Associations of Lower-Limb Phase Angle with Locomotion and Motor Function in Japanese Community-Dwelling Older Adults
Abstract
:1. Introduction
2. Materials and Methods
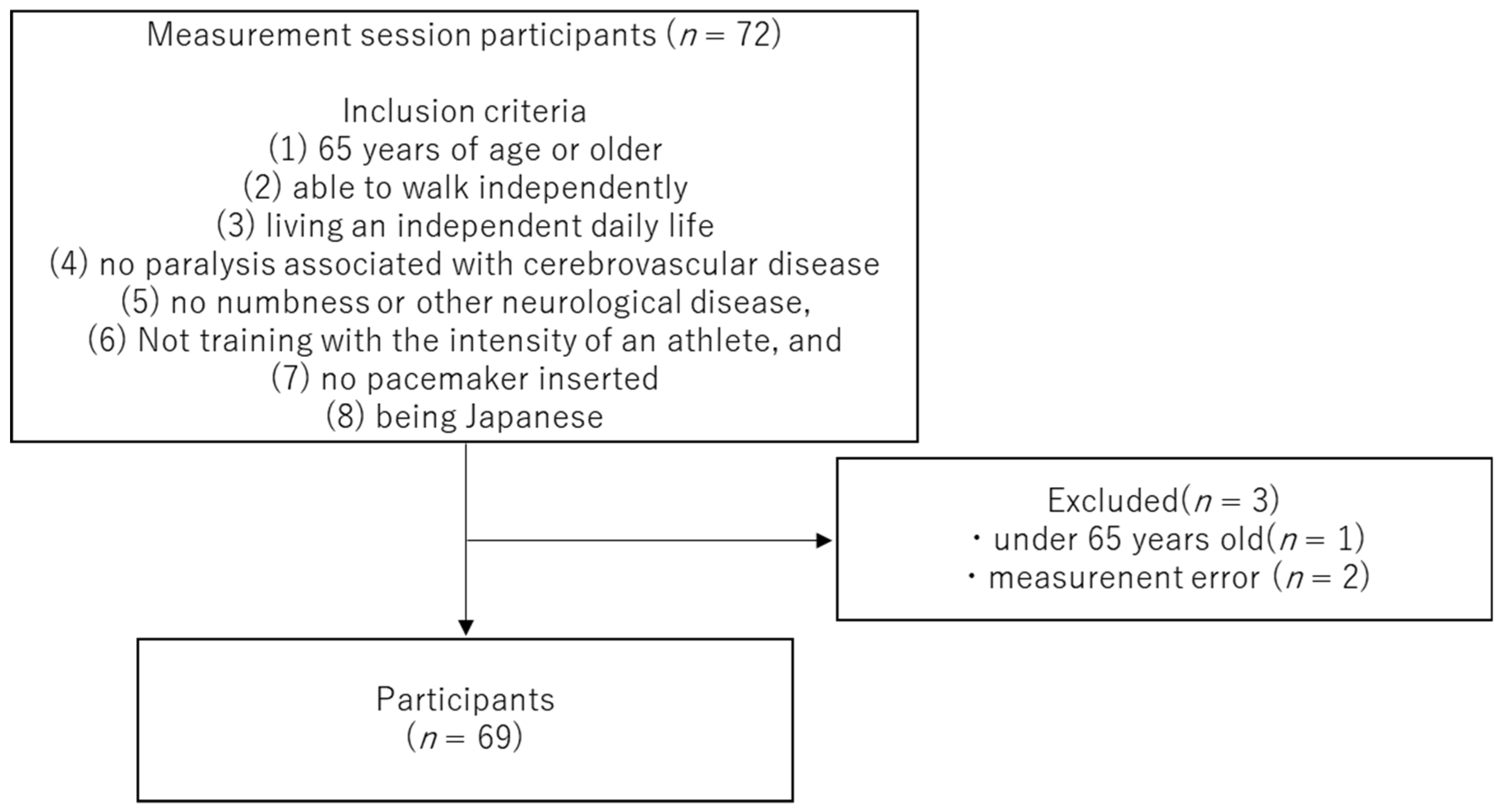
2.1. Participants
2.2. Study Design and Measurement Items
2.3. Phase Angle
2.4. Grip Strength
2.5. TUG
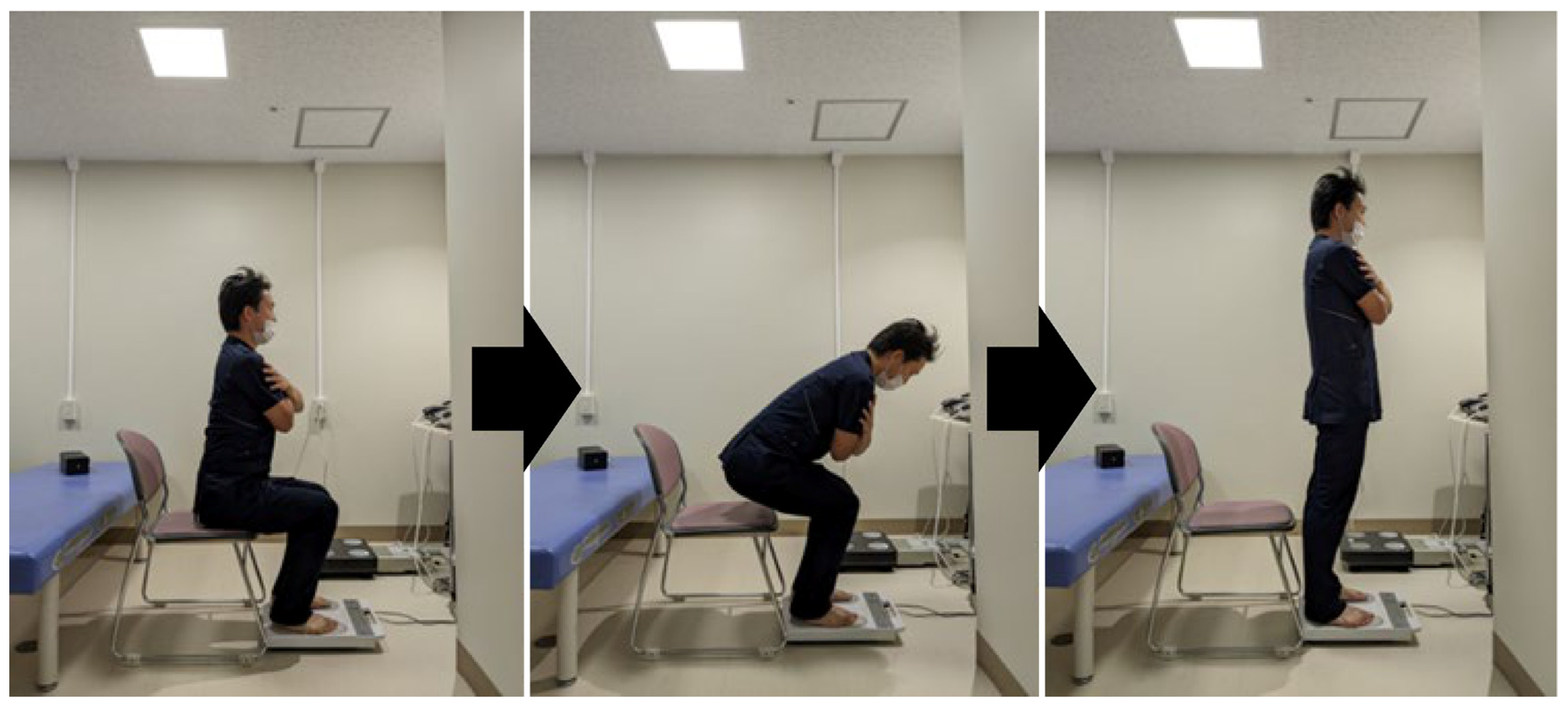
2.6. Floor Reaction Force Index during Standing Up
2.7. Questionnaire
2.8. Statistical Analysis
2.9. Ethical Considerations
3. Results
3.1. Basic Information on Participants and PA
3.2. Relationship between PhA and Measured Items
3.3. Multiple Regression Analysis
4. Discussion
4.1. Findings Obtained in This Study
4.2. Basic Information about the Participants and Relationship between PhA and Other Parameters
4.3. Clinical Applications and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gu, D.; Andreev, K.; Dupre, M.E. Major Trends in Population Growth Around the World. China CDC Wkly. 2021, 3, 604–613. [Google Scholar] [CrossRef] [PubMed]
- Murayama, H.; Kobayashi, E.; Okamoto, S.; Fukaya, T.; Ishizaki, T.; Liang, J.; Shinkai, S. National Prevalence of Frailty in the Older Japanese Population: Findings from a Nationally Representative Survey. Arch. Gerontol. Geriatr. 2020, 91, 104220. [Google Scholar] [CrossRef]
- Cheng, X.; Yang, Y.; Schwebel, D.C.; Liu, Z.; Li, L.; Cheng, P.; Ning, P.; Hu, G. Population Ageing and Mortality During 1990–2017: A Global Decomposition Analysis. PLoS Med. 2020, 17, e1003138. [Google Scholar] [CrossRef]
- Slee, A.; Birc, D.; Stokoe, D. Bioelectrical Impedance Vector Analysis, Phase-Angle Assessment and Relationship with Malnutrition Risk in a Cohort of Frail Older Hospital Patients in the United Kingdom. Nutrition 2015, 31, 132–137. [Google Scholar] [CrossRef]
- Nakamura, K. A “Super-Aged” Society and the “Locomotive Syndrome”. J. Orthop. Sci. 2008, 13, 1–2. [Google Scholar] [CrossRef]
- Nakamura, K. The Concept and Treatment of Locomotive Syndrome: Its Acceptance and Spread in Japan. J. Orthop. Sci. 2011, 16, 489–491. [Google Scholar] [CrossRef]
- Chen, L.K.; Liu, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Bahyah, K.S.; Chou, M.Y.; Chen, L.Y.; Hsu, P.S.; Krairit, O.; et al. Sarcopenia in Asia: Consensus Report of the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 2014, 15, 95–101. [Google Scholar] [CrossRef]
- Karampinos, D.C.; Baum, T.; Nardo, L.; Alizai, H.; Yu, H.; Carballido-Gamio, J.; Yap, S.P.; Shimakawa, A.; Link, T.M.; Majumdar, S. Characterization of the Regional Distribution of Skeletal Muscle Adipose Tissue in Type 2 Diabetes Using Chemical Shift-Based Water/Fat Separation. J. Magn. Reson. Imaging 2012, 35, 899–907. [Google Scholar] [CrossRef]
- Hamaguchi, Y.; Kaido, T.; Okumura, S.; Kobayashi, A.; Shirai, H.; Yagi, S.; Kamo, N.; Okajima, H.; Uemoto, S. Impact of Skeletal Muscle Mass Index, Intramuscular Adipose Tissue Content, and Visceral to Subcutaneous Adipose Tissue Area Ratio on Early Mortality of Living Donor Liver Transplantation. Transplantation 2017, 101, 565–574. [Google Scholar] [CrossRef]
- Goodpaster, B.H.; Kelley, D.E.; Thaete, F.L.; He, J.; Ross, R. Skeletal Muscle Attenuation Determined by Computed Tomography Is Associated with Skeletal Muscle Lipid Content. J. Appl. Physiol. 2000, 89, 104–110. [Google Scholar] [CrossRef]
- Akamatsu, Y.; Kusakabe, T.; Arai, H.; Yamamoto, Y.; Nakao, K.; Ikeue, K.; Ishihara, Y.; Tagami, T.; Yasoda, A.; Ishii, K.; et al. Phase Angle from Bioelectrical Impedance Analysis Is a Useful Indicator of Muscle Quality. J. Cachexia Sarcopenia Muscle 2022, 13, 180–189. [Google Scholar] [CrossRef]
- Fukumoto, Y.; Ikezoe, T.; Yamada, Y.; Tsukagoshi, R.; Nakamura, M.; Mori, N.; Kimura, M.; Ichihashi, N. Skeletal Muscle Quality Assessed from Echo Intensity Is Associated with Muscle Strength of Middle-Aged and Elderly Persons. Eur. J. Appl. Physiol. 2012, 112, 1519–1525. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Manuel Gómez, J.; Lilienthal Heitmann, B.; Kent-Smith, L.; Melchior, J.C.; Pirlich, M.; et al. Bioelectrical Impedance Analysis-Part II: Utilization in Clinical Practice. Clin. Nutr. 2004, 23, 1430–1453. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Stobäus, N.; Pirlich, M.; Bosy-Westphal, A. Bioelectrical Phase Angle and Impedance Vector Analysis—Clinical Relevance and Applicability of Impedance Parameters. Clin. Nutr. 2012, 31, 854–861. [Google Scholar] [CrossRef] [PubMed]
- Basile, C.; Della-Morte, D.; Cacciatore, F.; Gargiulo, G.; Galizia, G.; Roselli, M.; Curcio, F.; Bonaduce, D.; Abete, P. Phase Angle as Bioelectrical Marker to Identify Elderly Patients at Risk of Sarcopenia. Exp. Gerontol. 2014, 58, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Nishio, N.; Otobe, Y.; Tanaka, T.; Ohji, S.; Koyama, S.; Sato, A.; Suzuki, M.; et al. Phase Angle Is a Useful Indicator for Muscle Function in Older Adults. J. Nutr. Health Aging 2019, 23, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Campa, F.; Silva, A.M.; Toselli, S. Changes in Phase Angle and Handgrip Strength Induced by Suspension Training in Older Women. Int. J. Sports Med. 2018, 39, 442–449. [Google Scholar] [CrossRef]
- Uemura, K.; Doi, T.; Tsutsumimoto, K.; Nakakubo, S.; Kim, M.J.; Kurita, S.; Ishii, H.; Shimada, H. Predictivity of Bioimpedance Phase Angle for Incident Disability in Older Adults. J. Cachexia Sarcopenia Muscle 2020, 11, 46–54. [Google Scholar] [CrossRef]
- Tanaka, S.; Ando, K.; Kobayashi, K.; Seki, T.; Hamada, T.; Machino, M.; Ota, K.; Morozumi, M.; Kanbara, S.; Ito, S.; et al. Low Bioelectrical Impedance Phase Angle Is a Significant Risk Factor for Frailty. Biomed. Res. Int. 2019, 2019, 6283153. [Google Scholar] [CrossRef]
- Homma, D.; Minato, I.; Imai, N.; Miyasaka, D.; Sakai, Y.; Horigome, Y.; Suzuki, H.; Dohmae, Y.; Endo, N. Analysis of Phase Angle and Balance and Gait Functions in Pre-frail Individuals: A Cross-Sectional Observational Study. Acta Med. Okayama 2023, 77, 21–27. [Google Scholar] [CrossRef]
- Kobayashi, H.; Otani, K.; Nikaido, T.; Watanabe, K.; Kato, K.; Handa, J.; Yabuki, S.; Konno, S.I. Grip Strength as a Screening Index for Severe Degenerative Cervical Myelopathy in Primary Care: Development of Cutoff Values Using Receiver Operating Curve Analysis. Int. J. Gen. Med. 2021, 14, 9863–9872. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed “UP & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Kera, T.; Kawai, H.; Takahashi, J.; Hirano, H.; Watanabe, Y.; Fujiwara, Y.; Ihara, K.; Kim, H.; Obuchi, S. Association Between Ground Reaction Force in Sit-to-Stand Motion and Falls in Community-Dwelling Older Japanese Individuals. Arch. Gerontol. Geriatr. 2020, 91, 104221. [Google Scholar] [CrossRef]
- Sewo Sampaio, P.Y.; Sampaio, R.A.; Yamada, M.; Arai, H. Systematic Review of the Kihon Checklist: Is It a Reliable Assessment of Frailty? Geriatr. Gerontol. Int. 2016, 16, 893–902. [Google Scholar] [CrossRef]
- Seichi, A.; Hoshino, Y.; Doi, T.; Akai, M.; Tobimatsu, Y.; Iwaya, T. Development of a Screening Tool for Risk of Locomotive Syndrome in the Elderly: The 25-Question Geriatric Locomotive Function Scale. J. Orthop. Sci. 2012, 17, 163–172. [Google Scholar] [CrossRef]
- Hill, K.D.; Schwarz, J.A.; Kalogeropoulos, A.J.; Gibson, S.J. Fear of Falling Revisited. Arch. Phys. Med. Rehabil. 1996, 77, 1025–1029. [Google Scholar] [CrossRef]
- Baker, P.S.; Bodner, E.V.; Allman, R.M. Measuring Life-Space Mobility in Community-Dwelling Older Adults. J. Am. Geriatr. Soc. 2003, 51, 1610–1614. [Google Scholar] [CrossRef]
- Satake, S.; Senda, K.; Hong, Y.J.; Miura, H.; Endo, H.; Sakurai, T.; Kondo, I.; Toba, K. Validity of the Kihon Checklist for Assessing Frailty Status. Geriatr. Gerontol. Int. 2016, 16, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Uemura, K.; Yamada, M.; Okamoto, H. Association of Bioimpedance Phase Angle and Prospective Falls in Older Adults. Geriatr. Gerontol. Int. 2019, 19, 503–507. [Google Scholar] [CrossRef]
- Marzetti, E.; Calvani, R.; Bernabei, R.; Leeuwenburgh, C. Apoptosis in skeletal myocytes: A potential target for interventions against sarcopenia and physical frailty—A mini-review. Gerontology 2012, 58, 99–106. [Google Scholar] [CrossRef]
- Johnston, A.P.; De Lisio, M.; Parise, G. Resistance training, sarcopenia, and the mitochondrial theory of aging. Appl. Physiol. Nutr. Metab. 2008, 33, 191–199. [Google Scholar] [CrossRef]
- Degens, H.; Alway, S.E. Control of muscle size during disuse, disease, and aging. Int. J. Sports Med. 2006, 27, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Buford, T.W.; Anton, S.D.; Judge, A.R.; Marzetti, E.; Wohlgemuth, S.E.; Carter, C.S.; Leeuwenburgh, C.; Pahor, M.; Manini, T.M. Models of accelerated sarcopenia: Critical pieces for solving the puzzle of age-related muscle atrophy. Ageing Res. Rev. 2010, 9, 369–383. [Google Scholar] [CrossRef]
- Nilwik, R.; Snijders, T.; Leenders, M.; Groen, B.B.L.; van Kranenburg, J.; Verdijk, L.B.; van Loon, L.J.C. The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp. Gerontol. 2013, 48, 492–498. [Google Scholar] [CrossRef]
- Hughes, V.A.; Frontera, W.R.; Wood, M.; Evans, W.J.; Dallal, G.E.; Roubenoff, R.; Fiatarone Singh, M.A. Longitudinal Muscle Strength Changes in Older Adults: Influence of Muscle Mass, Physical Activity, and Health. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, B209–B217. [Google Scholar] [CrossRef] [PubMed]
- Kuh, D.; Bassey, E.J.; Butterworth, S.; Hardy, R.; Wadsworth, M.E.; Musculoskeletal Study Team. Grip Strength, Postural Control, and Functional Leg Power in a Representative Cohort of British Men and Women: Associations with Physical Activity, Health Status, and Socioeconomic Conditions. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 224–231. [Google Scholar] [CrossRef]
- Yamada, Y.; Buehring, B.; Krueger, D.; Anderson, R.M.; Schoeller, D.A.; Binkley, N. Electrical Properties Assessed by Bioelectrical Impedance Spectroscopy as Biomarkers of Age-Related Loss of Skeletal Muscle Quantity and Quality. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 72, 1180–1186. [Google Scholar] [CrossRef]

| Variable | Value |
|---|---|
| Age, years | 72.3 ± 5.7 |
| Height (cm) | 155 (152–162) |
| Weight (kg) | 54.7 (49.9–64) |
| Whole-body phase angle (°) | 4.7 ± 0.5 |
| Upper-limb phase angle (°) | 5.1 (4.8–5.6) |
| Lower-limb phase angle (°) | 4.2 ± 0.6 |
| Grip strength (kg) | 25.9 (23.4–29.2) |
| Timed Up and Go Test (seconds) | 6.1 (5.3–6.5) |
| F/w (kgf·kg−1) | 1.3 ± 0.1 |
| Kihon Checklist score (points) | 3 (1–4) |
| 25-Geriatric Locomotive Function Scale score (points) | 5 (2–12) |
| Life Space Assessment score (points) | 102 (92–120) |
| Modified Falls Efficacy Scale score (points) | 140 (138–140) |
| Grip Strength | Timed Up and Go Test | F/w | Kihon Checklist | 25-Geriatric Locomotive Function Scale Score | ||
|---|---|---|---|---|---|---|
| Whole-body phase angle | r | 0.621 | −0.014 | 0.431 | −0.074 | −0.294 |
| p | <0.001 * | 0.446 | <0.001 * | 0.549 | 0.015 * | |
| Upper-limb phase angle | r | 0.613 | 0.010 | 0.374 | −0.027 | −0.181 |
| p | <0.001 * | 0.938 | 0.002 * | 0.829 | 0.139 | |
| Lower-limb phase angle | r | 0.560 | −0.251 | 0.486 | −0.134 | −0.365 |
| p | <0.001 * | 0.039 * | <0.001 * | 0.274 * | 0.002 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Homma, D.; Minato, I.; Imai, N.; Miyasaka, D.; Horigome, Y.; Suzuki, H.; Dohmae, Y.; Endo, N. Associations of Lower-Limb Phase Angle with Locomotion and Motor Function in Japanese Community-Dwelling Older Adults. Geriatrics 2023, 8, 121. https://doi.org/10.3390/geriatrics8060121
Homma D, Minato I, Imai N, Miyasaka D, Horigome Y, Suzuki H, Dohmae Y, Endo N. Associations of Lower-Limb Phase Angle with Locomotion and Motor Function in Japanese Community-Dwelling Older Adults. Geriatrics. 2023; 8(6):121. https://doi.org/10.3390/geriatrics8060121
Chicago/Turabian StyleHomma, Daisuke, Izumi Minato, Norio Imai, Dai Miyasaka, Yoji Horigome, Hayato Suzuki, Yoichiro Dohmae, and Naoto Endo. 2023. "Associations of Lower-Limb Phase Angle with Locomotion and Motor Function in Japanese Community-Dwelling Older Adults" Geriatrics 8, no. 6: 121. https://doi.org/10.3390/geriatrics8060121
APA StyleHomma, D., Minato, I., Imai, N., Miyasaka, D., Horigome, Y., Suzuki, H., Dohmae, Y., & Endo, N. (2023). Associations of Lower-Limb Phase Angle with Locomotion and Motor Function in Japanese Community-Dwelling Older Adults. Geriatrics, 8(6), 121. https://doi.org/10.3390/geriatrics8060121






