Occurrence of Postoperative Delirium and the Use of Different Assessment Tools
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection and Endpoint Definition
2.3. Statistical Analysis
3. Results
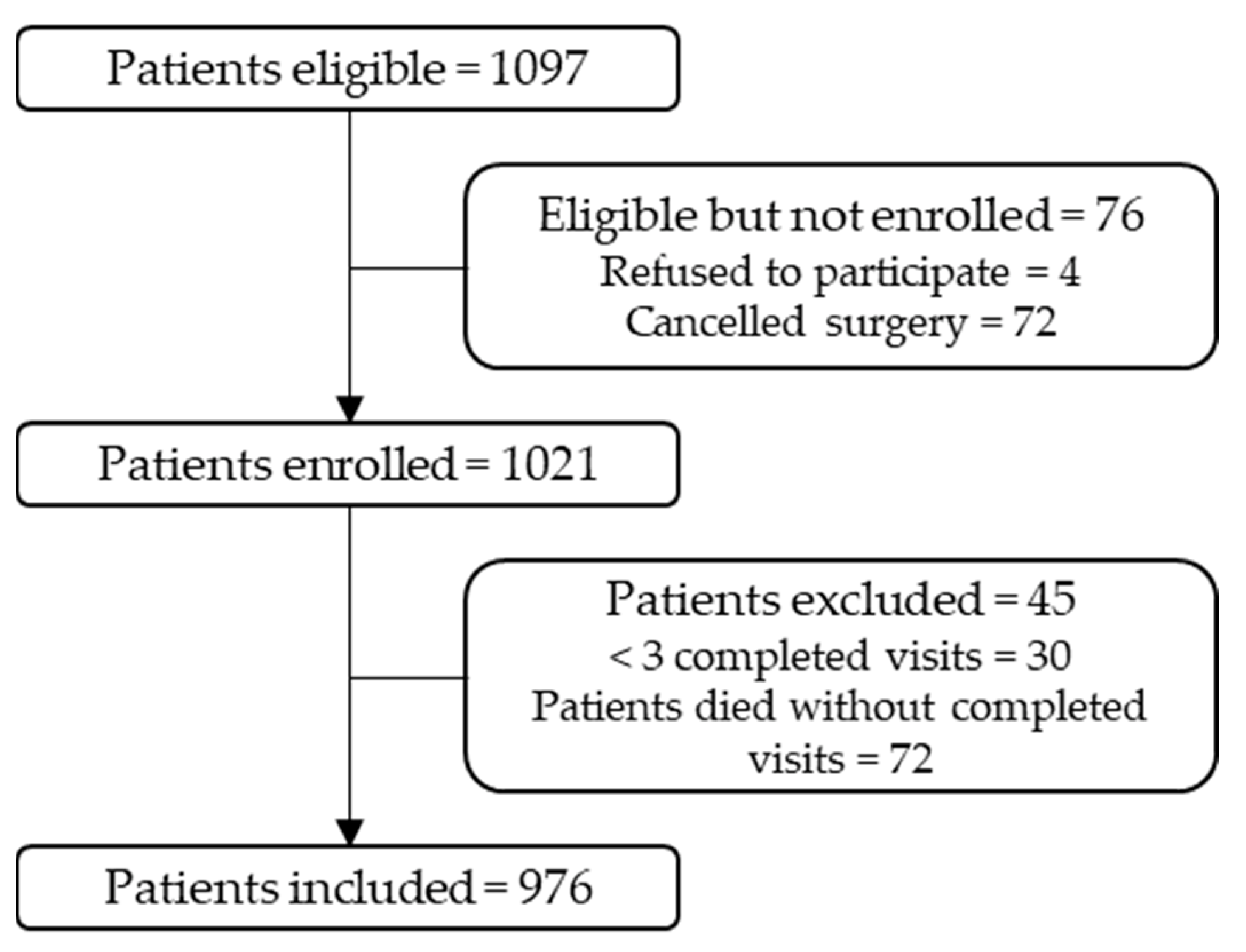
3.1. Participants
3.2. Characteristics
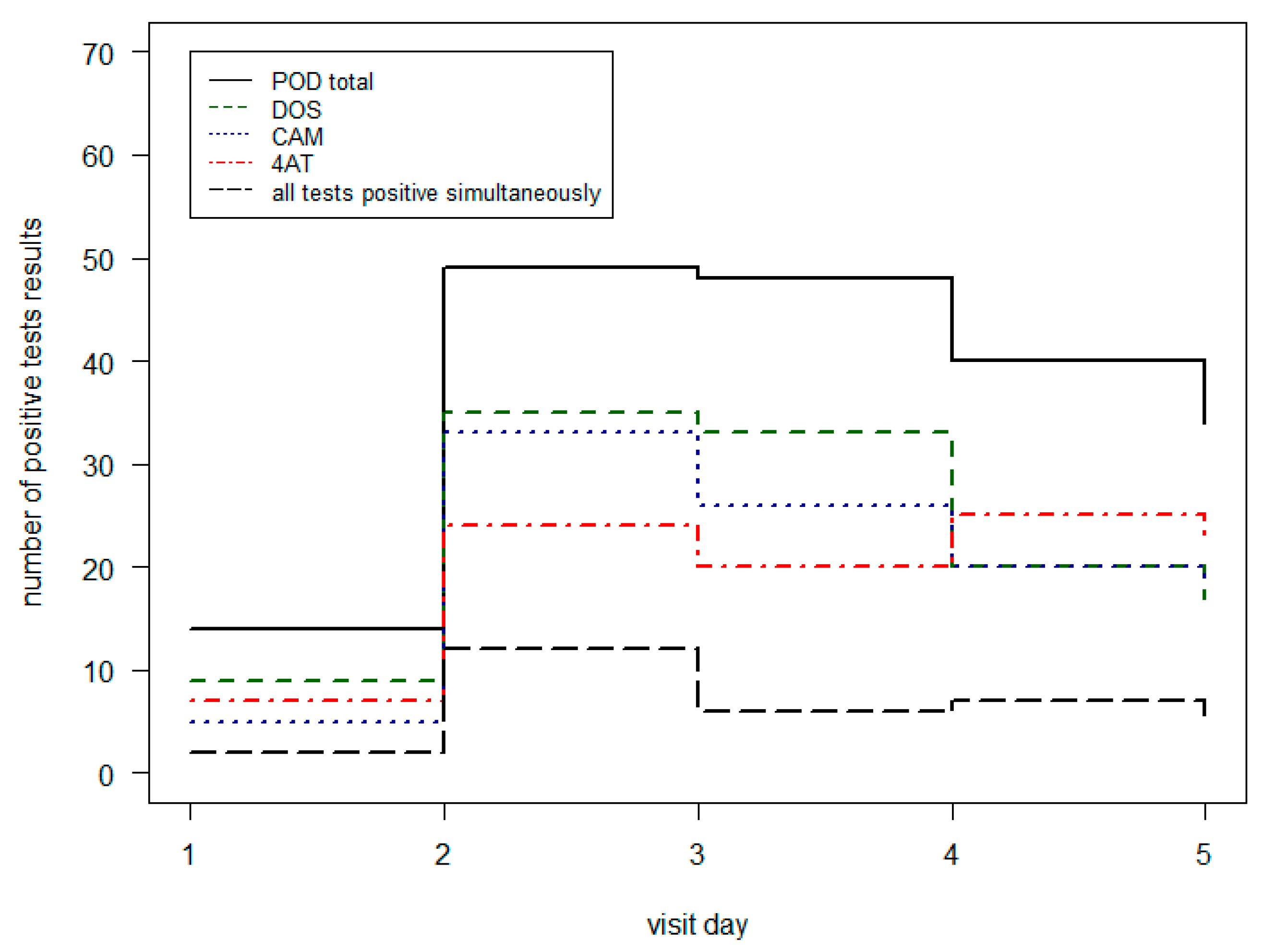
3.3. Visit Distribution and Occurrence of POD
3.4. Comparison of Different POD-Assessments
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. International Statistical Classification of Disease and Related Health Problems; 10th Revision; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013; ISBN 978-0-89042-555-8. [Google Scholar]
- Goldberg, T.E.; Chen, C.; Wang, Y.; Jung, E.; Swanson, A.; Ing, C.; Garcia, P.S.; Whittington, R.A.; Moitra, V. Association of Delirium With Long-Term Cognitive Decline: A Meta-Analysis. JAMA Neurol. 2020, 77, 1373. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K.; Westendorp, R.G.; Saczynski, J.S. Delirium in Elderly People. Lancet 2014, 383, 911–922. [Google Scholar] [CrossRef] [PubMed]
- Davis, D.H.J.; Muniz Terrera, G.; Keage, H.; Rahkonen, T.; Oinas, M.; Matthews, F.E.; Cunningham, C.; Polvikoski, T.; Sulkava, R.; MacLullich, A.M.J.; et al. Delirium Is a Strong Risk Factor for Dementia in the Oldest-Old: A Population-Based Cohort Study. Brain 2012, 135, 2809–2816. [Google Scholar] [CrossRef] [PubMed]
- Aldecoa, C.; Bettelli, G.; Bilotta, F.; Sanders, R.D.; Audisio, R.; Borozdina, A.; Cherubini, A.; Jones, C.; Kehlet, H.; MacLullich, A.; et al. European Society of Anaesthesiology Evidence-Based and Consensus-Based Guideline on Postoperative Delirium. Eur. J. Anaesthesiol. 2017, 34, 192–214. [Google Scholar] [CrossRef] [PubMed]
- Mc Donnell, S.; Timmins, F. A Quantitative Exploration of the Subjective Burden Experienced by Nurses When Caring for Patients with Delirium: Subjective Burden. J. Clin. Nurs. 2012, 21, 2488–2498. [Google Scholar] [CrossRef]
- Kirfel, A.; Guttenthaler, V.; Mayr, A.; Coburn, M.; Menzenbach, J.; Wittmann, M. Postoperative Delirium Is an Independent Factor Influencing the Length of Stay of Elderly Patients in the Intensive Care Unit and in Hospital. J. Anesth. 2022, 36, 341–348. [Google Scholar] [CrossRef]
- DAS-Taskforce 2015; Baron, R.; Binder, A.; Biniek, R.; Braune, S.; Buerkle, H.; Dall, P.; Demirakca, S.; Eckardt, R.; Eggers, V.; et al. Evidence and Consensus Based Guideline for the Management of Delirium, Analgesia, and Sedation in Intensive Care Medicine. Revision 2015 (DAS-Guideline 2015)—Short Version. GMS Ger. Med. Sci. 2015, 13, Doc19. [Google Scholar] [CrossRef]
- Hamadnalla, H.; Sessler, D.I.; Troianos, C.A.; Fang, J.; Rivas, E.; Ma, C.; Mascha, E.J.; Turan, A. Optimal Interval and Duration of CAM-ICU Assessments for Delirium Detection after Cardiac Surgery. J. Clin. Anesth. 2021, 71, 110233. [Google Scholar] [CrossRef]
- Katznelson, R.; Djaiani, G.N.; Borger, M.A.; Friedman, Z.; Abbey, S.E.; Fedorko, L.; Karski, J.; Mitsakakis, N.; Carroll, J.; Beattie, W.S. Preoperative Use of Statins Is Associated with Reduced Early Delirium Rates after Cardiac Surgery. Anesthesiology 2009, 110, 67–73. [Google Scholar] [CrossRef]
- Katznelson, R.; Djaiani, G.; Tait, G.; Wasowicz, M.; Sutherland, A.M.; Styra, R.; Lee, C.; Beattie, W.S. Hospital Administrative Database Underestimates Delirium Rate after Cardiac Surgery. Can. J. Anesth./J. Can. Anesth. 2010, 57, 898–902. [Google Scholar] [CrossRef]
- Adamis, D.; Meagher, D.; Murray, O.; O’Neill, D.; O’Mahony, E.; Mulligan, O.; McCarthy, G. Evaluating Attention in Delirium: A Comparison of Bedside Tests of Attention. Geriatr. Gerontol. Int. 2016, 16, 1028–1035. [Google Scholar] [CrossRef]
- Brefka, S.; Eschweiler, G.W.; Dallmeier, D.; Denkinger, M.; Leinert, C. Comparison of Delirium Detection Tools in Acute Care: A Rapid Review. Z. Gerontol. Geriat. 2022, 55, 105–115. [Google Scholar] [CrossRef]
- van Velthuijsen, E.L.; Zwakhalen, S.M.G.; Warnier, R.M.J.; Mulder, W.J.; Verhey, F.R.J.; Kempen, G.I.J.M. Psychometric Properties and Feasibility of Instruments for the Detection of Delirium in Older Hospitalized Patients: A Systematic Review: Review of Delirium Scales for Hospitalized Elderly. Int. J. Geriatr. Psychiatry 2016, 31, 974–989. [Google Scholar] [CrossRef]
- The American Geriatrics Society Expert Panel on Postoperative Delirium in Older Adults American Geriatrics Society Abstracted Clinical Practice Guideline for Postoperative Delirium in Older Adults. J. Am. Geriatr. Soc. 2015, 63, 142–150. [CrossRef]
- Panitchote, A.; Tangvoraphonkchai, K.; Suebsoh, N.; Eamma, W.; Chanthonglarng, B.; Tiamkao, S.; Limpawattana, P. Under-Recognition of Delirium in Older Adults by Nurses in the Intensive Care Unit Setting. Aging Clin. Exp. Res. 2015, 27, 735–740. [Google Scholar] [CrossRef]
- Stransky, M.; Schmidt, C.; Ganslmeier, P.; Grossmann, E.; Haneya, A.; Moritz, S.; Raffer, M.; Schmid, C.; Graf, B.M.; Trabold, B. Hypoactive Delirium After Cardiac Surgery as an Independent Risk Factor for Prolonged Mechanical Ventilation. J. Cardiothorac. Vasc. Anesth. 2011, 25, 968–974. [Google Scholar] [CrossRef]
- Meagher, D.J.; Leonard, M.; Donnelly, S.; Conroy, M.; Adamis, D.; Trzepacz, P.T. A Longitudinal Study of Motor Subtypes in Delirium: Frequency and Stability during Episodes. J. Psychosom. Res. 2012, 72, 236–241. [Google Scholar] [CrossRef]
- Yang, F.M.; Marcantonio, E.R.; Inouye, S.K.; Kiely, D.K.; Rudolph, J.L.; Fearing, M.A.; Jones, R.N. Phenomenological Subtypes of Delirium in Older Persons: Patterns, Prevalence, and Prognosis. Psychosomatics 2009, 50, 248–254. [Google Scholar] [CrossRef]
- Menzenbach, J.; Guttenthaler, V.; Kirfel, A.; Ricchiuto, A.; Neumann, C.; Adler, L.; Kieback, M.; Velten, L.; Fimmers, R.; Mayr, A.; et al. Estimating Patients’ Risk for Postoperative Delirium from Preoperative Routine Data—Trial Design of the PRe-Operative Prediction of Postoperative DElirium by Appropriate SCreening (PROPDESC) Study—A Monocentre Prospective Observational Trial. Contemp. Clin. Trials Commun. 2020, 17, 100501. [Google Scholar] [CrossRef]
- Menzenbach, J.; Kirfel, A.; Guttenthaler, V.; Feggeler, J.; Hilbert, T.; Ricchiuto, A.; Staerk, C.; Mayr, A.; Coburn, M.; Wittmann, M. PRe-Operative Prediction of Postoperative DElirium by Appropriate SCreening (PROPDESC) Development and Validation of a Pragmatic POD Risk Screening Score Based on Routine Preoperative Data. J. Clin. Anesth. 2022, 78, 110684. [Google Scholar] [CrossRef]
- Günther, U.; Wrigge, H.; Popp, J.; Andorfer, U.; Muders, T.; Putensen, C. Confusion Assessment Method for Intensive Care Unit zur routinemäßigen Kontrolle des Delirs auf Intensivstation. Anästh Intensiv. 2009, 50, 592–600. [Google Scholar]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R.K. The Richmond Agitation–Sedation Scale: Validity and Reliability in Adult Intensive Care Unit Patients. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Schuurmans, M.J.; Shortridge-Baggett, L.M.; Duursma, S.A. The Delirium Observation Screening Scale: A Screening Instrument for Delirium. Res. Theory Nurs. Pract. 2003, 17, 31–50. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K. Clarifying Confusion: The Confusion Assessment Method: A New Method for Detection of Delirium. Ann. Intern. Med. 1990, 113, 941. [Google Scholar] [CrossRef] [PubMed]
- Bellelli, G.; Morandi, A.; Davis, D.H.J.; Mazzola, P.; Turco, R.; Gentile, S.; Ryan, T.; Cash, H.; Guerini, F.; Torpilliesi, T.; et al. Validation of the 4AT, a New Instrument for Rapid Delirium Screening: A Study in 234 Hospitalised Older People. Age Ageing 2014, 43, 496–502. [Google Scholar] [CrossRef]
- Ely, E.W.; Margolin, R.; Francis, J.; May, L.; Truman, B.; Dittus, R.; Speroff, T.; Gautam, S.; Bernard, G.R.; Inouye, S.K. Evaluation of Delirium in Critically Ill Patients: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU): Crit. Care Med. 2001, 29, 1370–1379. [Google Scholar] [CrossRef]
- Simeone, S.; Pucciarelli, G.; Perrone, M.; Teresa, R.; Gargiulo, G.; Guillari, A.; Castellano, G.; Tommaso, L.D.; Niola, M.; Iannelli, G. Delirium in ICU Patients Following Cardiac Surgery: An Observational Study. J. Clin. Nurs. 2018, 27, 1994–2002. [Google Scholar] [CrossRef]
- Habeeb-Allah, A.; Alshraideh, J.A. Delirium Post-cardiac Surgery: Incidence and Associated Factors. Nurs. Crit. Care 2019, 26, 150–155. [Google Scholar] [CrossRef]
- Brown, C.H.; Laflam, A.; Max, L.; Lymar, D.; Neufeld, K.J.; Tian, J.; Shah, A.S.; Whitman, G.J.; Hogue, C.W. The Impact of Delirium After Cardiac Surgical Procedures on Postoperative Resource Use. Ann. Thorac. Surg. 2016, 101, 1663–1669. [Google Scholar] [CrossRef]
- Ansaloni, L.; Catena, F.; Chattat, R.; Fortuna, D.; Franceschi, C.; Mascitti, P.; Melotti, R.M. Risk Factors and Incidence of Postoperative Delirium in Elderly Patients after Elective and Emergency Surgery. Br. J. Surg. 2010, 97, 273–280. [Google Scholar] [CrossRef]
- Weinrebe, W.; Johannsdottir, E.; Karaman, M.; Füsgen, I. What Does Delirium Cost?: An Economic Evaluation of Hyperactive Delirium. Z. Gerontol. Geriat. 2016, 49, 52–58. [Google Scholar] [CrossRef]
- Wong, C.L.; Holroyd-Leduc, J.; Simel, D.L.; Straus, S.E. Does This Patient Have Delirium?: Value of Bedside Instruments. JAMA 2010, 304, 779. [Google Scholar] [CrossRef]
- Shenkin, S.D.; Fox, C.; Godfrey, M.; Siddiqi, N.; Goodacre, S.; Young, J.; Anand, A.; Gray, A.; Hanley, J.; MacRaild, A.; et al. Delirium Detection in Older Acute Medical Inpatients: A Multicentre Prospective Comparative Diagnostic Test Accuracy Study of the 4AT and the Confusion Assessment Method. BMC Med. 2019, 17, 138. [Google Scholar] [CrossRef]
- Wei, L.A.; Fearing, M.A.; Sternberg, E.J.; Inouye, S.K. The Confusion Assessment Method: A Systematic Review of Current Usage: CAM: A Systematic Review of Current Usage. J. Am. Geriatr. Soc. 2008, 56, 823–830. [Google Scholar] [CrossRef]
- Marcantonio, E.R.; Ngo, L.H.; O’Connor, M.; Jones, R.N.; Crane, P.K.; Metzger, E.D.; Inouye, S.K. 3D-CAM: Derivation and Validation of a 3-Minute Diagnostic Interview for CAM-Defined Delirium: A Cross-Sectional Diagnostic Test Study. Ann. Intern. Med. 2014, 161, 554. [Google Scholar] [CrossRef]

| Characteristics | Total (n = 976) | Non-POD Group (n = 747) | POD-Group (n = 229) | p Value | Missing Values |
|---|---|---|---|---|---|
| Age (mean, sd) | 72.3 ± 7.3 | 72.0 ± 7.3 | 73.3 ± 7.2 | 0.010 | 0 |
| Sex | <0.001 | 0 | |||
| female | 375 (38.4) | 311 (41.6) | 64 (27.9) | ||
| male | 601 (61.6) | 436 (58.4) | 165 (72.1) | ||
| ASA | <0.001 | 0 | |||
| ASA 1 | 25 (2.6) | 21 (2.8) | 4 (1.7) | ||
| ASA 2 | 339 (34.7) | 308 (41.2) | 31 (13.5) | ||
| ASA 3 | 544 (55.7) | 380 (50.9) | 164 (71.6) | ||
| ASA 4 | 68 (7.0) | 38 (5.1) | 30 (13.1) | ||
| Surgical discipline | <0.001 | 0 | |||
| Others | 193 (19.8) | 174 (23.3) | 19 (8.3) | ||
| Cardiac Surgery | 274 (28.1) | 136 (18.2) | 138 (60.3) | ||
| Orthopaedic Surgery | 337 (34.5) | 294 (39.4) | 43 (18.8) | ||
| Thoracic Surgery | 21 (2.2) | 17 (2.3) | 4 (1.7) | ||
| Abdominal Surgery | 123 (12.6) | 107 (14.3) | 16 (7.0) | ||
| Vascular Surgery | 28 (2.9) | 19 (2.5) | 9 (3.9) |
| Visit Day | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| POD | 113 (49%) | 49 (21%) | 28 (12%) | 23 (10%) | 16 (7%) |
| Visit Day | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| ICU | 80 (71%) | 58 (51%) | 29 (34%) | 24 (36%) | 27 (42%) |
| IMC | 19 (17%) | 7 (6%) | 8 (9%) | 2 (3%) | 4 (6%) |
| Norm | 14 (12%) | 49 (43%) | 48 (56%) | 40 (61%) | 34 (52%) |
| Visit Day | CAM-ICU | DOS | CAM | 4AT |
|---|---|---|---|---|
| 1 | 69 | 85 | 5 | 7 |
| 2 | 30 | 96 | 33 | 24 |
| 3 | 16 | 70 | 26 | 19 |
| 4 | 13 | 48 | 20 | 20 |
| 5 | 13 | 53 | 18 | 17 |
| Visit Day | POD | CAM-ICU Pos | DOS Pos | CAM-ICU + DOS Pos |
|---|---|---|---|---|
| 1 | 99 | 69 (70%) | 60 (61%) | 46 (46%) |
| 2 | 65 | 30 (46%) | 61 (94%) | 26 (40%) |
| 3 | 37 | 16 (43%) | 37 (100%) | 16 (43%) |
| 4 | 26 | 13 (50%) | 23 (88%) | 10 (38%) |
| 5 | 31 | 13 (42%) | 30 (97%) | 12 (39%) |
| Visit Day | POD | CAM Pos | DOS Pos | 4AT Pos | CAM + DOS + 4AT Pos |
|---|---|---|---|---|---|
| 1 | 14 | 5 (5%) | 9 (64%) | 7 (50%) | 2 (14%) |
| 2 | 49 | 33 (67%) | 35 (71%) | 24 (49%) | 12 (24%) |
| 3 | 48 | 26 (54%) | 33 (69%) | 20 (42%) | 6 (13%) |
| 4 | 40 | 20 (50%) | 20 (50%) | 25 (63%) | 7 (18%) |
| 5 | 34 | 18 (53%) | 17 (50%) | 23 (68%) | 5 (15%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kirfel, A.; Jossen, D.; Menzenbach, J.; Mayr, A.; Wittmann, M. Occurrence of Postoperative Delirium and the Use of Different Assessment Tools. Geriatrics 2023, 8, 11. https://doi.org/10.3390/geriatrics8010011
Kirfel A, Jossen D, Menzenbach J, Mayr A, Wittmann M. Occurrence of Postoperative Delirium and the Use of Different Assessment Tools. Geriatrics. 2023; 8(1):11. https://doi.org/10.3390/geriatrics8010011
Chicago/Turabian StyleKirfel, Andrea, Diane Jossen, Jan Menzenbach, Andreas Mayr, and Maria Wittmann. 2023. "Occurrence of Postoperative Delirium and the Use of Different Assessment Tools" Geriatrics 8, no. 1: 11. https://doi.org/10.3390/geriatrics8010011
APA StyleKirfel, A., Jossen, D., Menzenbach, J., Mayr, A., & Wittmann, M. (2023). Occurrence of Postoperative Delirium and the Use of Different Assessment Tools. Geriatrics, 8(1), 11. https://doi.org/10.3390/geriatrics8010011






