Risk Factors Analysis for 90-Day Mortality of Adult Patients with Mild Traumatic Brain Injury in an Italian Emergency Department
Abstract
1. Introduction
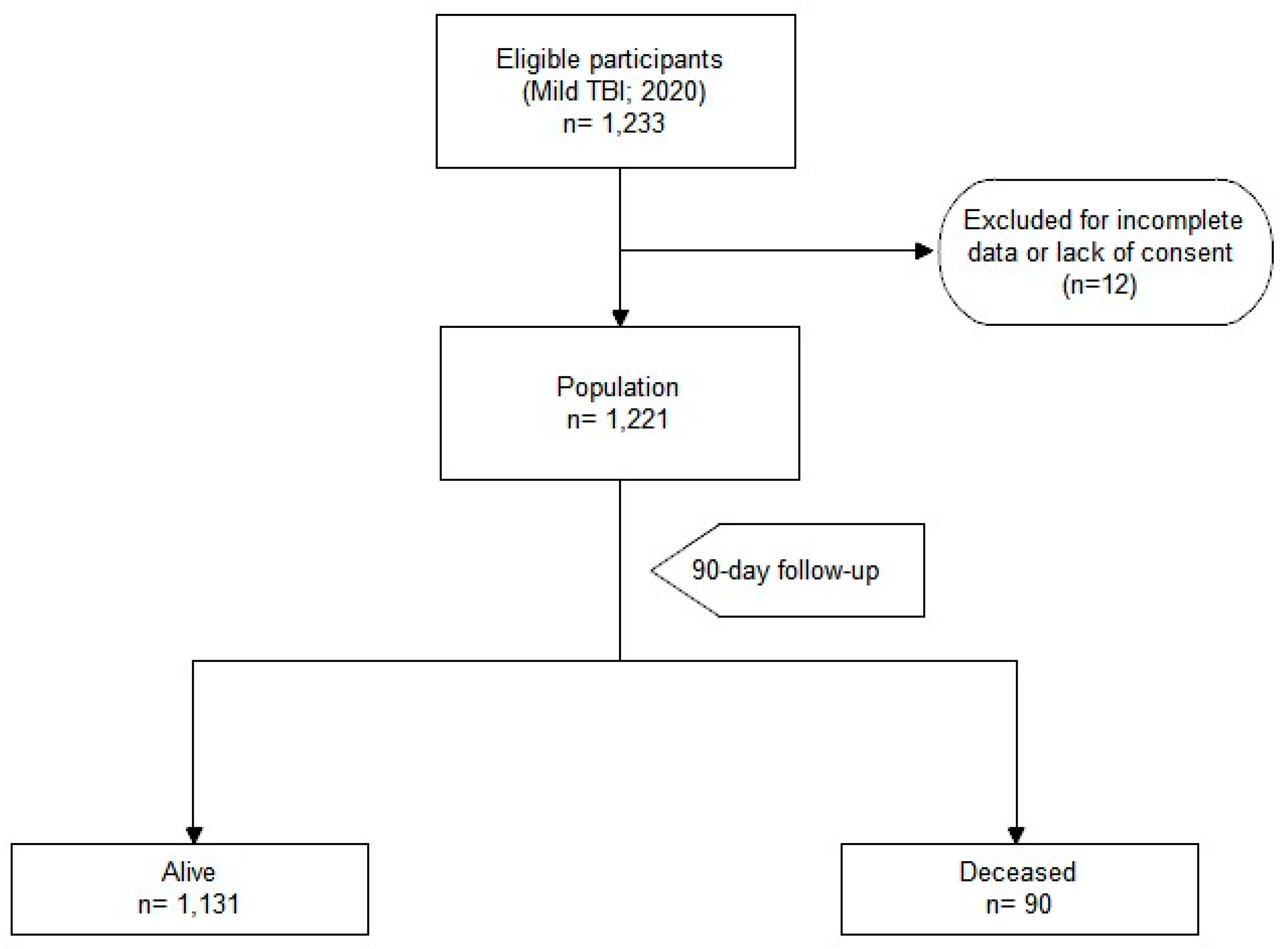
2. Materials and Methods
2.1. Study Design
2.2. Study Setting and Population
2.3. Study Variables
2.4. Age-Based Population Analysis
2.5. Statistical Analysis
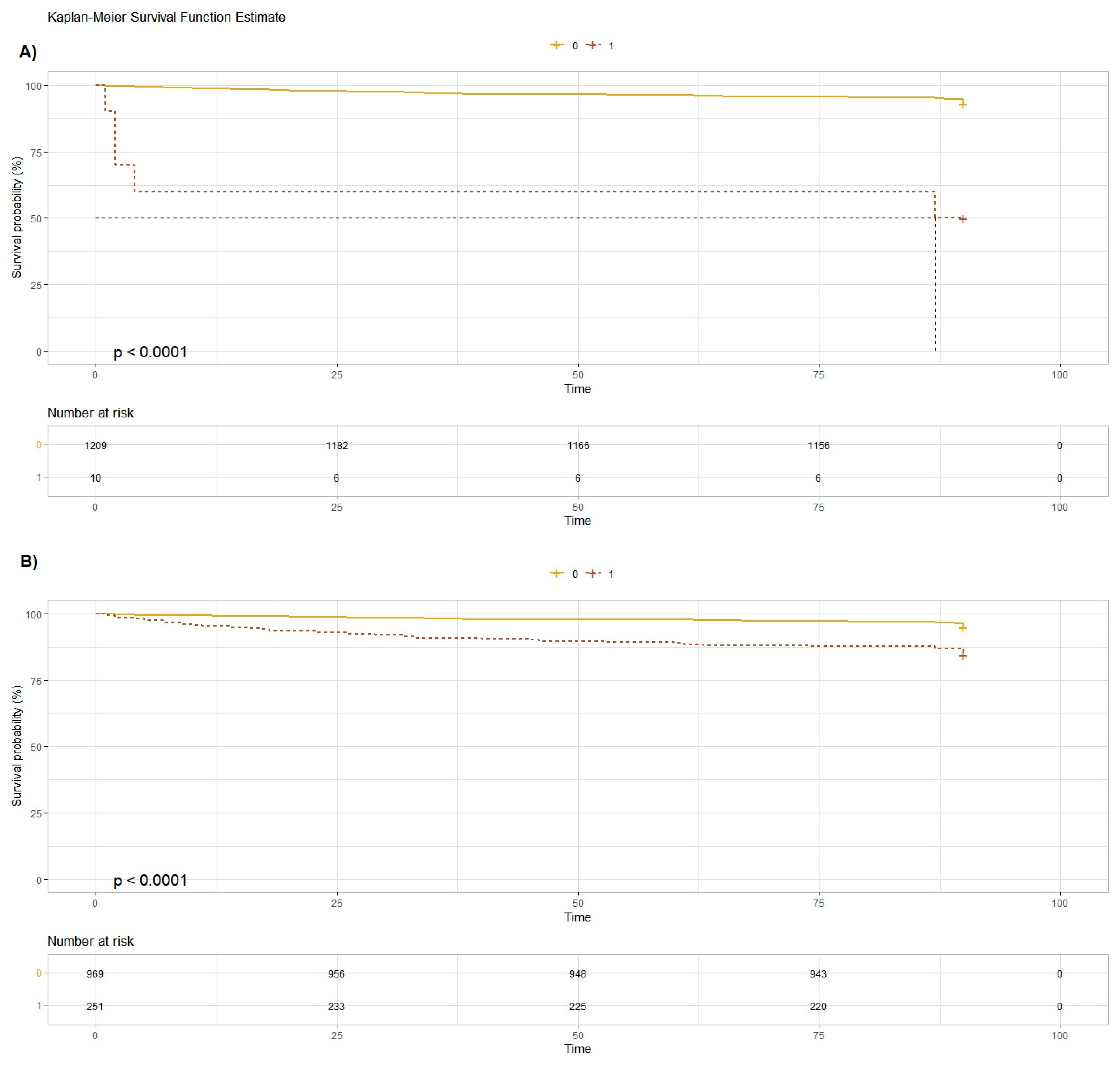
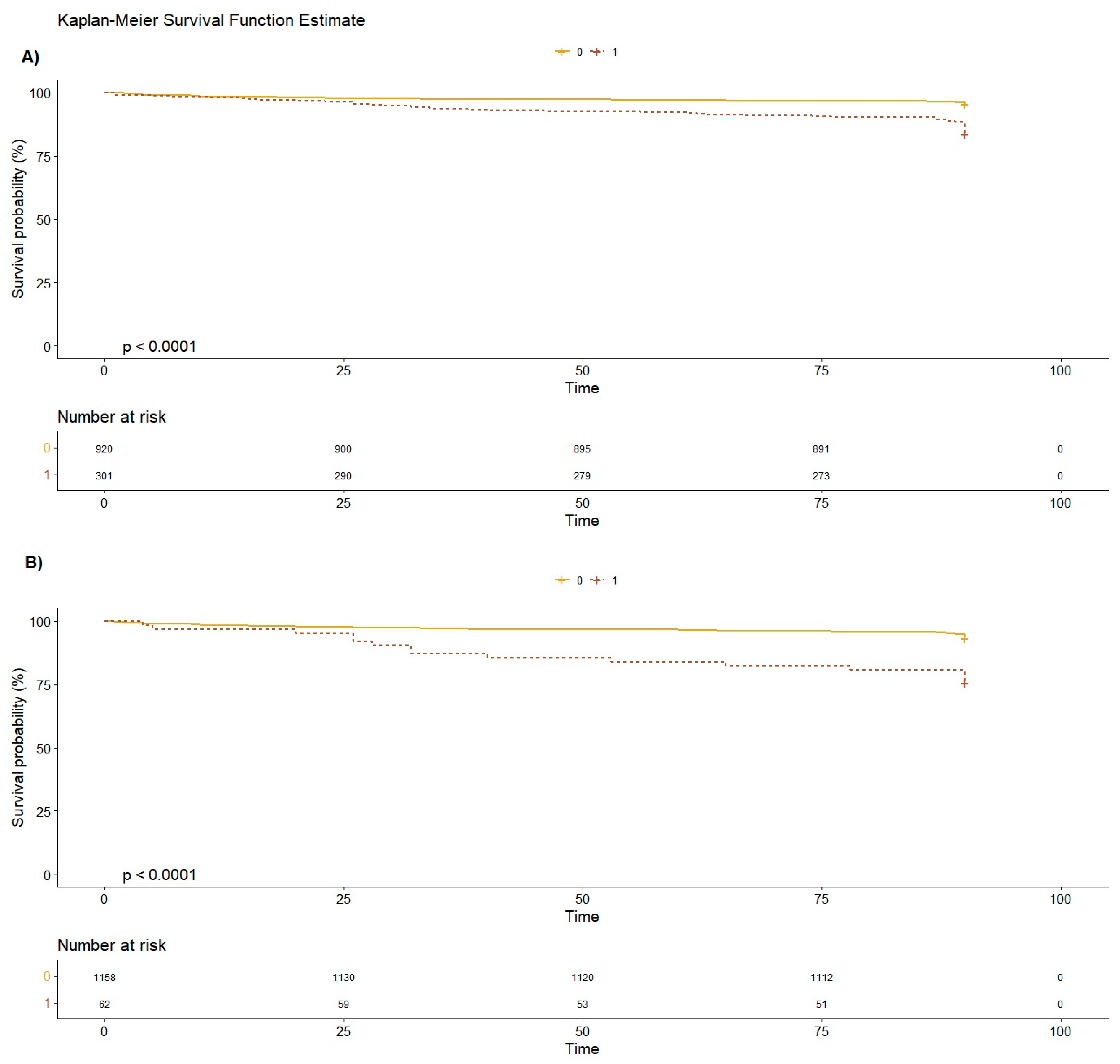
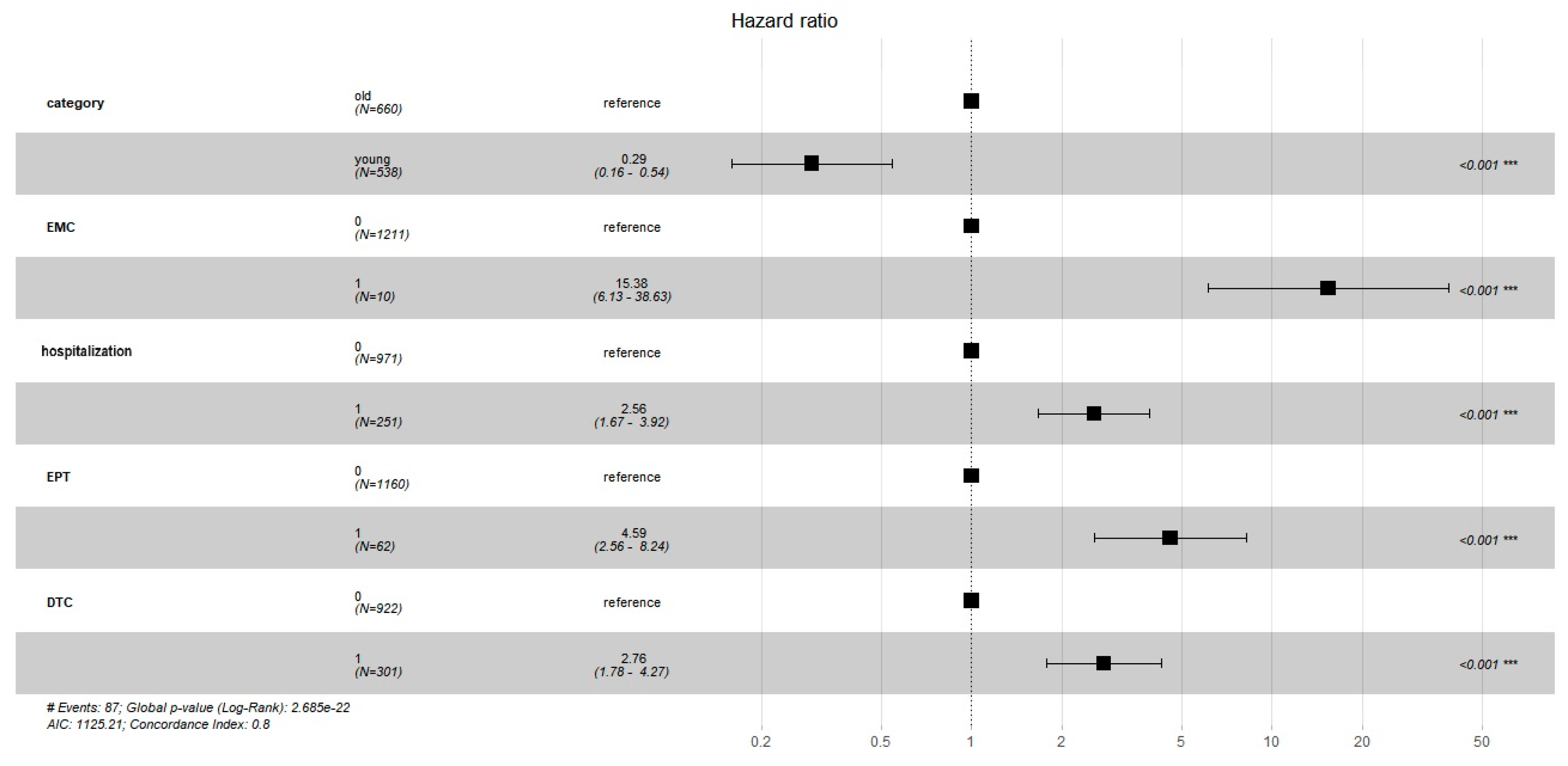
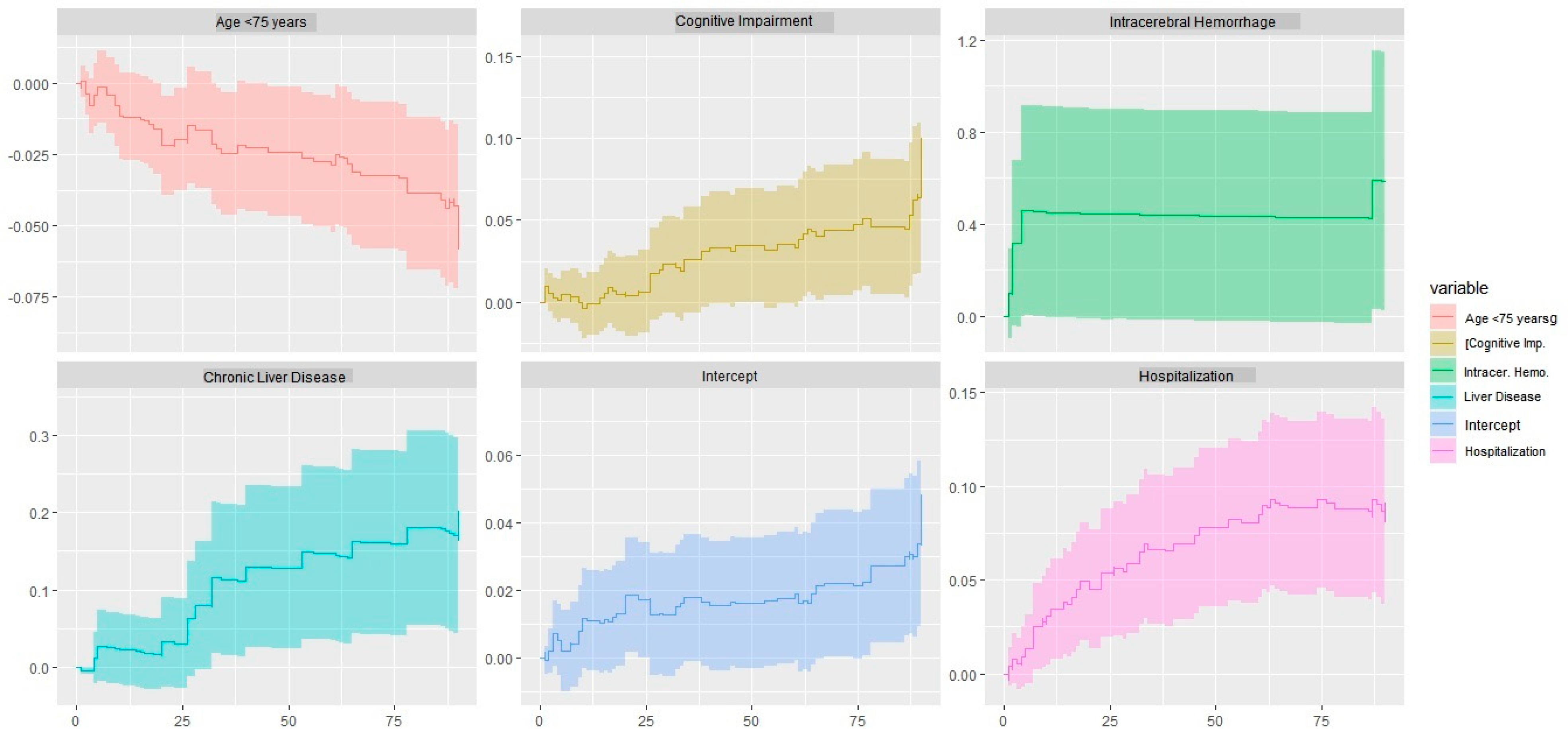
3. Results
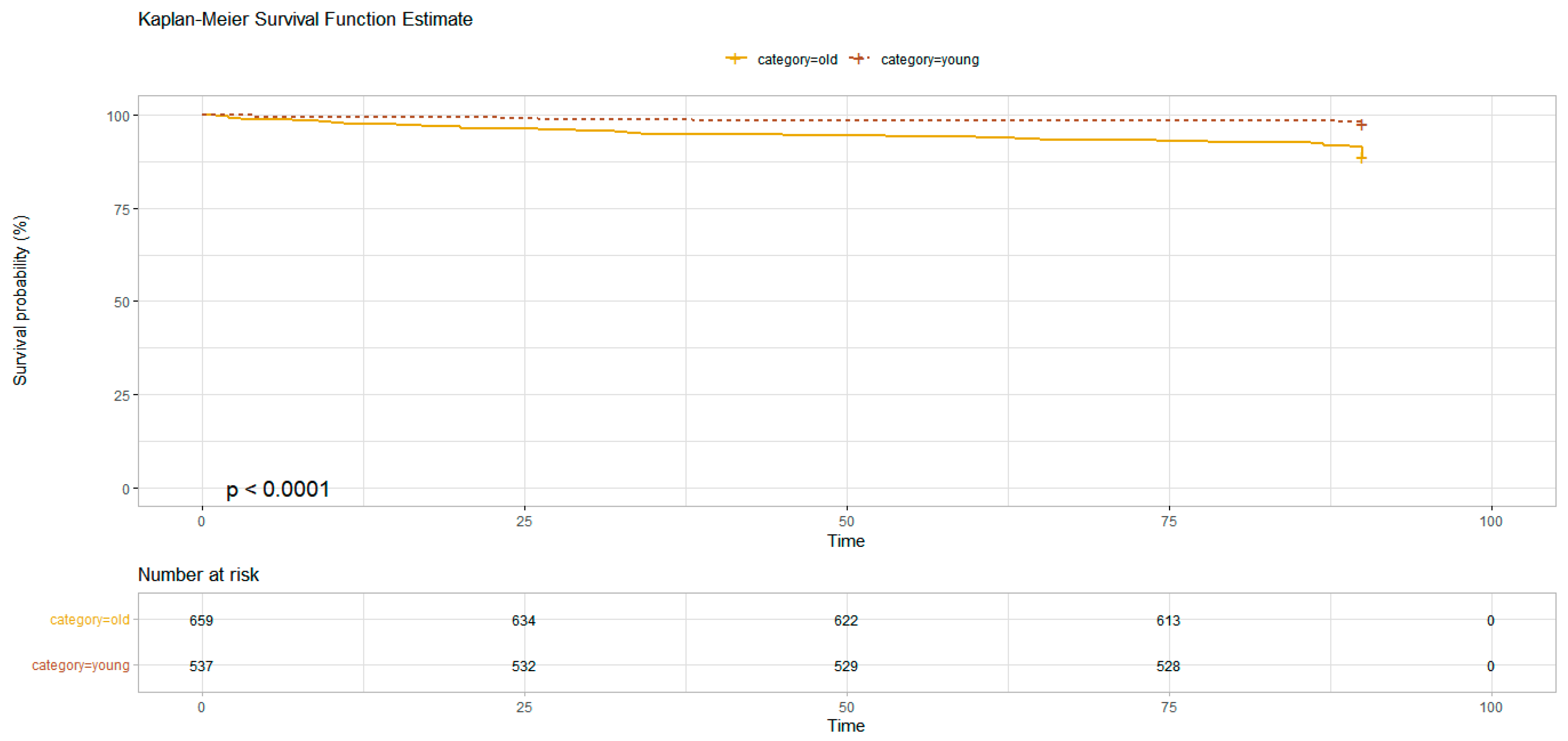
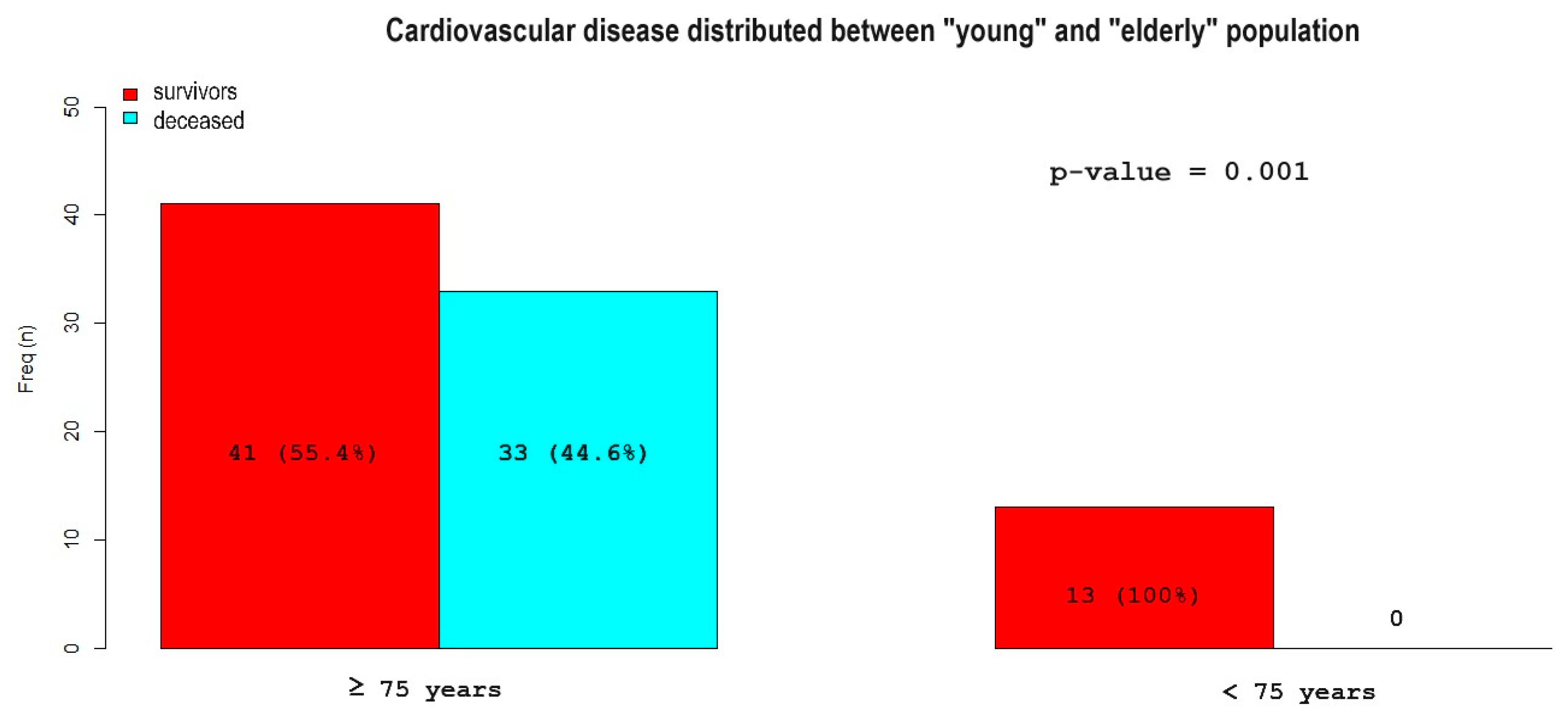
Age-Based Population Analysis
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Menon, D.K.; Schwab, K.; Wright, D.W.; Maas, A.I. Demographics and Clinical Assessment Working Group of the International and Interagency Initiative toward Common Data Elements for Research on Traumatic Brain Injury and Psychological Health. Position statement: Definition of traumatic brain injury. Arch. Phys. Med. Rehabil. 2010, 91, 1637–1640. [Google Scholar] [CrossRef] [PubMed]
- Sussman, E.S.; Pendharkar, A.V.; Ho, A.L.; Ghajar, J. Mild traumatic brain injury and concussion: Terminology and classification. Handb. Clin. Neurol. 2018, 158, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Kaur, P.; Sharma, S. Recent Advances in Pathophysiology of Traumatic Brain Injury. Curr. Neuropharmacol. 2018, 16, 1224–1238. [Google Scholar] [CrossRef] [PubMed]
- Mckee, A.C.; Daneshvar, D.H. The neuropathology of traumatic brain injury. Handb. Clin. Neurol. 2015, 127, 45–66. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.nice.org.uk/guidance/cg176/resources/head-injury-assessment-and-early-management-pdf-35109755595493 (accessed on 10 May 2021).
- Stiell, I.G.; Wells, G.A.; Vandemheen, K.; Clement, C.; Lesiuk, H.; Laupacis, A.; McKnight, R.D.; Verbeek, R.; Brison, R.; Cass, D.; et al. The Canadian CT Head Rule for patients with minor head injury. Lancet 2001, 357, 1391–1396. [Google Scholar] [CrossRef]
- Repplinger, M.D.; Li, A.J.; Svenson, J.E.; Ehlenbach, W.J.; Westergaard, R.P.; Reeder, S.B.; Jacobs, E.A. Emergency Department Patients’ Perceptions of Radiation From Medical Imaging. WMJ 2016, 115, 22–28. [Google Scholar]
- Steyerberg, E.W.; Wiegers, E.; Sewalt, C.; Buki, A.; Citerio, G.; De Keyser, V.; Ercole, A.; Kunzmann, K.; Lanyon, L.; Lecky, F.; et al. Case-mix, care pathways, and outcomes in patients with traumatic brain injury in CENTER-TBI: A European prospective, multicentre, longitudinal, cohort study. Lancet Neurol. 2019, 18, 923–934. [Google Scholar] [CrossRef]
- Groswasser, Z.; Peled, I. Survival and mortality following TBI. Brain Inj. 2018, 32, 149–157. [Google Scholar] [CrossRef]
- Leitner, L.; El-Shabrawi, J.H.; Bratschitsch, G.; Eibinger, N.; Klim, S.; Leithner, A.; Puchwein, P. Risk adapted diagnostics and hospitalization following mild traumatic brain injury. Arch. Orthop. Trauma Surg. 2021, 141, 619–627. [Google Scholar] [CrossRef]
- Ottochian, M.; Benfield, R.; Inaba, K.; Chan, L.S.; Demetriades, D. Prospective evaluation of a predictive model of mortality in patients with isolated head injury. J. Trauma 2009, 67, 81–84. [Google Scholar] [CrossRef]
- McMillan, T.M.; Weir, C.J.; Wainman-Lefley, J. Mortality and morbidity 15 years after hospital admission with mild head injury: A prospective case-controlled population study. J. Neurol. Neurosurg. Psychiatry 2014, 85, 1214–1220. [Google Scholar] [CrossRef]
- Popp, D.; Frankewycz, B.; Lang, S.; Ernstberger, A.; Alt, V.; Worlicek, M.; Kerschbaum, M. Are There Any Red Flag Injuries in Severely Injured Patients in Older Age? J. Clin. Med. 2021, 10, 185. [Google Scholar] [CrossRef]
- Castillo-Angeles, M.; Seshadri, A.J.; Benedict, L.A.; Patel, N.; Ramsis, R.; Askari, R.; Salim, A.; Nehra, D. Traumatic Brain Injury: Does Admission Service Matter? J. Surg. Res. 2021, 259, 211–216. [Google Scholar] [CrossRef]
- Naylor, R.M.; Henry, K.A.; Peters, P.A.; Bauman, M.M.J.; Lakomkin, N.; Van Gompel, J.J. High Long-Term Mortality Rate in Elderly Patients with Mild Traumatic Brain Injury and Subdural Hematoma due to Ground-Level Fall: Neurosurgery’s Hip Fracture? World Neurosurg. 2022, 167, e1122–e1127. [Google Scholar] [CrossRef]
- Lim, B.L.; Manaus, C.; Asians-Tan, M.L. Outcomes of warfarinized patients with minor head injury and normal initial CT scan. Am. J. Emerg. Med. 2016, 34, 75–78. [Google Scholar] [CrossRef]
- Afaneh, A.; Ford, J.; Gharzeddine, J.; Mazar, A.; Hayward, R.D.; Buck, J. Head injury on Warfarin: Likelihood of delayed intracranial bleeding in patients with negative initial head CT. BMC Res. Notes 2018, 11, 183. [Google Scholar] [CrossRef]
- Menditto, V.G.; Lucci, M.; Polonara, S.; Pomponio, G.; Gabrielli, A. Management of minor head injury in patients receiving oral anticoagulant therapy: A prospective study of a 24-hour observation protocol. Ann. Emerg. Med. 2012, 59, 451–455. [Google Scholar] [CrossRef]
- Stippler, M.; Smith, C.; McLean, A.R.; Carlson, A.; Morley, S.; Murray-Krizan, C.; Kraynik, J.; Kennedy, G. Utility of routine follow-up head CT scanning after mild traumatic brain injury: A systematic review of the literature. Emerg. Med. J. 2012, 29, 528–532. [Google Scholar] [CrossRef]
- Uccella, L.; Zoia, C.; Perlasca, F.; Bonetta, D.; Codecà, R.; Gaetani, P. Mild Traumatic Brain Injury in Patients on Long-Term Anticoagulation Therapy: Do They Really Need Repeated Head CT Scan? World Neurosurg. 2016, 93, 100–103. [Google Scholar] [CrossRef]
- Eroglu, S.E.; Onur, O.; Ozkaya, S.; Denızbasi, A.; Demır, H.; Ozpolat, C. Analysis of Repeated CT Scan Need in Blunt Head Trauma. Emerg. Med. Int. 2013, 2013, 916253. [Google Scholar] [CrossRef]
- Howlett, J.R.; Nelson, L.D.; Stein, M.B. Mental Health Consequences of Traumatic Brain Injury. Biol. Psychiatry 2022, 91, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Stocchetti, N.; Zanier, E.R. Chronic impact of traumatic brain injury on outcome and quality of life: A narrative review. Crit. Care 2016, 20, 148. [Google Scholar] [CrossRef] [PubMed]
- Elder, G.A. Update on TBI and Cognitive Impairment in Military Veterans. Curr. Neurol. Neurosci. Rep. 2015, 15, 68. [Google Scholar] [CrossRef] [PubMed]
- Pentland, B.; Hutton, L.S.; Jones, P.A. Late mortality after head injury. J. Neurol. Neurosurg. Psychiatry 2005, 76, 395–400. [Google Scholar] [CrossRef]
- Xiong, C.; Hanafy, S.; Chan, V.; Hu, Z.J.; Sutton, M.; Escobar, M.; Colantonio, A.; Mollayeva, T. Comorbidity in adults with traumatic brain injury and all-cause mortality: A systematic review. BMJ Open 2019, 9, e029072. [Google Scholar] [CrossRef] [PubMed]
- Hanafy, S.; Xiong, C.; Chan, V.; Sutton, M.; Escobar, M.; Colantonio, A.; Mollayeva, T. Comorbidity in traumatic brain injury and functional outcomes: A systematic review. Eur. J. Phys. Rehabil. Med. 2021, 57, 535–550. [Google Scholar] [CrossRef]
- Chandi, S.; Dekeseredy, P.; Brandmeir, N.J.; Fang, W.; Sedney, C.L. Traumatic brain injury in college students and the influence of alcohol consumption: A retrospective review from a rural state. J. Neurosci. Rural Pract. 2023, 14, 298–301. [Google Scholar] [CrossRef]
- Kornblith, E.; Bahorik, A.; Li, Y.; Peltz, C.B.; Barnes, D.E.; Yaffe, K. Traumatic brain injury, cardiovascular disease, and risk of dementia among older US Veterans. Brain Inj. 2022, 36, 628–632. [Google Scholar] [CrossRef]
- Cheng, P.L.; Lin, H.Y.; Lee, Y.K.; Hsu, C.Y.; Lee, C.C.; Su, Y.C. Higher mortality rates among the elderly with mild traumatic brain injury: A nationwide cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 7. [Google Scholar] [CrossRef]
- Lu, Y.; Jarrahi, A.; Moore, N.; Bartoli, M.; Brann, D.W.; Baban, B.; Dhandapani, K.M. Inflammaging, cellular senescence, and cognitive aging after traumatic brain injury. Neurobiol. Dis. 2023, 180, 106090. [Google Scholar] [CrossRef]
- Ostermann, R.C.; Joestl, J.; Tiefenboeck, T.M.; Lang, N.; Platzer, P.; Hofbauer, M. Risk factors predicting prognosis and outcome of elderly patients with isolated traumatic brain injury. J. Orthop. Surg. Res. 2018, 13, 277. [Google Scholar] [CrossRef] [PubMed]
- Selassie, A.W.; Fakhry, S.M.; Ford, D.W. Population-based study of the risk of in-hospital death after traumatic brain injury: The role of sepsis. J. Trauma 2011, 71, 1226–1234. [Google Scholar] [CrossRef] [PubMed]
- Gioffrè-Florio, M.; Murabito, L.M.; Visalli, C.; Pergolizzi, F.P.; Famà, F. Trauma in elderly patients: A study of prevalence, comorbidities, and gender differences. G. Chir. 2018, 39, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Elkbuli, A.; Smith, Z.; Shaikh, S.; Hai, S.; McKenney, M.; Boneva, D. Mild and Moderate Traumatic Brain Injury and Gender-Based Critical Care Outcomes. World J. Surg. 2020, 44, 1492–1497. [Google Scholar] [CrossRef]
- Nederpelt, C.J.; van der Aalst, S.J.M.; Rosenthal, M.G.; Krijnen, P.; Huisman, M.V.; Peul, W.C.; Schipper, I.B. Consequences of pre-injury utilization of direct oral anticoagulants in patients with traumatic brain injury: A systematic review and meta-analysis. J. Trauma Acute Care Surg. 2020, 88, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Santing, J.A.L.; Lee, Y.X.; van der Naalt, J.; van den Brand, C.L.; Jellema, K. Mild Traumatic Brain Injury in Elderly Patients Receiving Direct Oral Anticoagulants: A Systematic Review and Meta-Analysis. J. Neurotrauma 2022, 39, 458–472. [Google Scholar] [CrossRef]
- Hickey, S.; Hickman, Z.L.; Conway, J.; Giwa, A. The Effect of Direct Oral Anti-Coagulants on Delayed Traumatic Intracranial Hemorrhage After Mild Traumatic Brain Injury: A Systematic Review. J. Emerg. Med. 2021, 60, 321–330. [Google Scholar] [CrossRef]
- O’Brien, T.; Mitra, B.; Le Sage, N.; Tardif, P.A.; Emond, M.; D’Astous, M.; Mercier, E. Clinically significant traumatic intracranial hemorrhage following minor head trauma in older adults: A retrospective cohort study. Brain Inj. 2020, 34, 834–839. [Google Scholar] [CrossRef]
- Vehviläinen, J.; Virta, J.J.; Skrifvars, M.B.; Reinikainen, M.; Bendel, S.; Ala-Kokko, T.; Hoppu, S.; Laitio, R.; Siironen, J.; Raj, R. Effect of antiplatelet and anticoagulant medication use on injury severity and mortality in patients with traumatic brain injury treated in the intensive care unit. Acta Neurochir. 2023, 165, 4003–4012. [Google Scholar] [CrossRef] [PubMed]
- Fakhry, S.M.; Morse, J.L.; Garland, J.M.; Wilson, N.Y.; Shen, Y.; Wyse, R.J.; Watts, D.D. Antiplatelet and anticoagulant agents have minimal impact on traumatic brain injury incidence, surgery, and mortality in geriatric ground level falls: A multi-institutional analysis of 33,710 patients. J. Trauma Acute Care Surg. 2021, 90, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Hussein, W.; Mullins, P.M.; Alghamdi, K.; Sarani, B.; Pines, J.M. Trends in advanced computed tomography use for injured patients in United States emergency departments: 2007–2010. Acad. Emerg. Med. 2015, 22, 663–669. [Google Scholar] [CrossRef]
- Yun, B.J.; Borczuk, P.; Zachrison, K.S.; Goldstein, J.N.; Berlyand, Y.; Raja, A.S. Utilization of head CT during injury visits to United States emergency departments: 2012–2015. Am. J. Emerg. Med. 2018, 36, 1463–1466. [Google Scholar] [CrossRef]
- Pandor, A.; Goodacre, S.; Harnan, S.; Holmes, M.; Pickering, A.; Fitzgerald, P.; Rees, A.; Stevenson, M. Diagnostic management strategies for adults and children with minor head injury: A systematic review and an economic evaluation. Health Technol. Assess. 2011, 15, 1–202. [Google Scholar] [CrossRef]
- Holmes, M.W.; Goodacre, S.; Stevenson, M.D.; Pandor, A.; Pickering, A. The cost-effectiveness of diagnostic management strategies for adults with minor head injury. Injury 2012, 43, 1423–1431. [Google Scholar] [CrossRef] [PubMed]
- Smits, M.; Dippel, D.W.; Nederkoorn, P.J.; Dekker, H.M.; Vos, P.E.; Kool, D.R.; van Rijssel, D.A.; Hofman, P.A.; Twijnstra, A.; Tanghe, H.L.; et al. Minor head injury: CT-based strategies for management—A cost-effectiveness analysis. Radiology 2010, 254, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Easter, J.S.; Haukoos, J.S.; Meehan, W.P.; Novack, V.; Edlow, J.A. Will Neuroimaging Reveal a Severe Intracranial Injury in This Adult With Minor Head Trauma?: The Rational Clinical Examination Systematic Review. JAMA 2015, 314, 2672–2681, Erratum in JAMA 2017, 317, 2021. [Google Scholar] [CrossRef] [PubMed]
| Alive | Deceased | Hazard Ratio (95%CI) | p-Value | ||
|---|---|---|---|---|---|
| N = 1131 | N = 90 | ||||
| Demographic characteristics | |||||
| Age (years) [IQR] | 77 (57–85) | 88 (80–91) | 1.07 (1.05–1.09) | <0.001 | |
| Sex (males) (%) | 504 (45%) | 38 (42%) | 0.92 (0.60–1.40) | 0.696 | |
| Clinical history | |||||
| Arterial Hypertension (%) | 499 (44%) | 54 (60%) | 1.85 (1.21–2.82) | 0.004 | |
| Diabetes Mellitus (%) | 162 (14%) | 25 (28%) | 2.17 (1.37–3.44) | 0.001 | |
| Chronic Kidney Disease (%) | 111 (10%) | 19 (21%) | 2.38 (1.43–3.95) | 0.001 | |
| Alcoholism (%) | 83 (7%) | 6 (7%) | 0.90 (0.39–2.05) | 0.790 | |
| Chronic obstructive pulmonary disease (%) | 63 (6%) | 11 (12%) | 2.26 (1.20–4.25) | 0.009 | |
| Chronic Liver Disease (%) | 47 (4%) | 15 (17%) | 4.12 (2.37–7.18) | <0.001 | |
| Cardiac Disease (%) | 336 (30%) | 34 (38%) | 1.41 (0.92–2.15) | 0.116 | |
| Frequent Falls (%) | 236 (21%) | 38 (42%) | 2.59 (1.71–3.94) | <0.001 | |
| Cognitive Impairment (%) | 252 (22%) | 49 (54%) | 3.83 (2.53–5.81) | <0.001 | |
| Blood thinning medication | |||||
| Vitamin K antagonists (%) | 112 (10%) | 7 (8%) | 0.77 (0.36–1.67) | 0.515 | |
| Direct oral anticoagulants (%) | 57 (5%) | 3 (3%) | 0.65 (0.21–2.06) | 0.458 | |
| Low molecular weight heparin (or fondaparinux) (%) | 9 (1%) | 3 (3%) | 3.81 (1.20–12.0) | 0.015 | |
| Acetylsalicylic acid (%) | 191 (17%) | 16 (18%) | 1.07 (0.62–1.83) | 0.807 | |
| Clopidogrel (%) | 38 (3%) | 3 (3%) | 1.00 (0.32–1.83) | 0.998 | |
| Blood tests | |||||
| INR [IQR] | 1.07 [1.00–1.26] | 1.13 [1.03–1.28] | 0.97 (0.60–1.56) | 0.896 | |
| Platelets (count × 103/mm3) [IQR] | 218 [178–264] | 226 [184–286] | 1.00 (1.00–1.01) | 0.131 | |
| Blood Alcohol (g/L) [IQR] | 1.31 [0.10–2.84] | 0.10 [0.10–0.10] | 0.40 (0.12–1.39) | 0.151 | |
| Level of consciousness | |||||
| Glasgow Coma Scale [IQR] | 15 [15–15] | 15 [15–15] | 0.59 (0.28–1.21) | 0.149 | |
| Symptoms | |||||
| Amnesia (%) | 91 (8%) | 8 (9%) | 1.13 (0.55–2.34) | 0.741 | |
| Loss of Consciousness (%) | 92 (8%) | 4 (4%) | 0.54 (0.20–1.46) | 0.214 | |
| Vomiting (%) | 27 (2%) | 1 (1%) | 0.48 (0.07–3.43) | 0.453 | |
| Headache (%) | 85 (8%) | 0 (0%) | 0 | 0.008 | |
| Focal Neurological Deficit (%) | 13 (1%) | 1 (1%) | 1.01 (0.14–7.27) | 0.989 | |
| Confusion (%) | 113 (10%) | 23 (26%) | 2.98 (1.85–4.79) | <0.001 | |
| High Energy Impact | |||||
| High Energy Impact * (%) | 59 (5%) | 1 (1%) | 0.21 (0.03–1.54) | 0.092 | |
| Associated injuries | |||||
| Distal Upper Limb Fracture (%) | 46 (4%) | 4 (4%) | 1.09 (0.40–2.97) | 0.866 | |
| Proximal Upper Limb Fracture (%) | 43 (4%) | 1 (1%) | 0.29 (0.04–2.12) | 0.196 | |
| Rib fractures (%) | 36 (3%) | 2 (2%) | 0.71 (0.17–2.87) | 0.626 | |
| 1 rib (%) | 15 (1%) | 1 (1%) | |||
| 2 ribs (%) | 10 (1%) | 0 (0%) | |||
| ≥3 ribs (%) | 10 (1%) | 1 (1%) | |||
| Spine fracture (%) | 25 (2%) | 3 (3%) | 1.55 (0.49–4.89) | 0.452 | |
| Shoulder Girdle Fracture (%) | 9 (1%) | 1 (1%) | 1.45 (0.20–10.4) | 0.711 | |
| Pelvic fracture (%) | 12 (1%) | 3 (3%) | 2.89 (0.92–9.15) | 0.061 | |
| Distal Lower Limb Fracture (%) | 17 (2%) | 1 (1%) | 0.74 (0.10–5.31) | 0.765 | |
| Proximal Lower Limb Fracture (%) | 35 (3%) | 7 (8%) | 2.52 (1.16–5.44) | 0.015 | |
| Abdominal Trauma (%) | 13 (1%) | 0 (0%) | 0 | 0.315 | |
| Facial Fracture (%) | 86 (8%) | 5 (6%) | 0.72 (0.29–1.77) | 0.471 | |
| Neurocranium Fracture (%) | 14 (1%) | 1 (1%) | 0.92 (0.13–6.63) | 0.938 | |
| Head CT scan | |||||
| Subdural Hematoma (%) | 27 (2%) | 3 (3%) | 1.37 (0.43–4.34) | 0.586 | |
| Brain Contusion (%) | 17 (2%) | 0 (0%) | 0 | 0.250 | |
| Hemorrhagic Petechiae (%) | 14 (1%) | 1 (1%) | 0.92 (0.13–6.59) | 0.933 | |
| Intracerebral Hemorrhage (%) | 5 (0.4%) | 5 (6%) | 11.5 (4.68–28.4) | <0.001 | |
| Subarachnoid Hemorrhage (%) | 28 (2%) | 1 (1%) | 0.46 (0.06–3.29) | 0.427 | |
| Clinical management | |||||
| Hospitalization (%) | 212 (19%) | 39 (43%) | 3.17 (2.09–4.81) | <0.001 | |
| Discharge (%) | 798 (71%) | 51 (57%) | 0.55 (0.36–0.84) | 0.004 | |
| Abandonment (%) | 88 (8%) | 1 (1%) | 0.14 (0.02–0.99) | 0.021 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orso, D.; Furlanis, G.; Romanelli, A.; Gheller, F.; Tecchiolli, M.; Cominotto, F. Risk Factors Analysis for 90-Day Mortality of Adult Patients with Mild Traumatic Brain Injury in an Italian Emergency Department. Geriatrics 2024, 9, 23. https://doi.org/10.3390/geriatrics9020023
Orso D, Furlanis G, Romanelli A, Gheller F, Tecchiolli M, Cominotto F. Risk Factors Analysis for 90-Day Mortality of Adult Patients with Mild Traumatic Brain Injury in an Italian Emergency Department. Geriatrics. 2024; 9(2):23. https://doi.org/10.3390/geriatrics9020023
Chicago/Turabian StyleOrso, Daniele, Giulia Furlanis, Alice Romanelli, Federica Gheller, Marzia Tecchiolli, and Franco Cominotto. 2024. "Risk Factors Analysis for 90-Day Mortality of Adult Patients with Mild Traumatic Brain Injury in an Italian Emergency Department" Geriatrics 9, no. 2: 23. https://doi.org/10.3390/geriatrics9020023
APA StyleOrso, D., Furlanis, G., Romanelli, A., Gheller, F., Tecchiolli, M., & Cominotto, F. (2024). Risk Factors Analysis for 90-Day Mortality of Adult Patients with Mild Traumatic Brain Injury in an Italian Emergency Department. Geriatrics, 9(2), 23. https://doi.org/10.3390/geriatrics9020023






