Reducing Loneliness and Improving Social Support among Older Adults through Different Modalities of Personal Voice Assistants
Abstract
1. Introduction
1.1. Loneliness and Social Support in Older Adults
1.2. Information and Communication Technologies and Modality
2. Method
2.1. Measurement
2.2. Loneliness
2.3. Social Support
2.4. Coding of Older People’s Voice Interactions with PVA
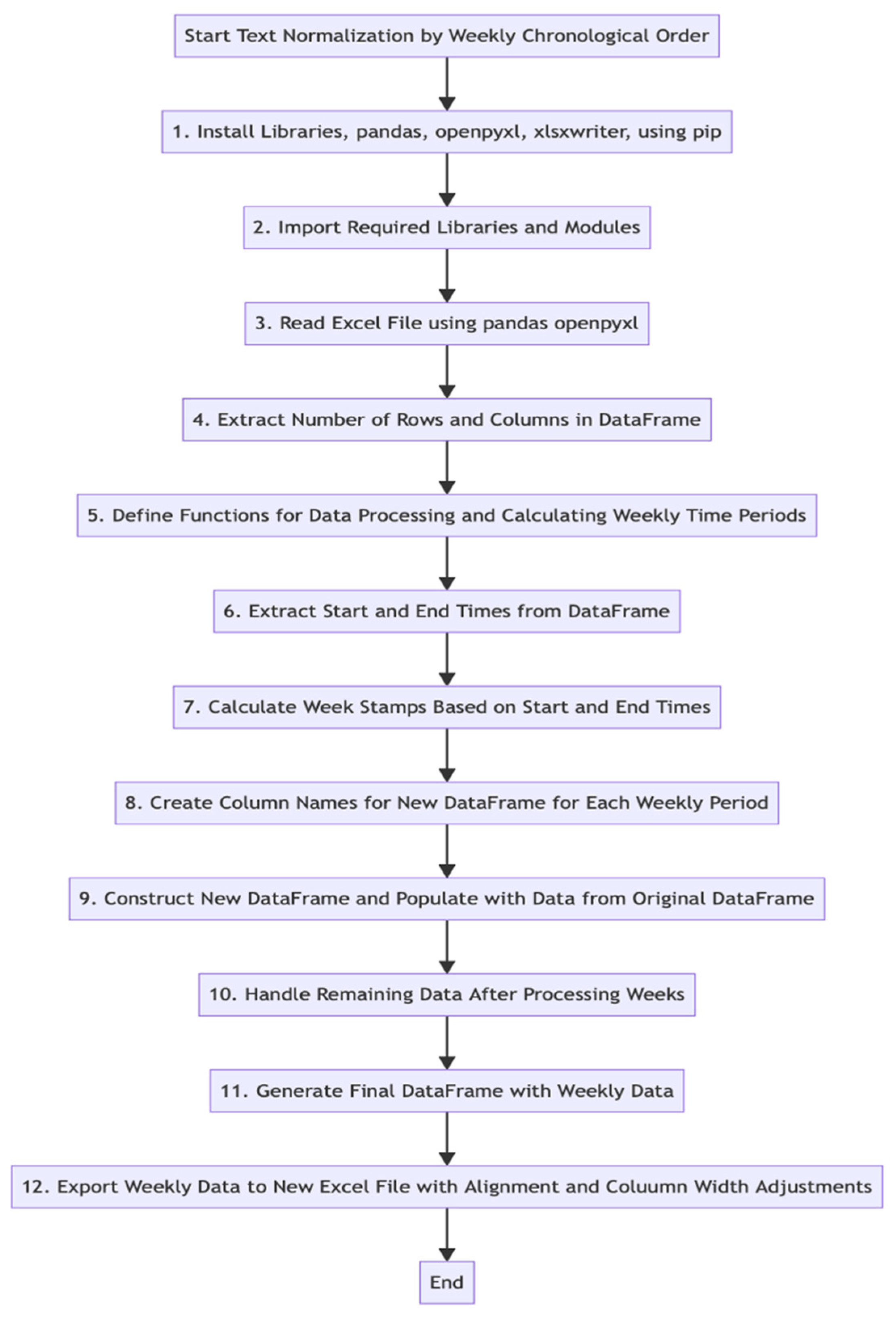
2.5. Coding Schema Development by a Human Coder
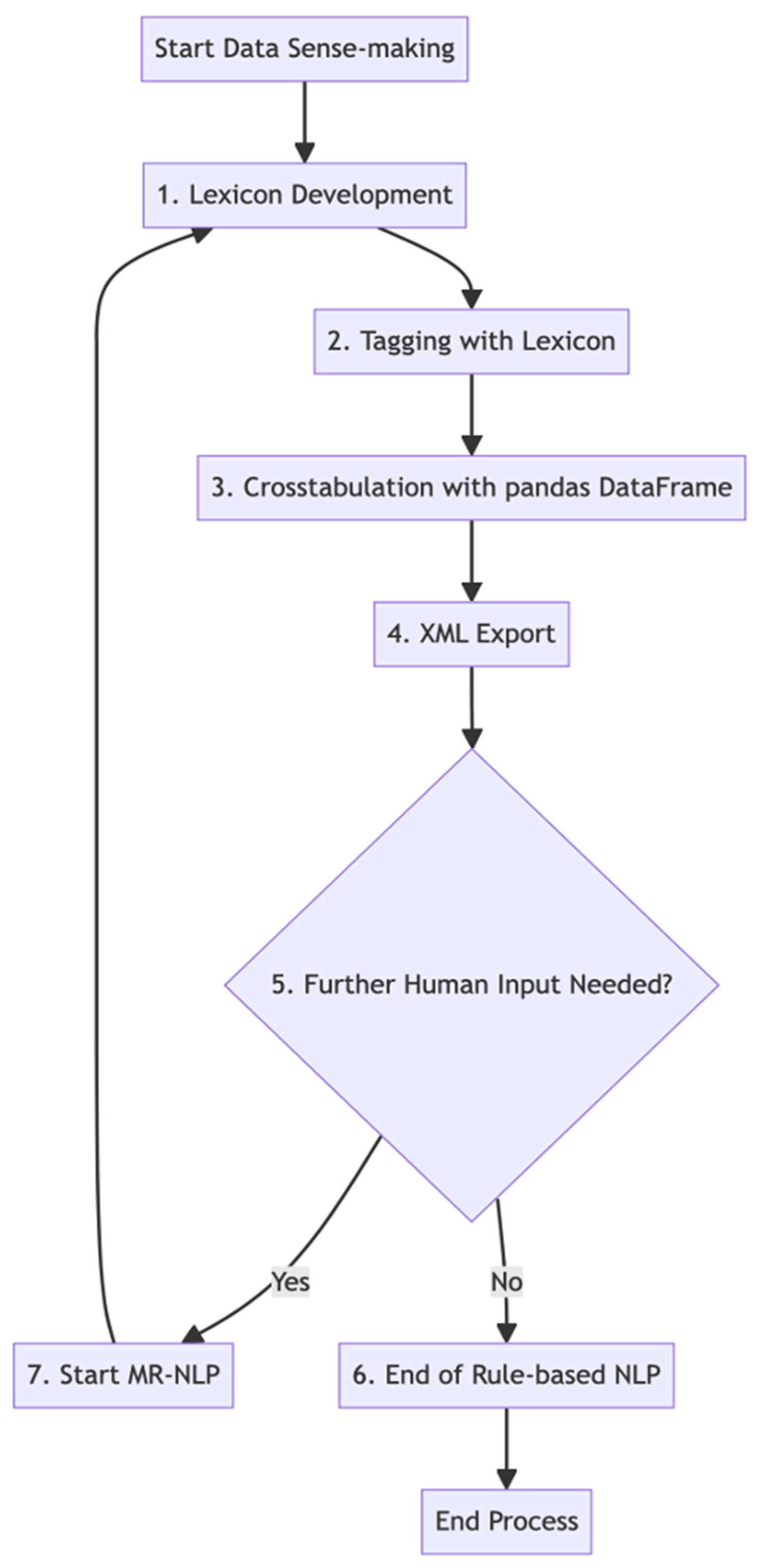
2.6. Rule-Based NLP Coding
3. Statistical Analysis
- General Statistical Procedures:
- -
- Descriptive Statistics and Normality Tests: Initially, descriptive statistics were calculated for the study’s dependent variables—perceived loneliness and perceived social support—across all intervention conditions. The Shapiro–Wilk test was utilized to assess the normality of these variables, determining the appropriateness of subsequent tests.
- Hypotheses 1 and 2 (H1 and H2):
- -
- Wilcoxon Signed-Rank Test: For H1 and H2, where normality was not assumed (as indicated by the Shapiro–Wilk test), the Wilcoxon signed-rank test, a nonparametric test, was used. This test compared pre- and post-study scores for both perceived loneliness and social support among all conditions combined.
- Hypothesis 3 (H3):
- -
- Spearman’s Rank Correlation Test: To explore the relationship between changes in perceived social support and perceived loneliness (H3), a two-tailed Spearman’s rank correlation test was conducted at a 95% confidence interval. This test was chosen due to its suitability for nonparametric data.
- Hypotheses 4 and 5 (H4 and H5):
- -
- Mann–Whitney U Test: For comparing the effectiveness of V-VAT and A-VAT interventions on perceived loneliness and social support (H4 and H5), the Mann–Whitney U test was applied. This test is appropriate for comparing differences between two independent groups, in this case, the V-VAT and A-VAT intervention groups.
- Hypothesis 6 (H6):
- -
- Spearman’s Rank Correlation Test for Subgroups: For H6, the Spearman’s rank correlation test was again employed, this time to separately examine the relationship between changes in perceived social support and loneliness in the V-VAT and A-VAT conditions. The choice of this test was due to its effectiveness in handling nonparametric data in small sample sizes.
4. Results
4.1. Loneliness Reduction and Social Support Increase
4.2. The Relationship between Social Support and Loneliness
4.3. Effects of VAT Modality
5. Discussion
6. Limitations and Future Research
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Ageing and Health 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 10 November 2023).
- Gerst-Emerson, K.; Jayawardhana, J. Loneliness as a public health issue: The impact of loneliness on health care utilization among older adults. Am. J. Public Health 2015, 105, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Donovan, N.J.; Blazer, D. Social isolation and loneliness in older adults: Review and commentary of a National Academies report. Am. J. Geriatr. Psychiatry 2020, 28, 1233–1244. [Google Scholar] [CrossRef] [PubMed]
- Cudjoe, T.K.; Roth, D.L.; Szanton, S.L.; Wolff, J.L.; Boyd, C.M.; Thorpe, R.J., Jr. The epidemiology of social isolation: National health and aging trends study. J. Gerontol. Ser. B 2020, 75, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.R.; Schultz, D.V. The effect of mobile touch screen devices on the behavior of older adults. Hum. Behav. Emerg. Technol. 2016, 1, 233–239. [Google Scholar]
- Portet, F.; Vacher, M.; Golanski, C.; Roux, C.; Meillon, B.; Beust, N. Design and evaluation of a smart home voice interface for the elderly: Acceptability and objection aspects. Pers. Ubiquitous Comput. 2013, 17, 127–144. [Google Scholar] [CrossRef]
- Balasubramanian, V.; Kanagasabai, R.; Katta, S.; Kanchan, S.; Dany, R.G.; Thangaraju, A. Performance assessment of voice-controlled personal assistants. J. Ambient. Intell. Humaniz. Comput. 2021, 12, 2531–2544. [Google Scholar]
- Bravo, J.; Díaz, M.; Villavicencio, F.; Alarcón, J.; Vilches, V.; Padilla, J.L. Evaluation of smart speakers as a means of human-AI interaction. Int. J. Hum.-Comput. Interact. 2020, 36, 1773–1785. [Google Scholar]
- O’Brien, T.; Kim, E.H.; Miyashita, S.; Wong, N.; Vinson, D.; Yang, J.J. Examining factors influencing older adults’ acceptance of smart home technology. Int. J. Med. Inform. 2022, 175, 104140. [Google Scholar]
- Perissinotto, C.M.; Cenzer, I.S.; Covinsky, K.E. Loneliness in older persons: A predictor of functional decline and death. Arch. Intern. Med. 2012, 172, 1078–1084. [Google Scholar] [CrossRef]
- Gerino, E.; Rollè, L.; Sechi, C.; Brustia, P.; Lonigro, A. Loneliness, resilience, mental health, and quality of life in old age: A structural equation model. Front. Psychol. 2003, 8, 2003. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lloyd-Evans, B.; Marston, L.; Mann, F. Loneliness in long-term neurological conditions: Systematic review and meta-analysis of determinants and outcomes. Eur. J. Neurol. 2018, 25, 1246–1256. [Google Scholar]
- Perissinotto, C.; Holt-Lunstad, J.; Periyakoil, V.S.; Covinsky, K. A practical approach to assessing and mitigating loneliness and isolation in older adults. J. Am. Geriatr. Soc. 2019, 67, 657–662. [Google Scholar] [CrossRef] [PubMed]
- O’Rourke, H.M.; Collins, L.; Sidani, S.; Puthussery, S. The prevalence of loneliness and social isolation in older people: An umbrella review of systematic reviews. PLoS ONE 2018, 13, e0180903. [Google Scholar]
- Tomaka, J.; Thompson, S.; Palacios, R. The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. J. Aging Health 2006, 18, 359–384. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Gorenko, J.A.; Moran, C.; Flynn, M.; Dobson, K.; Konnert, C. Social isolation and psychological distress among older adults related to COVID-19: A narrative review of remotely-delivered interventions and recommendations. J. Appl. Gerontol. 2021, 40, 3–13. [Google Scholar] [CrossRef]
- Khan, M.S.; Kadoya, Y. Loneliness during the COVID-19 pandemic: A comparison between older and younger people. Int. J. Environ. Res. Public Health 2021, 18, 7871. [Google Scholar] [CrossRef]
- Lin, N.; Ensel, W.M.; Simeone, R.S.; Kuo, W. Social support, stressful life events, and illness: A model and an empirical test. J. Health Soc. Behav. 1979, 20, 108–119. [Google Scholar] [CrossRef]
- Li, F.; Luo, S.; Mu, W.; Li, Y.; Ye, L.; Zheng, X.; Xu, B.; Ding, Y.; Ling, P.; Zhou, M.; et al. Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry 2021, 21, 16. [Google Scholar] [CrossRef]
- Wills, T.A.; Shinar, O. Measuring perceived and received social support. In Social Support Measurement and Intervention: A Guide for Health and Social Scientists; Cohen, S., Underwood, L.G., Gottlieb, B.H., Eds.; Oxford University Press: Oxford, UK, 2000; pp. 86–135. [Google Scholar]
- Cacioppo, J.T.; Cacioppo, S. Older adults reporting social isolation or loneliness show poorer cognitive function 4 years later. Evid.-Based Nurs. 2014, 17, 59–60. [Google Scholar] [CrossRef]
- Dahlberg, L.; McKee, K.J.; Frank, A.; Naseer, M. A systematic review of longitudinal risk factors for loneliness in older adults. Aging Ment. Health 2022, 26, 225–249. [Google Scholar] [CrossRef]
- Lee, S.H.; Lee, H.; Yu, S. Effectiveness of social support for community-dwelling elderly with depression: A systematic review and meta-analysis. Healthcare 2022, 10, 1598. [Google Scholar] [CrossRef]
- Zhang, X.; Dong, S. The relationships between social support and loneliness: A meta-analysis and review. Acta Psychol. 2022, 227, 103616. [Google Scholar] [CrossRef]
- Czaja, S.J.; Moxley, J.H.; Rogers, W.A. Social support, isolation, loneliness, and health among older adults in the PRISM randomized controlled trial. Front. Psychol. 2021, 12, 728658. [Google Scholar] [CrossRef] [PubMed]
- Haber, M.G.; Cohen, J.L.; Lucas, T.; Baltes, B.B. The relationship between self-reported received and perceived social support: A meta-analytic review. Am. J. Community Psychol. 2007, 39, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Jones, V.K.; Hanus, M.; Yan, C.; Shade, M.Y.; Blaskewicz Boron, J.; Maschieri Bicudo, R. Reducing loneliness among aging adults: The roles of personal voice assistants and anthropomorphic interactions. Front. Public Health 2021, 9, 750736. [Google Scholar] [CrossRef] [PubMed]
- Corbett, S.A.; Blanchard, L.M.; Roy, A.; Browne, A. The smart home system for older adults and their families: Function and attitude of the primary caregiver. Gerontechnology 2021, 20, 1–13. [Google Scholar]
- Jo, H.; Baek, H.J. Motivations for using voice-controlled virtual assistants among older adults. Comput. Hum. Behav. 2023, 138, 107183. [Google Scholar]
- Corbett, C.F.; Wright, P.J.; Jones, K.; Parmer, M. Voice-activated virtual home assistant use and social isolation and loneliness among older adults: Mini review. Front. Public Health 2021, 9, 742012. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.Y.; Lee, D. Effect of personal robots for elderly people: Exploratory study in a smart home. Healthc. Inform. Res. 2019, 25, 278–284. [Google Scholar]
- O’Brien, K.; Liggett, A.; Ramirez-Zohfeld, V.; Sunkara, P.; Lindquist, L.A. Voice-controlled intelligent personal assistants to support aging in place. J. Am. Geriatr. Soc. 2020, 68, 176–179. [Google Scholar] [CrossRef]
- Oewel, B.; Ammari, T.; Brewer, R.N. Voice assistant use in long-term care. In Proceedings of the 5th International Conference on Conversational User Interfaces, Eindhoven, The Netherlands, 19–21 July 2023; pp. 1–10. [Google Scholar]
- Heo, J.; Chun, S.; Lee, S.; Lee, K.H.; Kim, J. Internet use and well-being in older adults. Cyberpsychology Behav. Soc. Netw. 2015, 18, 268–272. [Google Scholar] [CrossRef]
- Castro-Alonso, J.C.; Sweller, J. The modality effect of cognitive load theory. In Advances in Human Factors in Training, Education, and Learning Sciences: Proceedings of the AHFE 2019 International Conference on Human Factors in Training, Education, and Learning Sciences, Washington DC, USA, 24–28 July 2019; Springer International Publishing: Berlin, Germany, 2020; Volume 10, pp. 75–84. [Google Scholar]
- Moreno, R.; Mayer, R.E. Cognitive principles of multimedia learning: The role of modality and contiguity. J. Educ. Psychol. 1999, 91, 358. [Google Scholar] [CrossRef]
- Mayer, R.E.; Moreno, R. Nine ways to reduce cognitive load in multimedia learning. Educ. Psychol. 2003, 38, 43–52. [Google Scholar] [CrossRef]
- Park, D.C. The basic mechanisms accounting for age-related decline in cognitive function. Cogn. Aging A Primer 2000, 11, 3–19. [Google Scholar]
- Sorden, S.D. The cognitive theory of multimedia learning. In Handbook of Educational Theories; Information Age Publishing: Charlotte, NC, USA, 2012; Volume 1, pp. 1–22. [Google Scholar]
- Kebede, A.S.; Ozolins, L.L.; Holst, H.; Galvin, K. Digital Engagement of Older Adults: Scoping Review. J. Med. Internet Res. 2022, 24, e40192. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Chan, A.H. Gerontechnology acceptance by elderly Hong Kong Chinese: A senior technology acceptance model (STAM). Ergonomics 2014, 57, 635–652. [Google Scholar] [CrossRef] [PubMed]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Russell, D.W. UCLA loneliness scale (Version 3): Reliability, validity, and factor structure. J. Personal. Assess. 1996, 66, 20–40. [Google Scholar] [CrossRef] [PubMed]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Lee, S.E.; Lee, H.S.; Yu, H. Measuring social support, loneliness, and worries in older adults during the COVID-19 pandemic: A longitudinal study. J. Gerontol. Ser. B 2022, 77, e230–e237. [Google Scholar]
- Kowalski, S.; Dhar, S.; Gründler, D.; Czapiewski, L.; Schröder, J. How voice assistants influence behavior in the home: An exploration of effects on children and implications for privacy through the lens of design. ACM Trans. Comput.-Hum. Interact. 2019, 26, 1–30. [Google Scholar]
- Zhong, L.; Ma, X. Towards ethical design and deployment of voice assistants for elderly users. In Proceedings of the 2022 CHI Conference on Human Factors in Computing Systems (CHI’22), New Orleans, LA, USA, 29 April 2022; pp. 1–12. [Google Scholar]
- Boyd, R.L.; Schwartz, H.A. A word or two about text analysis. Behav. Res. Methods 2021, 53, 1749–1758. [Google Scholar]
- Mortensen, L.; Meyer, A.S.; Humphreys, G.W. Age-related effects on speech production: A review. Lang. Cogn. Process. 2006, 21, 238–290. [Google Scholar] [CrossRef]
- Kim, S.; Choudhury, A. Exploring older adults’ perception and use of smart speaker-based voice assistants: A longitudinal study. Comput. Hum. Behav. 2021, 124, 106914. [Google Scholar] [CrossRef]
- Crowston, K.; Liu, L.; Allen, E. A taxonomy of motivations to contribute to online communities. Inf. Syst. J. 2010, 20, 1–24. [Google Scholar]
- Mather, M.; Scommegna, P. Fact Sheet: Aging in the United States. Population Reference Bureau. 9 January 2024. Available online: https://www.prb.org/resources/fact-sheet-aging-in-the-united-states/ (accessed on 10 January 2024).
- Jones, V.K. Why people use virtual assistants: Understanding engagement with Alexa. J. Brand Strategy 2022, 11, 80–101. [Google Scholar]
- Rafnsson, S.B.; Orrell, M.; d’Orsi, E.; Hogervorst, E.; Steptoe, A. Loneliness, social integration, and incident dementia over 6 years: Prospective findings from the English Longitudinal Study of Ageing. J. Gerontol. Psychol. Sci. 2017, 73, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Sorden, S.D. Cognitive load theory: A lasting and useful theory to guide multimedia design. In Cognitive Load Theory; Routledge: London, UK, 2013; pp. 255–268. [Google Scholar]
- Kebede, G.; Ozolins, A.L.; Holst, A.R.; Galvin, K.T. Assessing older adults’ engagement with multimedia: A systematic review of the literature. Educ. Gerontol. 2022, 48, 3–21. [Google Scholar]
- Sixsmith, J.; Horst, M.; Simeonov, D.; Mihailidis, A. Digital technologies and digital inequalities during COVID-19: Insights from a survey of adults aged 50 and over in Canada. Inf. Commun. Soc. 2022, 25, 218–232. [Google Scholar]
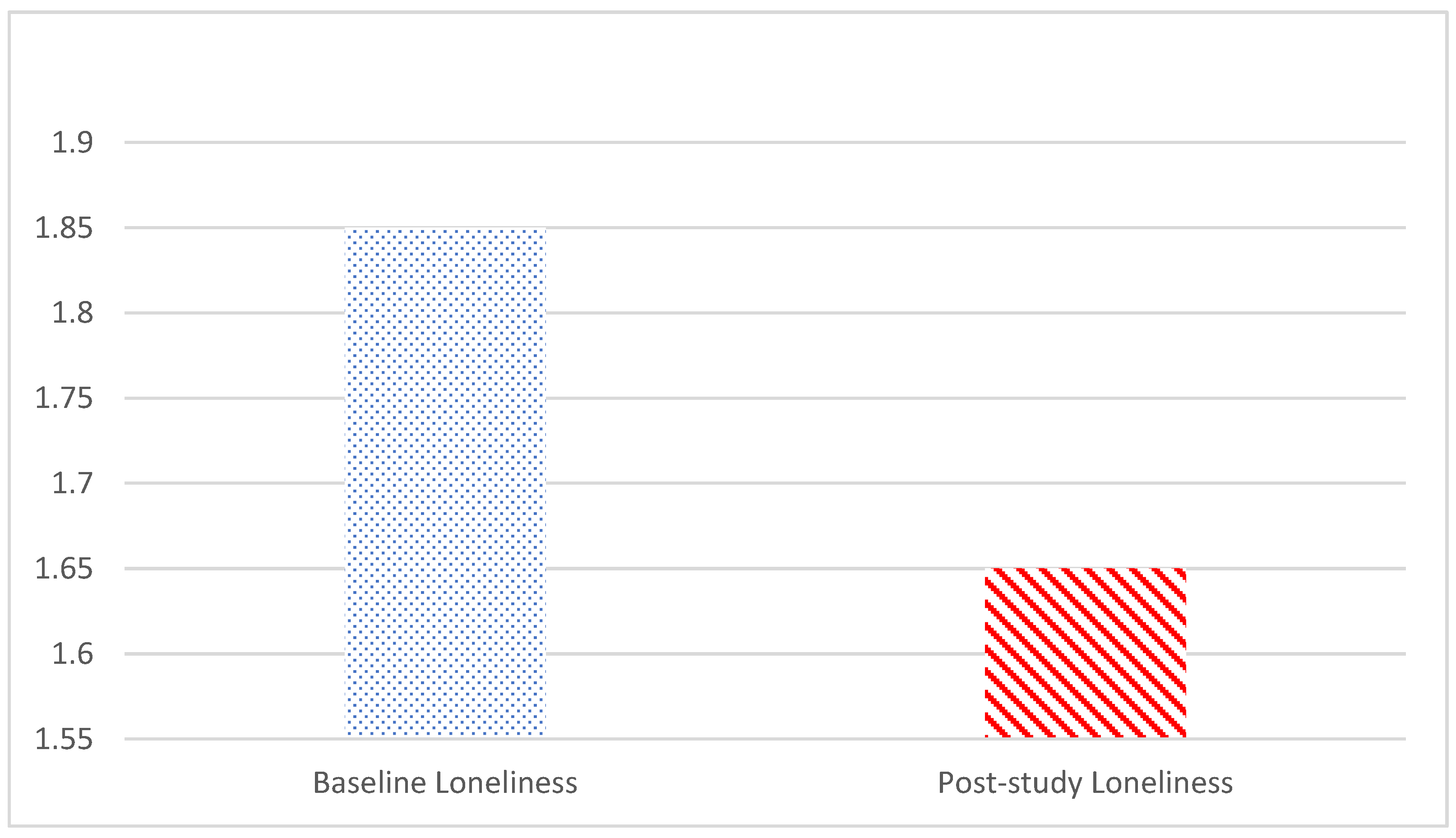
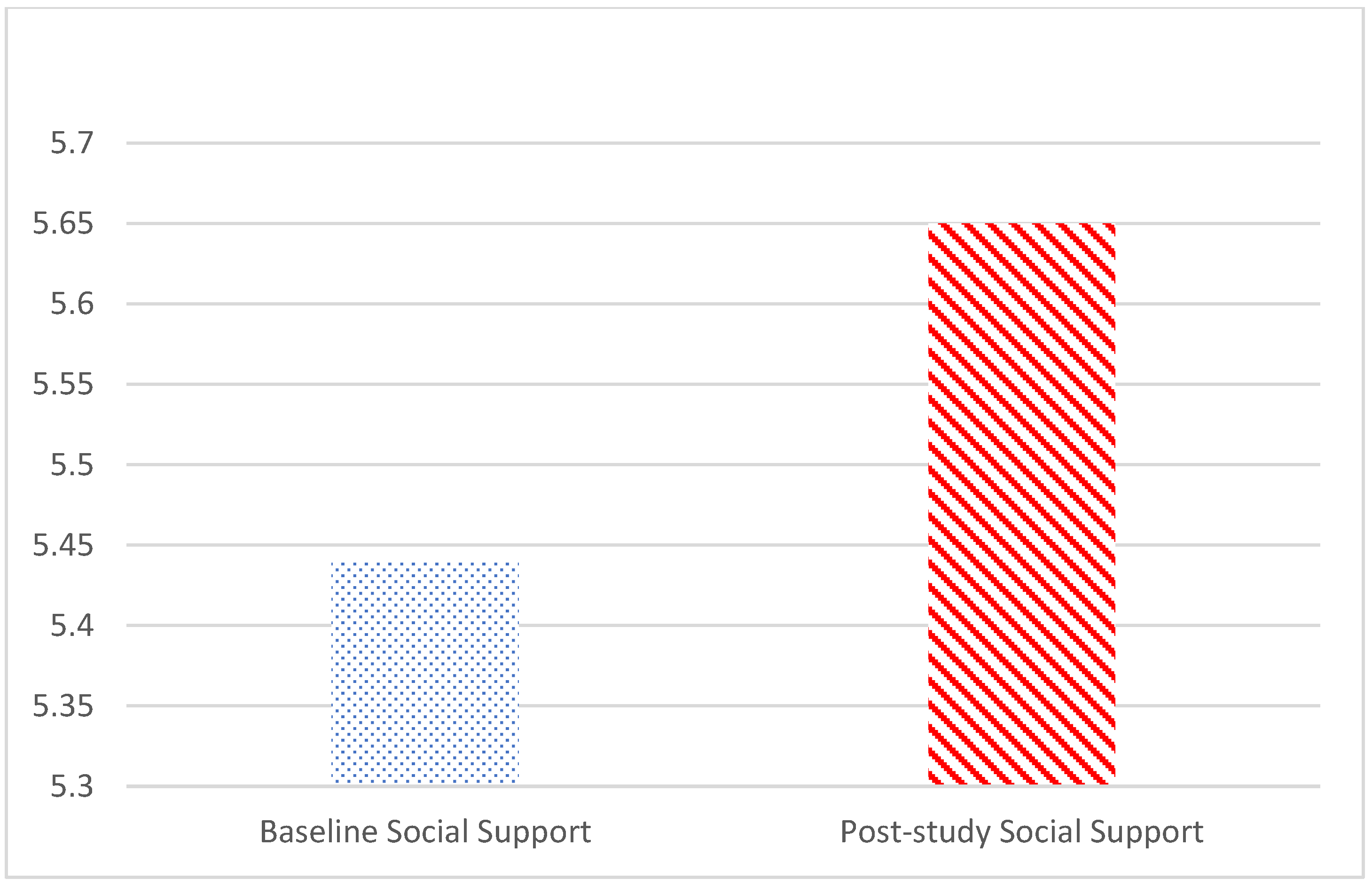
| Variables | Mean | Median | Variance | Standard Deviation | Range | Skewness | Kurtosis | Shapiro-Wilk Test |
|---|---|---|---|---|---|---|---|---|
| Baseline Loneliness | 1.85 | 1.73 | 0.37 | 0.61 | 2.15 | 0.39, SE = 0.40 | −0.77, SE = 0.79 | W(34) = 0.96, p = 0.266 |
| Post-study Loneliness | 1.65 | 1.58 | 0.33 | 0.57 | 2.60 | 1.52, SE = 0.40 | 2.86, SE = 0.79 | W(34) = 0.86, p < 0.001 |
| Baseline Social Support | 5.44 | 5.54 | 1.11 | 1.05 | 4.33 | −0.65, E = 0.40 | 0.15, SE = 0.79 | W(34) = 0.94, p = 0.072 |
| Post-study Social Support | 5.65 | 6 | 1.45 | 1.20 | 5.75 | −1.58, E = 0.40 | 3.89, SE = 0.79 | W(34) = 0.87, p = 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jones, V.K.; Yan, C.; Shade, M.Y.; Boron, J.B.; Yan, Z.; Heselton, H.J.; Johnson, K.; Dube, V. Reducing Loneliness and Improving Social Support among Older Adults through Different Modalities of Personal Voice Assistants. Geriatrics 2024, 9, 22. https://doi.org/10.3390/geriatrics9020022
Jones VK, Yan C, Shade MY, Boron JB, Yan Z, Heselton HJ, Johnson K, Dube V. Reducing Loneliness and Improving Social Support among Older Adults through Different Modalities of Personal Voice Assistants. Geriatrics. 2024; 9(2):22. https://doi.org/10.3390/geriatrics9020022
Chicago/Turabian StyleJones, Valerie K., Changmin Yan, Marcia Y. Shade, Julie Blaskewicz Boron, Zhengxu Yan, Hyeon Jung Heselton, Kate Johnson, and Victoria Dube. 2024. "Reducing Loneliness and Improving Social Support among Older Adults through Different Modalities of Personal Voice Assistants" Geriatrics 9, no. 2: 22. https://doi.org/10.3390/geriatrics9020022
APA StyleJones, V. K., Yan, C., Shade, M. Y., Boron, J. B., Yan, Z., Heselton, H. J., Johnson, K., & Dube, V. (2024). Reducing Loneliness and Improving Social Support among Older Adults through Different Modalities of Personal Voice Assistants. Geriatrics, 9(2), 22. https://doi.org/10.3390/geriatrics9020022








