Factors Associated with Volunteer Activities and Sleep Efficiency in Older Adults with Hypertension: A Sequential Model Study
Abstract
1. Introduction
2. Materials and Methods
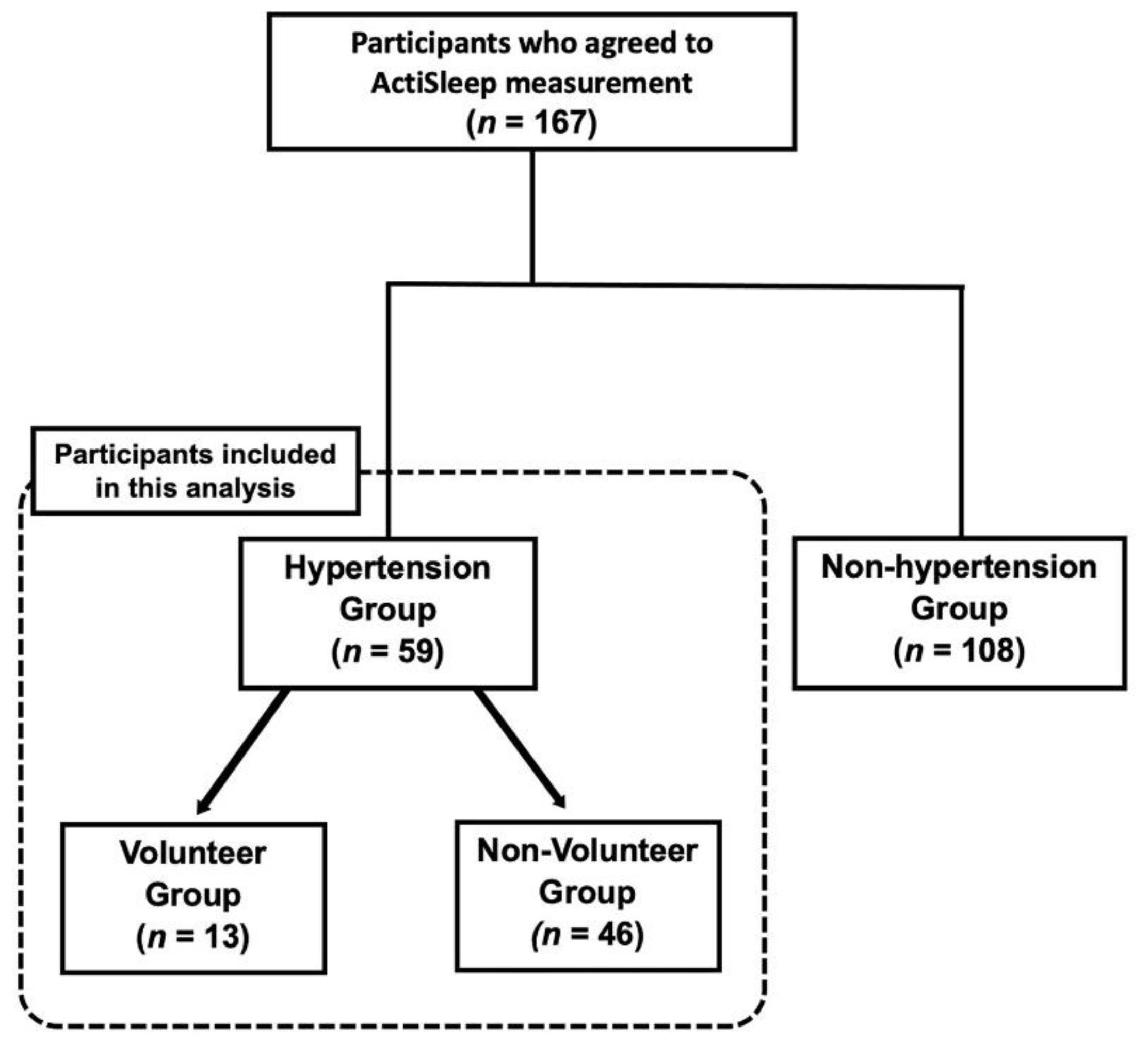
2.1. Participants
2.2. Survey
2.3. ActiSleep Measurement
2.4. Data Analysis
2.5. Ethical Statement
3. Results
3.1. Participant Demographics
3.2. Daily Activities
3.3. Sleep Status
3.4. Health Status
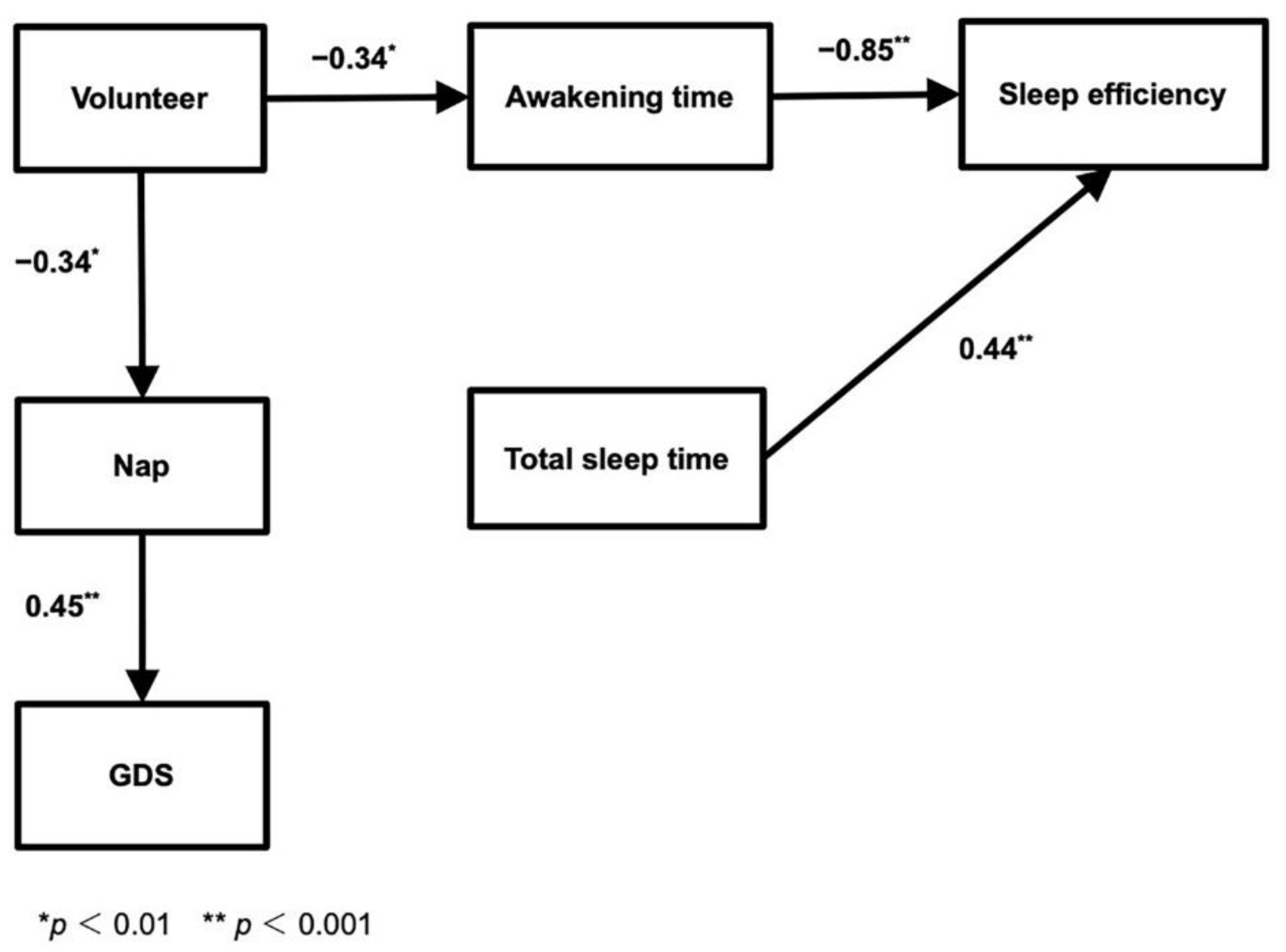
3.5. Model to Describe the Relationship between Factors Related to Volunteer Participation, Hypertension, and Sleep in Older Adults
4. Discussion
4.1. Sleep
4.2. Depression
4.3. Volunteer Participation in Older Adults
4.4. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Health Labour and Welfare. The National Health and Nutrition Survey in Japan. 2019. Available online: https://www.mhlw.go.jp/content/000710991.pdf (accessed on 6 August 2021).
- Yokoyama, T. National health promotion measures in Japan: Health Japan 21 (the second term). J. Natl. Inst. Public Health 2020, 69, 14–24. Available online: https://www.niph.go.jp/journal/data/69-1/202069010003.pdf (accessed on 6 August 2021).
- Calhoun, D. Sleep disorders and hypertension risk. J. Hum. Hypertens. 2017, 31, 371–372. [Google Scholar] [CrossRef][Green Version]
- Lin, C.L.; Liu, T.C.; Lin, F.H.; Chung, C.H.; Chien, W.C. Association between sleep disorders and hypertension in Taiwan: A nationwide population-based retrospective cohort study. J. Hum. Hypertens. 2017, 31, 220–224. [Google Scholar] [CrossRef]
- Kim, K.; Uchiyama, M.; Okawa, M.; Liu, X.; Ogihara, R. An epidemiological study of insomnia among the Japanese general population. Sleep 2000, 23, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Bansil, P.; Kuklina, E.V.; Merritt, R.K.; Yoon, P.W. Associations between sleep disorders, sleep duration, quality of sleep, and hypertension. Results from the national health and nutrition examination survey, 2005 to 2008. J. Clin. Hypertens. 2011, 13, 739–743. [Google Scholar] [CrossRef]
- Asakura, K. The Study of Sleep; Asakura Publishing Co., Ltd.: Tokyo, Japan, 2009; pp. 182–189, 584–591. [Google Scholar]
- Garbarino, S.; Magnavita, N. Sleep problems are a strong predictor of stress-related metabolic changes in police officers. A prospective study. PLoS ONE 2019, 14, e0224259. [Google Scholar] [CrossRef]
- Magnavita, N.; Tripepi, G.; Di Prinzio, R.R. Symptoms in health care workers during the COVID-19 epidemic. A cross-sectional survey. Int. J. Environ. Res. Public Health 2020, 17, 5218. [Google Scholar] [CrossRef]
- Yeung, J.W.K.; Zhang, Z.; Kim, T.Y. Volunteering and health benefits in general adults: Cumulative effects and forms. BMC Public Health 2018, 18, 1–8. [Google Scholar] [CrossRef]
- Hirsch, K.; Linn, M.W. How being helpful helps the elderly helper. Gerontologist 1977, 17, 75. [Google Scholar]
- Burr, J.A.; Tavares, J.L.; Mutchler, J.E. Volunteering and hypertension risk in later life. J. Aging Health 2011, 23, 24–51. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Thisted, R.A. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychol. Aging 2006, 21, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Almeida, O.P.; Almeida, S.A. Short versions of the geriatric depression scale: A study of their validity for the diagnosis of a major depressive episode according to ICD-10 and DSM-IV. Int. J. Geriatr. Psychiatry 1999, 14, 858–865. [Google Scholar] [CrossRef]
- Fukuhara, S.; Suzukamo, Y. Health-related QOL scale-SF-8 and SF-36: Current quality of life (QOL) measurement. Igakunoayumi 2005, 213, 133–136. [Google Scholar]
- Cellini, N.; Buman, M.P.; McDevitt, E.A.; Ricker, A.A.; Mednick, S.C. Direct comparison of two actigraphy devices with polysomnographically recorded naps in healthy young adults. Chronobiol. Int. 2013, 30, 691–698. [Google Scholar] [CrossRef]
- Toyoda, H. Submodels and applications in covariance structure analysis. Jpn. J. Educ. Psychol. 1991, 39, 467–478. [Google Scholar] [CrossRef]
- Oshio, A. First Covariance Structure Analysis: AMOS Path Analysis, 2nd ed.; Tokyo Tosho Co., Ltd.: Tokyo, Japan, 2009. [Google Scholar]
- Asano, H.; Suzuki, N.; Kojima, T. An Introduction to the Practice of Covariance Structure Analysis; Kōdansha: Tokyo, Japan, 2005; pp. 158–161. (In Japanese) [Google Scholar]
- Liu, R.Q.; Qian, Z.; Trevathan, E.; Chang, J.J.; Zelicoff, A.; Hao, Y.T.; Lin, S.; Dong, G.H. Poor sleep quality associated with high risk of hypertension and elevated blood pressure in China: Results from a large population-based study. Hypertens. Res. 2016, 39, 54–59. [Google Scholar] [CrossRef]
- Hirasawa, H.; Atsumi, Y.; Kojima, T. Polysomnographyic study of healthy aged persons. Rinshōnōha 1988, 30, 641–645. [Google Scholar]
- Uchida, N. Insomnia and depression in old age. Geriatr. Med. 2015, 53, 1073–1077. [Google Scholar]
- Mitsuishi, Y.; Tsunoda, K.; Kai, Y.; Kitano, N.; Tsuji, T.; Yoon, J.E.; Yoon, J.Y.; Kim, T.H.; Okura, T. Effect of volunteerism as exercise instructor on physical and cognitive function in community-dwelling elderly women. Jpn. J. Phys. Fit. Sport Med. 2013, 62, 79–86. [Google Scholar] [CrossRef]
- Ito, E. Sleep and hypertension. Ketsuatsu 2011, 18, 1087–1092. [Google Scholar]
- Kario, K.; Schwartz, J.E.; Pickering, T.G. Ambulatory physical activity as a determinant of diurnal blood pressure variation. Hypertension 1999, 34, 685–691. [Google Scholar] [CrossRef][Green Version]
- Pasqualini, R.; Foroni, M.; Salvioli, G.; Mussi, C. The “nondipper” elderly: A clinical entity or a bias? J. Am. Geriatr. Soc. 2004, 52, 967–971. [Google Scholar] [CrossRef] [PubMed]
- Ryoko, A.; Matsuda, H. The relationship between hypertension and nocturnal waking in community-dwelling elderly individuals. Nihon Ronen Igakkai Zasshi. 2017, 54, 56–62. [Google Scholar]
- Ohayon, M.M. Special issue: Sleep and the elderly. J. Psychosom. Res. 2004, 56, 463–464. [Google Scholar] [CrossRef] [PubMed]
- Maglione, J.E.; Ancoli-Israel, S.; Peters, K.W.; Paudel, M.L.; Yaffe, K.; Ensrud, K.E.; Stone, K.L. Depressive symptoms and subjective and objective sleep in community-dwelling older women. J. Am. Geriatr. Soc. 2012, 60, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Foley, D.J.; Vitiello, M.V.; Bliwise, D.L.; Ancoli-Israel, S.; Monjan, A.A.; Walsh, J.K. Frequent napping is associated with excessive daytime sleepiness, depression, pain, and nocturia in older adults: Findings from the National Sleep Foundation ‘2003 Sleep in America’ Poll. Am. J. Geriatr. Psychiatry 2007, 15, 344–350. [Google Scholar] [CrossRef]
- Eto, S.; Matsuda, H.; Takada, D. Relationship between daytime sleep and night-time sleep in a community-dwelling elderly person. J. Gerontol. Nurs. Caring Res. 2010, 1, 2–8. [Google Scholar]
- Aging Society NGO Cooperation Council Questionnaire results [monograph on the Internet] Kōrei shakai NGO renkei kyōgi-kai. 2004. Available online: https://40591.diarynote.jp/200410020818060000/ (accessed on 30 May 2020).
- Fujiwara, Y.; Sugihara, Y.; Shinkai, S. Effects of volunteering on the mental and physical health of senior citizens: Significance of senior-volunteering from the view point of community health and welfare. Nihon Koshu Eisei Zasshi 2005, 52, 293–307. [Google Scholar]
- Wheeler, J.A.; Gorey, K.M.; Greenblatt, B. The beneficial effects of volunteering for older volunteers and the people they serve: A meta-analysis. Int. J. Aging Hum. Dev. 1998, 47, 69–79. [Google Scholar] [CrossRef]
- Luoh, M.C.; Herzog, A.R. Individual consequences of volunteer and paid work in old age: Health and mortality. J. Health Soc. Behav. 2002, 43, 490–509. [Google Scholar] [CrossRef] [PubMed]
- Anme, T.; Shinohara, R.; Sugisawa, Y.; Itoh, S. Social interaction and mortality: A seven-year longitudinal study of elderly people. Nihon Koshu Eisei Zasshi 2006, 53, 681–687. [Google Scholar] [PubMed]
- Sainer, J.; Zander, M. Guidelines for older person volunteers. Gerontologist 1971, 11, 201–204. [Google Scholar] [CrossRef] [PubMed]
| N = 59 | ||||
|---|---|---|---|---|
| Entire Cohort | Volunteers | Non-Volunteers | p | |
| N = 59 | N = 13 (22.0) | N = 46 (78.0) | ||
| Sex | 0.762 † | |||
| Male | 25 (42.4) | 6 (46.2) | 19 (41.3) | |
| Female | 34 (57.6) | 7 (53.8) | 27 (58.7) | |
| Age | 77.27 ± 5.54 | 75.85 ± 4.26 | 77.67 ± 5.83 | 0.322 ‡ |
| Spouse | 0.480 † | |||
| Yes | 43 (74.1) | 11 (84.6) | 32 (71.1) | |
| No | 15 (25.9) | 2 (15.4) | 13 (28.9) | |
| Living arrangements | 0.668 † | |||
| Living alone | 9 (15.8) | 1 (7.7) | 8 (18.2) | |
| Not living alone | 48 (84.2) | 12 (92.3) | 36 (75.0) | |
| Children | 1.000 † | |||
| Yes | 53 (93.0) | 12 (92.3) | 41 (93.2) | |
| No | 4 (7.0) | 1 (7.7) | 3 (6.8) | |
| Housework | 0.128 † | |||
| Yes | 34 (57.6) | 5 (38.5) | 29 (63.0) | |
| No | 25 (42.4) | 8 (61.5) | 17 (37.0) | |
| Hobbies/lessons | 0.348 † | |||
| Yes | 28 (47.5) | 8 (61.5) | 20 (43.5) | |
| No | 31 (52.2) | 5 (38.5) | 26 (56.5) | |
| Exercise class | 0.154 † | |||
| Yes | 16 (27.1) | 6 (46.2) | 10 (21.7) | |
| No | 43 (72.9) | 7 (53.8) | 36 (78.3) | |
| Frequency of going out | 5.68 ± 1.69 | 6.23 ± 1.30 | 5.52 ± 1.76 | 0.203 ‡ |
| Smoking habits | 1.000 † | |||
| Yes | 2 (3.4) | 0 | 2(4.3) | |
| No | 57 (96.6) | 13 (100) | 44 (95.7) | |
| Drinking habit | 0.119 † | |||
| Yes | 6 (10.3) | 3 (23.1) | 3 (6.7) | |
| No | 52 (89.7) | 10 (76.9) | 42 (93.3) |
| N = 59 | ||||
|---|---|---|---|---|
| Entire Cohort | Volunteers | Non-Volunteers | p | |
| N = 59 | N = 13 (22.0) | N = 46 (78.0) | ||
| Total sleep time (min) | 364.95 ± 99.07 | 389.54 ± 130.81 | 358.00 ± 88.68 | 0.156 ‡ |
| Sleep latency (min) | 6.47 ± 5.37 | 7.85 ± 9.47 | 6.09 ± 3.56 | 0.578 ‡ |
| Awakening time (min) | 89.2 ± 46.17 | 59.92 ± 46.63 | 97.47 ± 43.01 | 0.003 *‡ |
| Sleep efficiency (%) | 79.39 ± 8.99 | 86.32 ± 6.79 | 77.43 ± 8.60 | 0.001 *‡ |
| Nap frequency | 3.08 ± 2.60 | 1.46 ± 2.18 | 3.54 ± 2.54 | 0.009 *‡ |
| Nocturnal urination | 1.000 † | |||
| Yes | 49 (83.1) | 11 (84.6) | 38 (82.6) | |
| No | 10 (16.9) | 2 (15.4) | 8 (17.4) | |
| Sleeping disorder | 1.000 † | |||
| Yes | 5 (8.5) | 1 (7.7) | 4 (8.7) | |
| No | 54 (91.5) | 12 (92.3) | 42 (91.3) | |
| BMI | 24.38 ± 3.11 | 23.83 ± 2.89 | 24.53 ± 3.18 | 0.564 ‡ |
| GDS | 2.29 ± 2.69 | 1.62 ± 1.33 | 2.48 ± 2.95 | 0.736 ‡ |
| PCS | 47.49 ± 7.38 | 50.04 ± 3.49 | 46.76 ± 8.03 | 0.351 ‡ |
| MCS | 50.13 ± 5.96 | 51.77 ± 3.53 | 49.66 ± 6.44 | 0.314 ‡ |
| Diabetes | 0.576 † | |||
| Yes | 5 (8.5) | 0 | 5 (10.9) | |
| No | 54 (91.5) | 13(100) | 41 (88.4) |
| Factors | ||||||
|---|---|---|---|---|---|---|
| Estimated Value | Standard Error | Statistical Test | p | |||
| Awakening Time | <− | Volunteering | −37.551 | 13.638 | −2.753 | 0.006 |
| Naps | <− | Volunteering | −2.082 | 0.768 | −2.711 | 0.007 |
| Sleep efficiency | <− | Awakening Time | −0.166 | 0.013 | −23.541 | ** |
| GDS | <− | Naps | 0.465 | 0.122 | 3.819 | ** |
| Sleep efficiency | <− | Total sleep time | 0.04 | 0.003 | 12.231 | ** |
| Path Coefficient (Direct Effect) | ||||||
| Estimated Value | ||||||
| Awakening Time | <− | Volunteering | −0.34 | |||
| Naps | <− | Volunteering | −0.34 | |||
| Sleep efficiency | <− | Awakening Time | −0.85 | |||
| GDS | <− | Naps | 0.45 | |||
| Sleep efficiency | <− | Total sleep time | 0.44 | |||
| Standardized Total Effect | ||||||
| Volunteering | ||||||
| Sleep efficiency | 0.29 | |||||
| GDS | −0.15 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aonuma, R.; Mayers, T.; Mizukami, K.; Aonuma, K.; Matsuda, H. Factors Associated with Volunteer Activities and Sleep Efficiency in Older Adults with Hypertension: A Sequential Model Study. Geriatrics 2021, 6, 89. https://doi.org/10.3390/geriatrics6030089
Aonuma R, Mayers T, Mizukami K, Aonuma K, Matsuda H. Factors Associated with Volunteer Activities and Sleep Efficiency in Older Adults with Hypertension: A Sequential Model Study. Geriatrics. 2021; 6(3):89. https://doi.org/10.3390/geriatrics6030089
Chicago/Turabian StyleAonuma, Ryoko, Thomas Mayers, Katsuyoshi Mizukami, Kazutaka Aonuma, and Hitomi Matsuda. 2021. "Factors Associated with Volunteer Activities and Sleep Efficiency in Older Adults with Hypertension: A Sequential Model Study" Geriatrics 6, no. 3: 89. https://doi.org/10.3390/geriatrics6030089
APA StyleAonuma, R., Mayers, T., Mizukami, K., Aonuma, K., & Matsuda, H. (2021). Factors Associated with Volunteer Activities and Sleep Efficiency in Older Adults with Hypertension: A Sequential Model Study. Geriatrics, 6(3), 89. https://doi.org/10.3390/geriatrics6030089







