Associations of Frailty Status with Low-Mileage Driving and Driving Cessation in a Cohort of Older Drivers
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Predictors
Frailty Status
2.3. Outcomes
2.3.1. Low-Mileage Driver Status
2.3.2. Driving Cessation
2.4. Covariates
2.5. Statistical Analyses
3. Results
3.1. Low-Mileage Driver Status Outcome
3.1.1. ≤3000 Miles per Year
3.1.2. ≤1865 Miles per Year
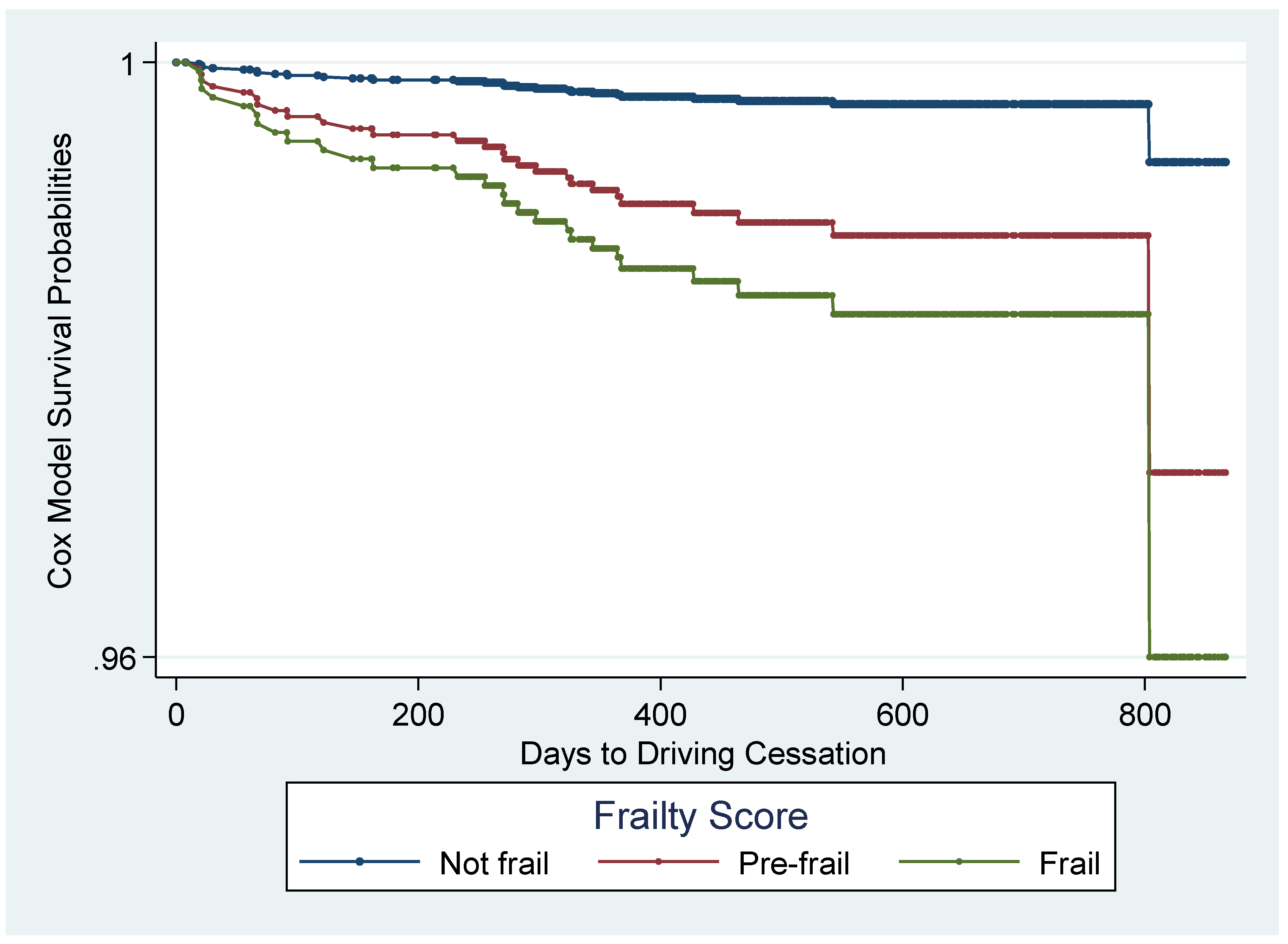
3.2. Driving Cessation Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Pomidor, A. Clinician’s Guide to Assessing and Counseling Older Drivers; National Highway Traffic Safety Administration: Washington, DC, USA, 2015.
- Choi, M.; Lohman, M.C.; Mezuk, B. Trajectories of cognitive decline by driving mobility: Evidence from the Health and Retirement Study. Int. J. Geriatr. Psychiatry. 2014, 29, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Liddle, J.; Gustafsson, L.; Bartlett, H.; McKenna, K. Time use, role participation and life satisfaction of older people: Impact of driving status. Aust. Occup. Ther. J. 2012, 59, 384–392. [Google Scholar] [CrossRef] [PubMed]
- Marottoli, R.A.; De Leon, C.F.M.; Glass, T.A.; Williams, C.S.; Cooney, L.M., Jr.; Berkman, L.F.; Tinetti, M.E. Driving cessation and increased depressive symptoms: Prospective evidence from the New Haven EPESE. J. Am. Geriatr. Soc. 1997, 45, 202–206. [Google Scholar] [CrossRef] [PubMed]
- Whelan, M.; Langford, J.; Oxley, J.; Koppel, S.; Charlton, J. The Elderly and Mobility: A Review of the Literature; Report No. 255; Victoria, Australia, November 2006. [Google Scholar]
- Antin, J.F.; Guo, F.; Fang, Y.; Dingus, T.A.; Perez, M.A.; Hankey, J.M. A validation of the low mileage bias using naturalistic driving study data. J. Safety. Res. 2017, 63, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Janke, M.K. Accidents, mileage, and the exaggeration of risk. Accid. Anal. Prev. 1991, 23, 183–188. [Google Scholar] [CrossRef]
- Bieniek, J.; Wilczyński, K.; Szewieczek, J. Fried frailty phenotype assessment components as applied to geriatric inpatients. Clin. Interv. Aging. 2016, 11, 453–459. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A. Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef]
- Xue, Q. The frailty syndrome: Definition and natural history. Clin. Geriatr. Med. 2011, 27, 1–15. [Google Scholar] [CrossRef]
- Bandeen-Roche, K.; Seplaki, C.L.; Huang, J.; Buta, B.; Kalyani, R.R.; Varadhan, R.; Kasper, J.D. Frailty in older adults: A nationally representative profile in the United States. J. Gerontol. A. Biol. Sci. Med. Sci. 2015, 70, 1427–1434. [Google Scholar] [CrossRef]
- Papa, M.; Boccardi, V.; Prestano, R.; Angellotti, E.; Desiderio, M.; Marano, L.; Rizzo, M.R.; Paolisso, G. Comorbidities and crash involvement among younger and older drivers. PLoS ONE 2014, 9, e94564. [Google Scholar] [CrossRef]
- Li, G.; Eby, D.W.; Santos, R.; Mielenz, T.J.; Molnar, L.J.; Strogatz, D.; Zakrajsek, J. Longitudinal Research on Aging Drivers (LongROAD): Study design and methods. Inj. Epidemiol. 2017, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- Bandeen-Roche, K.; Xue, Q.-L.; Ferrucci, L.; Walston, J.; Guralnick, J.M.; Chaves, P.; Fried, L.P. Phenotype of frailty: Characterization in the Women’s Health and Aging studies. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Bouillon, K.; Kivimaki, M.; Hamer, M.; Sabia, S.; Fransson, E.I.; Singh-Manoux, A.; Batty, G.D. Measures of frailty in population-based studies: An overview. BMC Geriatr. 2013, 13, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Buckinx, F.; Rolland, Y.; Reginster, J.-Y.; Ricour, C.; Petermans, J.; Bruyere, O. Burden of frailty in the elderly population: Perspectives for a public health challenge. Arch. Public. Health. 2015, 73, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet. 2013, 381, 752–762. [Google Scholar] [CrossRef]
- Langford, J.; Methorst, R.; Hakamies-Blomqvist, L. Older drivers do not have a high crash risk—A replication of low mileage bias. Accid. Anal. Prev. 2006, 38, 574–578. [Google Scholar] [CrossRef]
- Hakamies-Blomqvist, L.; Raitanen, T.; O’Neill, D. Driver ageing does not cause higher accident rates per km. Transp. Res. Part F Traffic Psychol. Behav. 2002, 5, 271–274. [Google Scholar] [CrossRef]
- Healthmeasures - NIH Toolbox. 2017. Available online: http://www.healthmeasures.net/explore-measurement-systems/nih-toolbox (accessed on 15 April 2019).
- Wallace, R.B.; Herzog, A.R. Overview of the Health Measures in the Health and Retirement Study. J. Hum. Resour. 1995, 30, S84–S107. [Google Scholar] [CrossRef]
- Ng, L.S.; Guralnik, J.M.; Man, C.; DiGuiseppi, C.; Strogatz, D.; Eby, D.W.; Li, G. Association of Physical Function With Driving Space and Crashes Among Older Adults. Gerontologist. 2020, 60, 69–79. [Google Scholar] [CrossRef]
- Clover, K.; Lambert, S.D.; Oldmeadow, C.; Britton, B.; King, M.T.; Mitchell, A.J.; Carter, G. PROMIS depression measures perform similarly to legacy measures relative to a structured diagnostic interview for depression in cancer patients. Qual. Life Res. 2018, 27, 1357–1367. [Google Scholar] [CrossRef]
- Carr, D.B.; Flood, K.L.; Steger-May, K.; Schechtman, K.B.; Binder, E.F. Characteristics of frail older adult drivers. J. Am. Geriatr. Soc. 2006, 54, 1125–1129. [Google Scholar] [CrossRef] [PubMed]
- Owsley, C.; Stalvey, B.; Wells, J.; Sloane, M.E. Older drivers and cataract: Driving habits and crash risk. J. Gerontol. A Biol. Sci. Med. Sci. 1999, 54, M203–M211. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S. Modeling and variable selection in epidemiologic analysis. Am. J. Public Health. 1989, 79, 340–349. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata Statistical Software: Release 14; StataCorp LP: College Station, TX, USA, 2015. [Google Scholar]
- Bond, E.G.; Durbin, L.L.; Cisewski, J.A.; Qian, M.; Guralnik, J.M.; Kasper, J.D.; Mielenz, T.J. Association between baseline frailty and driving status over time: A secondary analysis of The National health and Aging Trends Study. Inj. Epidemiol. 2017, 4, 9. [Google Scholar] [CrossRef]
- Man, C.; Ng, L.S.; Molnar, L.J.; Eby, D.W.; Ryan, L.H.; Diguiseppi, C.; Strogats, D.; Betz, M.E.; Hill, L.; Guralnik, J.; et al. Frailty Phenotype and Self-Reported Crashes and Driving Space: Baseline AAA LongROAD (Research Brief). J Transp. Health. 2017, 15, 100626. [Google Scholar] [CrossRef]
- Dedeyne, L.; Deschodt, M.; Verschueren, S.; Tournoy, J.; Gielen, E. Effects of multi-domain interventions in (pre) frail elderly on frailty, functional, and cognitive status: A systematic review. Clin. Interv. Aging. 2017, 12, 873–896. [Google Scholar] [CrossRef]
- Puts, M.T.E.; Toubasi, S.; Andrew, M.K.; Ashe, M.C.; Ploeg, J.; Atkinson, E.; McGilton, K. Interventions to prevent or reduce the level of frailty in community-dwelling older adults: A scoping review of the literature and international policies. Age Ageing. 2017, 46, 383–392. [Google Scholar] [CrossRef]
| N (%) | |
|---|---|
| Gender (N = 2964) | |
| Male | 1396 (47.10) |
| Female | 1568 (52.90) |
| Age (N = 2964) | |
| 65–69 | 1232 (41.57) |
| 70–74 | 1027 (34.65) |
| 75–79 | 705 (23.79) |
| Marital Status (N = 2936) | |
| Married/Living with Partner | 1965 (66.93) |
| Divorced/Separated/Never Married | 596 (20.30) |
| Widowed | 375 (12.77) |
| Education Level (N = 2955) | |
| High School or Less | 335 (11.34) |
| Some College | 721 (24.40) |
| Bachelor’s Degree | 690 (23.35) |
| Advanced Degree | 1209 (40.91) |
| Depression (N = 2960) | |
| ≤55 | 2774 (93.72) |
| >55 | 186 (6.28) |
| Cognitive Health (N = 2883) | |
| 0–10 | 1493 (51.79) |
| 11–20 | 1390 (48.21) |
| Vision (N = 2962) | |
| Poor to Good | 973 (32.85) |
| Very Good | 1249 (42.17) |
| Excellent | 740 (24.98) |
| Driving Importance (N = 2961) | |
| 1 to 5 | 109 (3.68) |
| 6 | 404 (13.64) |
| 7–Completely | 2448 (82.67) |
| Frailty Status (N = 2964) | |
| Frail | 86 (2.90) |
| Prefrail | 1656 (55.87) |
| Not Frail | 1222 (41.23) |
| < 3000 miles per year | |
| Frailty Status Frailty (not frail, prefrail, frail) | Adjusted Risk Ratio (95% CI)1 1.36 (1.11, 1.65) |
| < 1865 miles per year | |
| Frailty Status Frailty (not frail, prefrail, frail) | Adjusted Risk Ratio (95% CI)1 2.38 (1.63, 3.46) |
| Crude HR (95% Confidence Interval) 1 | Adjusted Hazard Ratio (95% Confidence Interval) 2 | |
|---|---|---|
| Frailty Status | ||
| Prefrail | 4.04 (1.72–9.46) | 4.15 (1.89–9.10) |
| Frail | 8.25 (2.08–32.75) | 6.08 (1.36–27.26) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crowe, C.L.; Kannoth, S.; Andrews, H.; Strogatz, D.; Li, G.; DiGuiseppi, C.; Hill, L.; Eby, D.W.; Molnar, L.J.; Mielenz, T.J. Associations of Frailty Status with Low-Mileage Driving and Driving Cessation in a Cohort of Older Drivers. Geriatrics 2020, 5, 19. https://doi.org/10.3390/geriatrics5010019
Crowe CL, Kannoth S, Andrews H, Strogatz D, Li G, DiGuiseppi C, Hill L, Eby DW, Molnar LJ, Mielenz TJ. Associations of Frailty Status with Low-Mileage Driving and Driving Cessation in a Cohort of Older Drivers. Geriatrics. 2020; 5(1):19. https://doi.org/10.3390/geriatrics5010019
Chicago/Turabian StyleCrowe, Christopher L., Sneha Kannoth, Howard Andrews, David Strogatz, Guohua Li, Carolyn DiGuiseppi, Linda Hill, David W. Eby, Lisa J. Molnar, and Thelma J. Mielenz. 2020. "Associations of Frailty Status with Low-Mileage Driving and Driving Cessation in a Cohort of Older Drivers" Geriatrics 5, no. 1: 19. https://doi.org/10.3390/geriatrics5010019
APA StyleCrowe, C. L., Kannoth, S., Andrews, H., Strogatz, D., Li, G., DiGuiseppi, C., Hill, L., Eby, D. W., Molnar, L. J., & Mielenz, T. J. (2020). Associations of Frailty Status with Low-Mileage Driving and Driving Cessation in a Cohort of Older Drivers. Geriatrics, 5(1), 19. https://doi.org/10.3390/geriatrics5010019





