A Novel Exercise for Enhancing Visuospatial Ability in Older Adults with Frailty: Development, Feasibility, and Effectiveness
Abstract
1. Introduction
2. Materials and Methods
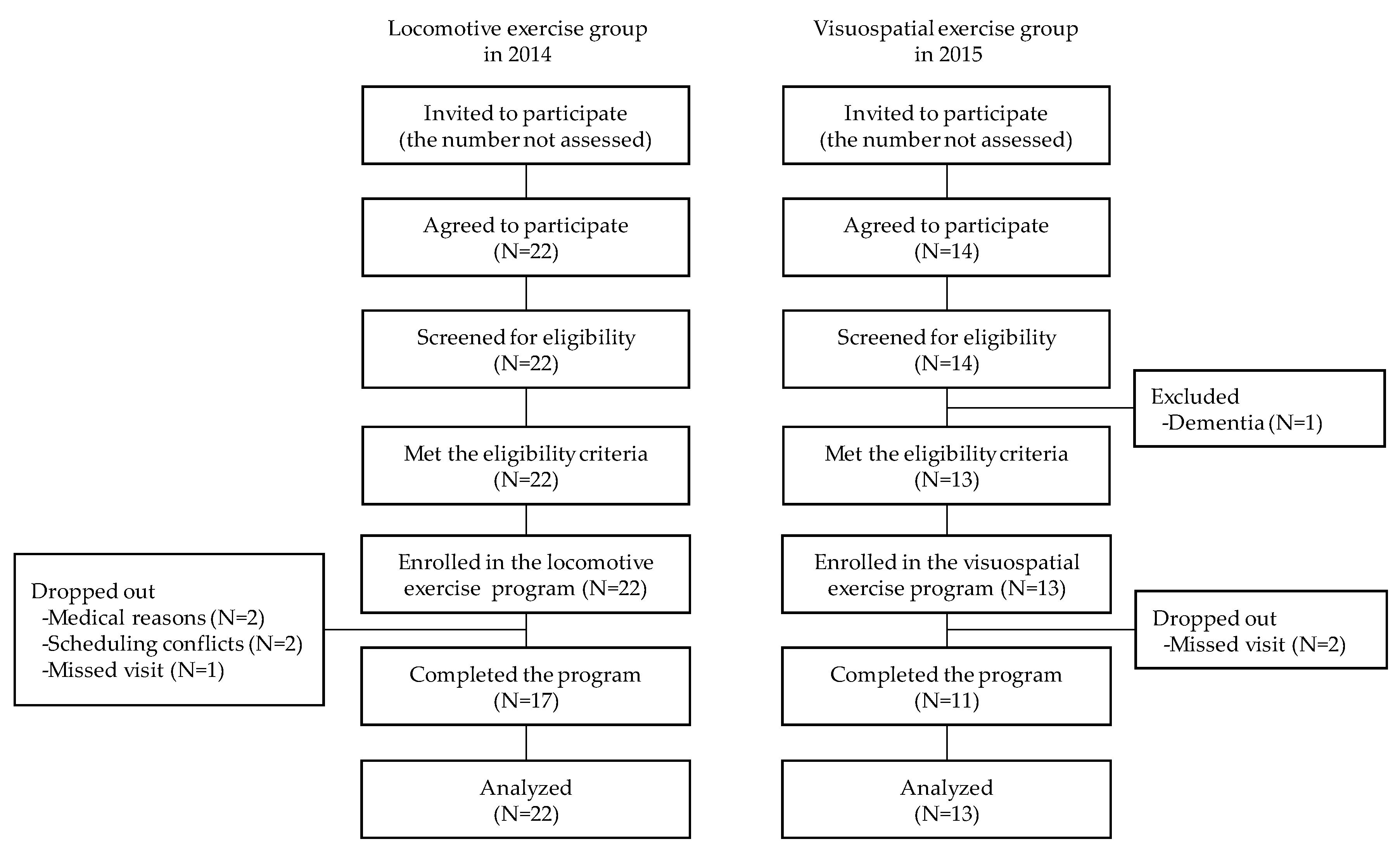
2.1. Design and Setting
2.2. Participants
2.3. Program Development
2.4. Interventions
2.4.1. Locomotive Exercise
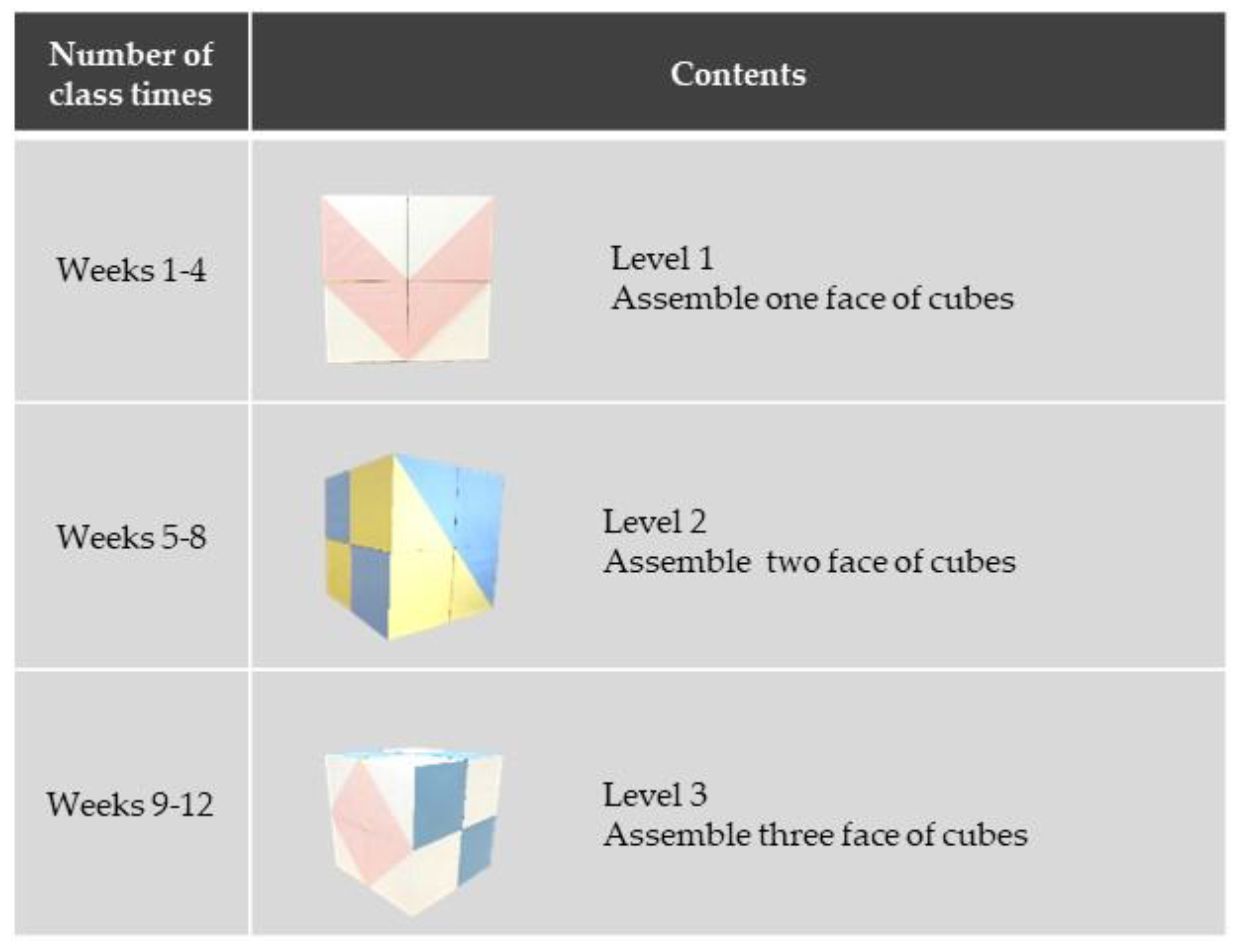
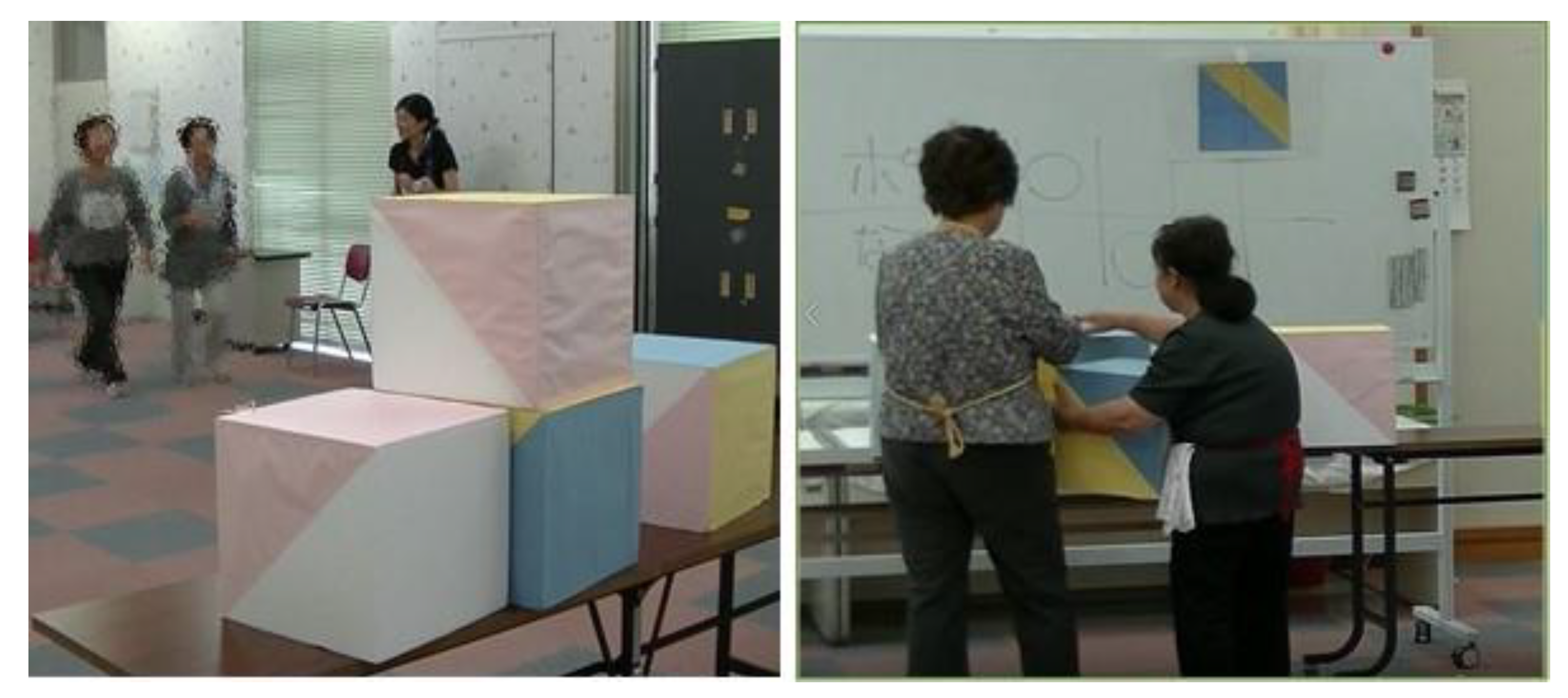
2.4.2. Visuospatial Exercise
2.5. Feasibility Assessment
2.6. Preliminary Effectiveness Assessment
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Walston, J.; Buta, B.; Xue, Q.L. Frailty Screening and Interventions: Considerations for Clinical Practice. Clin. Geriatr. Med. 2018, 34, 25–38. [Google Scholar] [CrossRef] [PubMed]
- de Labra, C.; Guimaraes-Pinheiro, C.; Maseda, A.; Lorenzo, T.; Millan-Calenti, J.C. Effects of Physical Exercise Interventions in Frail Older Adults: A Systematic Review of Randomized Controlled Trials. BMC Geriatr. 2015, 15, 154. [Google Scholar] [CrossRef] [PubMed]
- Kojima, G.; Taniguchi, Y.; Iliffe, S.; Walters, K. Frailty as a Predictor of Alzheimer Disease, Vascular Dementia, and All Dementia among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2016, 17, 881–888. [Google Scholar] [CrossRef]
- Öhman, H.; Savikko, N.; Strandberg, T.E.; Pitkälä, K.H. Effect of Physical Exercise on Cognitive Performance in Older Adults with Mild Cognitive Impairment or Dementia: A Systematic Review. Dement. Geriatr. Cogn. Disord. 2014, 38, 347–365. [Google Scholar] [CrossRef] [PubMed]
- Karssemeijer, E.G.A.; Aaronson, J.A.; Bossers, W.J.; Smits, T.; Olde Rikkert, M.G.M.; Kessels, R.P.C. Positive Effects of Combined Cognitive and Physical Exercise Training on Cognitive Function in Older Adults with Mild Cognitive Impairment or Dementia: A Meta-Analysis. Ageing Res. Rev. 2017, 40, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Quental, N.B.; Brucki, S.M.; Bueno, O.F. Visuospatial Function in Early Alzheimer’s Disease--the Use of The Visual Object and Space Perception (VOSP) Battery. PLoS ONE 2013, 8, e68398. [Google Scholar] [CrossRef] [PubMed]
- Geldmacher, D.S. Visuospatial Dysfunction in the Neurodegenerative Diseases. Front. Biosci. 2003, 8, e428–e436. [Google Scholar] [CrossRef][Green Version]
- Naslund, J. Visuospatial Ability in Relation to Fall Risk and Dementia. Arch. Neurol. 2010, 67, 643. [Google Scholar] [CrossRef]
- Hill, N.T.; Mowszowski, L.; Naismith, S.L.; Chadwick, V.L.; Valenzuela, M.; Lampit, A. Computerized Cognitive Training in Older Adults with Mild Cognitive Impairment or Dementia: A Systematic Review and Meta-Analysis. Am. J. Psychiatry 2017, 174, 329–340. [Google Scholar] [CrossRef]
- Des Jarlais, D.C.; Lyles, C.; Crepaz, N.; TREND Group. Improving the Reporting Quality of Nonrandomized Evaluations of Behavioral and Public Health Interventions: The TREND statement. Am. J. Public Health 2004, 94, 361–366. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare, Japan. Long-term Care Insurance in Japan. Available online: https://www.mhlw.go.jp/english/topics/elderly/care/index.html (accessed on 10 February 2020).
- Satake, S.; Senda, K.; Hong, Y.J.; Miura, H.; Endo, H.; Sakurai, T.; Kondo, I.; Toba, K. Validity of the Kihon Checklist for Assessing Frailty Status. Geriatr. Gerontol. Int. 2016, 16, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Sewo Sampaio, P.Y.; Sampaio, R.A.; Yamada, M.; Arai, H. Systematic Review of the Kihon Checklist: Is it a Reliable Assessment of Frailty? Geriatr. Gerontol. Int. 2016, 16, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Sewo Sampaio, P.Y.; Sampaio, R.A.; Yamada, M.; Ogita, M.; Arai, H. Validation and Translation of the Kihon Checklist (Frailty Index) into Brazilian Portuguese. Geriatr. Gerontol. Int. 2014, 14, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare, Japan. The Manual of Exercise Intervention for Older Adults with Frailty. Available online: https://www.mhlw.go.jp/topics/2009/05/dl/tp0501-1d.pdf (accessed on 10 February 2020).
- Lezak, M.D.; Howieson, D.B.; Bigler, E.D.; Tranel, D. Neuropsychological Assessment, 5th ed.; Oxford University Press: New York, NY, USA, 2012; ISBN 978-01-9539-552-5. [Google Scholar]
- Borg, G. Perceived Exertion as an Indicator of Somatic Stress. Scand. J. Rehabil. Med. 1970, 2, 92–98. [Google Scholar] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of Older People: Self-maintaining and Instrumental Activities of Daily Living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state” A Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Leyhe, T.; Milian, M.; Muller, S.; Eschweiler, G.W.; Saur, R. The Minute Hand Phenomenon in the Clock Test of Patients with Early Alzheimer Disease. J. Geriatr. Psychiatry Neurol. 2009, 22, 119–129. [Google Scholar] [CrossRef]
- Agrell, B.; Dehlin, O. The Clock-Drawing Test 1998. Age Ageing 2012, 41, iii41–iii45. [Google Scholar] [CrossRef]
- Freedman, M.; Leach, L.; Kaplan, E.; Winocur, G.; Shulman, K.; Delis, D.C. Clock Drawing: A Neuropsychological Analysis; Oxford University Press: New York, NY, USA, 1994; ISBN 978-01-9505-906-9. [Google Scholar]
- Rouleau, I.; Salmon, D.P.; Butters, N. Longitudinal Analysis of Clock Drawing in Alzheimer’s Disease Patients. Brain Cogn. 1996, 31, 17–34. [Google Scholar] [CrossRef][Green Version]
- Kaplan, E. The Process Approach to Neuropsychological Assessment of Psychiatric Patients. J. Neuropsychiatry Clin. Neurosci. 1990, 2, 72–87. [Google Scholar] [CrossRef]
- Rouleau, I.; Salmon, D.P.; Butters, N.; Kennedy, C.; McGuire, K. Quantitative and Qualitative Analyses of Clock Drawings in Alzheimer’s and Huntington’s Disease. Brain Cogn. 1992, 18, 70–87. [Google Scholar] [CrossRef]
- Shinkai, S.; Kumagai, S.; Fujiwara, Y.; Amano, H.; Yoshida, Y.; Watanabe, S.; Ishizaki, T.; Suzuki, T.; Shibata, H. Predictors for the Onset of Functional Decline among Initially Non-disabled Older People Living in a Community during a 6-year Follow-up. Geriatr. Gerontol. Int. 2003, 3, S31–S39. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Ferrucci, L.; Simonsick, E.M.; Salive, M.E.; Wallace, R.B. Lower-extremity Function in Persons over the Age of 70 Years as a Predictor of Subsequent Disability. N. Engl. J. Med. 1995, 332, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Rikli, R.; Busch, S. Motor Performance of Women as a Function of Age and Physical Activity Level. J. Gerontol. 1986, 41, 645–649. [Google Scholar] [CrossRef] [PubMed]
- Hoeger, W.W.K.; Hoeger, S.A. Lifetime Physical Fitness and Wellness: A Personalized Program, 12th ed.; Wadsworth Cengage Learning: Belmont, CA, USA, 2003; ISBN 13-978-1111990015. [Google Scholar]
- Podsiadlo, D.; Richardson, S. The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Shinkai, S.; Watanabe, S.; Kumagai, S.; Fujiwara, Y.; Amano, H.; Yoshida, H.; Ishizaki, T.; Yukawa, H.; Suzuki, T.; Shibata, H. Walking Speed as a Good Predictor for the Onset of Functional Dependence in a Japanese Rural Community Population. Age Ageing 2000, 29, 441–446. [Google Scholar] [CrossRef]
- Shigematsu, R.; Kim, H.; Chang, M.; Ueno, L.M.; Tanaka, K. A Physical Performance Battery Assessing Low/High Extremity Functional Fitness in Older Japanese Women. Nippon Koshu Eisei Zasshi 1999, 46, 14–24. (In Japanese) [Google Scholar]
- Verhaeghen, P.; Salthouse, T.A. Meta-Analyses of Age-Cognition Relations in Adulthood: Estimates of Linear and Nonlinear Age Effects and Structural Models. Psychol. Bull. 1997, 122, 231–249. [Google Scholar] [CrossRef]
- Mielke, M.M. Sex and Gender Differences in Alzheimer’s Disease Dementia. Psychiatr. Times 2018, 35, 14–17. [Google Scholar]
- Beydoun, M.A.; Beydoun, H.A.; Gamaldo, A.A.; Teel, A.; Zonderman, A.B.; Wang, Y. Epidemiologic Studies of Modifiable Factors Associated with Cognition and Sementia: Systematic Review and Meta-Analysis. BMC Public Health 2014, 14, 643. [Google Scholar] [CrossRef]
- Serra-Prat, M.; Sist, X.; Domenich, R.; Jurado, L.; Saiz, A.; Roces, A.; Palomera, E.; Tarradelles, M.; Papiol, M. Effectiveness of an Intervention to Prevent Frailty in Pre-frail Community-Dwelling Older People Consulting in Primary Care: A Randomised Controlled Trial. Age Ageing 2017, 46, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Konagaya, Y.; Konagaya, M.; Watanabe, T.; Washimi, Y. Quantitative and Qualitative Analyses for Characteristics of the Clock Drawing in Alzheimer’s Disease. Clin. Neurol. 2014, 54, 109–115. [Google Scholar] [CrossRef]
- Belleville, S.; Gilbert, B.; Fontaine, F.; Gagnon, L.; Menard, E.; Gauthier, S. Improvement of Episodic Memory in Persons with Mild Cognitive Impairment and Healthy Older Adults: Evidence from a Cognitive Intervention Program. Dement. Geriatr. Cogn. Disord. 2006, 22, 486–499. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Shimada, H.; Makizako, H.; Doi, T.; Yoshida, D.; Ito, K.; Shimokata, H.; Washimi, Y.; Endo, H.; Kato, T. A Randomized Controlled Trial of Multicomponent Exercise in Older Adults with Mild Cognitive Impairment. PLoS ONE 2013, 8, e61483. [Google Scholar] [CrossRef]
- Lipardo, D.S.; Aseron, A.M.C.; Kwan, M.M.; Tsang, W.W. Effect of Exercise and Cognitive Training on Falls and Fall-Related Factors in Older Adults with Mild Cognitive Impairment: A Systematic Review. Arch. Phys. Med. Rehabil. 2017, 98, 2079–2096. [Google Scholar] [CrossRef]

| Locomotive Exercise (N = 22) | Visuospatial Exercise (N = 13) | p-Values | Cohen’s d | |
|---|---|---|---|---|
| Demographics and anthropometrics | ||||
| Sex (women), n (%) | 17 (77.3) | 7 (53.8) | 0.26 | 0.24 |
| Age, years | 81.3 (5.9) | 78.1 (9.1) | 0.21 | 0.44 |
| Height, cm | 146.2 (9.3) | 150.9 (9.9) | 0.16 | 0.49 |
| Weight, kg | 48.5 (8.2) | 57.6 (14.5) | 0.02 | 0.83 |
| Body mass index, kg/m2 | 22.7 (3.1) | 25.1 (4.5) | 0.07 | 0.65 |
| Instrumental ADL scale, pts | 6.9 (1.7) | 7.3 (0.9) | 0.45 | 0.27 |
| Medical history | ||||
| Cerebrovascular disease, n (%) | 3 (14.3) | 2 (15.4) | 1.00 | 0.02 |
| Hypertension, n (%) | 10 (45.5) | 11 (84.6) | 0.34 | 0.39 |
| Diabetes mellitus, n (%) | 4 (19.0) | 2 (15.4) | 1.00 | 0.05 |
| Osteoporosis, n (%) | 2 (9.5) | 2 (15.4) | 0.63 | 0.09 |
| Low-back pain, n (%) | 1 (4.8) | 5 (38.5) | 0.02 | 0.43 |
| Knee pain, n (%) | 0 (0.0) | 3 (23.1) | 0.05 | 0.40 |
| Cognitive functions | ||||
| Mini-Mental State Examination, pts | 25.3 (3.4) | 25.3 (2.7) | 0.97 | 0.00 |
| Clock Drawing Test, pts | 11.8 (3.1) | 11.9 (2.3) | 0.91 | 0.04 |
| Physical functions | ||||
| Grip strength, kg | 19.5 (5.0) | 18.9 (6.3) | 0.76 | 0.11 |
| One-leg stance, s | 11.5 (10.9) | 8.3 (7.4) | 0.38 | 0.33 |
| Sit and reach, cm | 29.8 (9.2) | 26.7 (9.9) | 0.38 | 0.33 |
| Five chair sit-to-stands, s | 10.8 (4.4) | 11.4 (5.1) | 0.74 | 0.13 |
| Timed up and go, s | 9.5 (2.2) | 13.4 (8.8) | 0.54 | 0.70 |
| Usual gait speed, s | 4.4 (1.4) | 7.9 (3.8) | <0.01 | 1.37 |
| Hand working with peg board, n | 30.9 (7.7) | 31.7 (9.4) | 0.79 | 0.10 |
| Outcomes | Locomotive Exercise (N = 22) | Visuospatial Exercise (N = 13) | p-Values | Cohen’s d | ||
|---|---|---|---|---|---|---|
| Cognitive functions * | ||||||
| Mini-Mental State Examination, pts | 0.2 | (−0.5, 1.0) | 1.6 | (0.6, 2.6) | 0.04 | 0.79 |
| Clock Drawing Test, pts | 0.2 | (−0.6, 1.1) | 1.4 | (0.3, 2.5) | 0.09 | 0.70 |
| Physical functions ** | ||||||
| Grip strength, kg | −0.1 | (−1.1, 0.9) | 2.0 | (0.7, 3.3) | 0.02 | 1.07 |
| One-leg stance, s | 2.2 | (−3.0, 7.3) | 2.2 | (−4.6, 9.0) | 0.99 | 0.02 |
| Sit and reach, cm | −3.0 | (−4.7, −1.2) | 0.4 | (−2.2, 3.0) | 0.047 | 0.77 |
| Five chair sit-to-stands, s | −0.7 | (−2.1, 0.7) | −1.2 | (−3.1, 0.8) | 0.71 | 0.27 |
| Timed up and go, s | 0.5 | (−0.9, 1.8) | −1.6 | (−3.4, 0.4) | 0.10 | 0.70 |
| Usual gait speed, s | 1.0 | (−0.2, 2.2) | 0.1 | (−1.6, 1.7) | 0.39 | 0.71 |
| Hand working with peg board, n | 1.4 | (−0.1, 2.8) | 1.2 | (−0.7, 3.1) | 0.90 | 0.08 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nemoto, M.; Sasai, H.; Yabushita, N.; Tsuchiya, K.; Hotta, K.; Fujita, Y.; Kim, T.; Tsujimoto, T.; Arai, T.; Tanaka, K. A Novel Exercise for Enhancing Visuospatial Ability in Older Adults with Frailty: Development, Feasibility, and Effectiveness. Geriatrics 2020, 5, 29. https://doi.org/10.3390/geriatrics5020029
Nemoto M, Sasai H, Yabushita N, Tsuchiya K, Hotta K, Fujita Y, Kim T, Tsujimoto T, Arai T, Tanaka K. A Novel Exercise for Enhancing Visuospatial Ability in Older Adults with Frailty: Development, Feasibility, and Effectiveness. Geriatrics. 2020; 5(2):29. https://doi.org/10.3390/geriatrics5020029
Chicago/Turabian StyleNemoto, Miyuki, Hiroyuki Sasai, Noriko Yabushita, Keito Tsuchiya, Kazushi Hotta, Yoshihiko Fujita, Taeho Kim, Takehiko Tsujimoto, Tetsuaki Arai, and Kiyoji Tanaka. 2020. "A Novel Exercise for Enhancing Visuospatial Ability in Older Adults with Frailty: Development, Feasibility, and Effectiveness" Geriatrics 5, no. 2: 29. https://doi.org/10.3390/geriatrics5020029
APA StyleNemoto, M., Sasai, H., Yabushita, N., Tsuchiya, K., Hotta, K., Fujita, Y., Kim, T., Tsujimoto, T., Arai, T., & Tanaka, K. (2020). A Novel Exercise for Enhancing Visuospatial Ability in Older Adults with Frailty: Development, Feasibility, and Effectiveness. Geriatrics, 5(2), 29. https://doi.org/10.3390/geriatrics5020029





