.061 | |
| Distal Lower Limb Fracture (%) | 17 (2%) | 1 (1%) | 0.74 (0.10–5.31) | 0.765 | |
| Proximal Lower Limb Fracture (%) | 35 (3%) | 7 (8%) | 2.52 (1.16–5.44) | 0.015 | |
| Abdominal Trauma (%) | 13 (1%) | 0 (0%) | 0 | 0.315 | |
| Facial Fracture (%) | 86 (8%) | 5 (6%) | 0.72 (0.29–1.77) | 0.471 | |
| Neurocranium Fracture (%) | 14 (1%) | 1 (1%) | 0.92 (0.13–6.63) | 0.938 | |
| Head CT scan | |||||
| Subdural Hematoma (%) | 27 (2%) | 3 (3%) | 1.37 (0.43–4.34) | 0.586 | |
| Brain Contusion (%) | 17 (2%) | 0 (0%) | 0 | 0.250 | |
| Hemorrhagic Petechiae (%) | 14 (1%) | 1 (1%) | 0.92 (0.13–6.59) | 0.933 | |
| Intracerebral Hemorrhage (%) | 5 (0.4%) | 5 (6%) | 11.5 (4.68–28.4) | <0.001 | |
| Subarachnoid Hemorrhage (%) | 28 (2%) | 1 (1%) | 0.46 (0.06–3.29) | 0.427 | |
| Clinical management | |||||
| Hospitalization (%) | 212 (19%) | 39 (43%) | 3.17 (2.09–4.81) | <0.001 | |
| Discharge (%) | 798 (71%) | 51 (57%) | 0.55 (0.36–0.84) | 0.004 | |
| Abandonment (%) | 88 (8%) | 1 (1%) | 0.14 (0.02–0.99) | 0.021 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orso, D.; Furlanis, G.; Romanelli, A.; Gheller, F.; Tecchiolli, M.; Cominotto, F. Risk Factors Analysis for 90-Day Mortality of Adult Patients with Mild Traumatic Brain Injury in an Italian Emergency Department. Geriatrics 2024, 9, 23. https://doi.org/10.3390/geriatrics9020023
Orso D, Furlanis G, Romanelli A, Gheller F, Tecchiolli M, Cominotto F. Risk Factors Analysis for 90-Day Mortality of Adult Patients with Mild Traumatic Brain Injury in an Italian Emergency Department. Geriatrics. 2024; 9(2):23. https://doi.org/10.3390/geriatrics9020023
Chicago/Turabian StyleOrso, Daniele, Giulia Furlanis, Alice Romanelli, Federica Gheller, Marzia Tecchiolli, and Franco Cominotto. 2024. "Risk Factors Analysis for 90-Day Mortality of Adult Patients with Mild Traumatic Brain Injury in an Italian Emergency Department" Geriatrics 9, no. 2: 23. https://doi.org/10.3390/geriatrics9020023
APA StyleOrso, D., Furlanis, G., Romanelli, A., Gheller, F., Tecchiolli, M., & Cominotto, F. (2024). Risk Factors Analysis for 90-Day Mortality of Adult Patients with Mild Traumatic Brain Injury in an Italian Emergency Department. Geriatrics, 9(2), 23. https://doi.org/10.3390/geriatrics9020023






