Knee Extension Strength Measures Indicating Probable Sarcopenia Is Associated with Health-Related Outcomes and a Strong Predictor of 1-Year Mortality in Patients Following Hip Fracture Surgery
Abstract
1. Introduction
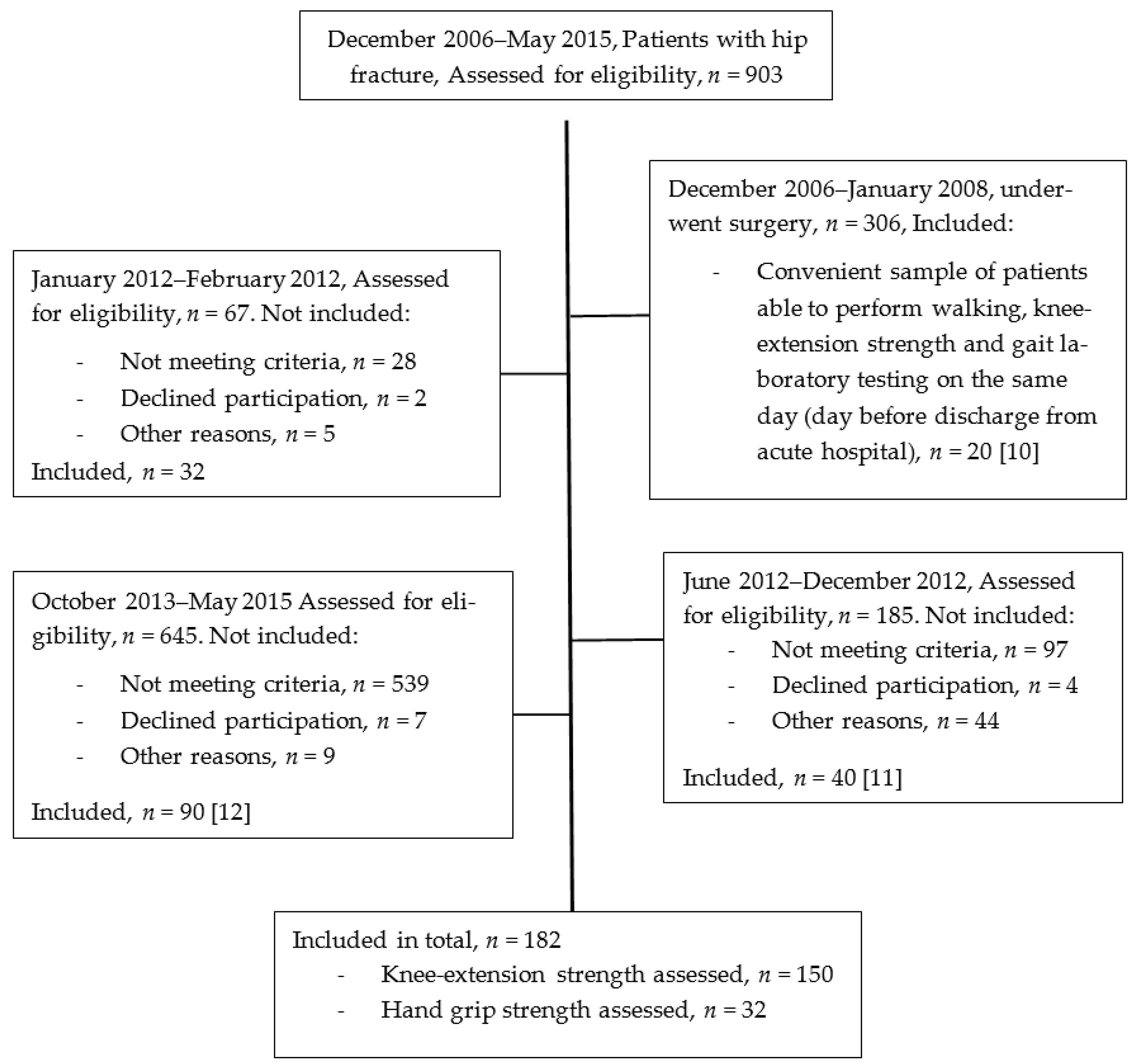
2. Materials and Methods
2.1. Study Design and Setting
2.2. Primary Exposures
2.3. Adjustment Variables
2.4. Physical Performance and Patient-Reported Measures
2.5. Primary and Secondary Outcomes
2.6. Statistical Analysis
3. Results
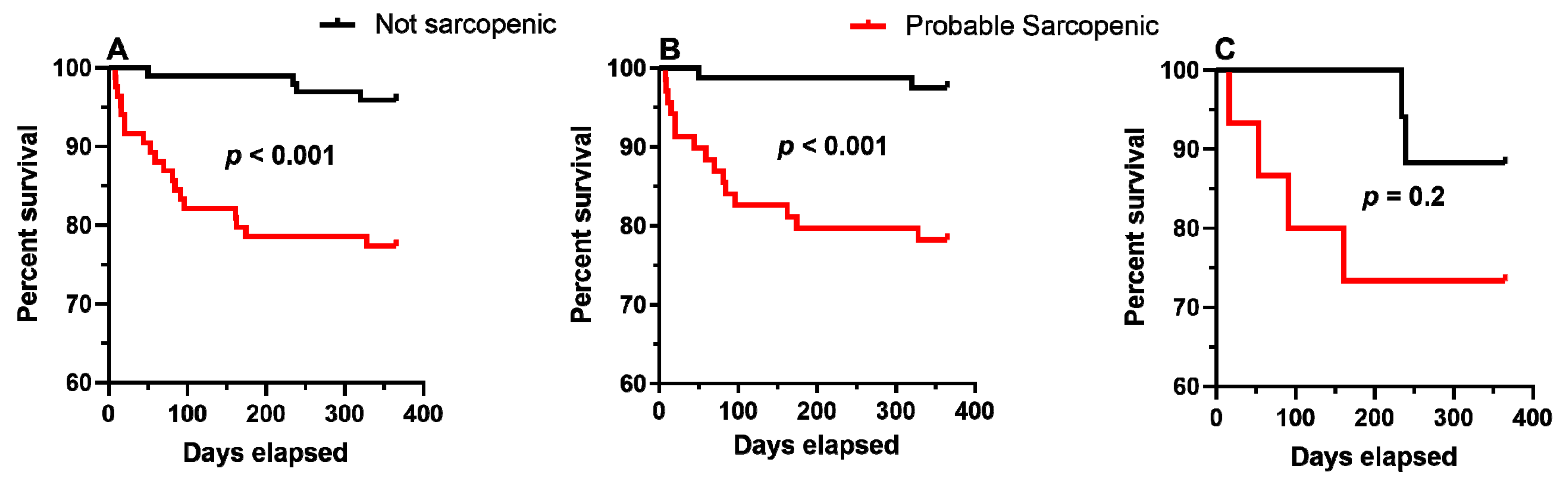
3.1. KES and HGS-Based Probable Sarcopenia Definitions and 1-Year Death
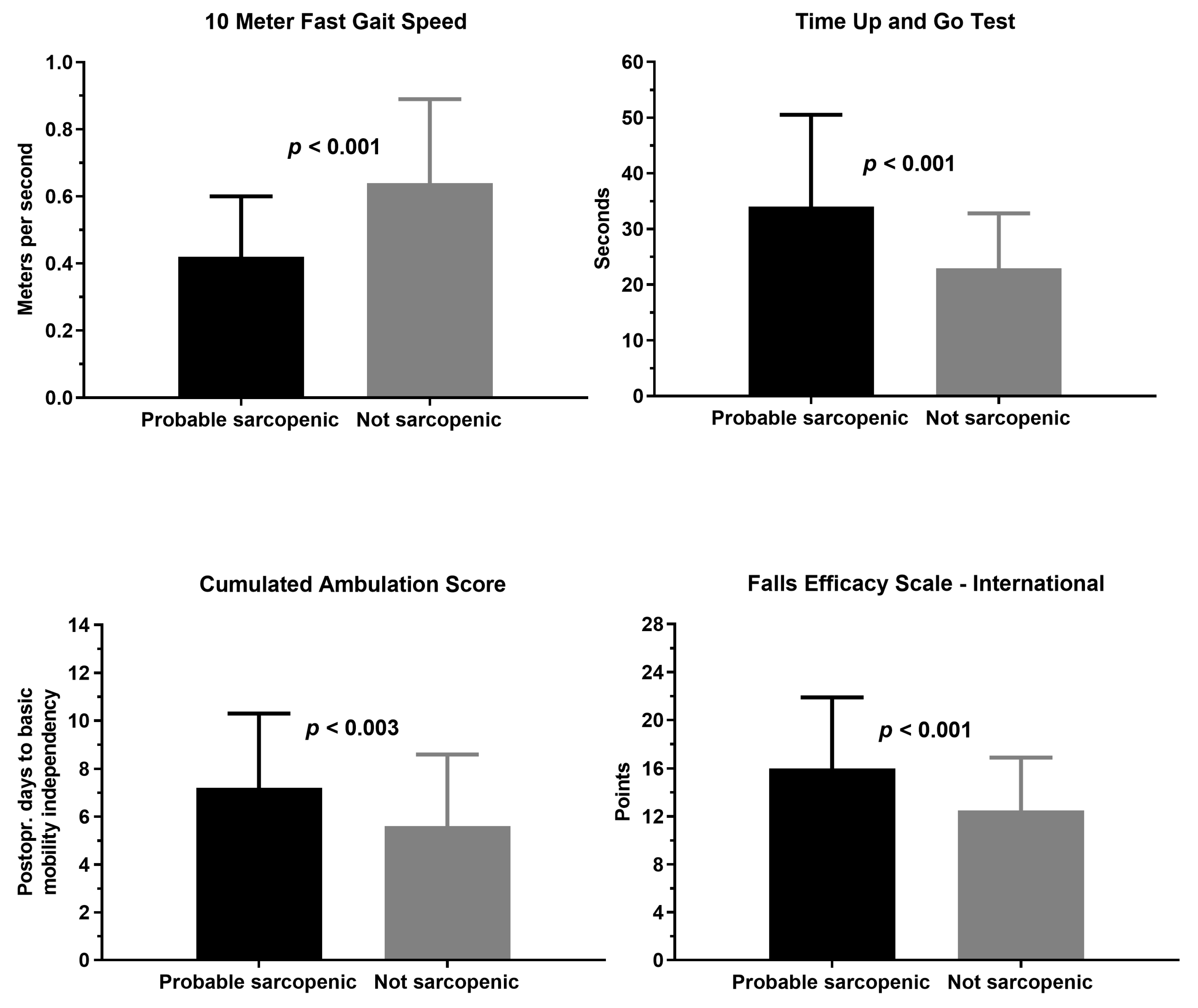
3.2. KES-Based Probable Sarcopenia Definition and Health-Related Outcomes
4. Discussion
4.1. Mortality
4.2. Health-Related Outcomes
4.3. Limitations
4.4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Sobestiansky, S.; Michaelsson, K.; Cederholm, T. Sarcopenia prevalence and associations with mortality and hospitalisation by various sarcopenia definitions in 85–89 year old community-dwelling men: A report from the ULSAM study. BMC Geriatr. 2019, 318. [Google Scholar] [CrossRef] [PubMed]
- Alonso, A.C.; Ribeiro, S.M.; Silva Luna, N.M.; Peterson, M.D.; Bocalini, D.S.; Serra, M.M.; Brech, G.C.; D’Andréa Greve, J.M.; Garcez-Leme, L.E. Association between handgrip strength, balance, and knee flexion/extension strength in older adults. PLoS ONE 2018, 13, e0198185. [Google Scholar] [CrossRef] [PubMed]
- Harris-Love, M.O.; Benson, K.; Leasure, E.; Adams, B.; McIntosh, V. The influence of upper and lower extremity strength on performance-based sarcopenia assessment tests. J. Funct. Morphol. Kinesiol. 2018, 3, 53. [Google Scholar] [CrossRef] [PubMed]
- Yeung, S.S.Y.; Reijnierse, E.M.; Trappenburg, M.C.; Blauw, G.J.; Meskers, C.G.M.; Maier, A.B. Knee extension strength measurements should be considered as part of the comprehensive geriatric assessment. BMC Geriatr. 2018, 18, 130. [Google Scholar] [CrossRef]
- Menant, J.C.; Weber, F.; Lo, J.; Sturnieks, D.L.; Close, J.C.; Sachdev, P.S.; Brodaty, H.; Lord, S.R. Strength measures are better than muscle mass measures in predicting health-related outcomes in older people: Time to abandon the term sarcopenia? Osteoporos. Int. 2017, 28, 59–70. [Google Scholar] [CrossRef]
- Mayhew, A.J.; Raina, P. Sarcopenia: New definitions, same limitations. Age Ageing 2019, 48, 613–614. [Google Scholar] [CrossRef]
- Hulsbæk, S.; Larsen, R.F.; Rosthøj, S.; Kristensen, M.T. The Barthel Index and the Cumulated Ambulation Score are superior to the de Morton Mobility Index for the early assessment of outcome in patients with a hip fracture admitted to an acute geriatric ward. Disabil. Rehabil. 2019, 41, 1351–1359. [Google Scholar] [CrossRef]
- Lim, S.K.; Beom, J.; Lee, S.Y.; Lim, J.Y. Functional Outcomes of Fragility Fracture Integrated Rehabilitation Management in Sarcopenic Patients after Hip Fracture Surgery and Predictors of Independent Ambulation. J. Nutr. Health Aging 2019, 23, 1034–1042. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Bandholm, T.; Bencke, J.; Ekdahl, C.; Kehlet, H. Knee-extension strength, postural control and function are related to fracture type and thigh edema in patients with hip fracture. Clin. Biomech. 2009, 24, 218–224. [Google Scholar] [CrossRef]
- Kronborg, L.; Bandholm, T.; Palm, H.; Kehlet, H.; Kristensen, M.T. Feasibility of progressive strength training implemented in the acute ward after hip fracture surgery. PLoS ONE 2014, 9, e0093332. [Google Scholar] [CrossRef] [PubMed]
- Kronborg, L.; Bandholm, T.; Palm, H.; Kehlet, H.; Kristensen, M.T. Effectiveness of acute in-hospital physiotherapy with knee-extension strength training in reducing strength deficits in patients with a hip fracture: A randomised controlled trial. PLoS ONE 2017, 12, e0179867. [Google Scholar] [CrossRef] [PubMed]
- Foss, N.B.; Kristensen, M.T.; Jensen, P.S.; Palm, H.; Krasheninnikoff, M.; Kehlet, H. The effects of liberal versus restrictive transfusion thresholds on ambulation after hip fracture surgery. Transfusion 2009, 49, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Studenski, S.A.; Peters, K.W.; Alley, D.E.; Cawthon, P.M.; Mclean, R.R.; Harris, T.B.; Ferrucci, L.; Guralnik, J.M.; Fragala, M.S.; Kenny, A.M.; et al. The FNIH Sarcopenia Project: Rationale, Study and Final Estimates. J. Gerontol. Ser. A 2014, 69, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.T.; Bandholm, T.; Foss, N.B.; Ekdahl, C.; Kehlet, H. High inter-tester reliability of the New Mobility Score in patients with hip fracture. J. Rehabil. Med. 2008, 40, 589–591. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Kehlet, H. Most patients regain prefracture basic mobility after hip fracture surgery in a fast-track programme. Dan. Med. J. 2012, 59. [Google Scholar]
- Parker, M.J.; Palmer, C.R. A new mobility score for predicting mortality after hip fracture. J. Bone Joint Surg. Br. 1993, 75, 797–798. [Google Scholar] [CrossRef]
- American Society of Anesthesiologists. New classification of physical status. Anesthesiology 1963, 24, 111. [Google Scholar]
- Mayhew, D.; Mendonca, V.; Murthy, B.V.S. A review of ASA physical status—historical perspectives and modern developments. Anaesthesia 2019, 74, 373–379. [Google Scholar] [CrossRef]
- Sheehan, K.J.; Sobolev, B.; Chudyk, A.; Stephens, T.; Guy, P. Patient and system factors of mortality after hip fracture: A scoping review. BMC Musculeskelet. Disord. 2016, 17. [Google Scholar] [CrossRef]
- Kristensen, M.T. Hip Fracture-Related Pain Strongly Influences Functional Performance of Patients With an Intertrochanteric Fracture Upon Discharge From the Hospital. PM&R 2013, 5, 135–141. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Andersen, L.; Bech-Jensen, R.; Moos, M.; Hovmand, B.; Ekdahl, C.; Kehlet, H. High intertester reliability of the Cumulated Ambulation Score for the evaluation of basic mobility in patients with hip fracture. Clin. Rehabil. 2009, 23, 1116–1123. [Google Scholar] [CrossRef] [PubMed]
- Bloch, M.L.; Jønsson, L.R.; Kristensen, M.T. Introducing a Third Timed Up & Go Test Trial Improves Performances of Hospitalized and Community-Dwelling Older Individuals. J. Geriatr. Phys. Ther. 2017, 40, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.T.; Henriksen, S.; Stie, S.B.; Bandholm, T. Relative and absolute intertester reliability of the timed up and go test to quantify functional mobility in patients with hip fracture. J. Am. Geriatr. Soc. 2011, 59, 565–567. [Google Scholar] [CrossRef]
- Andersen, C.W.; Kristensen, M.T. Performance Stability and Interrater Reliability of Culturally Adapted 10-Meter Walking Test for Danes with Neurological Disorders. J. Stroke Cerebrovasc. Dis. 2019, 28, 2459–2467. [Google Scholar] [CrossRef]
- Kempen, G.I.J.M.; Yardley, L.; Van Haastregt, J.C.M.; Zijlstra, G.A.R.; Beyer, N.; Hauer, K.; Todd, C. The Short FES-I: A shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing 2008, 37, 45–50. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Bandholm, T.; Holm, B.; Ekdahl, C.; Kehlet, H. Timed up & go test score in patients with hip fracture is related to the type of walking aid. Arch. Phys. Med. Rehabil. 2009, 90, 1760–1765. [Google Scholar] [CrossRef]
- Chen, Y.P.; Wong, P.K.; Tsai, M.J.; Chang, W.C.; Hsieh, T.S.; Leu, T.H.; Jeff Lin, C.F.; Lee, C.H.; Kuo, Y.J.; Lin, C.Y. The high prevalence of sarcopenia and its associated outcomes following hip surgery in Taiwanese geriatric patients with a hip fracture. J. Formos. Med. Assoc. 2020. [Google Scholar] [CrossRef]
- Steihaug, O.M.; Gjesdal, C.G.; Bogen, B.; Kristoffersen, M.H.; Lien, G.; Hufthammer, K.O.; Ranhoff, A.H. Does sarcopenia predict change in mobility after hip fracture? A multicenter observational study with one-year follow-up. BMC Geriatr. 2018, 18, 65. [Google Scholar] [CrossRef]
- Kristensen, M.T.M.T.; Kehlet, H. The basic mobility status upon acute hospital discharge is an independent risk factor for mortality up to 5 years after hip fracture surgery: Survival rates of 444 pre-fracture ambulatory patients evaluated with the Cumulated Ambulation Score. Acta Orthop. 2018, 89, 47–52. [Google Scholar] [CrossRef]
- Smith, T.; Pelpola, K.; Ball, M.; Ong, A.; Myint, P.K. Pre-operative indicators for mortality following hip fracture surgery: A systematic review and meta-analysis. Age Ageing 2014, 43, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Foss, N.B.; Kristensen, M.T.; Kehlet, H. Prediction of postoperative morbidity, mortality and rehabilitation in hip fracture patients: The cumulated ambulation score. Clin. Rehabil. 2006, 20, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.T.; Öztürk, B.; Röck, N.D.; Ingeman, A.; Palm, H.; Pedersen, A.B. Regaining pre-fracture basic mobility status after hip fracture and association with post-discharge mortality and readmission—A nationwide register study in Denmark. Age Ageing 2019, 48, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Ferris, H.; Brent, L.; Coughlan, T. Early mobilisation reduces the risk of in-hospital mortality following hip fracture. Eur. Geriatr. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, L.; Maietti, E.; Abete, P.; Bellelli, G.; Bo, M.; Cherubini, A.; Corica, F.; Di Bari, M.; Maggio, M.; Martone, A.M.; et al. Comparing EWGSOP2 and FNIH Sarcopenia Definitions: Agreement and Three-Year Survival Prognostic Value in Older Hospitalized Adults. The GLISTEN Study. J. Gerontol. Ser. A 2019. [Google Scholar] [CrossRef] [PubMed]
- Newman, A.B.; Kupelian, V.; Visser, M.; Simonsick, E.M.; Goodpaster, B.H.; Kritchevsky, S.B.; Tylavsky, F.A.; Rubin, S.M.; Harris, T.B. Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2006, 61, 72–77. [Google Scholar] [CrossRef]
- Volaklis, K.A.; Halle, M.; Meisinger, C. Muscular strength as a strong predictor of mortality: A narrative review. Eur. J. Intern. Med. 2015, 26, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Mangione, K.K.; Craik, R.L.; Tomlinson, S.S.; Palombaro, K.M. Can elderly patients who have had a hip fracture perform moderate- to high-intensity exercise at home? Phys. Ther. 2005, 85, 727–739. [Google Scholar] [CrossRef]
- Mangione, K.K.; Craik, R.L.; Palombaro, K.M.; Tomlinson, S.S.; Hofmann, M.T. Home-based leg-strengthening exercise improves function 1 year after hip fracture: A randomized controlled study. J. Am. Geriatr. Soc. 2010, 58, 1911–1917. [Google Scholar] [CrossRef]
- Binder, E.F.; Brown, M.; Sinacore, D.R.; Steger-May, K.; Yarasheski, K.E.; Schechtman, K.B. Effects of Extended Outpatient Rehabilitation After Hip Fracture. JAMA 2004, 292, 837. [Google Scholar] [CrossRef]
- Diong, J.; Allen, N.; Sherrington, C. Structured exercise improves mobility after hip fracture: A meta-analysis with meta-regression. Br. J. Sports Med. 2016, 50, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, C.; Fairhall, N.; Wallbank, G.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S. Exercise for preventing falls in older people living in the community: An abridged Cochrane systematic Review. Br. J. Sports Med. 2019, 885–891. [Google Scholar] [CrossRef] [PubMed]
- Palombaro, K.M.; Craik, R.L.; Mangione, K.K.; Tomlinson, J.D. Determining Meaningful Changes in Gait Speed After Hip Fracture. Phys. Ther. 2006, 86, 809–816. [Google Scholar] [CrossRef] [PubMed]
- Tu, C.Y.; Shields, N.; Gill, S.D.; Tacey, M.; Lindner, C.; Hill, K.D. Longitudinal changes in physical activity levels and fear of falling after hip fracture. Physiother. Res. Int. 2020. [Google Scholar] [CrossRef] [PubMed]
- Bullo, V.; Roma, E.; Gobbo, S.; Duregon, F.; Bergamo, M.; Bianchini, G.; Doria, E.; Cugusi, L.; Di Blasio, A.; Bocalini, D.S.; et al. Lower limb strength profile in elderly with different pathologies: Comparisons with healthy subjects. Geriatrics 2020, 5, 83. [Google Scholar] [CrossRef]
- Manini, T.M.; Visser, M.; Won-Park, S.; Patel, K.V.; Strotmeyer, E.S.; Chen, H.; Goodpaster, B.; De Rekeneire, N.; Newman, A.B.; Simonsick, E.M.; et al. Knee extension strength cutpoints for maintaining mobility. J. Am. Geriatr. Soc. 2007, 55, 451–457. [Google Scholar] [CrossRef]
- Menéndez-Colino, R.; Alarcon, T.; Gotor, P.; Queipo, R.; Ramírez-Martín, R.; Otero, A.; González-Montalvo, J.I. Baseline and pre-operative 1-year mortality risk factors in a cohort of 509 hip fracture patients consecutively admitted to a co-managed orthogeriatric unit (FONDA Cohort). Injury 2018, 49, 656–661. [Google Scholar] [CrossRef]
- Glinkowski, W.; Narloch, J.; Krasuski, K.; Śliwczyński, A. The Increase of Osteoporotic Hip Fractures and Associated One-Year Mortality in Poland: 2008–2015. J. Clin. Med. 2019, 8, 1487. [Google Scholar] [CrossRef]
| Knee-Extension Strength, n = 150 Probable Sarcopenic (Menant et al.) [6] | Hand Grip Strength, n = 32 Probable Sarcopenic (EWGSOP2) [1] | ||||||
|---|---|---|---|---|---|---|---|
| Variables | Total, n = 182 | No, n = 81 (54) | Yes, n = 69 (46) | p | No, n = 17(53) | Yes, n = 15 (47) | p |
| Women | 136 (74.7) | 59 (52) | 55 (48) | 0.3 | 17 (54) | 15 (46) | 0.8 |
| Men | 46 (25.3) | 22 (61) | 14 (39) | 5 (50) | 5 (50) | ||
| Age, years, mean (SD) * | 78.7 (7.8) | 76.6 (7.2) | 82.4 (7.0) | <0.001 | 75.2 (7.8) | 77.1 (9.3) | 0.6 |
| Weight, kg, mean (SD) | 64.1 (13.3) | 66.7 (12.8) | 61.1 (13.9) | 0.01 | 65.8 (13.1) | 61.4 (11.5) | 0.3 |
| Height, cm, mean (SD) | 166.5 (9.0) | 167.7 (8.7) | 164.0 (8.4) | 0.009 | 169.2 (10.7) | 168.1 (9.7) | 0.8 |
| BMI, mean (SD) | 23.0 (4.0) | 23.6 (3.9) | 22.6 (4.3) | 0.1 | 22.8 (3.1) | 21.7 (3.6) | 0.4 |
| Cervical femoral neck fractures | 88 (48.4) | 36 (53) | 32 (47) | 0.8 | 11 (55) | 9 (45) | 0.8 |
| Per- and Subtrochanteric fractures | 94 (51.6) | 45 (55) | 37 (45) | 6 (50) | 6 (50) | ||
| Low pre-fracture function, NMS 2–6 * | 51 (28.0) | 9 (24) | 28 (76) | <0.001 | 4 (29) | 10 (71) | 0.03 |
| High Pre-fracture function, NMS 7–9 * | 131 (72.0) | 72 (64) | 41 (36) | 13 (72) | 5 (28) | ||
| Low cognitive status | 9 (4.9) | 1 (17) | 5 (83) | 0.1 | 0 (0) | 3 (100) | 0.09 |
| High cognitive status | 173 (95.1) | 80 (56) | 64 (44) | 17 (59) | 12 (41) | ||
| Low health status, ASA grade 3–4 | 38 (20.9) | 11 (33.3) | 22 (66.7) | 0.007 | 1 (20) | 4 (80) | 0.2 |
| High health status, ASA grade 1–2 | 144 (79.1) | 70 (59.8) | 47 (40.2) | 16 (59) | 11 (41) | ||
| At-home fallers | n/a | 33 (43) | 43 (57) | 0.008 | n/a | ||
| Outdoor fallers | 48 (65) | 23 (35) | |||||
| Days to surgery from admission, median (25–75% IQR) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 0.4 | 1 (1–1) | 1 (0–1) | 0.8 |
| 1-year mortality | 23 (12.6) | 2/81 (2.5) | 15/69 (21.7) | <0.001 | 2/17 (11.8) | 4/15 (26.7) | 0.4 |
| Variables | Univariable Analyses | Multivariable Analyses | ||||||
|---|---|---|---|---|---|---|---|---|
| 95.0% CI for Exp(B) | 95.0% CI for Exp(B) | |||||||
| Exp(B) | Lower | Upper | p | Exp(B) | Lower | Upper | p | |
| Age, per year older | 1.078 | 1.01 | 1.15 | 0.03 | 1.04 | 0.97 | 1.12 | 0.3 |
| Women (reference) | ||||||||
| Men | 2.4 | 0.89 | 6.2 | 0.08 | 3.1 | 1.2 | 8.4 | 0.03 |
| BMI, per point higher | 0.98 | 0.87 | 1.1 | 0.8 | 0.98 | 0.87 | 1.1 | 0.8 |
| High prefracture level, NMS, 7–9 (reference) | ||||||||
| Low prefracture level NMS, 2–6 | 3.7 | 1.4 | 9.6 | 0.007 | 1.5 | 0.54 | 4.19 | 0.4 |
| High health status ASA, 1–2 (reference) | ||||||||
| Low health status ASA, 3–4 | 5.8 | 2.2 | 15.3 | <0.001 | 3.7 | 1.3 | 10.3 | 0.01 |
| Cervical femoral fracture (reference) | ||||||||
| Trochanteric fracture | 2.1 | 0.72 | 5.83 | 0.2 | 1.8 | 0.61 | 5.3 | 0.3 |
| Not sarcopenic * (reference) | ||||||||
| Probable sarcopenic * | 9.8 | 2.2 | 43.0 | 0.002 | 7.2 | 1.6 | 33.4 | 0.01 |
| Variables | Total, n = 150 | Probable Sarcopenia | Difference Mean (95%CI) | p | |
|---|---|---|---|---|---|
| No, n = 81 | Yes, n = 69 | ||||
| POD of independent mobility, CAS = 6, mean (SD) | 6.2 (3.1) | 5.6 (3.0) | 7.2 (3.1) | 1.7 (0.6; 2.8) | 0.003 |
| Not independent in basic mobility, CAS < 6, n (%) | 22 (14.7) | 3 (13.6) | 19 (86.4) | n/a | <0.001 |
| Independent in basic mobility, CAS = 6, n (%) | 128 (85.3) | 78 (60.9) | 50 (39.1) | ||
| Timed Up and Go test, seconds, n = 122, mean (SD) | 27.2 (13.9) | 22.9 (9.9) | 34.0 (16.5) | 11.1 (6.4; 15.9) | <0.001 |
| Timed Up and Go test ≥ 20 s *, n (%) | 105 (70) | 45 (43) | 60 (57) | n/a | <0.001 |
| Timed Up and Go test < 20 s, n (%) | 45 (30) | 36 (80) | 9 (20) | ||
| Fast Gait speed, seconds, n = 121, mean (SD) | 23.5 (17.1) | 19.3 (13.4) | 29.9 (29.9) | 10.6 (4.6; 16.6) | 0.002 |
| Fast Gait speed, m/s, n = 121, mean (SD) | 0.55 (0.24) | 0.64 (0.25) | 0.42 (0.18) | −0.21 (−0.29; −0.13) | <0.001 |
| Gait speed ≤ 0.8 s *, n (%) | 132 (88) | 64 (48) | 68 (52) | n/a | <0.001 |
| Fast Gait speed > 0.8 s, n (%) | 18 (12) | 17 (94) | 1 (6) | ||
| Short Falls Efficacy Scale–I, n = 131, mean (SD) | 14.0 (5.4) | 12.5 (4.4) | 16.0 (5.9) | 3.5 (1.7; 5.3) | <0.001 |
| Fractured knee-extension strength, Nm/kg, mean (SD) | 0.57 (0.32) | 0.70 (0.35) | 0.43 (0.20) | −0.27 (−0.36; −0.17) | <0.001 |
| Non-fractured Knee-extension strength, Nm/kg, mean (SD) | 1.04 (0.41) | 1.31 (0.32) | 0.72 (0.24) | −0.60 (−0.69; −0.50) | <0.001 |
| Non-fractured knee-extension strength, kg, mean (SD) | 19.2 (8.5) | 25.0 (6.9) | 12.4 (4.0) | −12.6 (−14.5; −10.8) | <0.001 |
| POD of strength testing, mean (SD) | 8.2 (2.8) | 7.8 (2.6) | 8.7 (2.9) | 0.94 (0.1; 1.8) | 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kristensen, M.T.; Hulsbæk, S.; Faber, L.L.; Kronborg, L. Knee Extension Strength Measures Indicating Probable Sarcopenia Is Associated with Health-Related Outcomes and a Strong Predictor of 1-Year Mortality in Patients Following Hip Fracture Surgery. Geriatrics 2021, 6, 8. https://doi.org/10.3390/geriatrics6010008
Kristensen MT, Hulsbæk S, Faber LL, Kronborg L. Knee Extension Strength Measures Indicating Probable Sarcopenia Is Associated with Health-Related Outcomes and a Strong Predictor of 1-Year Mortality in Patients Following Hip Fracture Surgery. Geriatrics. 2021; 6(1):8. https://doi.org/10.3390/geriatrics6010008
Chicago/Turabian StyleKristensen, Morten Tange, Signe Hulsbæk, Louise Lohmann Faber, and Lise Kronborg. 2021. "Knee Extension Strength Measures Indicating Probable Sarcopenia Is Associated with Health-Related Outcomes and a Strong Predictor of 1-Year Mortality in Patients Following Hip Fracture Surgery" Geriatrics 6, no. 1: 8. https://doi.org/10.3390/geriatrics6010008
APA StyleKristensen, M. T., Hulsbæk, S., Faber, L. L., & Kronborg, L. (2021). Knee Extension Strength Measures Indicating Probable Sarcopenia Is Associated with Health-Related Outcomes and a Strong Predictor of 1-Year Mortality in Patients Following Hip Fracture Surgery. Geriatrics, 6(1), 8. https://doi.org/10.3390/geriatrics6010008





