Palatability and Swallowability of Pimavanserin When Mixed with Selected Food Vehicles: An Exploratory Open-Label Crossover Study
Abstract
1. Introduction
2. Materials and Methods
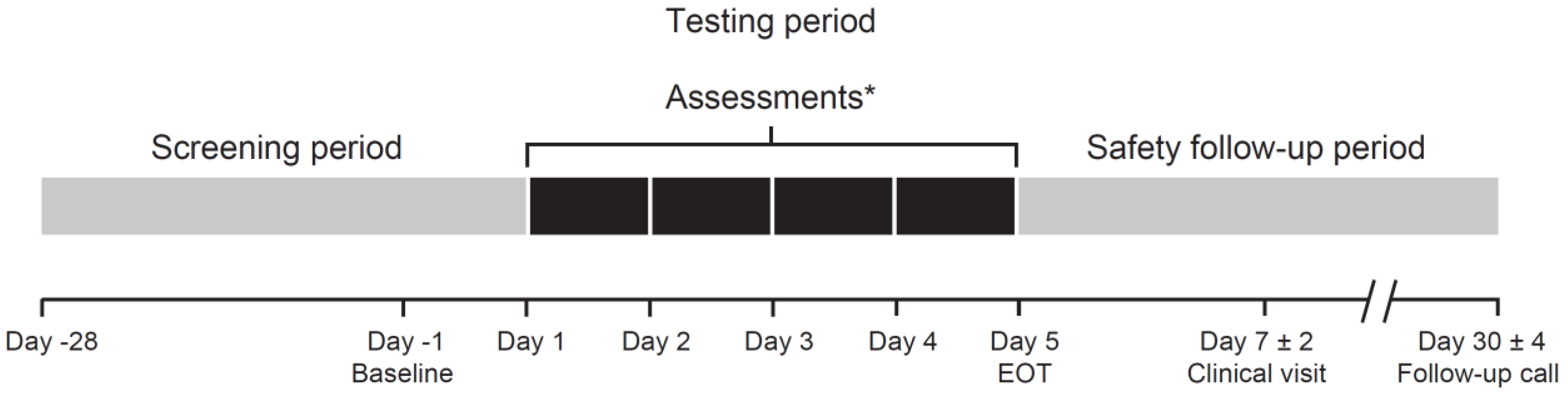
2.1. Study Design
2.2. Participant Selection
2.3. Treatment Administration
2.4. Endpoints and Assessments
2.5. Statistical Analyses
3. Results
3.1. Study Population
3.2. Food Vehicle Volume Assessments
3.3. Primary Study Endpoints
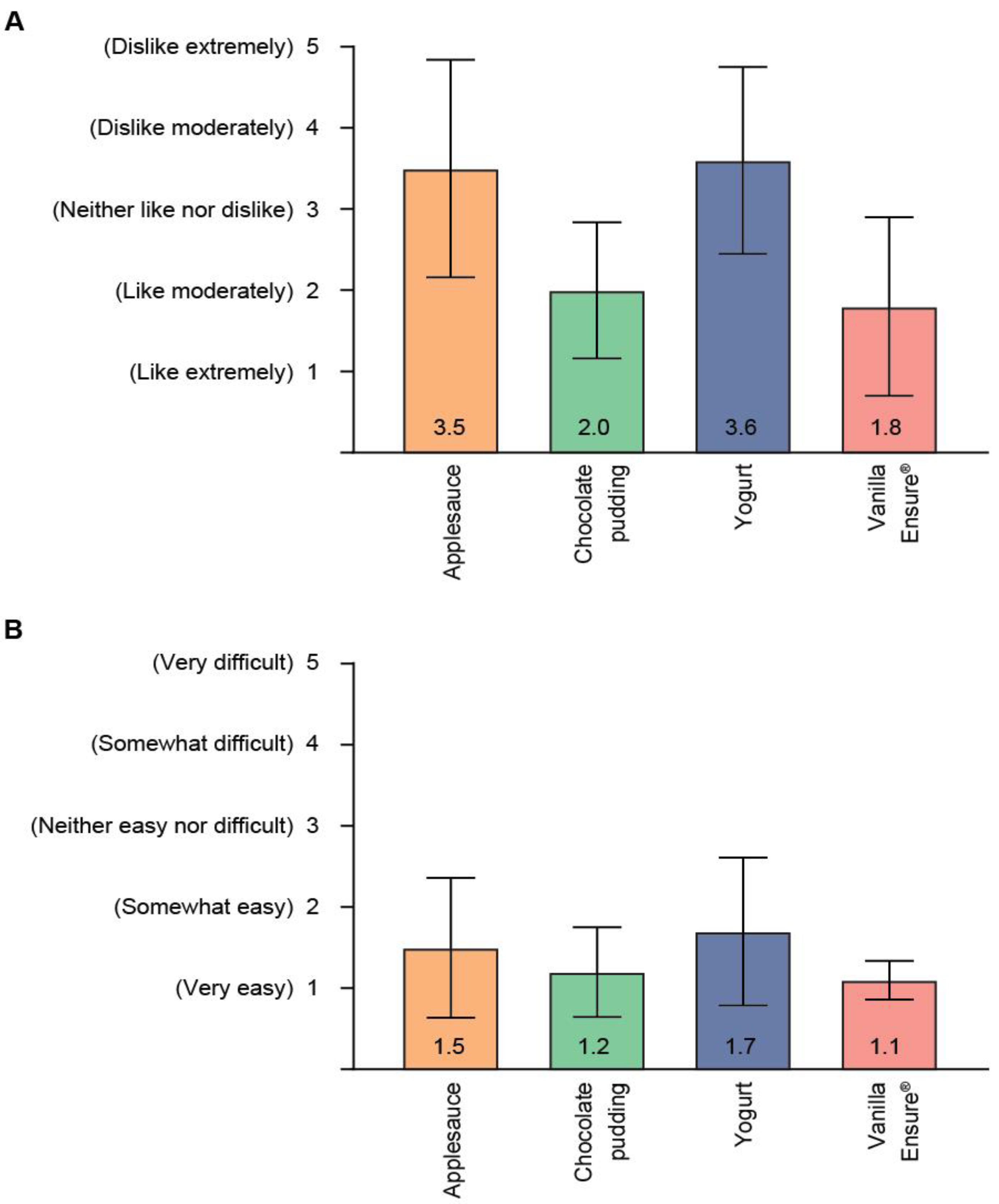
Palatability (Taste) and Swallowability
3.4. Secondary Study Endpoints
3.4.1. Mouthfeel, Smell, Aftertaste, and Bitterness
3.4.2. Capsule Manipulation
3.5. Safety
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cummings, J.; Isaacson, S.; Mills, R.; Williams, H.; Chi-Burris, K.; Corbett, A.; Dhall, R.; Ballard, C. Pimavanserin for patients with Parkinson’s disease psychosis: A randomised, placebo-controlled phase 3 trial. Lancet 2014, 383, 533–540. [Google Scholar] [CrossRef]
- Kitten, A.K.; Hallowell, S.A.; Saklad, S.R.; Evoy, K.E. Pimavanserin: A novel drug approved to treat Parkinson’s disease psychosis. Innov. Clin. Neurosci. 2018, 15, 16–22. [Google Scholar] [PubMed]
- Goodin, D.S.; Bates, D. Review: Treatment of early multiple sclerosis: The value of treatment initiation after a first clinical episode. Mult. Scler. 2009, 15, 1175–1182. [Google Scholar] [CrossRef] [PubMed]
- Nuplazid Dosing Information. Available online: https://www.nuplazidhcp.com/dosing (accessed on 30 October 2020).
- Wirth, R.; Dziewas, R.; Beck, A.M.; Clavé, P.; Hamdy, S.; Heppner, H.J.; Langmore, S.; Leischker, A.H.; Martino, R.; Pluschinski, P.; et al. Oropharyngeal dysphagia in older persons—From pathophysiology to adequate intervention: A review and summary of an international expert meeting. Clin. Interv. Aging 2016, 11, 189–208. [Google Scholar] [CrossRef] [PubMed]
- Maher, R.L.; Hanlon, J.; Hajjar, E.R. Clinical consequences of polypharmacy in elderly. Expert Opin. Drug Saf. 2014, 13, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Sokoloff, L.G.; Pavlakovic, R. Neuroleptic-induced dysphagia. Dysphagia 1997, 12, 177–179. [Google Scholar] [CrossRef] [PubMed]
- Takizawa, C.; Gemmell, E.; Kenworthy, J.; Speyer, R. A systematic review of the prevalence of oropharyngeal dysphagia in stroke, Parkinson’s disease, Alzheimer’s disease, head injury, and pneumonia. Dysphagia 2016, 31, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Mu, L.; Sobotka, S.; Chen, J.; Su, H.; Sanders, I.; Adler, C.H.; Shill, H.A.; Caviness, J.N.; Samanta, J.E.; Beach, T.G.; et al. Altered pharyngeal muscles in Parkinson disease. J. Neuropathol. Exp. Neurol. 2012, 71, 520–530. [Google Scholar] [CrossRef] [PubMed]
- Mu, L.; Sobotka, S.; Chen, J.; Su, H.; Sanders, I.; Nyirenda, T.; Adler, C.H.; Shill, H.A.; Caviness, J.N.; Samanta, J.E.; et al. Parkinson disease affects peripheral sensory nerves in the pharynx. J. Neuropathol. Exp. Neurol. 2013, 72, 614–623. [Google Scholar] [CrossRef] [PubMed]
- Simons, J.A. Swallowing dysfunctions in Parkinson’s disease. Int. Rev. Neurobiol. 2017, 134, 1207–1238. [Google Scholar] [PubMed]
- Ranmal, S.R.; O’Brien, F.; Lopez, F.; Ruiz, F.; Orlu, M.; Tuleu, C.; Walsh, J.; Liu, F. Methodologies for assessing the acceptability of oral formulations among children and older adults: A systematic review. Drug Discov. Today 2018, 23, 830–847. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration Center for Drug Evaluation and Research. Use of Liquids and/or Soft Foods as Vehicles for Drug Administration: General Considerations for Selection and in Vitro Methods for Product Quality Assessments (Draft Guidance for Industry); U.S. Department of Health and Human Services: Rockville, MD, USA, 2018.
- European Medicines Agency (EMA). Reflection Paper on the Pharmaceutical Development of Medicines for Use in the Older Population. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/draft-reflection-paper-pharmaceutical-development-medicines-use-older-population-first-version_en.pdf (accessed on 11 May 2021).
- Vanover, K.E.; Robbins-Weilert, D.; Wilbraham, D.G.; Mant, T.G.; van Kammen, D.P.; Davis, R.E.; Weiner, D.M. Pharmacokinetics, tolerability, and safety of ACP-103 following single or multiple oral dose administration in healthy volunteers. J. Clin. Pharmacol. 2007, 47, 704–714. [Google Scholar] [CrossRef] [PubMed]
- Forough, A.S.; Lau, E.T.; Steadman, K.J.; Cichero, J.A.; Kyle, G.J.; Serrano Santos, J.M.; Nissen, L.M. A spoonful of sugar helps the medicine go down? A review of strategies for making pills easier to swallow. Patient Prefer. Adherence 2018, 12, 1337–1346. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Ghaffur, A.; Bains, J.; Hamdy, S. Acceptability of oral solid medicines in older adults with and without dysphagia: A nested pilot validation questionnaire based observational study. Int. J. Pharm. 2016, 512, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Calabresi, P.A.; Kieseier, B.C.; Arnold, D.L.; Balcer, L.J.; Boyko, A.; Pelletier, J.; Liu, S.; Zhu, Y.; Seddighzadeh, A.; Hung, S.; et al. Pegylated interferon beta-1a for relapsing-remitting multiple sclerosis (ADVANCE): A randomised, phase 3, double-blind study. Lancet Neurol. 2014, 13, 657–665. [Google Scholar] [CrossRef]
- Logrippo, S.; Ricci, G.; Sestili, M.; Cespi, M.; Ferrara, L.; Palmieri, G.F.; Ganzetti, R.; Bonacucina, G.; Blasi, P. Oral drug therapy in elderly with dysphagia: Between a rock and a hard place! Clin. Interv. Aging 2017, 12, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Suttrup, I.; Warnecke, T. Dysphagia in Parkinson’s disease. Dysphagia 2016, 31, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Liew, K.B.; Tan, Y.T.; Peh, K.K. Characterization of oral disintegrating film containing donepezil for Alzheimer disease. AAPS PharmSciTech 2012, 13, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Lopez, F.L.; Ernest, T.B.; Orlu, M.; Tuleu, C. The effect of administration media on palatability and ease of swallowing of multiparticulate formulations. Int. J. Pharm. 2018, 551, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Lopez, F.L.; Mistry, P.; Batchelor, H.K.; Bennett, J.; Coupe, A.; Ernest, T.B.; Orlu, M.; Tuleu, C. Acceptability of placebo multiparticulate formulations in children and adults. Sci. Rep. 2018, 8, 1–10. [Google Scholar] [CrossRef]



| Characteristic | Overall (n = 18) |
|---|---|
| Sex, n (%) | |
| Female | 9 (50.0) |
| Male | 9 (50.0) |
| Age, mean (SD) | 65.2 (4.9) |
| Race, n (%) | |
| American Indian or Alaskan Native | 1 (5.6) |
| Asian | 1 (5.6) |
| Black or African American | 1 (5.6) |
| White | 15 (83.3) |
| Ethnicity | |
| Hispanic or Latino | 8 (44.4) |
| Not Hispanic or Latino | 10 (55.6) |
| BMI, mean (SD), kg/m2 | 26.1 (3.7) |
| TEAE, n (%) a | Overall (n = 18) |
|---|---|
| Any TEAE | 5 (27.8) |
| Gastrointestinal disorders | 4 (22.2) |
| Constipation | 1 (5.6) |
| Diarrhea | 1 (5.6) b |
| Lip dry | 1 (5.6) |
| Vomiting | 1 (5.6) b |
| Musculoskeletal and connective tissue disorders | 1 (5.6) |
| Back pain | 1 (5.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Forman, M.; Kouassi, A.; Brandt, T.; Barsky, L.; Zamora, C.; Dekarske, D. Palatability and Swallowability of Pimavanserin When Mixed with Selected Food Vehicles: An Exploratory Open-Label Crossover Study. Geriatrics 2021, 6, 61. https://doi.org/10.3390/geriatrics6020061
Forman M, Kouassi A, Brandt T, Barsky L, Zamora C, Dekarske D. Palatability and Swallowability of Pimavanserin When Mixed with Selected Food Vehicles: An Exploratory Open-Label Crossover Study. Geriatrics. 2021; 6(2):61. https://doi.org/10.3390/geriatrics6020061
Chicago/Turabian StyleForman, Mark, Alex Kouassi, Teresa Brandt, Lee Barsky, Cynthia Zamora, and Daryl Dekarske. 2021. "Palatability and Swallowability of Pimavanserin When Mixed with Selected Food Vehicles: An Exploratory Open-Label Crossover Study" Geriatrics 6, no. 2: 61. https://doi.org/10.3390/geriatrics6020061
APA StyleForman, M., Kouassi, A., Brandt, T., Barsky, L., Zamora, C., & Dekarske, D. (2021). Palatability and Swallowability of Pimavanserin When Mixed with Selected Food Vehicles: An Exploratory Open-Label Crossover Study. Geriatrics, 6(2), 61. https://doi.org/10.3390/geriatrics6020061






