LGBTQ+ Aging Research in Canada: A 30-Year Scoping Review of the Literature
Abstract
1. Introduction
2. Methods
3. Results
3.1. Major Themes in the Literature
- Risk: reducing it, predicting it, patterns of risk, and sociodemographic factors;
- Improving HIV testing and the experiences of living with HIV;
- Homophobia, transphobia, stigma, and discrimination as barriers to care;
- Navigating care and identity;
- Documenting history and changing policy landscapes.
3.2. Theme 1: Risk: Reducing It, Predicting It, Patterns of Risk, and Sociodemographic Factors
3.3. Theme 2: Improving HIV Testing and the Experiences of Living with HIV
3.4. Theme 3: Homophobia, Transphobia, Stigma, and Discrimination as Barriers to Care
3.5. Theme 4: Navigating Care and Identity
3.6. Theme 5: Documenting History and Changing Policy Landscapes
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Citation | Study Information |
|---|---|
| Alderson, K. (2004). A phenomenological investigation of same-sex marriage. The Canadian Journal of Human Sexuality,13(2), 107–122. | Age: Range = 30–66; mean = 46.3 65+: 1 Gender: M and F LGBTQ+ Inclusion: Gay and lesbian same-sex couples Sample Size: 43 Location: International Approach: Qualitative |
| Bauer, G. R., Travers, R., Scanlon, K., & Coleman, T. A. (2012). High heterogeneity of HIV-related sexual risk among transgender people in Ontario, Canada: A province-wide respondent-driven sampling survey. BMC Public Health, 12(1), 292. | Age: Range = 16–65+ 65+: 3% Gender: M and F LGBTQ+ Inclusion: FTM, MTF Sample Size: 433 Location: Ontario Approach: Quantitative |
| Bergeron, S., & Senn, C. (2003). Health care utilization in a sample of Canadian lesbian women: Predictors of risk and resilience. Women & Health, 37(3), 19–35, doi:10.1300/J013v37n03_02 | Age: Range = 18–67; mean = 38.85 Gender: F LGTBQ+ Inclusion: Lesbian women Sample Size: 254 Location: Canada Approach: Quantitative |
| Bossio, J. A., Pukall, C. F., & Bartley, K. (2015). You either have it or you don’t: The impact of male circumcision status on sexual partners. The Canadian Journal of Human Sexuality, 24(2), 104–119. | Age: M: Range = 20–71; mean = 31.50, F: Range = 19–57, mean = 26.87 Gender: M and F LGBTQ+ Inclusion: Gay men Sample Size: 196 Location: International Approach: Quantitative |
| Brennan, D., Craig, S., & Thompson, D. (2012). Factors associated with a drive for muscularity among gay and bisexual men. Culture, Health & Sexuality, 14(1), 1–15, doi:10.1080/13691058.2011.619578. | Age: Range =16–76; mean = 34.1 Gender: M LGBTQ+ Inclusion: Gay and bisexual men and other men who have sex with men Sample Size: 400 Location: Toronto, Ontario Approach: Quantitative |
| Brennan, D. J., Emlet, C. A., Brennenstuhl, S., & Rueda, S. (2013). Socio-demographic profile of older adults with HIV/AIDS: Gender and sexual orientation differences. Canadian Journal on Aging/La Revue Canadienne du Vieillissement, 32(1), 31–43. | Age: Range = 50–86; mean = 57, SD = 6.2 65+: 136 Gender: M and F LGBTQ+ Inclusion: Gay and Bisexual Men Sample Size: 1103 Location: Ontario Approach: Quantitative |
| Brotman, S., Ryan, B., Collins, S., Chamberland, L., Cormier, R., Julien, D., Meyer, E., Peterkin, A., & Richard, B. (2007). Coming out to care: Caregivers of gay and lesbian seniors in Canada. The Gerontologist, 47(4), 490–503, doi:10.1093/geront/47.4.490 | Age: Range = 36–72; mean = N/A 65+: 2 Gender: M and F LGBTQ+ Inclusion: Gay men and lesbian women Sample Size: 17 Location: Montreal, Qubece; Halifax, Nova Scotia; and Vancouver, British Colubmia Approach: Qualitative |
| Brownrigg, B., Taylor, D., Phan, F., Sandstra, I., Stimpson, R., Barrios, R., ... & Ogilvie, G. (2017). Improving linkage to HIV care at low-threshold STI/HIV testing sites: An evaluation of the Immediate Staging Pilot Project in Vancouver, British Columbia. Canadian Journal of Public Health, 108(1), e79–e84. | Age: Range = 19–71; mean = 32.3 Gender: M LGBTQ+ Inclusion: Men who have either male or female sexual partners Sample Size: 108 Location: Vancouver, British Columbia Approach: Quantitative |
| Chamberland, L. (2003). Elderly women, invisible lesbians. Canadian Journal of Community Mental Health= Revue Canadienne de Sante Mentale Communautaire, 22(2), 85–103. | Age: Range = 60–76 Gender: F LGBTQ+ Inclusion: Lesbian women Sample Size: 20 Location: Montreal, Quebec Approach: Qualitative |
| Chandarana, P. C., Conlon, P., Noh, S., & Field, V. A. (1990). The AIDS dilemma: Worry and concern over AIDS. Canadian Journal of Public Health= Revue Canadienne de Sante Publique, 81(3), 222–225. | Age: Range = 19–66; mean = 34 Gender: M LGBTQ+ Inclusion: Homosexual and bisexual men Sample Size: 148 Location: Canada Approach: Qualitative |
| Chow, C., Vallance, K., Stockwell, T., Macdonald, S., Martin, G., Ivsins, A., ... & Duff, C. (2013). Sexual identity and drug use harm among high-risk, active substance users. Culture, health & sexuality, 15(3), 311–326. | Age: Range = 14–76; mean = 30.5 Gender: M, F, Transgender LGBTQ+ Inclusion: Gay, lesbian, bisexual, transgender individuals Sample Size: 2353 Location: Vancouver and Victoria, British Columbia Approach: Qualitative |
| Clarke, M. P., & Coughlin, J. R. (2012). Prevalence of smoking among the lesbian, gay, bisexual, transsexual, transgender and queer (LGBTTQ) subpopulations in Toronto—The Toronto Rainbow Tobacco Survey (TRTS). Canadian journal of public health, 103(2), 132–136. | Age: Range =13–91 mean = 35.3 Gender: M, F and Transgender LGBTQ+ Inclusion: lesbian, gay, bisexual, transsexual, transgender and queer individuals Sample Size: 3,140 Location: Toronto, Ontario Approach: Quantitative |
| Colpitts, E., & Gahagan, J. (2016). “I feel like I am surviving the health care system”: understanding LGBTQ health in Nova Scotia, Canada. BMC Public Health, 16(1), 1005–1012, doi:10.1186/s12889-016-3675-8. | Age: Range = mid 20’s–late 60’s Gender: Not reported LGBTQ+ Inclusion: LGBTQ individuals Sample Size: 20 Location: Truro and Halifax, Nova Scotia Approach: Qualitative |
| Cox, J., Beauchemin, J., & Allard, R. (2004). HIV status of sexual partners is more important than antiretroviral treatment related perceptions for risk taking by HIV positive MSM in Montreal, Canada. Sexually Transmitted Infections, 80(6), 518–523, doi:10.1136/sti.2004.011288. | Age: Range = 24–73; mean = 45 Gender: M LGBTQ+ Inclusion: Men who have sex with men Sample Size: 346 Location: Montreal, Quebec Approach: Quantitative |
| Das, A. (2012). LGBTQ Women and Mental Health “Recovery.” Psychiatric Rehabilitation Journal, 35(6), 474–475, doi:10.1037/h0094583. | Age: Range = 24–66; mean = N/A Gender: F LGBTQ+ Inclusion: LGBTQ women Sample Size: 13 Location: Southern Ontario Approach: Qualitative |
| Deonarine, A., Ogilvie, G., Montgomery, C., Makaroff, S., Holgerson, N., Grennan, T., ... & Wong, J. (2016). Trends in Syphilis partner notification among gay, bisexual, and other men who have sex with men in British Columbia, 2010 to 2013. Sexually Transmitted Diseases, 43(8), 489–493. | Age: All years; mean = 42; SD = 12 years 70+: 5 Gender: M LGBTQ+ Inclusion: Men who have sex with men Sample Size: 350 Location: British Columbia Approach: Quantitative |
| de Pokomandy, A., Rouleau, D., Ghattas, G., Vézina, S., Coté, P., Macleod, J., Allaire, G., Franco, E., Coutlée, F., Allaire, G., Baril, J., Boissonnault, M., Charest, L., Charron, M., Coté, P., Coté, S., Coutlée, F., de Pokomandy, A., Dion, H., … Franco, E. (2009). Prevalence, clearance, and incidence of anal human papillomavirus infection in HIV-infected men: the HIPVIRG cohort study. The Journal of Infectious Diseases, 199(7), 965–973, doi:10.1086/597207 | Age: Range = 21–66; mean = 43 60+: 5 Gender: M LGBTQ+ Inclusion: Men who have sex with men Sample Size: 247 Location: Montreal, Quebec Approach: Quantitative |
| Dufour, A., Alary, M., Otis, J., Noël, R., Remis, R. S., Mâsse, B., ... & Vincelette, J. (2000). Correlates of risky behaviors among young and older men having sexual relations with men in Montreal, Quebec, Canada. JAIDS-HAGERSTOWN MD-, 23(3), 272–278. | Age: Range = 16–73; mean = 33 Gender: M LGBTQ+ Inclusion: Men who have sex with men Sample Size: 810 Location: Montreal, Quebec Approach: Quantitative |
| Dufour, A., Alary, M., Otis, J., Remis, R. S., Mâsse, B., Turmel, B., ... & Omega Study Group. (2000). Risk behaviours and HIV infection among men having sexual relations with men: Baseline characteristics of participants in the Omega Cohort Study, Montreal, Quebec, Canada. Canadian Journal of Public Health, 91(5), 345–349. | Age: Range = 16–73; mean = 33 Gender: M LGBTQ+ Inclusion: Men who have sex with men Sample Size: 810 Location: Montreal, Quebec Approach: Quantitative |
| Dufour, A., Remis, R. S., Alary, M., Otis, J., Mâsse, B., Turmel, B., ... & Omega Study Group. (1999). Factors associated with hepatitis B vaccination among men having sexual relations with men in Montreal, Quebec, Canada. Sexually Transmitted Diseases, 26(6), 317-324. | Age: Range = 16–73; mean = 34 Gender: M LGBTQ+ Inclusion: Men who have affective and sexual relations with men Sample Size: 653 Location: Montreal, Quebec Approach: Quantitative |
| Eady, A., Dobinson, C., & Ross, L. E. (2011). Bisexual people’s experiences with mental health services: A qualitative investigation. Community Mental Health Journal, 47(4), 378–389. | Age: Range = 16–69 60+: 2 Gender: M, F, Transgender LGBTQ+ Inclusion: Bisexual male, female and transgender individuals Sample Size: 55 Location: Ontario Approach: Qualitative |
| Ferro, S., & Salit, I. E. (1992). HIV infection in patients over 55 years of age. Journal of Acquired Immune Deficiency Syndromes, 5(4), 348–353. | Age: (1) Range = 55–72; mean = 60.1; (2) Range = 21-39; mean = 30.1 Gender: LGBTQ+ Inclusion: HIV Positive Individuals Sample Size: (1) N = 33, (2) N = 58 Location: Toronto, Ontario Approach: Quantitative |
| Furlotte, C., Gladstone, J. W., Cosby, R. F., & Fitzgerald, K. (2016). “Could we hold hands?”: Older lesbian and gay couples. Canadian Journal on Aging, 35(4), 432–446. | Age: Range = 39–75, mean = N/A Gender: M and F LGBTQ+ Inclusion: Same-sex couples Sample Size: 24 Location: Canada Approach: Quantitative |
| Furlotte, C., & Schwartz, K. (2017). Mental health experiences of older adults living with HIV: Uncertainty, stigma, and approaches to resilience. Canadian Journal on Aging/La Revue canadienne du vieillissement, 36(2), 125–140. | Age: Range = 52–67; mean = 60 Gender: M and F LGBTQ+ Inclusion: Gay, bisexual and two-spirited individuals Sample Size: 11 Location: Ottawa, Ontario Approach: Qualitative |
| Gaudreau, C., Ratnayake, R., Pilon, P., Gagnon, S., Roger, M., & Levesque, S. (2011). Ciprofloxacin-resistant Shigella sonnei among men who have sex with men, Canada, 2010. Emerging Infectious Diseases, 17(9), 1747–1750, doi:10.3201/eid1709.102034 | Age: M: Range = 20–65; mean = 40, F: Range = 45–50; mean = N/A 65+: 1 Gender: M and F LGBTQ+ Inclusion: Men who have sex with men Sample Size: 13 Location: Montreal, Quebec Approach: Mixed-methods |
| Giblon, R., & Bauer, G. (2017). Health care availability, quality, and unmet need: a comparison of transgender and cisgender residents of Ontario, Canada. BMC Health Services Research, 17(1), 283, doi:10.1186/s12913-017-2226-z. | Age: 16+; mean = N/A 65+: 2.5% Gender: M, F, Transgender LGBTQ+ Inclusion: Transgender men and women Sample Size: 433 Location: Ontario Approach: Quantitative |
| Gilbert, M., Hottes, T. S., Kerr, T., Taylor, D., Fairley, C. K., Lester, R., ... & Ogilvie, G. (2013). Factors associated with intention to use internet-based testing for sexually transmitted infections among men who have sex with men. Journal of Medical Internet Research, 15(11), e254. | Age: Range = 13–84; mean = 30.1 Gender: M LGBTQ+ Inclusion: Gay and bisexual men Sample Size: 8388 Location: Canada Approach: Qualitative |
| Godin, G., Myers, T., Lambert, J., Calzavara, L., & Locker, D. (1997). Understanding the intention of gay and bisexual men to take the HIV antibody test. AIDS education and prevention: official publication of the International Society for AIDS Education, 9(1), 31–41. | Age: Range = 16–75 mean = 32.7 Gender: M LGBTQ+ Inclusion: gay and bi-sexual men Sample Size: (Total sample)= 4803 (Included Sample)= 1512 Location: Canada Approach: Quantitative |
| Grigorovich, A. (2015a). Negotiating sexuality in home care settings: older lesbians and bisexual women’s experiences. Culture, Health & Sexuality, 17(8), 947–961, doi:10.1080/13691058.2015.1011237 | Age: Range = 55–72; mean = 63.9 Gender: F LGBTQ+ Inclusion: Women who identify as lesbian, bisexual or related term Sample Size: 16 Location: Ontario Approach: Qualitative |
| Grigorovich, A. (2015b). Restricted access: Older lesbian and bisexual women’s experiences with home care services. Research on Aging, 37(7), 763–783. | Age: Range = 55–72; mean = 63.9 Gender: F LGBTQ+ Inclusion: Lesbian and bisexual women Sample Size: 16 Location: Ontario Approach: Qualitative |
| Grigorovich, A. (2016). The meaning of quality of care in home care settings: Older lesbian and bisexual women’s perspectives. Scandinavian Journal of Caring Sciences, 30(1), 108–116. | Age: Range = 55–72; mean = 64 Gender: F LGBTQ+ Inclusion: Lesbian and bisexual women Sample Size: 16 Location: Ontario Approach: Qualitative |
| Harbin, A., Beagan, B., & Goldberg, L. (2012). Discomfort, judgment, and health care for queers. Journal of Bioethical Inquiry, 9(2), 149–160, doi:10.1007/s11673-012-9367-x. | Age: Range = 23–73; mean = N/A 60+: 2 Gender: F, Non-binary, Transgender LGBTQ+ Inclusion: Women who identify as lesbian, bisexual, queer or transgender Sample Size: 19 Location: Halifax, Nova Scotia Approach: Qualitative |
| Hogg, R. S., Craib, K. J., Willoughby, B., Sestak, P., Montaner, J. S., & Schechter, M. T. (1993). Sociodemographic correlates for risk-taking behaviour among HIV seronegative homosexual men. Canadian journal of public health= Revue canadienne de sante publique, 84(6), 423–426. | Age: Risk-takers: Range = 22–47; mean = 35, Controls: Range = 24-66, mean = 40 Gender: M LGBTQ+ Inclusion: Gay men Sample Size: 139 Location: Vancouver, British Columbia Approach: Quantitative |
| Hoffarth, M., & Bogaert, A. (2017). Opening the closet door: Openness to experience, masculinity, religiosity, and coming out among same-sex attracted men. Personality and Individual Differences, 109, 215–219, doi:10.1016/j.paid.2017.01.011. | Age: Range = 15–78 mean = 36.25 Gender: M LGBTQ+ Inclusion: Same sex attracted men Sample Size: 257 Location: Ontario, Canada Approach: Quantitative |
| Humble, Á. (2013). Moving from ambivalence to certainty: older same-sex couples marry in Canada. Canadian Journal on Aging = La Revue Canadienne Du Vieillissement, 32(2), 131–144, doi:10.1017/S0714980813000196. | Age: Range = 42–72; mean = 54 Gender: M and F LGBTQ+ Inclusion: Lesbian women and gay and bisexual men Sample Size: 28 Location: Nova Scotia Approach: Qualitative |
| Katz, A. (2009). Gay and lesbian patients with cancer. Oncology Nursing Forum, 36(2), 203–207, doi:10.1188/09.ONF.203-207. | Age: Range = 39–69; mean = 41.9 65+: 1 Gender: M and F LGBTQ+ Inclusion: Lesbian women and gay men Sample Size: 7 Location: Mid-sized Canadian city Approach: Qualitative |
| Lacombe-Duncan, A., & Logie, C. (2016). Correlates of clinical breast examination among lesbian, gay, bisexual, and queer women. Canadian Journal of Public Health, 107(4-5), e467–e472, doi:10.17269/CJPH.107.5351. | Age: Range = 18–70; mean = N/A Gender: F, Non-Binary LGBTQ+ Inclusion: Lesbian, queer, bisexual, gay or other women Sample Size: 414 Location: Greater Toronto Area, Ontario Approach: Quantitative |
| Lee, J. A. (1989). Invisible men: Canada’s aging homosexuals. Can they be assimilated into Canada’s “liberated” gay communities?. Canadian Journal on Aging/La Revue Canadienne du Vieillissement,8(1), 79–97. | Age: (1) Range = does not specify; (2) Range = 50–80; mean = 60.5 Gender: M LGBTQ+ Inclusion: Older gay men Sample Size: (1) N = does not specify; (2) N = 47 Location: Canada Approach: Qualitative |
| Lessard, D., Lebouché, B., Engler, K., & Thomas, R. (2016). An analysis of socio-demographic and behavioural factors among immigrant MSM in Montreal from an HIV-testing site sample. The Canadian Journal of Human Sexuality, 25(1), 53–60. | Age: Range = 17–75; mean = 37.5 Gender: M LGBTQ+ Inclusion: Men who have sex with men, gay and bisexual males Sample Size: 1353 Location: Montreal, Quebec Approach: Quantitative |
| Lessard, D., Lebouché, B., Engler, K., Thomas, R., & Machouf, N. (2015). Explaining the appeal for immigrant men who have sex with men of a community-based rapid HIV-testing site in Montreal (Actuel sur Rue). AIDS Care, 27(9), 1098–1103. | Age: Range = 18–72; mean = 33 Gender: M LGBTQ+ Inclusion: Men who have sex with men Sample Size: 40 Location: Montreal, Quebec Approach: Qualitative |
| Liboro, R., & Walsh, R. (2016). Understanding the irony: Canadian gay men living with HIV/AIDS, their Catholic devotion, and greater well-being. Journal of Religion and Health, 55(2), 650–670, doi:10.1007/s10943-015-0087-5. | Age: Range = 31–70; mean = N/A Gender: M LGBTQ+ Inclusion: Gay males Sample Size: 9 Location: Greater Toronto Area, Ontario Approach: Qualitative |
| Logie, C., & Earnshaw, V. (2015). Adapting and validating a scale to measure sexual stigma among lesbian, bisexual and queer women. PLoS ONE, 10(2), doi:10.1371/journal.pone.0116198. | Age: 18+, Phase 2: Range = 18–70; mean = 31.38, Phase 3: Range = 22–24; mean = 28.69 Gender: F, Non-Binary LGBTQ+ Inclusion: Lesbian, bisexual and/or queer women Sample Size: Phase 1: 10, Phase 2: 466, Phase 3: 44 Location: Toronto, Ontario and Calgary, Alberta Approach: Qualitative |
| Logie, C., Lacombe-Duncan, A., MacKenzie, R.K. & Poteat, T. (2016). Minority stress and safer sex practices among sexual minority women in Toronto, Canada: Results from a cross-sectional internet-based survey. LGBT Health 3(6): 407–415, doi:10.1089/lgbt.2016. | Age: (2) Range =18–70 mean = 31.38 (3) Range =22–44 mean = 28.69 Gender: F LGBTQ+ Inclusion: Lesbian, Bisexual and Queer Women Sample Size: (1) 10 (2) 466 (3) 44 Location: Toronto, Ontario and Calgary, Alberta Approach: Mixed-methods |
| Low-Beer, S., Bartholomew, K., Weber, A. E., Chan, K., Landolt, M., Oram, D., Schilder, A., & Hogg, R. (2010). A demographic and health profile of gay and bisexual men in a large Canadian urban setting. AIDS Care, 14(1), 111–115, doi:10.1080/09540120220097982. | Age: 20+; mean = N/A 65+: 22% of gay and bisexual males Gender: M LGBTQ+ Inclusion: Gay and bisexual males Sample Size: 1176 Location: West-End Vancouver, British Columbia Approach: Qualitative |
| Lyon, K. A., & Frohard-Dourlent, H. (2015). “Let’s Talk about the Institution”: Same-Sex Common-Law Partners Negotiating Marriage Equality and Relationship Legitimacy. Canadian Review of Sociology/Revue canadienne de sociologie, 52(4), 402–428. | Age: Range = 23–63; mean = 38 60+: 1 Gender: M, F, Non-binary LGBTQ+ Inclusion: Gay men and lesbian, same-sex, queer and unknown women Sample Size: 22 Location: Toronto, Ontario Approach: Qualitative |
| Macintosh, H., Reissing, E., & Andruff, H. (2010). Same-sex marriage in Canada: The impact of legal marriage on the first cohort of gay and lesbian Canadians to wed. The Canadian Journal of Human Sexuality, 19(3), 79–90. | Age: Range = 23–72; mean = 48.8 Gender: M and F LGBTQ+ Inclusion: Gay men, lesbian women, same-sex couples Sample Size: 52 Location: Ontario and British Columbia Approach: Qualitative |
| Moody, C., & Smith, N. G. (2013). Suicide protective factors among trans adults. Archives of Sexual Behavior,42(5), 739–752. | Age: Range = 18–75; mean = 36.75; SD = 13.01 Gender: M, F, Transgender LGBTQ+ Inclusion: Transgender men and women Sample Size: 133 Location: Canada Approach: Qualitative |
| Morrison, M. A. (2012). Psychological health correlates of perceived discrimination among Canadian gay men and lesbian women. Canadian Journal of Community Mental Health, 30(2), 81–98. | Age: Range = 18–78; mean = 35.65; SD = 12.96 Gender: M and F LGBTQ+ Inclusion: Gay men and lesbian women Sample Size: 348 Location: Canada Approach: Qualitative |
| Murray, J., & Adam, B. (2001). Aging, sexuality, and HIV issues among older gay men. The Canadian Journal of Human Sexuality, 10(3), 75–90. | Age: Range = 40–79; mean = 45.4 65+: 1 Gender: M LGBTQ+ Inclusion: Gay men Sample Size: 27 Location: Toronto, Ontario Approach: Qualitative |
| Myers, T., Allman, D., Calzavara, L., Morrison, K., Marchand, R., & Major, C. (1999). Gay and bisexual men’s sexual partnerships and variations in risk behaviour. Canadian Journal of Human Sexuality, 8(2), 115–126. | Age: Range = 15–72; mean = 31.9 Gender: M LGBTQ+ Inclusion: Gay and bisexual men Sample Size: ~500 Location: Canada Approach: Quantitative |
| Myers, T., Godin, G., Lambert, J., Calzavara, L., & Locker, D. (1996). Sexual risk and HIV-testing behaviour by gay and bisexual men in Canada. AIDS Care, 8(3), 297-310. | Age: Range = 16–75; mean = 32.7; SD = 8.8 Gender: M LGBTQ+ Inclusion: Gay and bisexual men Sample Size: 4803 Location: Canada Approach: Qualitative |
| Myers, T., Orr, K. W., Locker, D., & Jackson, E. A. (1993). Factors affecting gay and bisexual men’s decisions and intentions to seek HIV testing. American Journal of Public Health, 83(5), 701–704. | Age: Range = 18–70; mean = 34.3 Gender: M LGBTQ+ Inclusion: Gay and bisexual men Sample Size: 1295 Location: Toronto, Ontario Approach: Quantitative |
| Myers, T., Tudiver, F. G., Kurtz, R. G., Jackson, E. A., Orr, K. W., Rowe, C. J., & Bullock, S. L. (1992). The Talking Sex Project: descriptions of the study population and correlates of sexual practices at baseline. Canadian journal of public health= Revue canadienne de sante, 83(1), 47–52. | Age: Range = 14–72; mean = 32 Gender: M LGBTQ+ Inclusion: Gay and bisexual men Sample Size: 612 Location: Toronto, Ontario Approach: Quantitative |
| O’Neill, T. J., Raboud, J. M., Tinmouth, J., Rourke, S. B., Gardner, S., Cooper, C., ... & OHTN Cohort Study Team. (2017). Burden and risk factors for gastrointestinal symptom distress in HIV patients in the modern antiretroviral era. AIDS care, 29(2), 156–167. | Age: 16+; mean = 45.7 Gender: M LGBTQ+ Inclusion: Men who have sex with men Sample Size: 1532 Location: Ontario Approach: Qualitative |
| Persson, T., Pfaus, J., & Ryder, A. (2015). Explaining mental health disparities for non-monosexual women: Abuse history and risky sex, or the burdens of non-disclosure? Social Science & Medicine, 128, 334–335, doi:10.1016/j.socscimed.2014.08.038. | Age: Range = 18–66; mean = 24.4 Gender: F LGBTQ+ Inclusion: Bisexual, mostly lesbian women Sample Size: 388 Location: National |
| Ploeg, J., Lohfeld, L., & Walsh, C. (2013). What is “elder abuse”? Voices from the margin: The views of underrepresented Canadian older adults. Journal of Elder Abuse & Neglect, 25(5), 396–424, doi:10.1080/08946566.2013.780956. | Age: 60+; mean = N/A Gender: F LGBTQ+ Inclusion: Lesbian women Sample Size: 87 Location: Canada Approach: Qualitative |
| Rank, C., Gilbert, M., Ogilvie, G., Jayaraman, G. C., Marchand, R., Trussler, T., Hogg, R. S., Gustafson, R., Wong, T., & The ManCount Study Team (2012). Acceptability of human papillomavirus and sexual experience prior to disclosure to health care providers among men who have sex with men in Vancouver, Canada: Implications for targeted vaccination programs. Vaccine, 30, 5755–5760 | Age: Range = 19–83; mean = N/A Gender: M LGBTQ+ Inclusion: Men who have sex with men, gay and bisexual men Sample Size: 1169 Location: Vancouver, British Columbia |
| Remis, R., Alary, M., Otis, J., & Hogg, R. (2000). HIV infection and risk behaviors in young gay and bisexual men / the authors respond. Canadian Medical Association. Journal, 163(1), 14. | Age: Range = 18–73; mean = 34.5 Gender: M LGBTQ+ Inclusion: Men who have sex with men Sample Size: 650 Location: Montreal, Quebec Approach: Quantitative |
| Remis, R., Liu, J., Loutfy, M., Tharao, W., Rebbapragada, A., Huibner, S., Kesler, M., Halpenny, R., Grennan, T., Brunetta, J., Smith, G., Reko, T., & Kaul, R. (2016). Prevalence of sexually transmitted viral and bacterial infections in HIV-positive and HIV-negative men who have sex with men in Toronto. PloS One, 11(7), e0158090, doi:10.1371/journal.pone.0158090. | Age: Range=22+ Mean = 44.35 Gender: M LGBTQ+ Inclusion: Gay men and other men who have sex with men Sample Size: 442 Location: Toronto, Ontario Approach: Quantitative |
| Ross, L. E., Bauer, G. R., MacLeod, M. A., Robinson, M., MacKay, J., & Dobinson, C. (2014). Mental health and substance use among bisexual youth and non-youth in Ontario, Canada. PLoS one, 9(8), e101604. | Age: 16+; mean = N/A 55+: 12 Gender: M and F LGBTQ+ Inclusion: Bisexual males and females Sample Size: 405 Location: Ontario Approach: Quantitative |
| Ross, L. E., O’Gorman, L., MacLeod, M. A., Bauer, G. R., MacKay, J., & Robinson, M. (2016). Bisexuality, poverty and mental health: A mixed methods analysis. Social Science & Medicine, 156, 64–72. | Age: Range = 25–66; mean = N/A 55+: 12 Gender: M, F, Non-Binary, Transgender LGBTQ+ Inclusion: Bisexual men and women, genderqueer, 2-spirited, trans men and women, and other Sample Size: 302 Location: Ontario Approach: Mixed-methods |
| Rotondi, N. K., Bauer, G. R., Scanlon, K., Kaay, M., Travers, R., & Travers, A. (2013). Nonprescribed hormone use and self-performed surgeries: “Do-it-yourself” transitions in transgender communities in Ontario, Canada. American Journal of Public Health, 103(10), 1830–1836. | Age: 16+ 65+: 2.5% Gender: M, F, Transgender LGBTQ+ Inclusion: Transgender men and women Sample Size: 433 Location: Ontario Approach: Qualitative |
| Scheim, A. I., & Bauer, G. R. (2015). Sex and gender diversity among transgender persons in Ontario, Canada: results from a respondent-driven sampling survey. The Journal of Sex Research, 52(1), 1–14. | Age: Range = 16–77; mean = N/A Gender: M, F, Non-Binary, Transgender LGBTQ+ Inclusion: Transgender males, females and fluid Sample Size: 433 Location: Ontario Approach: Quantitative |
| Scheim, A., Bauer, G., & Shokoohi, M. (2016). Heavy episodic drinking among transgender persons: Disparities and predictors. Drug and Alcohol Dependence, 167, 156–162, doi:10.1016/j.drugalcdep.2016.08.011. | Age: 16+; mean = N/A Gender: M, F, Non-Binary, Transgender, Transsexual LGBTQ+ Inclusion: Transgender, transsexual, or transitioned including genderqueer or other non-binary gender identities Sample Size: 433 Location: Ontario Approach: Quantitative |
| Shuper, P. A., & Fisher, W. A. (2008). The role of sexual arousal and sexual partner characteristics in HIV+ MSM’s intentions to engage in unprotected sexual intercourse. Health Psychology, 27(4), 445. | Age: Range = 26–66; mean = 44 Gender: M LGBTQ+ Inclusion: Men who have sex with men Sample Size: 77 Location: Ontario Approach: Quantitative |
| Sinding, C., Grassau, P., & Barnoff, L. (2007). Community support, community values: The experiences of lesbians diagnosed with cancer. Women & Health, 44(2), 59–79. | Age: Range = 36–72; mean = 50 Gender: F LGBTQ+ Inclusion: Lesbian women Sample Size: 26 Location: Ontario Approach: Quantitative |
| Sinding, C., Barnoff, L., & Grassau, P. (2004). Homophobia and heterosexism in cancer care: The experiences of lesbians. CJNR (Canadian Journal of Nursing Research), 36(4), 170–188. | Age: Range = 36–72; mean = 50 Gender: F LGBTQ+ Inclusion: Lesbian women Sample Size: 26 Location: Ontario Approach: Qualitative |
| Soskolne, C., Coates, R., & Sears, A (1986). Characteristics of a male homosexual/bisexual study population in Toronto, Canada. Canadian Journal of Public Health = Revue Canadienne de Sante Publique, 77(1), 12–16, doi:10.1007/s10508-009-9556-9. | Age: Range = 17–67; mean = 30.8 Gender: M LGBTQ+ Inclusion: Men who have sex with men, gay and bisexual men Sample Size: 339 Location: Toronto, Ontario Approach: Quantitative |
| Wallach, I., & Brotman, S. (2013). Ageing with HIV/AIDS: A scoping study among people aged 50 and over living in Quebec. Ageing & Society, 33(7), 1212–1242, doi:10.1017/S0144686X12000529. | Age: Range = 50–68; mean = N/A Gender: M and F LGBTQ+ Inclusion: Gay men and women Sample Size: 9 Location: Quebec Approach: Qualitative |
| Yuan, L., & Robinson, G. (1994). Hepatitis B vaccination and screening for markers at a sexually transmitted disease clinic for men. Canadian Journal of Public Health = Revue Canadienne de Sante Publique, 85(5), 338–341. | Age: Gay/Bisexual Men Range = 16–68; mean = 30.3, Heterosexual Men Range = 16–51; mean = 27.4 Gender: M LGBTQ+ Inclusion: Gay and bisexual men Sample Size: 887 Location: Toronto, Ontario Approach: Quantitative |
References
- Holstein, M.B.; Minkler, M. Self, society, and the “new gerontology”. Gerontologist 2003, 43, 787–796. [Google Scholar] [CrossRef]
- Martinson, M.; Berridge, C. Successful aging and its discontents: A systematic review of the social gerontology literature. Gerontologist 2015, 55, 58–69. [Google Scholar] [CrossRef]
- Khan, M.; Kobayashi, K.; Lee, S.M.; Vang, Z. (In)visible minorities in Canadian health data and research. Popul. Chang. Lifecourse Strateg. Knowl. Clust. Discuss. Pap. Ser. 2015, 34. Available online: https://ir.lib.uwo.ca/pclc/vol3/iss1/5 (accessed on 3 June 2021).
- Koehn, S.; Neysmith, S.; Kobayashi, K.; Khamisa, H. Revealing the shape of knowledge using an intersectionality lens: Results of a scoping review on the health and health care of ethnocultural minority older adults. Ageing Soc. 2013, 33, 437–464. [Google Scholar] [CrossRef]
- Wilson, K.; Stinchcombe, A.; Ismail, M.; Kortes-Miller, K. LGBTQ2+ aging in Canada: Building the evidence and informing action. Can. J. Hum. Sex. 2019, 28, 257–260. [Google Scholar] [CrossRef]
- Hooper, T.; Kinsman, G.; Pearlston, K. Anti-69 FAQ: If decriminalization didn’t happen in 1969, when did it happen? Available online: https://anti-69.ca/faq/#4 (accessed on 3 June 2021).
- CBC Digital Archives. The First Gay March [Video File]. 1971. Available online: https://www.cbc.ca/archives/entry/the-first-gay-march (accessed on 3 June 2021).
- Queer Events. History of Canadian Pride. 2020. Available online: https://www.queerevents.ca/canada/pride/history (accessed on 3 June 2021).
- Knegt, P. The Fruit Machine: Why Every Canadian Should Learn about this Country’s ’Gay Purge’. Available online: https://www.cbc.ca/arts/the-fruit-machine-why-every-canadian-should-learn-about-this-country-s-gay-purge-1.4678718 (accessed on 30 May 2018).
- CBC Radio. ’A Small Victory’: LGBTQ Canadians ’Purged’ from Military and Public Service Await Apology. Available online: https://www.cbc.ca/radio/thecurrent/the-current-for-november-24-2017-1.4416453/a-small-victory-lgbtq-canadians-purged-from-military-and-public-service-await-apology-1.4416502 (accessed on 4 November 2017).
- Orisini, M.; Hindmarch, S.; Gagnon, M. Seeing Red: HIV/AIDS and Public Policy in Canada; Hindmarch, S., Orsini, M., Gagnon, M., Eds.; University of Toronto Press: Toronto, ON, Canada, 2018. [Google Scholar]
- Meyer, I.H. Resilience in the study of minority stress and health of sexual and gender minorities. Psychol. Sex. Orientat. Gend. Divers. 2015, 2, 209–213. [Google Scholar] [CrossRef]
- Fredriksen-Goldsen, K.I.; Muraco, A. Aging and sexual orientation: A 25-year review of the literature. Res. Aging 2010, 32, 372–413. [Google Scholar] [CrossRef] [PubMed]
- Murray, E.; Numer, M.; Merritt, B.; Gahagan, J.; Comber, S. Healthy aging among LGBT seniors in Canada: A review of the literature. Int. J. Health Wellness Soc. 2011, 1, 179–192. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- De Pokomandy, A.; Rouleau, D.; Ghattas, G.; Vézina, S.; Coté, P.; Macleod, J.; Allaire, G.; Franco, E.; Coutlée, F.; Allaire, G.; et al. Prevalence, clearance, and incidence of anal human papillomavirus infection in HIV-infected men: The HIPVIRG cohort study. J. Infect. Dis. 2009, 199, 965–973. [Google Scholar] [CrossRef]
- Chow, C.; Vallance, K.; Stockwell, T.; Macdonald, S.; Martin, G.; Ivsins, A.; Duff, C. Sexual identity and drug use harm among high-risk, active substance users. Cult. Health Sex. 2013, 15, 311–326. [Google Scholar] [CrossRef] [PubMed]
- Remis, R.; Liu, J.; Loutfy, M.; Tharao, W.; Rebbapragada, A.; Huibner, S.; Kesler, M.; Halpenny, R.; Grennan, T.; Brunetta, J.; et al. Prevalence of sexually transmitted viral and bacterial infections in HIV-positive and HIV-negative men who have sex with men in Toronto. PLoS ONE 2016, 11, e0158090. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.; Beauchemin, J.; Allard, R. HIV status of sexual partners is more important than antiretroviral treatment related perceptions for risk taking by HIV positive MSM in Montreal, Canada. Sex. Transm. Infect. 2004, 80, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Soskolne, C.; Coates, R.; Sears, A. Characteristics of a male homosexual/bisexual study population in Toronto, Canada. Can. J. Public Health Rev. Can. De Sante Publique 1986, 77, 12–16. [Google Scholar] [CrossRef]
- Chandarana, P.C.; Conlon, P.; Noh, S.A.M.U.E.L.; Field, V.A. The AIDS dilemma: Worry and concern over AIDS. Can. J. Public Health Rev. Can. de Sante Publique 1990, 81, 222–225. [Google Scholar]
- Ferro, S.; Salit, I.E. HIV infection in patients over 55 years of age. J. Acquir. Immune Defic. Syndr. 1992, 5, 348–353. [Google Scholar]
- Gaudreau, C.; Ratnayake, R.; Pilon, P.; Gagnon, S.; Roger, M.; Levesque, S. Ciprofloxacin-resistant Shigella sonnei among men who have sex with men, Canada, 2010. Emerg. Infect. Dis. 2011, 17, 1747–1750. [Google Scholar] [CrossRef]
- Deonarine, A.; Ogilvie, G.; Montgomery, C.; Makaroff, S.; Holgerson, N.; Grennan, T.; Wong, J. Trends in Syphilis partner notification among gay, bisexual, and other men who have sex with men in British Columbia, 2010 to 2013. Sex. Transm. Dis. 2016, 43, 489–493. [Google Scholar] [CrossRef]
- Remis, R.; Alary, M.; Otis, J.; Hogg, R. HIV infection and risk behaviors in young gay and bisexual men/the authors respond. Can. Med Assoc. J. 2000, 163, 14. [Google Scholar]
- Rank, C.; Gilbert, M.; Ogilvie, G.; Jayaraman, G.C.; Marchand, R.; Trussler, T.; Hogg, R.S.; Gustafson, R.; Wong, T. The ManCount Study Team Acceptability of human papillomavirus and sexual experience prior to disclosure to health care providers among men who have sex with men in Vancouver, Canada: Implications for targeted vaccination programs. Vaccine 2012, 30, 5755–5760. [Google Scholar] [CrossRef]
- Yuan, L.; Robinson, G. Hepatitis B vaccination and screening for markers at a sexually transmitted disease clinic for men. Can. J. Public Health Rev. Can. de Sante Publique 1994, 85, 338–341. [Google Scholar]
- Myers, T.; Tudiver, F.G.; Kurtz, R.G.; Jackson, E.A.; Orr, K.W.; Rowe, C.J.; Bullock, S.L. The Talking Sex Project: Descriptions of the study population and correlates of sexual practices at baseline. Can. J. Public Health Rev. Can. de Sante Publique 1992, 83, 47–52. [Google Scholar]
- Dufour, A.; Alary, M.; Otis, J.; Noël, R.; Remis, R.S.; Mâsse, B.; Vincelette, J. Correlates of risky behaviors among young and older men having sexual relations with men in Montreal, Quebec, Canada. JAIDS-HAGERSTOWN MD- 2000, 23, 272–278. [Google Scholar]
- Dufour, A.; Alary, M.; Otis, J.; Remis, R.S.; Mâsse, B.; Turmel, B. Omega Study Group. Risk behaviours and HIV infection among men having sexual relations with men: Baseline characteristics of participants in the Omega Cohort Study, Montreal, Quebec, Canada. Can. J. Public Health 2000, 91, 345–349. [Google Scholar] [CrossRef]
- Myers, T.; Allman, D.; Calzavara, L.; Morrison, K.; Marchand, R.; Major, C. Gay and bisexual men’s sexual partnerships and variations in risk behaviour. Can. J. Hum. Sex. 1999, 8, 115–126. [Google Scholar]
- Shuper, P.A.; Fisher, W.A. The role of sexual arousal and sexual partner characteristics in HIV+ MSM’s intentions to engage in unprotected sexual intercourse. Health Psychol. 2008, 27, 445. [Google Scholar] [CrossRef] [PubMed]
- Clarke, M.P.; Coughlin, J.R. Prevalence of smoking among the lesbian, gay, bisexual, transsexual, transgender and queer (LGBTTQ) subpopulations in Toronto—The Toronto Rainbow Tobacco Survey (TRTS). Can. J. Public Health 2012, 103, 132–136. [Google Scholar] [CrossRef]
- Brennan, D.; Craig, S.; Thompson, D. Factors associated with a drive for muscularity among gay and bisexual men. Cult. Health Sex. 2012, 14, 1–15. [Google Scholar] [CrossRef]
- Hogg, R.S.; Craib, K.J.; Willoughby, B.; Sestak, P.; Montaner, J.S.; Schechter, M.T. Sociodemographic correlates for risk-taking behaviour among HIV seronegative homosexual men. Can. J. Public Health Rev. Can. De Sante Publique 1993, 84, 423–426. [Google Scholar]
- Lessard, D.; Lebouché, B.; Engler, K.; Thomas, R. An analysis of socio-demographic and behavioural factors among immigrant MSM in Montreal from an HIV-testing site sample. Can. J. Hum. Sex. 2016, 25, 53–60. [Google Scholar] [CrossRef]
- Ross, L.E.; Bauer, G.R.; MacLeod, M.A.; Robinson, M.; MacKay, J.; Dobinson, C. Mental health and substance use among bisexual youth and non-youth in Ontario, Canada. PLoS ONE 2014, 9, e101604. [Google Scholar] [CrossRef] [PubMed]
- Ross, L.E.; O’Gorman, L.; MacLeod, M.A.; Bauer, G.R.; MacKay, J.; Robinson, M. Bisexuality, poverty and mental health: A mixed methods analysis. Soc. Sci. Med. 2016, 156, 64–72. [Google Scholar] [CrossRef]
- Moody, C.; Smith, N.G. Suicide protective factors among trans adults. Arch. Sex. Behav. 2013, 42, 739–752. [Google Scholar] [CrossRef] [PubMed]
- Dufour, A.; Remis, R.S.; Alary, M.; Otis, J.; Mâsse, B.; Turmel, B. Omega Study Group. Factors associated with hepatitis B vaccination among men having sexual relations with men in Montreal, Quebec, Canada. Sex. Transm. Dis. 1999, 26, 317–324. [Google Scholar] [CrossRef]
- Logie, C.H.; Lacombe-Duncan, A.; MacKenzie, R.K.; Poteat, T. Minority stress and safer sex practices among sexual minority women in Toronto, Canada: Results from a cross-sectional internet-based survey. LGBT Health 2016, 3, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Persson, T.; Pfaus, J.; Ryder, A. Explaining mental health disparities for non-monosexual women: Abuse history and risky sex, or the burdens of non-disclosure? Soc. Sci. Med. 2015, 128, 334–335. [Google Scholar] [CrossRef]
- Ploeg, J.; Lohfeld, L.; Walsh, C. What is “elder abuse”? Voices from the margin: The views of underrepresented Canadian older adults. J. Elder Abus. Negl. 2013, 25, 396–424. [Google Scholar] [CrossRef]
- Bauer, G.R.; Travers, R.; Scanlon, K.; Coleman, T.A. High heterogeneity of HIV-related sexual risk among transgender people in Ontario, Canada: A province-wide respondent-driven sampling survey. BMC Public Health 2012, 12, 292. [Google Scholar] [CrossRef]
- Scheim, A.; Bauer, G.; Shokoohi, M. Heavy episodic drinking among transgender persons: Disparities and predictors. Drug Alcohol Depend. 2016, 167, 156–162. [Google Scholar] [CrossRef]
- Rotondi, N.K.; Bauer, G.R.; Scanlon, K.; Kaay, M.; Travers, R.; Travers, A. Nonprescribed hormone use and self-performed surgeries: “Do-it-yourself” transitions in transgender communities in Ontario, Canada. Am. J. Public Health 2013, 103, 1830–1836. [Google Scholar] [CrossRef]
- Godin, G.; Myers, T.; Lambert, J.; Calzavara, L.; Locker, D. Understanding the intention of gay and bisexual men to take the HIV antibody test. AIDS Educ. Prev. Off. Publ. Int. Soc. AIDS Educ. 1997, 9, 31–41. [Google Scholar]
- Myers, T.; Godin, G.; Lambert, J.; Calzavara, L.; Locker, D. Sexual risk and HIV-testing behaviour by gay and bisexual men in Canada. AIDS Care 1996, 8, 297–310. [Google Scholar] [CrossRef]
- Myers, T.; Orr, K.W.; Locker, D.; Jackson, E.A. Factors affecting gay and bisexual men’s decisions and intentions to seek HIV testing. Am. J. Public Health 1993, 83, 701–704. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, M.; Hottes, T.S.; Kerr, T.; Taylor, D.; Fairley, C.K.; Lester, R.; Ogilvie, G. Factors associated with intention to use internet-based testing for sexually transmitted infections among men who have sex with men. J. Med. Internet Res. 2013, 15, e254. [Google Scholar] [CrossRef] [PubMed]
- Brownrigg, B.; Taylor, D.; Phan, F.; Sandstra, I.; Stimpson, R.; Barrios, R.; Lester, R.; Ogilvie, G. Improving linkage to HIV care at low-threshold STI/HIV testing sites: An evaluation of the Immediate Staging Pilot Project in Vancouver, British Columbia. Can. J. Public Health 2017, 108, E79. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lessard, D.; Lebouché, B.; Engler, K.; Thomas, R.; Machouf, N. Explaining the appeal for immigrant men who have sex with men of a community-based rapid HIV-testing site in Montreal (Actuel sur Rue). AIDS Care 2015, 27, 1098–1103. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.; Adam, B. Aging, sexuality, and HIV issues among older gay men. Can. J. Human Sex. 2001, 10, 75–90. [Google Scholar]
- Low-Beer, S.; Bartholomew, K.; Weber, A.E.; Chan, K.; Landolt, M.; Oram, D.; Schilder, A.; Hogg, R. A demographic and health profile of gay and bisexual men in a large Canadian urban setting. AIDS Care 2010, 14, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Brennan, D.J.; Emlet, C.A.; Brennenstuhl, S.; Rueda, S. Socio-demographic profile of older adults with HIV/AIDS: Gender and sexual orientation differences. Can. J. Aging La Rev. Can. Du Vieil. 2013, 32, 31–43. [Google Scholar] [CrossRef]
- O’Neill, T.J.; Raboud, J.M.; Tinmouth, J.; Rourke, S.B.; Gardner, S.; Cooper, C. OHTN Cohort Study Team. Burden and risk factors for gastrointestinal symptom distress in HIV patients in the modern antiretroviral era. AIDS Care 2017, 29, 156–167. [Google Scholar] [CrossRef]
- Furlotte, C.; Schwartz, K. Mental health experiences of older adults living with HIV: Uncertainty, stigma, and approaches to resilience. Can. J. Aging La Rev. Can. du Vieil. 2017, 36, 125–140. [Google Scholar] [CrossRef] [PubMed]
- Liboro, R.; Walsh, R. Understanding the irony: Canadian gay men living with HIV/AIDS, their Catholic devotion, and greater well-being. J. Relig. Health 2016, 55, 650–670. [Google Scholar] [CrossRef]
- Bergeron, S.; Senn, C. Health care utilization in a sample of Canadian lesbian women: Predictors of risk and resilience. Women Health 2003, 37, 19–35. [Google Scholar] [CrossRef] [PubMed]
- Lacombe-Duncan, A.; Logie, C. Correlates of clinical breast examination among lesbian, gay, bisexual, and queer women. Can. J. Public Health 2016, 107, e467–e472. [Google Scholar] [CrossRef] [PubMed]
- Morrison, M.A. Psychological health correlates of perceived discrimination among Canadian gay men and lesbian women. Can. J. Community Ment. Health 2012, 30, 81–98. [Google Scholar] [CrossRef]
- Logie, C.; Earnshaw, V. Adapting and validating a scale to measure sexual stigma among lesbian, bisexual and queer women. PLoS ONE 2015, 10, e0116198. [Google Scholar] [CrossRef]
- Das, A. LGBTQ Women and Mental Health “Recovery”. Psychiatr. Rehabil. J. 2012, 35, 474–475. [Google Scholar] [CrossRef]
- Giblon, R.; Bauer, G. Health care availability, quality, and unmet need: A comparison of transgender and cisgender residents of Ontario, Canada. BMC Health Serv. Res. 2017, 17, 283. [Google Scholar] [CrossRef]
- Brotman, S.; Ryan, B.; Collins, S.; Chamberland, L.; Cormier, R.; Julien, D.; Meyer, E.; Peterkin, A.; Richard, B. Coming out to care: Caregivers of gay and lesbian seniors in Canada. Gerontologist 2007, 47, 490–503. [Google Scholar] [CrossRef] [PubMed]
- Harbin, A.; Beagan, B.; Goldberg, L. Discomfort, judgment, and health care for queers. J. Bioethical Inq. 2012, 9, 149–160. [Google Scholar] [CrossRef]
- Colpitts, E.; Gahagan, J. I feel like I am surviving the health care system: Understanding LGBTQ health in Nova Scotia, Canada. BMC Public Health 2016, 16, 1005–1012. [Google Scholar] [CrossRef][Green Version]
- Grigorovich, A. Negotiating sexuality in home care settings: Older lesbians and bisexual women’s experiences. Cult. Health Sex. 2015, 17, 947–961. [Google Scholar] [CrossRef] [PubMed]
- Grigorovich, A. Restricted access: Older lesbian and bisexual women’s experiences with home care services. Res. Aging 2015, 37, 763–783. [Google Scholar] [CrossRef]
- Grigorovich, A. The meaning of quality of care in home care settings: Older lesbian and bisexual women’s perspectives. Scand. J. Caring Sci. 2016, 30, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Furlotte, C.; Gladstone, J.W.; Cosby, R.F.; Fitzgerald, K. Could we hold hands?: Older lesbian and gay couples. Can. J. Aging 2016, 35, 432–446. [Google Scholar] [CrossRef]
- Chamberland, L. Elderly women, invisible lesbians. Can. J. Community Mental Health Rev. Can. de Sante Ment. Communaut. 2003, 22, 85–103. [Google Scholar] [CrossRef]
- Sinding, C.; Barnoff, L.; Grassau, P. Homophobia and heterosexism in cancer care: The experiences of lesbians. Can. J. Nurs. Res. 2004, 36, 170–188. [Google Scholar] [PubMed]
- Katz, A. Gay and lesbian patients with cancer. Oncol. Nurs. Forum 2009, 36, 203–207. [Google Scholar] [CrossRef][Green Version]
- Eady, A.; Dobinson, C.; Ross, L.E. Bisexual people’s experiences with mental health services: A qualitative investigation. Community Ment. Health J. 2011, 47, 378–389. [Google Scholar] [CrossRef]
- Alderson, K. A phenomenological investigation of same-sex marriage. Can. J. Human Sex. 2004, 13, 107–122. [Google Scholar]
- Macintosh, H.; Reissing, E.; Andruff, H. Same-sex marriage in Canada: The impact of legal marriage on the first cohort of gay and lesbian Canadians to wed. Can. J. Human Sex. 2010, 19, 79–90. [Google Scholar]
- Humble, Á. Moving from ambivalence to certainty: Older same-sex couples marry in Canada. Can. J. Aging La Rev. Can. Du Vieil. 2013, 32, 131–144. [Google Scholar] [CrossRef]
- Lyon, K.; Frohard-Dourlent, H. Let’s Talk about the Institution: Same-sex common-law partners negotiating marriage equality and relationship legitimacy. Can. Rev. Sociol. Rev. Can. De Sociol. 2015, 52, 402–428. [Google Scholar] [CrossRef]
- Lee, J.A. Invisible men: Canada’s aging homosexuals. Can they be assimilated into Canada’s “liberated” gay communities? Can. J. Aging La Rev. Can. Du Vieil. 1989, 8, 79–97. [Google Scholar] [CrossRef]
- Hoffarth, M.; Bogaert, A. Opening the closet door: Openness to experience, masculinity, religiosity, and coming out among same-sex attracted men. Personal. Individ. Differ. 2017, 109, 215–219. [Google Scholar] [CrossRef]
- Meyer, I.H. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol. Bull. 2003, 129, 674–697. [Google Scholar] [CrossRef]
- Wallach, I.; Brotman, S. Ageing with HIV/AIDS: A scoping study among people aged 50 and over living in Quebec. Ageing Soc. 2013, 33, 1212–1242. [Google Scholar] [CrossRef]
- De Vries, B.; Gutman, G.; Soheilipour, S.; Gahagan, J.; Humble, Á.; Mock, S.; Chamberland, L. Advance care planning among older LGBT Canadians: Heteronormative influences. Sexualities 2020, 1–20. [Google Scholar] [CrossRef]
- Stinchcombe, A.; Wilson, K.; Kortes-Miller, K.; Chambers, L.; Weaver, B. Physical and mental health inequalities among aging lesbian, gay, and bisexual Canadians: Cross-sectional results from the Canadian Longitudinal Study on Aging (CLSA). Can. J. Public Health 2018, 109, 833–844. [Google Scholar] [CrossRef]
- Sussman, T.; Brotman, S.; MacIntosh, H.; Chamberland, L.; MacDonnell, J.; Daley, A.; Churchill, M. Supporting lesbian, gay, bisexual, transgender inclusivity in long-term care homes: A Canadian perspective. Can. J. Aging La Rev. Can. Du Vieil. 2018, 37, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Bossio, J.A.; Pukall, C.F.; Bartley, K. You either have it or you don’t: The impact of male circumcision status on sexual partners. Can. J. Hum. Sex. 2015, 24, 104–119. [Google Scholar] [CrossRef]
- Scheim, A.I.; Bauer, G.R. Sex and gender diversity among transgender persons in Ontario, Canada: Results from a respondent-driven sampling survey. J. Sex Res. 2015, 52, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Sinding, C.; Grassau, P.; Barnoff, L. Community support, community values: The experiences of lesbians diagnosed with cancer. Women Health 2007, 44, 59–79. [Google Scholar] [CrossRef] [PubMed]
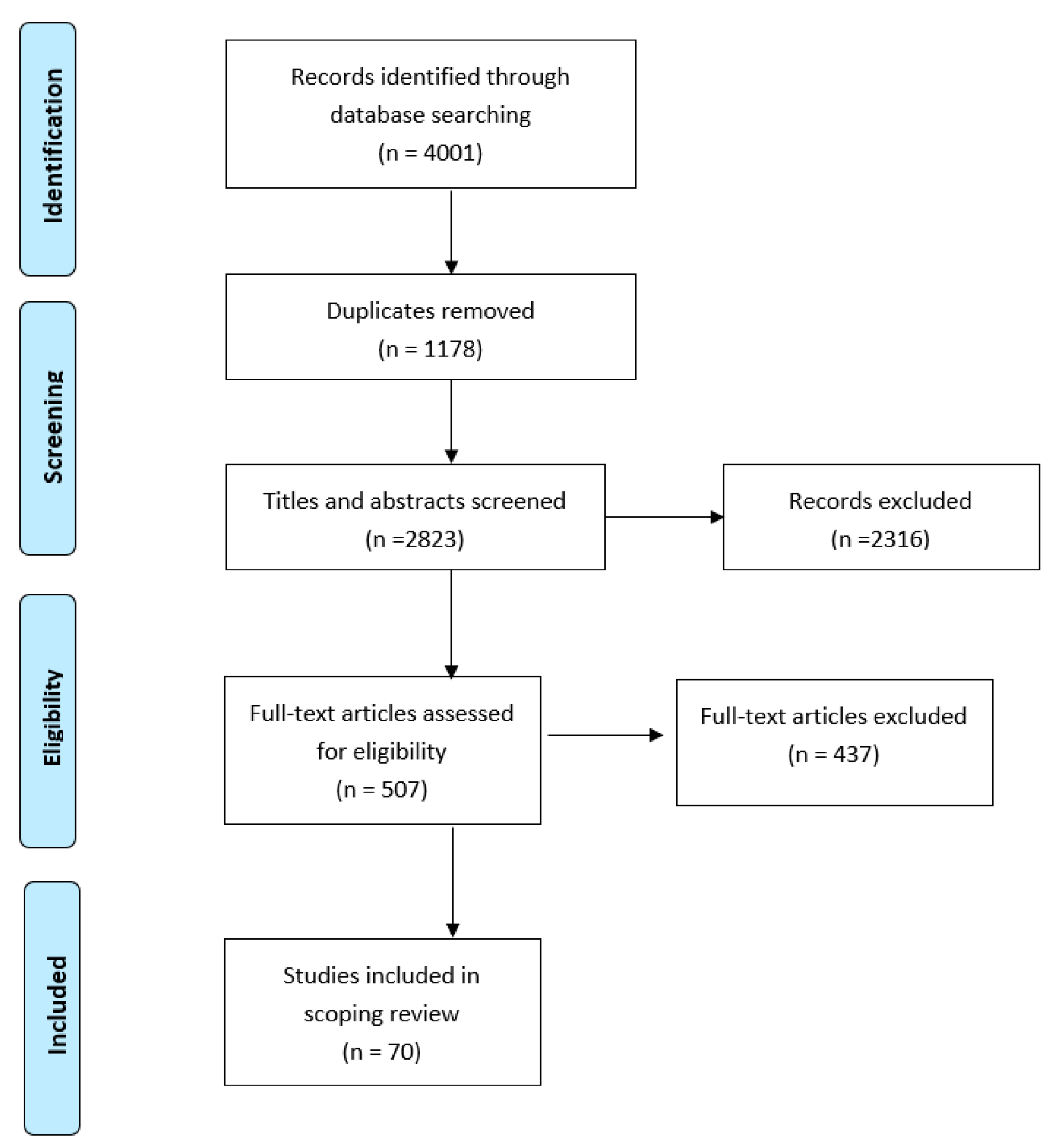
| Database | Initial Results |
|---|---|
| Medline | 1426 |
| PsycINFO | 430 |
| Embase | 1073 |
| Web of Science | 820 |
| CINAHL | 252 |
| TOTAL | 4001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilson, K.; Stinchcombe, A.; Regalado, S.M. LGBTQ+ Aging Research in Canada: A 30-Year Scoping Review of the Literature. Geriatrics 2021, 6, 60. https://doi.org/10.3390/geriatrics6020060
Wilson K, Stinchcombe A, Regalado SM. LGBTQ+ Aging Research in Canada: A 30-Year Scoping Review of the Literature. Geriatrics. 2021; 6(2):60. https://doi.org/10.3390/geriatrics6020060
Chicago/Turabian StyleWilson, Kimberley, Arne Stinchcombe, and Sophie M. Regalado. 2021. "LGBTQ+ Aging Research in Canada: A 30-Year Scoping Review of the Literature" Geriatrics 6, no. 2: 60. https://doi.org/10.3390/geriatrics6020060
APA StyleWilson, K., Stinchcombe, A., & Regalado, S. M. (2021). LGBTQ+ Aging Research in Canada: A 30-Year Scoping Review of the Literature. Geriatrics, 6(2), 60. https://doi.org/10.3390/geriatrics6020060






